Abstract
Purpose of review:
The aim of this article is to summarize the status of syndemic research on HIV and noncommunicable diseases (NCDs) to identify opportunities for improving research to benefit prevention and treatment of NCDs among persons living with HIV.
Recent findings:
The majority of research on syndemics of HIV and NCDs has been conducted in the United States, with few studies in low and middle-income countries. The substance abuse, violence, and AIDS syndemic model was used by a quarter of the studies, however, most other studies failed to outline a syndemic model for interpreting their findings. Mental illnesses were the dominant NCD (15 out of 16 studies), and only one study explored physical health NCDs.
Summary:
Recent studies referring to syndemics of HIV and NCDs often do not meet criteria for a syndemic framework. Future research needs to assure minimum criteria are met: articulation of two or more health conditions, descriptions of social/geographic context that impact the relationship among these conditions, a syndemic model with proposed mechanisms for interaction in the particular social/geographic context, and a population or context without the observed syndemic. Expanding the current syndemic research beyond the United States context and beyond mental illness also would enrich the field.
Keywords: comorbidity, developing countries, HIV, mental illness, noncommunicable diseases, syndemic
INTRODUCTION
All syndemics are local. Syndemic theory is unique approach in medicine and public health because it requires clear articulation of specific local sociocultural, economic, environmental, and geographic context influence the interaction of two or more health conditions [1-3]. Syndemic theory grew of out of anthropological observations in the 1990s that AIDS was more prevalent in inner-city context where substance use and violence clustered together - this came to be known as the substance abuse, violence, and AIDS (SAVA) syndemic [1]. More recently, the clustering of diabetes and depression among Mexican immigrant women in Chicago has been described as a syndemic interaction among violence, immigration, depression, diabetes, and abuse (VIDDA) [2]. This work has been expanded to understand why diabetes is more likely to be comorbid with depression in some context, but it is comorbid with HIV in a different context, and comorbid with tuberculosis in a different context [4], as well as uncovering how diabetes occurs in the context of obesity in most settings but malnutrition in another setting [5]. Similarly, in some populations inflammatory arthritis is more likely to be comorbid with a host of noncommunicable diseases, whereas in other context there is less multimorbidity associated with the condition [6]. Ultimately, syndenmic theory is a powerful tool to more accurately map the distribution of multimorbidity across populations and settings, and then to develop more effective approaches to prevention and treatment.
STATE OF THE RESEARCH: HIV AND NONCOMMUNICABLE DISEASE SYNDEMICS
Our objective was to determine the current state of the research field on syndemics of HIV and noncommunicable diseases (NCDs). As more people with HIV live with this as chronic condition and early mortality has dropped, it is increasingly important to consider how to prevent and treat NCDs in this population. A literature search was done on January 22nd, 2020, using OVID for articles within 2018 and 2019 that used the following key terms: syndemics, HIV, noncommunicable disease. This preliminary search yielded 126 articles. Articles that had infectious diseases as comorbid conditions, did not describe a syndemic and did not look at a population that was HIV positive were excluded from this review. From here, authors excluded 76 articles through the step of title exclusion; another 34 articles were excluded after reading the full text and using the same exclusion criteria. The search and exclusion steps yielded 16 articles.
The majority of the studies were cross-sectional epidemiologic studies with a purpose of quantifying and describing the prevalence of cooccurring mental health disorders and HIV (see Table 1). There was only one study that longitudinally assessed the additive effect of the syndemic relationship between mental health disorders over a year [7]. Jemison et al.[8] was the only study that implemented an intervention, the Trauma Intervention for Affect Regulation, AIDS and Stimulant, and assessed the feasibility and acceptability of it addressing components of the SAVA syndemic model. Qualitative methods were not often used to outline the syndemic relationships with only three articles using qualitative methods, one of which uses mixed methods [8,9,10].
Table 1.
Characteristics of Included Articles (n=16)
| Characteristics | N (%) |
|---|---|
| Study Design | |
| Epidemiology | 12 (80) |
| Qualitative | 3 (18.75) |
| Intervention | 1 (6.25) |
| Site | |
| USA | 12 (75) |
| China | 1 (6.25) |
| Kazakhstan | 1 (6.25) |
| South Africa | 1 (6.25) |
| Botswana | 1 (6.25) |
| Syndemic Model | |
| Substance Abuse, Violence, and AIDS (SAVA) | 4 (25) |
| Substance Use, Mental Illness and familial Conflict non-negotiation Model (SUMIC) | 1 (6.25) |
| Unspecified | 11 (68.75) |
| Co-morbid condition with HIV | |
| Mental Health (depression, substance use, PTSD, anxiety, schizophrenia, | 15 (93.75) |
| Physical Health (high blood pressure, diabetes, arthritis) | 1 (6.25) |
Of the group of articles, 75% of them were based in the United States with the majority focusing urban centers. There were two studies done in Asia, one in China and one is Kazakhstan and two in Africa, specifically Botswana and South Africa. No studies came from South East Asia or Europe. Studies across geographic settings reported similar results and used the same syndemic framings. Diversity of study population was seen among the 16 articles in regards to gender, sexual orientation, and ethnicity. Though a couple of studies allowed for participants to be 18 and older, no study focused specifically on adolescents, whereas two studies focused elderly populations above the age of 50 [9,11]. Diversity in socioeconomic status was lacking in the group of studies, with most focusing on those in a lower socioeconomic status such as formerly incarcerated individuals, individuals who unemployed, individuals who had unstable housing, or individuals that have a year income under $20 000 [12-14].
NONCOMMUNICABLE DISEASES COMORBIDITIES AND SYNDEMIC MODELS IN CURRENT RESEARCH
Only one article looked at physical health conditions, specifically high blood pressure, diabetes, and arthritis, when looking at syndemic relationships [9]. All other studies focused on mental health disorders with substance use being the most focused upon. The temporality of what condition came first was not often mentioned with the exception of experiences of childhood trauma [7]. Specific syndemic models were not referred to in the majority of the studies. The SAVA syndemic model was refereed by four papers [8,15,16,17]. One article referred to the substance use, mental illness, and familial conflict nonnegotiation model (SUMIC) [18].
In general, the studies that looked at prevalence rates of factors that were a part of the syndemic models show trends of lower odds of viral suppression for those who have a mental health disorder. Wang et al.[19] showed an outcome for mental health disorders rather than one for HIV. They show that for people living with HIV/AIDS, the psychosocial factors in the syndemic model are associated with a magnifying effect in predicting suicidal ideation. Few studies had comparison groups, but a couple did compare relationships between the same syndemic factors for people who are living with HIV/AIDS and those who are not [19]. The longitudinal study did not show different trends than what was reported by the cross-sectional ones, thus, supporting in that instance that the syndemic trends are sustained over a year [7]. Only one study looked at an intervention and looked at the feasibility and acceptability of a three-month case management intervention. Results showed that the case management intervention results in reduced substance use and lower HIV viral loads [8]. Three studies reported qualitative findings, one was a mixed-methods study. Both of the solely qualitative were based in Africa, with one being in South Africa and one in Botswana. Findings from the South African study highlight the unique challenges that people living with HIV and a cooccurring NCD face with navigating the healthcare system. Examples of challenges were clashing appointments at different clinics and high costs of traveling to clinics far away [9]. Findings from the study in Botswana highlighted the stigma associated with mental health and HIV such as how witchcraft is often seen as the causal belief for mental illness. Of interest, most participants endorsed that it is worse to have a mental illness than HIV [10].
A RESEARCH AGENDA FOR SYNDEMICS OF HIV AND NONCOMMUNICABLE DISEASES
The current literature reveals the disconnect between syndemic theory and how studies are designed and analyzed. Below, we outline six recommendations for a research agenda to optimize the use and interpretation of syndemic models:
1. Identify the specific HIV and NCD comorbidity:
Syndemic theory assumes that there is an interaction between the two or more health conditions in the comorbidity or multimorbidity relationship. In mental health, there has been specific work on when comorbid conditions are presumed to interact versus cooccur without some mutual reinforcement or influence [20,21]. For example, depression and post-traumatic stress disorder (PTSD) suppress antiviral immune responses and increase proinflammatory responses, thus increasing susceptibility to certain types of comorbidities [22,23]. Other conditions, such as gastroesophageal reflux or plantar fasciitis, do not appear to be more common in persons with depression or PTSD compared with the general population. When studying syndemics, it is crucial that there be a hypothesized connection between health conditions that can then be studied in relation to social, economic, and geographic context influencing the relationship. A model has recently been proposed to assess syndemic interaction of inflammatory arthritis with depression via common biological pathways [6]. In the current literature on HIV and NCDs, this is not well articulated because studies lump together multiple forms of mental illness or multiple physical illnesses (hypertension, diabetes, and arthritis) into the same model, thus making it difficult to clarify pathways and processes.
2. Document the social, economic, and geographic context in the comorbidity is occurring:
It is vital to document the context in which a proposed comorbidity or multimorbidity is observed. In syndemic models, this context is what drives the association between the conditions of interest. If an association between two health conditions occurs at the same prevalence across all populations, then that is not a syndemic, that is just a common universal comorbidity. However, if the rates of occurrence vary by context, then there is something about that context that is contributing. Therefore, there needs to be clear understanding of social, cultural, political, economic, geographic, and environmental aspects of that context. For example, cultural models related to gender roles influence the likelihood of exposure to interpersonal violence and the availability of resources to mitigate that violence risk, this then contributes to differences in risk of negative reproductive health outcomes [24,25]. Some studies of HIV and NCD syndemics evaluated men who have sex with men. However, the cultural context of men who have sex with men varies considerably by setting as shaped by economics, religion, politics, culture, and numerous other factors. Therefore, the specific local social world of men who have sex with men in one community needs to understood and not assumed to be synonymous with the next community, country, or world region.
3. Propose a mechanism of action for the syndemic interaction:
A syndemic requires a proposed pathway from the social context to the interaction of two or more health conditions. There needs to be a proposed mechanism by which the proposed association occurs. Clearly articulating that association allows for appropriate study design and analysis to test the pathway. Then, that leads to being able to design syndemic care models that are most likely to be effective for prevention or intervention [4]. With HIV, the type of antiretroviral regimen and other medications influence the likelihood of comorbidities. Similarly, the availability of health services to diagnose and treat NCDs will influence the prevalence of comorbidities. Under social conditions, with high exposure to social stressors, especially loneliness and social isolation, the impact on antiviral and proinflammatory pathways contributes to if and what type of comorbidities could be present [6,22,26]. Moreover, the specific contribution for how a context influences the comorbidity needs to be outlined. Poverty can have a range of impacts on health, but the specific consequences will vary by social structure, social welfare services, and impact on exposure to other risk factors.
4. Demonstrate a context or population where the syndemic does not occur:
In the research worlds of infectious disease, cancer biology, and other health conditions, study designs are required that do not have an exposure of interest to demonstrate lower or no prevalence of the disease in the unexposed group. A similar approach is needed in syndemic research. If a particular social, economic, and geographic context is hypothesized to contribute to greater likelihood of disease comorbidity, then in a setting that lacks that particular socioeconomic-geographic profile, there should be a weaker association between the health conditions. For example, in VIDDA syndemic among Mexican immigrants, the immigrant status reduces access to healthcare and increases exposure to violence [2]. This increases the likelihood of depression, which biological and behaviorally impacts association with diabetes. Moreover, cultural issues related to misdiagnosis by healthcare workers increases the likelihood of inappropriate treatment with diabetogenic psychiatric medications [27]. In syndemic thinking, this predicts that in settings without this same constellation of social, economic, and political factors that there will not be the same association among depression and diabetes. In philosophy and logic models, this represents the idea of the counterfactual. Figure 1 illustrates this visually. In context A, we assume that some specific feature of the social, economic, and geographic context influences the specific comorbidity. But, in context B, some aspect of the social, economic, and geographic context is not present, and therefore, the influence on the comorbidity will not occur.
FIGURE 1.
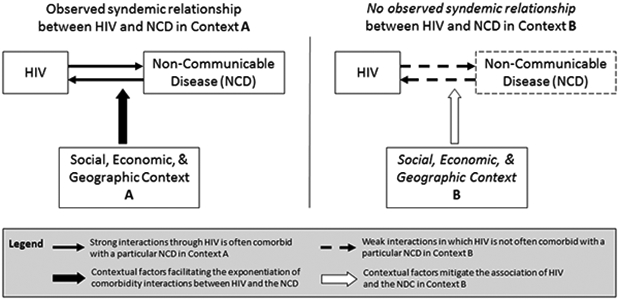
Syndemics of HIV and noncommunicable disease occur in specific social, economic, and geographical context (context A), but the comorbidities are less likely to occur in other settings and populations (context B).
5. Develop a more representative global scope of syndemic research:
The current syndemic literature on NCDs is strongly skewed to US populations. This short changes the research field because we lack other context to explore when, where, and among whom there are different HIV and NCDs comorbidity. Owing to diversity in social experience, cultural practices, healthcare availability, geographic and environmental determinants of health, and other factors, we are best able to capture potential syndemics and settings where syndemic relationships do not occur when we have a comprehensive global picture of disease associations. Populations affected by humanitarian crises, for example, bear a high burden of mortality and morbidity and often have exposure that are less prevalent in the general population. There has recently been a call for more syndemic research in humanitarian settings [28]. Refugees in Ethiopia show high rates of diabetes despite undernutrition and malnutrition in this population [5]. Given high rates of exposure to sexual violence among populations in humanitarian settings, this is an important group to evaluate potential HIV and NCD syndemics.
6. Address the breadth of possible NCDs among persons living with HIV:
One of the major limitations of the current field was that almost all studies only explored the relationship of HIV with mental illness. There is public health and clinical need to explore HIV and other NCDs. Because of the nature of HIV and the long-term impacts of the treatments, a host of NCDs could be explored. HIV and diabetes are comorbid in some populations, and this can have important social implications because of stigma associated with the conditions, as demonstrated among populations in Kenya, whereas the diabetes has not been documented to increase stigma among other populations such as those in the United States [4]. As people with HIV live longer, there is an increased burden of cancer, and cancer is known to have wide variations in prevalence across populations and settings. Therefore, it is reasonable to explore potential HIV and cancer syndemics.
CONCLUSION
Current research practices to understand comorbidity of HIV and NCDs have not optimally integrated syndemic theory to benefit prevention and intervention efforts. Most research studies employing the 'syndemic' label have documented epidemiological associations among HIV and particular NCDs (e.g., mental illness), but few have outlined the specific social, economic, and geographic factors that contribute this comorbidity. Moreover, the research studies typically fail to provide examples of different social, economic, or geographic factors where the specific comorbidity is not as prevalent. This precludes demonstrating that a syndemic interaction is at play. Because public health and clinical initiatives have different effectiveness across settings and populations, it is likely that syndemics play a large part in HIV and NCDs. Therefore, we are obligated to improve the science of syndemic research by clearly demonstrating a comorbidity, describing the socioeconomic-geographic context in which it is occurring, proposing a mechanism of interaction for the relationship, and demonstrating a different population or context where the relationship does not occur. This will ultimately open new opportunities for prevention and treatment to improve the lives of people living with HIV.
KEY POINTS.
The vast majority of recent articles looking at syndemics between HIV and noncommunicable diseases focus on mental illnesses rather than physical noncommunicable diseases.
Few studies describing an HIV and noncommunicable disease syndemic have been conducted outside the United States.
Recent studies mentioning syndemics for HIV and noncommunicable diseases often do not provide a model incorporating social, economic, and geographic factors.
Most studies of HIV and noncommunicable disease lack comparative samples and settings where the syndemic does not occur.
Most research studies are using epidemiological methods to outline syndemic relationships between HIV and noncommunicable diseases, but few employ interventions to try to reduce aspects of the syndemic relationship.
Acknowledgments
Financial support and sponsorship
No funding was involved in development of this manuscript.
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Singer M A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inquiry 1996; 24:99–110. [Google Scholar]
- 2.Mendenhall E Syndemic suffering: social distress, depression, and diabetes among Mexican immigrant women. Walnut Creek, California: Left Coast Press; 2012. [Google Scholar]
- 3.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet 2017; 389:941–950. [DOI] [PubMed] [Google Scholar]
- 4.Mendenhall E, Kohrt BA, Norris SA, et al. Noncommunicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet 2017; 389:951–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carruth L, Mendenhall E. 'Wasting away': diabetes, food insecurity, and medical insecurity in the Somali Region of Ethiopia. Soc Sci Med 2019; 228:155–163. [DOI] [PubMed] [Google Scholar]
- 6.Nikiphorou E, Lempp H, Kohrt BA. Treatment failure in inflammatory arthritis: time to think about syndemics? Rheumatology (Oxford, England) 2019; 58:1526–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harkness A, Bainter SA, O'Cleirigh C, et al. Longitudinal effects of syndemics on HIV-positive sexual minority men's sexual health behaviors. Arch Sex Behav 2019; 48:1159–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jemison D, Jackson S, Oni O, et al. Pilot randomized controlled trial of a syndemics intervention with HIV-positive, cocaine-using women. AIDS Behav 2019; 23:2467–2476.This article uses a known and previously outlined syndemic model of substance abuse, violence, and HIV/AIDS (SAVA) and tests an intervention specifically targeted to addressing this syndemic. Feasibility and acceptability of the intervention was assessed using mixed methods.
- 9.Knight L, Schatz E, Mukumbang FC. 'I attend at Vanguard and I attend here as well': barriers to accessing healthcare services among older South Africans with HIV and noncommunicable diseases. Int J Equity Health 2018; 17:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becker TD, Ho-Foster AR, Poku OB, et al. 'It's when the trees blossom': explanatory beliefs, stigma, and mental illness in the context of HIV in Botswana. Qual Health Res 2019; 29:1566–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chichetto NE, Kundu S, Freiberg MS, et al. Association of syndemic unhealthy alcohol use, cigarette use, and depression with all-cause mortality among adults living with and without HIV infection: veterans aging cohort study. Open forum infectious diseases 2019; 6:ofz188.https://doi-org.proxy.lib.duke.edu/10.1093/ofid/ofz188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yellin H, Beckwith C, Kurth A, et al. Syndemic effect of mental illness and substance use on viral suppression among recently-incarcerated, HIV-infected individuals in the CARE+ Corrections study. AIDS Care 2018; 30:1252–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Cleirigh C, Pantalone DW, Batchelder AW, et al. Co-occurring psychosocial problems predict HIV status and increased healthcare costs and utilization among sexual minority men. J Behav Medicine 2018; 41:450–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMahon JM, Braksmajer A, Zhang C, et al. Syndemic factors associated with adherence to antiretroviral therapy among HIV-positive adult heterosexual men. AIDS Res Ther 2019; 16:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thurston IB, Howell KH, Kamody RC, et al. Resilience as a moderator between syndemics and depression in mothers living with HIV. AIDS Care 2018; 30:1257–1264.This article uses a known and previously outlined syndemic model of substance abuse, violence, and HIV/AIDS (SAVA) as a basis for looking at resilience as a moderator between the outlined syndemic effects.
- 16.Jiwatram-Negron T, Michalopoulos LM, El-Bassel N. The syndemic effect of injection drug use, intimate partner violence, and HIV on mental health among drug-involved women in Kazakhstan. Glob Soc Welfare 2018; 5:71–81.This article uses a known and previously outlined syndemic model of substance abuse, violence, and HIV/AIDS (SAVA).
- 17.Anderson JC, Campbell JC, Glass NE, et al. Impact of intimate partner violence on clinic attendance, viral suppression and CD4 cell count of women living with HIV in an urban clinic setting. AIDS Care 2018; 30:399–408.This article uses a known and previously outlined syndemic model of substance abuse, violence, and HIV/AIDS (SAVA).
- 18.Maragh-Bass AC, Denison JA, Thorpe RJ Jr, Knowlton AR. The interactive effects of social support and physical functioning on HIV medical outcomes among African Americans whom inject drugs. J Ethnicity Subst Abuse 2018; 17:401–419.The article uses a previously outlined syndemic model, the SUMIC model.
- 19.Wang W, Xiao C, Yao X, et al. Psychosocial health and suicidal ideation among people living with HIV/AIDS: a cross-sectional study in Nanjing, China. PLoS ONE 2018; 13:https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0192940[Context Link] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bridges KW, Goldberg DP. Somatic presentation of DSM-III psychiatric disorders in primary care. J Psychosom Res 1985; 29:563–569. [DOI] [PubMed] [Google Scholar]
- 21.Kohrt BA, Kunz RD, Baldwin JL, et al. 'Somatization' and 'comorbidity': a study of Jhum-Jhum and depression in rural Nepal. Ethos 2005; 33:125–147. Full Text [Google Scholar]
- 22.Cole SW, Levine ME, Arevalo JM, et al. Loneliness, eudaimonia, and the human conserved transcriptional response to adversity. Psychoneuroendocrinology 2015; 62:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kohrt BA, Worthman CM, Adhikari RP, et al. Psychological resilience and the gene regulatory impact of posttraumatic stress in Nepali child soldiers. Proc Natl Acad Sci 2016; 113:8156–8161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhardwaj A, Bourey C, Rai S, et al. Interpersonal violence and suicidality among former child soldiers and war-exposed civilian children in Nepal. Global Mental Health 2018; 5:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kohrt BA, Bourey C. Culture and comorbidity: intimate partner violence as a common risk factor for maternal mental illness and reproductive health problems among former child soldiers in Nepal. Med Anthropol Q 2016; 30:515–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fredrickson BL, Grewen KM, Algoe SB, et al. Psychological well being and the human conserved transcriptional response to adversity. PLoS ONE 2015; 10:e0121839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mendenhall E Kohrt BA, Mendenhall E. The 'cost' of healthcare: poverty, depression, and diabetes among Mexican immigrants in the United States. Global mental health: anthropological perspectives anthropology and global public health. New York: Routledge; 2016. 205–220. [Google Scholar]
- 28.Kohrt BA, Mistry AS, Anand N, et al. Health research in humanitarian crises: an urgent global imperative. BMJ Global Health 2019; 4:e001870. [DOI] [PMC free article] [PubMed] [Google Scholar]


