On 11 March 2020, the World Health Organization declared the COVID-19 outbreak a pandemic. Just over four months later, with over 15 million people infected in over 200 countries, and global mortality exceeding 600,000, both non-pharmacological and pharmacological interventions have been deployed to try to limit patient exposure, arrest further spread and provide medical treatments for those infected.1 COVID-19 has high morbidity and mortality due to autoimmune destruction of the lungs stemming from the release of a storm of pro-inflammatory cytokines.2 Other unusual features of this COVID-19 pandemic include a marked thrombotic diathesis, high rates of acute kidney injury and gross destructive parenchymal lung damage.3,4
Non-pharmacological options available to be deployed include personal hygiene and ‘social distancing’, hard isolation (“shield-at-home” lockdowns), other physical distancing and movement restrictions (travel bans, country border and school/university closures), shielding of vulnerable groups, and robust testing and contact tracing programmes.5 Many advanced healthcare economies (certainly the UK, less so Germany) lost their best chance of controlling national epidemics close to their onset due to a toxic melange of inadequate public health resource to attempt community-based case detection with contact tracing and low pandemic preparedness. Pharmacological interventions with a proven benefit at this early stage of the pandemic include the use of immunomodulatory therapeutics in severely respiratorily compromised (ventilated or oxygen-dependent) patients: remdesivir6 and dexamethasone,7 but neither of these interventions is applicable early in the disease or at scale.
It is striking to see how little difference among countries there has been in many measures deployed in this initial four-month period. Infection surge management – the immediate risk of ITU/hospitals being overwhelmed – was implemented almost ubiquitously, following harrowing scenes from Wuhan, then Lombardy. However, only two advanced countries – Sweden and the UK – have seriously considered a softer general approach to this challenge, namely to shield the more vulnerable while accepting some viral infection continuing to spread among the less vulnerable majority.8,9 The current infection, death and testing frequency statistics for the Scandinavian countries and the UK are shown in Table 1.
When most of a population is immune to an infectious disease, this provides indirect protection—herd immunity—to those who are not immune to the disease by acting as a bulwark against further population infection surges. This is how vaccines can be effective without 100% population coverage. In the case of SARS-CoV-2, with its ‘R’ number appearing to be around 3, epidemiologists had estimated that about 70% of the population attaining immunity should be enough to achieve herd immunity.10,11 This can happen when a population gets infected naturally or after there is a formal vaccination programme in place, either for everyone or for those at greatest risk of severe consequences of infection
In more detail, the Swedish strategy, directed and endorsed by State Epidemiologist (‘Stadsepidemiolog’) Anders Tegnell and his team, has meant that Sweden eschewed the more draconian ‘curve flattening’ measures of the sort deployed with great urgency in most other countries.12 Instead, Sweden opted to rely on an approach of more explicit cooperation between the state’s response and people’s individual responsibility to curtail the spread – itself a very ‘Swedish’ strategy, integrating the sociocultural concept of ‘folkvett’; the common sense of the people as a collective.12 Fully to situate the Swedish strategy, it must first be positioned within the broader framing of sociocultural responses to risk. Risks are conceptually more accurately broken down into risks and hazards; risk being the perceived chance of something happening, and the hazard being that ‘something’. Risks and hazards are both culturally coded, that is to say sociocultural forces underpin the understanding of both. This is particularly important to keep in mind with regards to hazards, as a hazardous object for one can be reduced to something benign by another.13 The response to the COVID-19 pandemic is, at its core, a matter of managing and prioritising risks, as is the response to any such crisis. The Swedish justification for their approach was therefore based on culturally relevant concerns and considerations, all informed by a Swedish perception of risk. The first concern was real doubt whether any population or economy could sustain a protracted lockdown, or repeated cycles of lockdown and relaxation (not known to be likely but more likely with rapid post-lockdown releases, based on previous pandemic behaviour). Second, the knock-on impact on non-COVID health would be highly significant in a situation where the population was locked down while health services were only able to prioritise COVID-19 healthcare; this is all too evident in the UK with cancer, heart and organ transplantation services all now in a serious situation.14 Third, the economic impact of the Swedish measures would likely be less severe than the precipitate collapse in government revenues seen elsewhere, as people in Sweden would be able to travel to work, or work at home, thereby reducing the need for significant employee furloughing.
The guiding judgement was to calibrate the impact of comprehensive ‘shield-at-home’ measures on the compact between the Swedish state and the individual Swedes inhabiting that state. Sweden has been referred to as a society of state individualism; an eclectic blend of deeply individualistic behaviours suspended within a framework of strong state and governance. As such, Swedes are far more open to voluntary cooperation with state requirements in the face of crisis, than to heavy-handed draconian directives of legislation. It is therefore telling that strategy and response have been largely coordinated by Anders Tegnell at the Public Health Agency of Sweden (‘Folkhälsomyndigheten’), part of the state as opposed to the government. The state as a broader entity is understood as being more apolitical, and therefore not subject to bipartisanship with regards to whether people are willing or unwilling to follow their guidelines. Given the nature of Swedish society as consensus-driven, the strategy ought to be read as a cooperation between the state and its citizenry, rather than the state dictating what is to be done.15,16
It would be a serious oversimplification to view the current Swedish strategy solely as the product of two people – Tegnell and Giesecke. It is noteworthy that Giesecke was appointed in 1995 and left his post in 2005; after an inter-regnum, the post was awarded to Anders Tegnell in 2013 who remains at the helm. Their pandemic preparedness strategy, therefore, seems likely to have enjoyed strong institutional support over a long period of time. Furthermore, it is important to remember that though the Public Health Agency has led the charge in devising the response to, and enacting the strategy against, the virus, it has required broad institutional, state, and governmental support and cooperation, even though some healthy scientific debate was publicly and rightly undertaken in the early stages.12 The need to ‘buy time’ to expand Sweden’s low base of hospital/ITU services (just as inadequate as the UK’s are) was clear at the outset, and was quickly achieved. Following from that, to avoid the societal challenges thought likely from maintaining, then emerging from, a ‘hard lockdown’, the policy of permitting limited infection to continue by controlled spread of viral infection in the Swedish population was envisaged as a sensible approach for the medium to long term, which could usefully lead to herd immunity. So, an explicit goal of their approach was to bridge the pre- and post-vaccine (or no vaccine) periods while still having a functional and functioning society.
Recent clinical and research findings suggest that the acquisition of neutralising IgM and IgG antibodies (Ab) is regularly seen in severely infected individuals (e.g. those ventilated in ITU). In a recent case series of 285 hospitalised COVID-19 patients from China, over 90% had seroconverted after three weeks of infection.17 Such Ab-generating responses to COVID-19 infections are much less commonly found in the far more numerous asymptomatic or mildly symptomatic (non-hospitalised community) patient cohorts. Table 218–24 shows the data from many of the reported series (some reports being pre-formal publication); it is clear that nowhere is the prevalence of IgG seropositivity high (the maximum being around 20%) or climbing convincingly over time. This is especially clear in Sweden, where the authorities publicly predicted 40% seroconversion in Stockholm by May 2020; the actual IgG seroprevalence was around 15%. Differences in testing methodology, viral load, clinical severity, intrinsic health of the studied population and various other potential confounding factors likely explain the inter-population variability.
Our uncertainty also extends to whether Ab produced in any clinical COVID-19 setting can confer any clinically-relevant protection against new or recurrent SARS-CoV-2 infections; some answers to this may come from the several ongoing convalescent plasma trials.25 There are certainly going to be more sophisticated tests of innate immunity measuring reactive T-cell populations against viral antigen targets which are more informative and clinically relevant than simple reliance on the generation of IgG and IgM Ab post infection. Nor do we know today whether there will be the development of a safe, reliable, affordable and accessible vaccine in a reasonable timeframe–this was not achieved with Dengue, HIV-AIDS, SARS, MERS or Zika.26
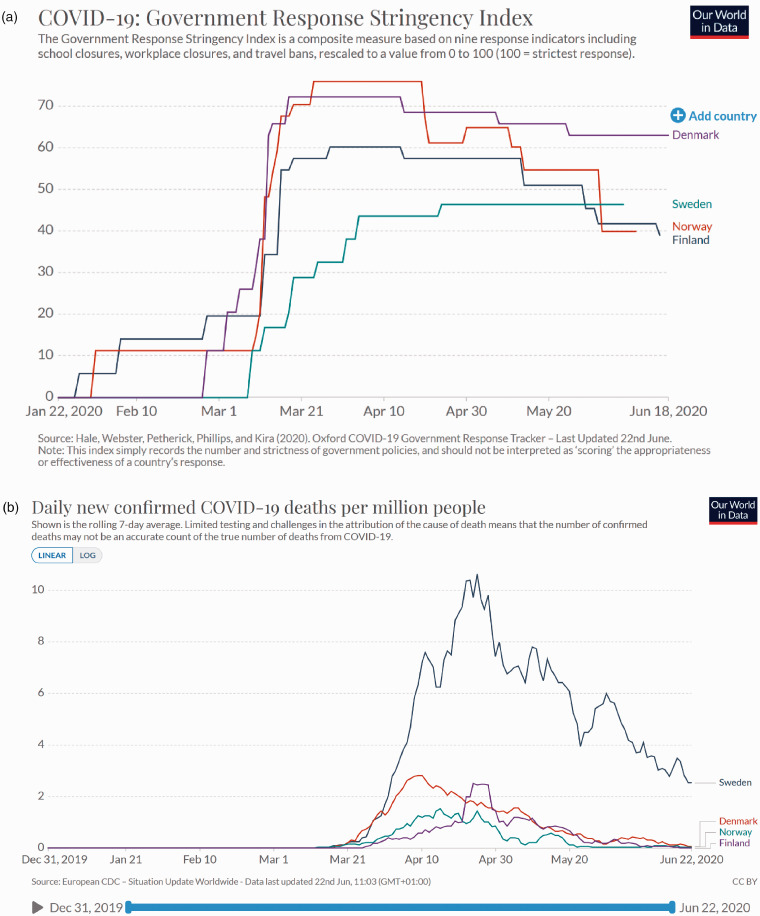
If we now make judgements about the first four months (so not as Sweden would wish us to do), what has happened in Sweden and the other Scandinavian countries is instructive. Table 3 lists in detail the different measures taken and their timings in Sweden, Denmark, Finland and Norway, while Figure 1a shows the ‘severity’ score for each country’s plans, as well as some of the data about the impact these measures had on the relevant populations. The inter-country disparities in cases of infection and mortality – with Sweden clearly having many more infections and fatalities (see Table 1 and Figure 1b); this is something that has seriously concerned the other members of the Scandinavian family.27 It is clear that not only are the rates of viral infection, hospitalisation and mortality (per million population) much higher than those seen in neighbouring Scandinavian countries, but also that the time-course of the epidemic in Sweden is different, with continued persistence of higher infection and mortality (as one is inexorably linked to the other) well beyond the few critical weeks period seen in Denmark, Finland and Norway, whose rapid lock-down measures seem to have been initially more successful in curtailing the infection surge.
Table 2.
Detailing the results of serological testing (with dates) for diverse tested populations (and different test methodologies): focus on IgM and IgG positivity for COVID-19. Scandinavian and other countries. March to June (inclusive) 2020.
| Country | Date (2020) | % SERO + ve (IgM/IgG) | Population tested | Reference citation |
|---|---|---|---|---|
| Sweden | ||||
| Malmo | April | 4% | General | 18 |
| Stockholm | April | 17% | General | 18 |
| Germany | ||||
| Gangelt | April | 14% | General (super-spreader event) | 19 |
| U | ||||
| East | April-May | 5% | General | 20 |
| London | April-May | 17% | General | 20 |
| Denmark | April | 2% | All Danish blood donors | 21 |
| USA | ||||
| New York State | April | 12.3% | General | 22 |
| New York City | May/June | 21.6% | General | 22 |
| Switzerland | ||||
| Geneva | April-May | 5%–10% | Bus Sante screening study | 23 |
| China | ||||
| Wuhan | March | 3% | General | 24 |
A very recent report from Spain also high-lights the lack of significant Ab production in a large studied population of over 60,000 infected people (ENE-COVID study). Published:July 06, 2020 DOI:https://doi.org/10.1016/S0140-6736(20)31483-5.
Table 3.
Detailing the nature and timing of the population movement and behaviour regulations brought into force during the period March to June (inclusive) 2020 in Sweden and close neighbouring countries. Data gathered from: local, national, international press; government official announcements; personal communications; https://nordregio.org/maps/mobility-changes-due-to-covid-19; https://www.scb.se/; https://www.gstatic.com/covid19/mobility/ (all last accessed 23.6.2020).
| Date of | Sweden | Denmark | Finland | Norway |
|---|---|---|---|---|
| Borders closed | Never undertaken* | 13 March | 18 March | 14 March |
| Junior school closed | Never undertaken | 13 March | 16 March | 12 March |
| High school / Uni changes | Distance education 17 March | 13 March | 16 March | 12 March |
| Ban on gatherings | >500 11 March >50 27 March | >500 13 March >10 17 March | >500 13 March >5 16 March | >5 24.3 |
| Pubs, bars, restaurants closed | Never undertaken: Some restrictions recommended | 13 March | 16 March | 12 March |
| Non-essential shops closed | Never undertaken | 18 March | 4 April | 12 March |
| Shielding of vulnerable (>70 years) | 16 March | 13 March | 17 March | 12 March |
| Population lock-down (not medicine/food) | Never undertaken | 11 March | 16 March | 13 March |
| Travel restrictions | International 11 March National 19 March | 13 March | International National 25 March | 13 March then 16 March |
| % Journeys to work in April (compared to Jan/Feb 2020) | 70%–80% | 40%–60% | 50%–60% | 50%–60% |
| Use of parks and recreation % usual | 240% (all regions) | 170% (all) | 220% (all) | 140% (all) |
| Travel by vehicle within/to capital in April % usual | ∼25% Stockholm | ∼10% Copenhagen | ∼10% Helsinki | ∼10% Oslo |
*The Swedish border never officially closed, but as neighbouring countries’ borders were all closed, this resulted in a de facto border closure. European directive recommending curtailing travel among Schengen group countries was imposed on 17 March.
Figure 1.
(a) This portrays the Government Response Stringency Index which melds severity and timing of imposed or recommended mitigatory measures. Figure 1(b) shows the daily new COVID-19 deaths per million population. Sweden had a clearly more severe death rate, and for much longer, than did its Scandinavian neighbours.
Table 1.
Cases, fatalities and testing numbers expressed as absolute numbers and also as per million population as of 23 June 2020 for Scandinavian countries (Sweden, Denmark, Norway and Finland) and for the UK.
| Country | Total cases | Total deaths | Cases pmp | Deaths pmp | Tests per 1000 | Date first death |
|---|---|---|---|---|---|---|
| U | 307,682 | 43,011 | 4,534 | 637 | 64 | 5 March |
| Sweden* | 60,837 | 5,161 | 6,026 | 511 | 38 | 11 March |
| Denmark | 12,561 | 603 | 2,169 | 104 | 156 | 12 March |
| Norway | 8,772 | 248 | 1,621 | 45 | 54 | 12 March |
| Finland | 7,155 | 327 | 1,292 | 59 | 42 | 20 March |
Data from the E-CDC; Johns Hopkins COVID-19; Our World in Data websites. *2366 COVID-19 patients have been in intensive care as of 23 June, which also includes fatalities and patients who have recovered and been discharged.
The data shown in Table 1 and Figure 1b clearly demonstrate first the degree to which the measures undertaken in Sweden were ‘less harsh’ (less severe and slower to be enacted) than those undertaken by its neighbours, and second that the behavioural impact of those measure on the Swedish national population was less evident, again compared to its neighbouring countries with their more stringent early measures. All of these differences we would contend were predictable, and deliberate, on the part of the Swedish authorities, and are, we contend, a possible explanation for the different time-course of their local epidemic (though there will likely be many other contributors; this is something that should become clearer over time). It is likely that some of this inter-Scandinavian difference in mortality outcomes might have also have arisen from a failure to shield the most vulnerable Swedes from viral infections (40%–50% of their cases have been in the elderly nursing home resident population).28 But as with other aspects of this unparalleled crisis, more time is needed to understand the many lasting impacts.
Despite the above critical remarks, there is neither justification for schadenfreude, nor for Swedes to feel unduly sheepish about their folkvett. Lest this strategy seem like just the traditional risky Swedish exceptionalism, we in the UK would do well to remember we nearly trod the same path. Right now, despite ‘strict (but tardy) lock-down’ in the UK, and the more measured Swedish response, both countries have high seven-day averaged SARS-CoV-2 death rates when compared to other Scandinavian and European countries (see Table 1 and Figure 1). Only once we can fully understand both the pandemic and the impact of the measures that were taken – after 1–2 years at least – can we then begin fairly to judge what was done correctly.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethics approval
Not required.
Guarantor
DJAG.
Contributorship
DJAG and EJWO wrote, revised, critiqued and finalised the article. The final version of the article was approved by both authors prior to publication.
Acknowledgements
None.
Provenance
Not commissioned; peer-reviewed by David Heymann and Martin Mckee.
ORCID iD
David J A Goldsmith https://orcid.org/0000-0002-4349-9193
References
- 1.Tay MZ, Poh CM, Rénia L, et al. The trinity of COVID-19: immunity, inflammation and intervention [published online ahead of print, 2020 Apr 28]. Nat Rev Immunol 2020; 1–12. doi:10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed]
- 2.Cascella M, Rajnik M, Cuomo A, et al. Features, Evaluation and Treatment Coronavirus (COVID-19). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. [PubMed]
- 3.Carsana L, Sonzogni A, Nasr A, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study [published online ahead of print, 2020 Jun 8]. Lancet Infect Dis 2020; S1473-3099(20)30434-5. doi:10.1016/S1473-3099(20)30434–5. [DOI] [PMC free article] [PubMed]
- 4.Ronco C, Reis T and Husain-Syed F. Management of acute kidney injury in patients with COVID-19 [published online ahead of print, 2020 May 14]. Lancet Respir Med 2020; S2213-2600(20)30229-0. doi:10.1016/S2213-2600(20)30229-0. [DOI] [PMC free article] [PubMed]
- 5.Bedford J, Enria D, Giesecke J, et al. COVID-19: towards controlling of a pandemic. Lancet 2020; 395(10229): 1015–1018. [DOI] [PMC free article] [PubMed]
- 6.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the Treatment of Covid-19 - Preliminary Report [published online ahead of print, 2020 May 22]. N Engl J Med 2020; NEJMoa2007764. doi:10.1056/NEJMoa2007764. [DOI] [PubMed]
- 7.Recovery Collaborative Group. Effect of Dexamethasone in Hospitalized Patients with COVID-19: Preliminary Report. medRxiv 2020-06-22. doi: 10.1101/2020.06.22.20137273 (last checked 22 June 2020). [DOI]
- 8.Sweden chooses a third way on coronavirus. https://www.ft.com/content/22302f60-95fb-11ea-af4b-499244625ac4 (last checked 22 June 2020).
- 9.Chief UK Scientist Valance’s interview given to Sky News 13th March 2020: https://www.youtube.com/watch?v=2XRc389TvG8. (last checked 31 May 2020).
- 10.Randolph HE and Barreiro LB. Herd Immunity: Understanding COVID-19. Immunity 2020; 52(5): 737-741. doi:10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed]
- 11.Kwok KO, Lai F, Wei WI, et al. Herd immunity - estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect 2020; 80(6): e32–e33. doi:10.1016/j.jinf.2020.03.027. [DOI] [PMC free article] [PubMed]
- 12.Regeringen (2020) Strategi med anledning av det nya coronaviruset. Accessible online: https://www.regeringen.se/regeringens-politik/regeringens-arbete-med-anledning-av-nya-coronaviruset/strategi-med-anledning-av-det-nya-coronaviruset/ (last checked 22 June 2020).
- 13.Fox NJ. Postmodern reflections on ‘risks’, ‘hazards’ and life choices. In: D. Lupton (ed.) Risk and sociocultural theory: new directions and perspectives. Cambridge: Cambridge University Press, 1999, pp. 12–34.
- 14.https://www.nice.org.uk/guidance/NG178.
- 15.Berggren H and Trägårdh L. Är svensken människa?: gemenskap och oberoende i det moderna Sverige. Norstedts: Elib. 2015.
- 16.Petersson O. Maktutredningen och statsindividualismen. Stockholm: Timbro, 2012.
- 17.Long QX, Liu BZ, Deng HJ, et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med 2020; 26(6): 845–848. doi:10.1038/s41591-020-0897-1. [DOI] [PubMed]
- 18.https://www.folkhalsomyndigheten.se/nyheter-och-press press/ nyhetsarkiv/2020/maj/forsta-resultaten-fran-pagaende-undersokning-av-antikroppar-for-covid-19-virus (last checked 22 June 2020).
- 19.Streek H, Schulte B, Kuemmerer B, et. al. Infection fatality rate of SARS-CoV-2 infection in a German community with a super-spreading event. medRxiv 2020.05.04. doi: 10.1101/2020.05.04.20090076. [DOI] [PMC free article] [PubMed]
- 20.https://www.gov.uk/government/publications/national-covid-19-surveillance-reports/sero-surveillance-of-covid-19/ (last checked 22 June 2020).
- 21.10.1101/2020.04.24.20075291. [DOI]
- 22.https://www.6sqft.com/new-york-covid-antibody-test-preliminary-results/ (last checked 22 June 2020).
- 23.Stringhini S, Wisniak A, Piumatti G, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study [published online ahead of print, 2020 Jun 11]. Lancet 2020; S0140-6736(20)31304-0. doi:10.1016/S0140-6736(20)31304-0. [DOI] [PMC free article] [PubMed]
- 24.Xu X, Sun J, Nie S, et al. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China [published online ahead of print, 2020 Jun 5]. Nat Med 2020; 10.1038/s41591-020-0949-6. doi:10.1038/s41591-020-0949-6.
- 25.Li L, Zhang W, Hu Y, et al. Effect of Convalescent Plasma Therapy on Time to Clinical Improvement in Patients With Severe and Life-threatening COVID-19: A Randomized Clinical Trial [published online ahead of print, 2020 Jun 3]. JAMA 2020; e2010044. doi:10.1001/jama.2020.10044. [DOI] [PMC free article] [PubMed]
- 26.Plotkin S. History of vaccination. Proc Natl Acad Sci USA 2014; 111(34): 12283–12287. doi:10.1073/pnas.1400472111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.https://www.nytimes.com/2020/06/22/world/europe/sweden-coronavirus-pariah-scandinavia.html (last checked 22 June 2020).
- 28.https://www.spectator.co.uk/article/dying-of-neglect-the-other-covid-care-home-scandal (last checked 22 June 2020).