Abstract
Objectives
We analyzed the dosage pattern of anesthetic drugs administered to maintain anesthesia during rigid bronchoscopy.
Methods
We enrolled a total of 81 patients who underwent rigid bronchoscopy under total intravenous anesthesia between April 2015 and March 2019. Anesthesia was maintained using propofol (target brain concentration 2.0 - 6.0 µg/mL) and remifentanil (target brain concentration 2.0 - 6.0 ng/mL). We analyzed the dosage patterns of the anesthetic agents during the procedure, as well as the changes in the dose of the anesthetic agents and the number of procedures repeated in the same patient.
Results
The dose of propofol administered per minute to maintain anesthesia was inversely correlated with the total operation time (r2 = 0.355, β = -0.067, P < 0.000) but was not significantly correlated with the number of times the procedure was repeated. The dose of remifentanil did not significantly differ during repeated procedures in the same patient.
Conclusions
The dose of propofol infusion tended to decrease over time during the rigid bronchoscopy procedure. This pattern was specific to propofol but not to remifentanil using TIVA. Understanding the pharmacokinetic properties of anesthetic drugs will help in their appropriate administration.
Keywords: Airway Obstruction, Bronchoscope, General Anesthesia, Intravenous Anesthesia, Propofol, Remifentanil
1. Background
Rigid bronchoscopy is performed under deep sedation or general anesthesia. Therefore, maintaining oxygenation and ventilation via the uncuffed and open rigid bronchoscope requires the use of ventilation strategies that may be difficult to perform. The appropriate ventilation technique should be determined based on staff expertise and equipment availability (1). Hence, previous studies have mainly focused on various anesthetic management methods related to ventilation care (1-4). However, there has been no study on the dosage patterns of drugs administered during anesthetic management. Anesthesia can be maintained using either the inhalation or intravenous technique. Propofol is an ideal choice for anesthesia maintenance during total intravenous anesthesia because of its rapid onset and offset, as well as its effect on airway reflex suppression. The rigid bronchoscopy procedure constantly requires intense anesthesia induction. Therefore, we expected that drug doses required to maintain adequate anesthesia would constantly be large.
2. Objectives
In this study, we aimed to analyze the infusion pattern of anesthetic drugs used to maintain anesthesia during rigid bronchoscopy.
3. Methods
3.1. Ethical Considerations
The study was performed following the principles of the 1975 Helsinki Declaration (revised in 2018) and approved by the Institutional Review Board of our hospital (IRB no. 2019-04-011).
3.2. Patient Population
We reviewed the electronic medical records of patients aged > 18 years who had undergone rigid bronchoscopy under Total Intravenous Anesthesia (TIVA) between April 2015 and March 2019. Patients whose procedure was not completed or anesthesia was interrupted during the procedure, as well as those who had missing data, were excluded.
3.3. Anesthetic Management
Noninvasive blood pressure monitoring, electrocardiography, and pulse oximetry were used for patient monitoring. The hemodynamic parameters were recorded every three minutes until the end of the procedure to monitor the change in the vital signs during the continuous infusion of anesthetic maintenance agents and every five minutes in the recovery room. General anesthesia was induced with propofol and remifentanil using a target-controlled infusion pump (Module DPS Orchestra IS 3, Fresenius Vial, France). Depending on the patient’s renal function, rocuronium (0.8 - 1.0 mg/kg) or atracurium (0.4 - 0.6 mg/kg) was used for muscle relaxation. Patients who had a history of kidney disease or whose serum creatinine levels were higher than the normal range (0.8 - 1.3 mg/dL) in the preoperative tests were administered atracurium. A rigid bronchoscope was inserted and connected to the ventilator circuit using a corrugated tube on the side port. Initially, 100% oxygen was applied via high-flow manual bagging and stabilized during the procedure. The fraction of inspired oxygen was changed from 0.5 to 1.0 while maintaining the oxygen saturation of more than 95%. Anesthesia was maintained using propofol (target brain concentration 2.0 - 6.0 µg/mL), and additional midazolam was administered as needed to keep the Bispectral index below 60. The infusion rate of remifentanil (target brain concentration 2.0 - 6.0 ng/mL) was constantly adjusted for varying systolic blood pressure and was maintained within 20% of baseline. At the end of the procedure, the bronchoscope was removed and replaced with a plain endotracheal tube to secure the airway, and then, reversal agents were administered. After extubation, patients were assessed for spontaneous breathing and recovery of consciousness and transferred to the recovery room.
3.4. Data Collection
One researcher retrospectively reviewed the electronic medical records. The patients’ preoperative evaluation data were extracted, including the presence of respiratory distress, performed emergency procedures, and the cause and location of airway obstruction. Data on the procedure time, anesthesia time, and the total dosage of anesthetic drugs were collected from the anesthesia records. Data on complications related to the rigid bronchoscopy procedure (such as pain, nausea, pneumothorax) were collected from the nursing charts.
3.5. Outcome Measures
Based on the total dose of propofol and remifentanil administered during the procedure and the duration of the procedure, we converted the dose of each agent to the dose administered per minute during the procedure for each patient. We analyzed the differences in the dose of drug administered per minute according to the number of procedures. We also investigated whether differences in drug doses required to maintain anesthesia were related to the overall procedure time or the number of repeated procedures. In addition, we analyzed the incidence and the type of complications related to the procedure.
3.6. Statistical Analysis
Statistical analysis was performed using SPSS software (IBM SPSS Statistics 21; IBM Corp., USA). Linear regression analysis was used to determine the correlation of differences in drug doses required to maintain anesthesia with the overall procedure time and the number of repeated procedures. P values of < 0.05 indicated statistical significance. Univariate regression analysis was performed to evaluate the relationship between variables and complications. Multivariate stepwise modeling was then performed using variables with p-values of ≤ 0.25 from the univariate analysis.
4. Results
A total of 81 patients underwent rigid bronchoscopy between April 2015 and March 2019. All patients were classified within grade II to IV of the ASA physical status. Thirty-four (42.0%) patients had dyspnea before the procedure, and the most common reason for the procedure was airway mass effect due to granulation or tumor growth (38 patients, 46.9%). The most common lesion location was the main bronchi (43 patients, 53.1%), followed by the subglottic airway and the trachea (30 patients, 37%) (Table 1).
Table 1. Demographic and Perioperative Data.
| Variable | Patientsa |
|---|---|
| Gender | |
| Male | 41 (50.6) |
| Female | 40 (49.4) |
| Age (y) | 59.1 ± 12.3 |
| Height (cm) | 161.1 ± 6.9 |
| Weight (kg) | 63.7 ± 11.4 |
| BMI | 24.7 ± 4.4 |
| Dyspnea before the procedure | 34 (42.0) |
| Cause of airway problem | |
| Trauma (stenosis) | 9 (11.1) |
| Mass effect (granulation, tumor growth) | 38 (46.9) |
| malacic change | 3 (3.7) |
| Correction of the previous procedure | 19 (23.5) |
| Other | 12 (14.8) |
| Site of the airway problem | |
| Subglottic or trachea | 30 (37.0) |
| Main bronchus | 43 (53.1) |
| Branch of bronchus | 8 (9.9) |
| Procedure time (min) | 60.0 [38.5-75.0] |
| Anesthetic time (min) | 85.0 [65.0-105.0] |
| Patients received additional midazolam | 29 (35.8) |
| Total dose of midazolam (mg) | 1.01 ± 1.54 |
| Total infusion rate of anesthetic drugs | |
| Propofol (mg) | 567.3 ± 246.8 |
| Remifentanil (µg) | 462.0 ± 272.0 |
| Infusion rate per minute during the procedure | |
| Propofol (mg/min) | 10.3 ± 3.9 |
| Remifentanil (µg/min) | 7.9 ± 3.2 |
Abbreviation: BMI, body mass index.
aData are presented as number (%), mean ± SD, or median [interquartile range].
The dose of administered propofol per minute to maintain anesthesia showed a linear correlation with the total procedure time (r2 = 0.355, β = -0.067, P < 0.001). It was estimated that there was an inverse correlation in the curve goodness of fit (r2 = 0.565, β = -0.752, P < 0.001, Figure 1). However, the dose of administered remifentanil per minute did not show a significant correlation with the total procedure time (r2 = 0.093, β = 0.305, P = 0.310). In addition, the dose of administered propofol per minute when the procedure was repeated in the same patient among those who underwent the procedure three or more times was not significantly correlated with the number of times the procedure was repeated, except for just two patients (Table 2).
Figure 1. The curve fit graph of regression analysis. The graph shows that the total propofol infusion rate per minute was inversely correlated with the procedure duration. OP time: operation time.
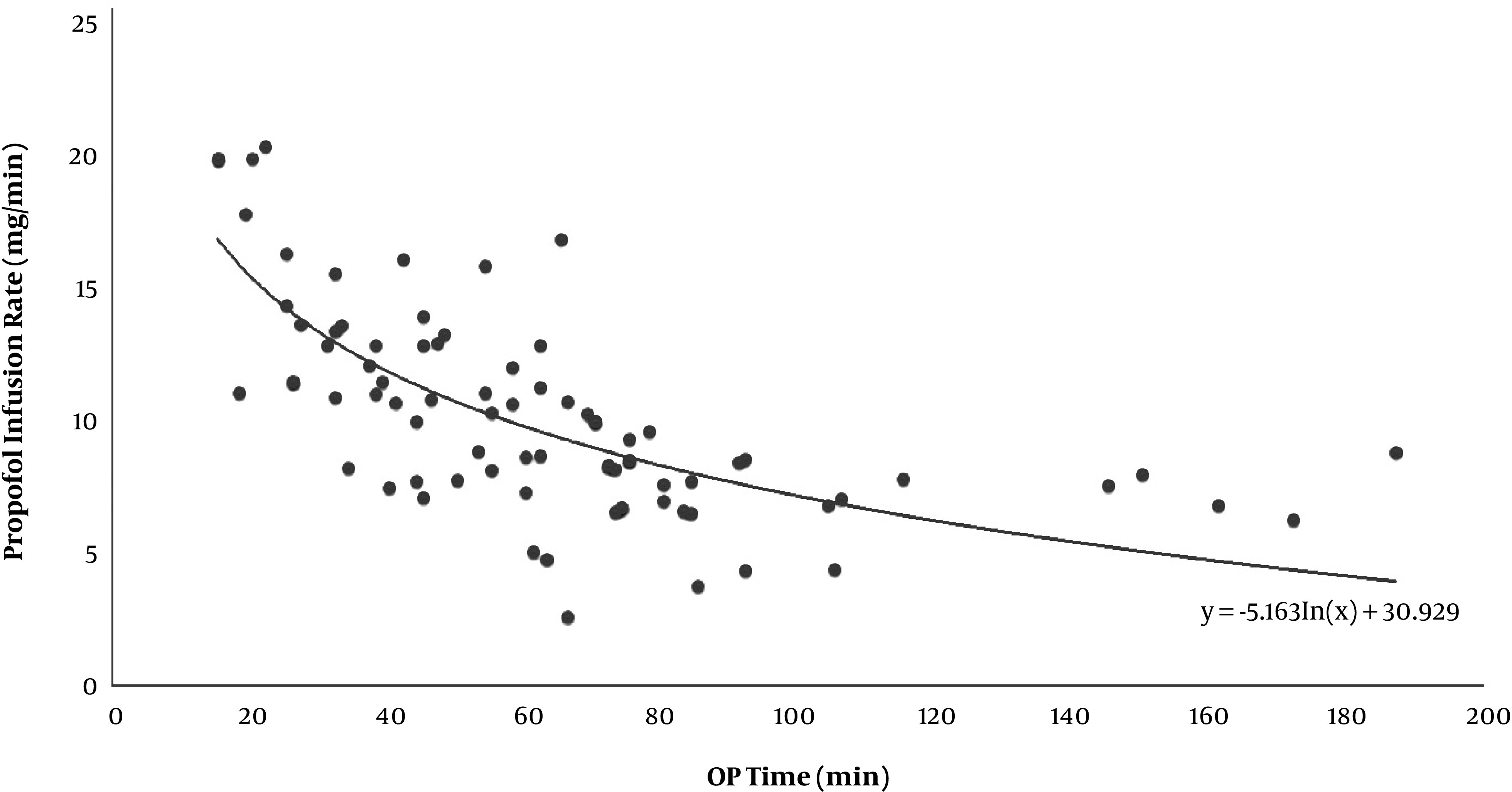
Table 2. Linear Regression Analysis of the Changes in the Total Propofol Infusion Rate per Minute in Patients Who Underwent More Than Three Repeated Procedures.
| ID | r2 | β | P Value |
|---|---|---|---|
| A | 0.95 | -1.36 | 0.03 |
| B | 0.68 | 0.99 | 0.38 |
| C | 0.00 | -0.07 | 0.96 |
| D | 0.01 | -0.26 | 0.89 |
| E | 0.72 | 1.62 | 0.36 |
| F | 0.37 | 1.20 | 0.58 |
| G | 0.02 | -0.94 | 0.91 |
| H | 0.51 | 0.45 | 0.01 |
| I | 0.00 | -0.07 | 0.93 |
| J | 0.38 | 0.52 | 0.10 |
The most common complication of rigid bronchoscopy was hemorrhage. Pneumothorax due to airway injury occurred in one patient (Table 3). However, none of the complications were life-threatening or severe. Univariate regression analysis of the complication outcome was performed using a variety of patient variables as potential predictors (Table 4).
Table 3. Complications of Rigid Bronchoscopy.
| Variable | Number of Patients (%) |
|---|---|
| Dental and facial trauma | 2 (2.4) |
| Hemorrhage | 6 (7.3) |
| Pneumothorax | 1 (1.2) |
| Central airway obstruction a | 2 (2.4) |
| Peripheral airway obstruction b | 2 (2.4) |
| Airway trauma | 2 (2.4) |
aTumor, blood, secretions
bAsthma, chronic bronchitis, emphysema, bronchospasm
Table 4. Predictors of Complications in Univariate Logistic Regression Analysis.
| Variable | χ2 | P Value | OR [95% CI] |
|---|---|---|---|
| Age | 0.36 | 0.55 | 0.98 [0.92 - 1.04] |
| Gender | 0.04 | 0.95 | 0.96 [0.24 - 3.79] |
| BMI | 2.37 | 0.14 | 0.89 [0.78 - 1.04] |
| ASA score | 0.89 | 0.35 | 0.62 [0.22 - 1.71] |
| Cause of airway problem | 0.51 | 0.47 | 0.82 [0.47 - 1.42] |
| Emergent situation | 1.94 | 0.16 | 0.39 [0.10 - 1.48] |
| Repetition | 0.75 | 0.41 | 1.14 [0.84 - 1.56] |
| Procedure time | 1.11 | 0.28 | 0.99 [0.97 - 1.01] |
Abbreviations: ASA, American Society of Anesthesiologists Physical Status Score; BMI, body mass index
5. Discussion
Rigid bronchoscopy represents a challenge for anesthesiologists because it requires allowing the interventionist easy access to the airway with an adequate degree of muscle paralysis while maintaining proper ventilation and oxygenation (2-4). For any anesthetic procedure, the combination of hypnosis, analgesia, muscular relaxation, and Total Intravenous Anesthesia (TIVA) is required. Specific considerations for airway surgery via rigid bronchoscopy include the need for a rapid and complete offset of anesthetic agents.
Until the development of propofol, TIVA was rarely performed for surgeries with planned extubation owing to the prolonged emergences. Infusing propofol using pharmacokinetic parameters to target blood concentrations has been considered a significant improvement in propofol administration. Propofol has several advantages over other anesthetics, one of which is a more relaxing effect on the pharyngeal musculature compared to thiopental (5), a commonly used anesthetic induction agent. In particular, the intravenous agent is more useful than the inhalation gas due to a large amount of leakage around the scope without packing.
In the past, surgery was the primary method of treatment for central airway obstruction. Recently, palliative procedures have been widely used, such as laser resection, coagulation, balloons, and insertion of silicone stents using rigid bronchoscopes (6-8). However, even if the airway is expected to be permanently secured using the stent, some complications may arise (9). Complication rates vary depending on the patient health status and the performed procedure (10-12). Ost et al described that the predictors of the increased complication rate of therapeutic bronchoscopy include emergent situation, ASA score, repetition, and the need for moderate sedation (13). In our study, all patients underwent rigid bronchoscopy under general anesthesia, and there were no systemic cardiovascular complications that could occur during hypoxemia and hypercapnia. However, there were some local complications. Hemorrhage was the most frequent adverse event, occurring in 7% of patients, but no additional procedure was required for hemostasis. One patient developed pneumothorax, and chest tube insertion was performed.
Endobronchial tumor destruction and removal are commonly performed using rigid bronchoscopy. Other frequently used indications include mechanical dilation, endobronchial ablation, and airway stent placement for obstructions, tracheoesophageal fistulae, or tracheobronchomalacia (14-16). In this study, the most frequent indication for this procedure was a therapeutic approach to mass effects, such as granulations and tumor growth (46.9%).
This study has some limitations. The number of patients was small, and the patient’s actual plasma drug levels were not confirmed. In addition, due to the retrospective nature of the study, various aspects were not considered because the results were interpreted based only on the recorded objective facts.
Nevertheless, we found that the dose of administered propofol decreased over time. This pattern was specific to propofol but not to remifentanil during TIVA. However, the dose administered per minute was not significantly correlated with the number of times the procedure was repeated in the same patient. These results are associated with the pharmacokinetic properties of both drugs, and understanding these mechanisms will help in the adequate administration of the drug. Therefore, when maintaining anesthesia with TIVA using propofol in a rigid bronchoscope procedure, caution should be exercised since large drug doses may be required from the early stage.
Footnotes
Authors' Contribution: Study concept and design: SH. Yun., CH Kim, and JC. Park.; Analysis and interpretation of data: SH. Yun.; Drafting of the manuscript: JC. Park.; Critical revision of the manuscript for important intellectual content: SH. Yun., CH. Kim, and JC. Park; Statistical analysis: SH. Yun. and JC. Park
Conflict of Interests: No potential conflict of interest relevant to this article is reported.
Ethical Approval: The study was performed following the principles of the 1975 Helsinki Declaration (revised in 2018) and was approved by the Institutional Review Board of our hospital (IRB no. 2019-04-011).
Funding/Support: This study was conducted without any financial support.
Contributor Information
Jong Cook Park, Email: pjcook@jejunu.ac.kr.
So Hui Yun, Email: juguyam@gmail.com.
Changhwan Kim, Email: masque70@naver.com.
References
- 1.Pathak V, Welsby I, Mahmood K, Wahidi M, MacIntyre N, Shofer S. Ventilation and anesthetic approaches for rigid bronchoscopy. Ann Am Thorac Soc. 2014;11(4):628–34. doi: 10.1513/AnnalsATS.201309-302FR. [DOI] [PubMed] [Google Scholar]
- 2.Jose RJ, Shaefi S, Navani N. Anesthesia for bronchoscopy. Curr Opin Anaesthesiol. 2014;27(4):453–7. doi: 10.1097/ACO.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 3.Min JY, Jo H, Roh K, Chung MY. Preventing deoxygenation with high flow nasal cannula oxygen during induction of general anesthesia for rigid bronchoscopy: Two case reports. Medicine (Baltimore). 2019;98(27):e15998. doi: 10.1097/MD.0000000000015998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chadha M, Kulshrestha M, Biyani A. Anaesthesia for bronchoscopy. Indian J Anaesth. 2015;59(9):565–73. doi: 10.4103/0019-5049.165851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hemmings HJ, Egan TD. Pharmacology and physiology for anesthesia. 2nd ed. Elsevier; 2018. [Google Scholar]
- 6.Giovacchini CX, Kessler ER, Merrick CM, Gao J, Wang X, Wahidi MM, et al. Clinical and radiographic predictors of successful therapeutic bronchoscopy for the relief of malignant central airway obstruction. BMC Pulm Med. 2019;19(1):219. doi: 10.1186/s12890-019-0987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murgu SD, Egressy K, Laxmanan B, Doblare G, Ortiz-Comino R, Hogarth DK. Central Airway Obstruction: Benign Strictures, Tracheobronchomalacia, and Malignancy-related Obstruction. Chest. 2016;150(2):426–41. doi: 10.1016/j.chest.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Ernst A, Feller-Kopman D, Becker HD, Mehta AC. Central airway obstruction. Am J Respir Crit Care Med. 2004;169(12):1278–97. doi: 10.1164/rccm.200210-1181SO. [DOI] [PubMed] [Google Scholar]
- 9.Semaan R, Yarmus L. Rigid bronchoscopy and silicone stents in the management of central airway obstruction. J Thorac Dis. 2015;7(Suppl 4):S352–62. doi: 10.3978/j.issn.2072-1439.2015.11.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Lima A, Kheir F, Majid A, Pawlowski J. Anesthesia for interventional pulmonology procedures: a review of advanced diagnostic and therapeutic bronchoscopy. Can J Anaesth. 2018;65(7):822–36. doi: 10.1007/s12630-018-1121-3. [DOI] [PubMed] [Google Scholar]
- 11.Batra H, Yarmus L. Indications and complications of rigid bronchoscopy. Expert Review of Respiratory Medicine. 2018;12(6):509–20. doi: 10.1080/17476348.2018.1473037. [DOI] [PubMed] [Google Scholar]
- 12.Dincq AS, Gourdin M, Collard E, Ocak S, D'Odemont JP, Dahlqvist C, et al. Anesthesia for adult rigid bronchoscopy. Acta Anaesthesiol Belg. 2014;65(3):95–103. [PubMed] [Google Scholar]
- 13.Ost DE, Ernst A, Grosu HB, Lei X, Diaz-Mendoza J, Slade M, et al. Complications Following Therapeutic Bronchoscopy for Malignant Central Airway Obstruction: Results of the AQuIRE Registry. Chest. 2015;148(2):450–71. doi: 10.1378/chest.14-1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Selzer AR, Murrell M, Shostak E. New trends in interventional pulmonology. Curr Opin Anaesthesiol. 2017;30(1):17–22. doi: 10.1097/ACO.0000000000000414. [DOI] [PubMed] [Google Scholar]
- 15.Jeon K, Kim H, Yu CM, Koh WJ, Suh GY, Chung MP, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol. 2006;1(4):319–23. [PubMed] [Google Scholar]
- 16.Freitag L, Darwiche K. Endoscopic treatment of tracheal stenosis. Thorac Surg Clin. 2014;24(1):27–40. doi: 10.1016/j.thorsurg.2013.10.003. [DOI] [PubMed] [Google Scholar]


