Abstract
Background
Intensive lipid management is critical to reduce cardiovascular (CV) risk for patients with diabetes mellitus (DM).
Methods
We performed an observational study of 7,628 patients with (n=2,943) and without DM (n=4,685), enrolled in the Provider Assessment of Lipid Management (PALM) registry and treated at 140 outpatient clinics across the United States in 2015. Patient self-estimated CV risk, patient-perceived statin benefit and risk, observed statin therapy use and dosing were assessed.
Results
Patients with DM were more likely to believe that their CV risk was elevated compared with patients without DM (39.1% vs 29.3%, p<0.001). Patients with DM were more likely to receive a statin (74.2% vs 63.5%, p<0.001) but less likely to be treated with guideline-recommended statin intensity (36.5% vs 46.9%, p<0.001), driven by the low proportion (16.5%) of high risk (ASCVD risk ≥7.5%) primary prevention DM patients treated with a high intensity statin. Patients with DM treated with guideline-recommended statin intensity were more likely to believe they were at high CV risk (44.9% vs. 38.4%, p=0.005) and that statins can reduce this risk (41.1% vs. 35.6%, p=0.02), compared with patients treated with lower than guideline-recommended statin intensity. Compared with patients with an elevated HgbA1c, patients with well-controlled DM were no more likely to be on a statin (77.9% vs. 79.3%, p=0.43).
Conclusions
In this nationwide study, the majority of patients with DM were treated with lower than guideline-recommended statin intensity. Patient education and engagement may help providers improve lipid therapy for these high-risk patients.
Background
Diabetes mellitus (DM) affects 30.3 million people, or 9.4%, of the population in the United States, with increasing prevalence over time1-3. Among patients with DM, atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death with rates two to four times higher than for patients without DM4. Despite the large excess of cardiovascular (CV) disease associated with DM, prior studies have shown that a minority of patients are treated to goal levels for low density lipoprotein cholesterol (LDL-C), blood pressure and hemoglobin A1C (HbA1C)5, 6. Starting in 2013, the American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults recommended treatment with at least moderate intensity statin therapy for all patients between the age of 40 and 75 years old with DM, and consideration of high intensity statin therapy for DM patients with prior ASCVD or primary prevention patients with either 10-year ASCVD risk ≥7.5% or LDL-C ≥190 mg/dL7. Statin treatment based on risk status rather than LDL-C level was similarly recommended in the 2015 American Diabetes Association Standards of Medical Care Revisions8. The 2018 AHA/ACC guideline update more broadly recommended a high-intensity statin for patients with DM deemed to be high risk due to the presence of DM specific risk factors (previously 10-year ASCVD risk score ≥7.5%)9.
The Patient and Provider Assessment of Lipid Management (PALM) registry was a cross-sectional registry which evaluated lipid management practices across the United States in 20157. This registry allowed us to examine: 1) patient perceived CV risk and beliefs about statin therapy in those with and without DM; 2) the intensity of statin therapy use and achieved LDL-C levels in patients with and without DM; and 3) the association of diabetic glycemic control with the intensity of statin use among patients with DM.
Methods
Study Population
The PALM registry enrolled 7,938 patients treated with a statin or with CV risk factors from 140 outpatient CV, endocrinology and primary care practices across the United States. The design, rationale, inclusion, and exclusion criteria for the PALM registry have been previously published10. Patient enrollment for the PALM registry was completed between May 27, 2015 and November 12, 2015.
Chart abstractions and core laboratory lipid panels from the time of enrollment were available for 7,722 patients. We excluded patients from this analysis who had missing core lab lipid samples (n=91) or who were missing DM status (n=3), yielding a final analysis population of 7,628 patients treated at 140 practices across the United States. Among this final population of patients, 7285 (95.5%) were linked to the patient survey responses.
Data Collection and Definitions
At the time of enrollment, patients completed a survey which queried self-estimated risk of CV disease, beliefs about cholesterol lowering and its impact on CV disease risk, perceived statin benefits and risks, and knowledge of their own cholesterol levels. Additionally, patients currently on statin therapy were asked to indicate the reason(s) the statin medication was prescribed, and those who discontinued previous statin therapy were asked patient-perceived reason(s) for stopping treatment and willingness to resume statin therapy. Current statin users and those previously on statins were asked about statin-related symptoms and methods used to resolve these symptoms (if any). Survey questions are shown in Supplemental Table 1. For questions which included answer choices of “strongly disagree, disagree, neither agree or disagree, agree, strongly agree, don’t know/not sure”, responses were categorized as percent agreement, defined as responding with agree or strongly agree.
Detailed sociodemographic information was obtained from patient surveys, and medication and laboratory results, including DM treatment and most recent HbA1c levels, were extracted from the medical record. Additionally, medical diagnoses such as heart failure, chronic kidney disease, stroke, peripheral arterial disease were determined based on diagnoses documented in the medical record. On the day of enrollment, each patient underwent phlebotomy, and total cholesterol, direct LDL-C, high-density lipoprotein cholesterol and triglyceride levels were measured by LabCorp (Burlington, NC).
Patients were characterized as having DM or not based on a documented medical diagnosis at the time of enrollment. Patients with both DM1 and DM2 were included. Guideline-recommended statin treatment was defined as follows in accordance with the 2013 ACC/AHA Guideline, the guideline active at the time of PALM enrollment. A high-intensity statin was recommended for patients who met at least one of the following criteria: 1) ASCVD and patient age ≤75 years; 2) LDL-C ≥190 mg/dL; or 3) DM and patient age 40–75 years with estimated 10-year ASCVD risk ≥7.5% and LDL-C ≥70 mg/dL. At least moderate-intensity statin therapy was recommended for patients who did not meet criteria for a high-intensity statin and who met at least one of the following: 1) DM and patient age 40–75 years, with estimated 10-year ASCVD risk <7.5% and LDL-C ≥70 mg/dL or LDL-C <70 mg/dL with active statin treatment; 2) ASCVD and patient age >75 years; or 3) no DM with 10-year ASCVD risk ≥7.5% and LDL-C ≥70 mg/dL or LDL-C <70 mg/dL with active statin treatment. A history of ASCVD was defined as prior myocardial infarction (MI), coronary artery disease (CAD), coronary artery bypass grafting (CABG), prior percutaneous intervention (PCI), prior stroke, prior TIA, abdominal aortic aneurysm, peripheral arterial disease (PAD), carotid artery stenosis, and non-coronary arterial revascularization.
Statistical Analysis
Baseline characteristics, including age, sex, race, BMI, and presence of other comorbidities, of patients with DM were compared to those without DM. Rates of guideline-recommended statin therapy were compared between patients with and without DM. Patients were then stratified based on presence or absence of ASCVD. In secondary prevention patients, those with and without DM were compared based on treatment with any statin therapy and guideline-recommended statin intensity use at the time of the visit. Total cholesterol, LDL-C, high-density lipoprotein cholesterol (HDL-C) and triglyceride levels were also compared. In patients without documented ASCVD, patients were grouped first according to 10-year ASCVD risk (≥7.5% versus <7.5%). Then, a similar comparison of lipid lowering therapy and lipid testing results was completed for each group in patients with and without DM.
We then compared patient perceptions regarding CV risk, safety of statin medications and efficacy of lipid lowering therapy with statins in patients with and without DM. Patient reported rates of prior statin use and adverse symptoms during statin use were evaluated. Among patients with DM and on statins, patient perceptions of CV risk and experiences related to treatment with statin therapy were compared among those who were on at least guideline-recommended statin intensity versus those who were under treated.
Finally, among patients with DM, patients were divided into those with glycemic control (HgbA1c <7.0%) versus those without (HgbA1c ≥7.0%). We first compared statin use and lipid levels by glycemic control in all patients with DM and then based on presence or absence of ASCVD.
Categorical variables were presented using percentages among non-missing values, and continuous variables were presented using medians (25th and 75th percentiles). One patient had missing data on ASCVD history and 10-year ASCVD risk could not be calculated for 138 DM patients (4.7%) and 356 patients without DM (7.6%) due to unavailability of one or more variables needed to calculate the risk score. These patients were excluded from the respective data analyses. Pearson Chi-square test was used to compare categorical variables and Wilcoxon rank-sum test was used to compare differences in continuous variables. For each analysis, a p-value of <0.05 was considered statistically significant. All statistical analyses were performed at the Duke Clinical Research Institute using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
This study was supported by Sanofi and Regeneron Pharmaceuticals who contributed to the design of the study and interpretation of the data but were not involved in the conduct of the study, the data analysis, nor the decision to publish. All participants provided signed informed consent to participate. Each site obtained institutional review board approval for participation.
Results
Patient Characteristics
Among the final analysis population of 7,628 patients, 2,943 (38.6%) had a diagnosis of DM, including 39.7% (n=1,302 of 3,282) of patients with ASCVD and 45.2% (n=1,197 of 2,649) of primary prevention patients with 10-year ASCVD risk ≥7.5%, and 25.4% (n=306 of 1,203) of primary prevention patients with a 10-year ASCVD risk <7.5%.
Compared with those without DM, patients with DM were younger, more likely to be a non-white race, and more likely to be covered by government health insurance such as Medicare or Medicaid (Table 1). Nearly two-thirds (62.5%) of patients with DM were obese. Patients with DM were also more likely to have hypertension, a history of stroke, CABG, peripheral arterial disease and chronic kidney disease (Table 1). Among patients with DM, 907 (34.5%) were on insulin and 1170 (52.5%) were considered to have good glycemic control with hemoglobin A1c levels <7.0%.
Table 1.
Patient Characteristics
| Overall N=7628 |
Diabetes N=2943 |
No Diabetes N=4685 |
p-value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (year) | 68.0 (59.0, 75.0) | 66.0 (58.0, 73.0) | 68.0 (60.0, 75.0) | <0.001 |
| Female Gender | 47.3% | 47.1% | 47.5% | 0.77 |
| White Race | 84.8% | 78.8% | 88.6% | <0.001 |
| Insurance | ||||
| Private | 58.1% | 52.8% | 61.4% | <0.001 |
| Government | 39.6% | 44.3% | 36.7% | |
| Other | 2.3% | 2.9% | 2.0% | |
| Highest level of education | ||||
| Middle School | 7.0% | 7.2% | 6.8% | <0.001 |
| High School | 30.0% | 32.9% | 28.2% | |
| Some College | 26.9% | 28.1% | 26.2% | |
| College Graduate | 24.2% | 21.6% | 25.8% | |
| Post-Graduate Degree | 12.0% | 10.3% | 13.0% | |
| Clinic Visit Data | ||||
| Body Mass Index (kg/m2) | 29.7 (26.1, 34.3) | 32.0 (28.2, 36.9) | 28.5 (25.3, 32.6) | <0.001 |
| Obese (BMI ≥30 kg/m2) | 48.1% | 62.5% | 39.2% | <0.001 |
| SBP ≥140 mmHg or DBP ≥90 mmHg | 27.6% | 29.6% | 26.4% | 0.002 |
| Clinician Specialty* | ||||
| Cardiology | 31.8% | 25.4% | 35.9% | <0.001 |
| Endocrinology | 3.03% | 6.8% | 0.6% | |
| Primary Care | 40.1% | 44.4% | 37.4% | |
| Other | 0.7% | 0.7% | 0.7% | |
| Medical History | ||||
| Any ASCVD | 43.0% | 44.2% | 42.3% | 0.09 |
| Coronary Artery Disease | 33.1% | 33.5% | 32.8% | 0.53 |
| Stroke | 4.3% | 5.7% | 3.4% | <0.001 |
| Peripheral Arterial Disease | 6.5% | 8.3% | 5.3% | <0.001 |
| Myocardial Infarction | 12.7% | 12.5% | 12.8% | 0.69 |
| CABG | 10.1% | 12.0% | 9.0% | <0.001 |
| Heart Failure | 8.7% | 9.9% | 8.0% | 0.004 |
| Hypertension | 77.4% | 85.2% | 72.5% | <0.001 |
| Chronic Kidney Disease | 9.5% | 13.3% | 7.1% | <0.001 |
| Dialysis | 0.5% | 0.8% | 0.2% | <0.001 |
SBP: Systolic Blood pressure; DBP: Diastolic Blood pressure
CABG: Coronary Artery Bypass Grafting
Clinician specialty missing in 24.3% of all patients; 22.7% of patients with DM and 25.3% of patients without DM
Patient-Reported Beliefs
Patients with DM were more likely to believe their CV risk was higher than age and sex-matched peers (39.1% vs 29.3%, p<0.001) and to report “I often worry about having a heart attack or stroke” than patients without DM (11.6% vs 7.5%, p<0.001) (Table 4). While approximately 84% of patients in both groups agreed to the statement that “people with high cholesterol are more likely to have a heart attack or stroke,” patients with DM were less likely to report knowing the result of their last cholesterol test (69.0% vs 74.5%, p<0.001). The majority of patients with and without DM (83%) agreed that “statins are effective in reducing the risk of heart disease and stroke”; patients with DM were more likely to report concern that “statins can cause diabetes” but were similarly likely to report that “statins can cause muscle aches or pains” as patients without DM (Table 4).
Table 4.
Patient Self-Assessment of Risk and Perceptions Associated with Statin Medications
| Diabetes N=2805 |
No Diabetes N=4480 |
p-value | |
|---|---|---|---|
| My risk for having a heart attack or stroke is higher than most men/women my age | 39.1% | 29.3% | <0.001 |
| I often worry about having a heart attack or stroke | 11.6% | 7.5% | <0.001 |
| People with high cholesterol are more likely to have a heart attack or stroke | 84.0% | 84.9% | 0.37 |
| Statins are effective in reducing the risk of heart disease and stroke | 82.7% | 82.9% | 0.89 |
| Statins can cause diabetes | 16.7% | 11.1% | <0.001 |
| Statins can cause muscle aches or pains | 59.3% | 61.8% | 0.11 |
| Statins can cause liver damage | 51.5% | 55.7% | 0.01 |
| Statins can cause memory loss | 27.9% | 24.9% | 0.06 |
| Know their own last cholesterol results | 69.0% | 74.5% | <0.001 |
Patient survey responses for these questions were missing in 2.7-12.2% of patients and were excluded from this analysis
Patients who answered do not know/not sure were excluded from the following items:
- People with high cholesterol are more likely to have a heart attack or stroke: N=169 with DM and N=274 without DM
- Statins are effective: N=383 with DM and N=648 without DM
- Statins can cause diabetes: N=1037 with DM and N=2129 without DM
- Statins can cause muscle aches or pains: N=759 with DM and N=1361 without DM
- Statins can cause liver damage: N=1037 with DM and N=1736 without DM
- Statins can cause memory loss: N=1169 with DM and N=2045 without DM
Patients with DM who were not treated with a guideline-recommended statin intensity were less likely to believe they were at high CV risk and that statins can reduce CV risk than patients with DM who received guideline recommended statin intensity (Figure 1). DM patients not treated with a guideline-recommended intensity of statin therapy were also less likely to have been taking a statin medication for over 10 years, but with similar rates of reported statin side-effects when compared with DM patients who were undertreated (Figure 1).
Figure 1.
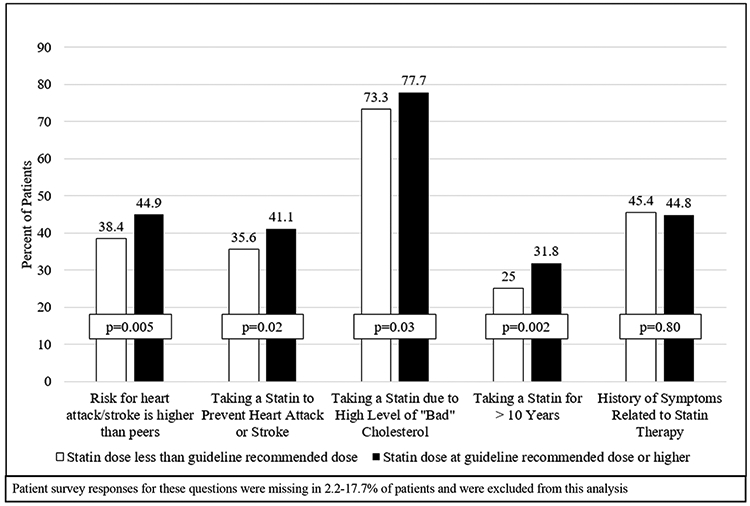
Patient Perceptions, Reported Indications, Duration and Symptoms Related to Guideline-recommended Statin Therapy
In 571 (7.8%) patients previously but no longer taking statin therapy, DM patients were less likely to report a statin side effect as a reason for stopping treatment (51.7% vs 61.2%, p=0.02). There were no differences in statin dose reduction (17.7% vs 20.1%, p=0.60) or switch to another statin (28.2% vs 35.9%, p=0.15) between patients with and without DM. The majority of patients with and without DM reported being willing to consider treatment with a statin medication again (69.2% vs 69.8%, p=0.90).
Statin Therapy and LDL-C Levels
Patients with DM were more likely to be treated with a statin (74.2% vs 63.5%, p<0.001). However, 25% of patients with DM were untreated with a statin. Among those indicated for statin therapy, patients with DM were less likely than patients without DM to be treated with guideline-recommended statin intensity (36.2% vs. 46.7%, p<0.001).
Among patients with ASCVD, patients with DM were more likely than those without DM to be treated with a statin (87.0% vs 81.5%, p<0.001), but no more likely to be treated with a guideline-recommended intensity of statin therapy (47.9% vs 46.7%, p=0.53) (Table 2). Among the 536 (16.3%) patients with ASCVD who were not treated with a statin, 49.0% reported never being offered or prescribed a statin medication before, with similar results for patients with and without DM (49.4% vs. 48.9%, p=0.06). Median LDL-C values were lower for ASCVD patients with DM (median 82.0 vs 87.0, p<0.001) than without DM but 29% of ASCVD patients with DM had levels of LDL-C ≥100 mg/dL (Table 2).
Table 2.
Statin Therapy and Lipid Levels in Patients with ASCVD
| Diabetes N=1302 |
No Diabetes N=1980 |
p-value | |
|---|---|---|---|
| Statin use | 87.0% | 81.5% | <0.001 |
| Guideline-recommended statin intensity use | 47.9% | 46.7% | 0.53 |
| Total cholesterol (mg/dL) | 154.0 (132.0, 184.0) | 160.0 (138.0, 190.0) | <0.001 |
| LDL-C (mg/dL) | 82.0 (65.0, 105.0) | 87.0 (70,0, 111.0) | <0.001 |
| Achievement of LDL-C <100 (mg/dL) | 71.0% | 63.8% | <0.001 |
| Non-HDL-C (mg/dL) | 104.0 (85.0, 134.0) | 105.0 (84.0, 133.0) | 0.90 |
| HDL-C (mg/dL) | 46.0 (38.0, 56.0) | 52.0 (44.0, 63.0) | <0.001 |
| Triglyceride (mg/dL) | 154.0 (107.0, 218.0) | 123.5 (91.0, 174.0) | <0.001 |
In primary prevention patients with DM, 70.1% were treated with a statin as compared with 57.7% of patients without DM (p<0.001). While 70.8% of patients with DM and an ASCVD risk ≥7.5% were treated with a statin, a lower proportion of these patients received guideline-recommended intensity as compared with patients without DM (16.5% vs 48.8%, p<0.001). Among patients with a 10-year ASCVD risk <7.5% and an indication for statin therapy, 58.4% of patients with DM, compared with 9.5% of patients without DM, were treated with a guideline recommended intensity of statin therapy (p<0.001, Table 3). Among the 1530 primary prevention patients who were eligible but not treated with a statin, 1128 (73.7%) reported never being offered or prescribed a statin medication, lower for patients with than without DM (65.4% vs. 77.3%, p<0.001). Primary prevention patients with DM, both with ASCVD risk ≥7.5% and <7.5% had lower median LDL-C values but higher triglyceride levels than primary prevention patients without DM (Table 3).
Table 3.
Statin Therapy and Lipid Levels in Patients without ASCVD
| 10-year ASCVD Risk ≥7.5% | 10-year ASCVD Risk <7.5% | ||||||
|---|---|---|---|---|---|---|---|
| Diabetes N=1197 |
No Diabetes N=1452 |
p-value | Diabetes N=306 |
No Diabetes N=897 |
p-value | ||
| Statin use | 70.8% | 55.0% | <0.001 | 66.3% | 63.1% | 0.31 | |
| Guideline-recommended statin intensity use* | 16.5% | 48.89 | <0.001 | 58.4% | 9.5% | <0.001 | |
| Total cholesterol (mg/dL) | 168.0 (143.0, 199.0) | 188.0 (165.0, 216.0) | <0.001 | 173.0 (148.0, 201.0) | 192.0 (169.0, 221.0) | <0.001 | |
| LDL-C (mg/dL) | 95.0 (73.0, 120.0) | 110.0 (89.0, 135.0) | <0.001 | 95.5 (75.0, 117.0) | 113.0 (91.0, 141.0) | <0.001 | |
| Non-HDL-C (mg/dL) | 117.0 (92.0, 147.0) | 128.0 (106.0, 156.0) | <0.001 | 118.0 (92.0, 142.0) | 131.0 (107.0, 162.0) | <0.001 | |
| HDL-C (mg/dL) | 49.0 (41.0, 58.0) | 56.0 (46.0, 68.5) | <0.001 | 54.0 (44.0, 65.0) | 56.0 (46.0, 69.0) | 0.01 | |
| Triglyceride (mg/dL) | 147.0 (106.0, 221.0) | 128.0 (93.0, 184.5) | <0.001 | 148.5 (103.0, 210.0) | 135.0 (96.0, 188.0) | 0.005 | |
Among patients with an indication for statin use:
N=1064 and N=1213 respectively for patients with and without DM with ASCVD 10-year risk ≥7.5%
N=296 and N=42 respectively for patients with and without DM with ASCVD 10-year risk<7.5%
Association between Glycemic Control, Statin Use, and LDL-C levels
Of the 2,943 patients with DM, 2,230 (75.8%) had a hemoglobin A1c measurement available in the electronic health record within the year prior to enrollment. Among patients with DM and known HgbA1c value, 1060 (47.5%) had uncontrolled DM with an HgbA1c ≥7%. Compared with patients with an elevated HgbA1c, patients with well-controlled DM were no more likely to be on a statin (77.9% vs. 79.3%, p=0.43), on at least moderate-intensity statin (70.0% vs. 70.9%, p=0.51), or on non-statin lipid lowering therapy (27.6% vs. 28.3%, p=0.74).
Non-statin lipid lowering therapy was frequent among both primary and secondary prevention patients with DM (22.4% and 30.8% respectively). The most common non-statin lipid lowering therapy was fish oil, which was prescribed to 12.5% of primary and 17.4% of secondary prevention patients with DM (Table 5). In patients with ASCVD and DM, there were no significant differences in statin or other lipid lowering therapy use and median LDL-C values between patients with HgbA1c ≥7% vs. <7%. Among primary prevention patients with DM, those with HgbA1c ≥7% had higher LDL-C cholesterol (median 96.5 vs. 90.0 mg/dL, p=0.02) and triglyceride levels (median 156.0 vs. 142.0 mg/dL, p =0.003) compared with patients with well controlled DM (Table 5).
Table 5.
Lipid-lowering Therapy and Lipid Levels in Patients with Diabetes based on HgbA1c Level
| ASCVD | No ASCVD | ||||||
|---|---|---|---|---|---|---|---|
| A1c ≥7.0% (n=457) |
A1c <7.0% (n=537) |
p-value | A1c ≥7.0% (n=560) |
A1c <7.0% (n=577) |
p-value | ||
| Statin use | 89.7% | 86.0% | 0.08 | 70.9% | 71.2% | 0.90 | |
| Guideline-recommended statin intensity use* | 48.0% | 47.2% | 0.80 | 28.0% | 25.2% | 0.30 | |
| Non-statin lipid lowering therapy use** | 31.9% | 32.6% | 0.82 | 25.1% | 23.8% | 0.61 | |
| Total Cholesterol (mg/dL) | 155.0 (132.0, 185.0) | 151.0 (131.0, 177.0) | 0.05 | 169.0 (145.0, 200.0) | 167.0 (141.0, 196.0) | 0.06 | |
| LDL-C (mg/dL) | 82.0 (64.0, 107.0) | 80.0 (64.0, 99.0) | 0.24 | 96.5 (75.0, 120.0) | 90.0 (71.0, 116.0) | 0.02 | |
| HDL-C (mg/dL) | 44.0 (37.0, 52.0) | 48.0 (39.0, 58.0) | <0.001 | 48.0 (40.0, 58.5) | 51.0 (43.0, 61.0) | 0.003 | |
| Triglyceride (mg/dL) | 173.0 (122.0, 238.0) | 137.0 (96.0, 192.0) | <0.001 | 156.0 (109.0, 237.5) | 142.0 (103.0, 200.0) | 0.003 | |
Among patients with an indication for statin use:
N=452 and N=536 for patients with ASCVD and A1C ≥7.0% and <7.0% respectively
N=511 and N=517 for patients without ASCVD and A1C ≥7.0% and <7.0% respectively
non-statin lipid lowering therapy included Ezetimibe, Fibrate, Niacin, Bile Acid sequestrants, fish oil / Omega-3, red yeast rice extract
Discussion
The PALM registry uniquely captured patient-estimated CV risk, statin treatment perceptions, statin therapy use, and LDL-C levels for a diverse population of primary and secondary prevention patients. We found that: 1) patients with DM were more likely to report concern regarding statin treatment risks but were not observed to report more statin-related side effects than patients without DM; 2) patients with DM not on a guideline-recommended intensity of statin therapy were less likely to believe themselves to be at higher CV risk and to believe in the clinical benefits of statin therapy; 3) patients with DM were more likely to be treated with a statin medication, but less than half of patients with DM were treated with a guideline-recommended statin intensity; and 4) glycemic control did not correlate with intensity of statin treatment.
Patients with DM represent a group at heightened risk for the development of CV disease, future CV events and death from a CV cause. LDL-C remains an important CV risk factor for patients with DM with data showing a 1.57-fold increase in the risk for coronary artery disease for every 39 mg/dL increase in LDL-C11. A meta-analysis of statin trials shows that statin therapy reduces CV risk by about 22% per 39 mg/dl reduction in LDL-C in both DM and non-DM patients12, and that high intensity statin therapy reduced CV risk more than moderate intensity statin therapy. Thus, the guidelines reflect this excess risk and the importance of LDL-C reduction. Both the 2013 and the 2018 ACC/AHA guidelines recommend that all patients with DM receive at least moderate intensity statin therapy and a high intensity statin for those at the highest risk (prior ASCVD, 10-year risk ≥7.5% per the 2013 guideline, or multiple ASCVD risk factors per the 2018 guideline)7, 9. Similarly, the 2017 American Association of Clinical Endocrinologists placed patients with DM and ASCVD into the “extreme risk” category and patients with primary prevention DM into the “very high risk” category, with a recommendation for treatment goals of LDL-C <55 mg/dL and LDL-C <70 mg/dL respectively13.
In alignment with the medical literature, patients with DM in our study assessed themselves to be at higher risk than their peers for CV events. Despite the higher objective and patient self-assessed risk for CV events, we found that over 25% of patients DM were not treated with any statin. Among those treated with a statin, there was a substantial under-treatment, with only 36.2% of DM patients treated at guideline recommended intensities. This was frequently due to treatment with lower intensity statin therapy in scenarios where a patient met a guideline indication for high intensity statin use. Less than half of patients with DM and ASCVD and a small minority (16.5%) of patients with DM and 10-year ASCVD risk of ≥ 7.5% received a high intensity statin in alignment with guideline recommendations. Less than two-thirds of patients with DM and a 10-year ASCVD risk of <7.5% were treated with at least moderate intensity statin therapy. Additionally, among all patients with DM, treatment with guideline recommended statin intensity was less likely as compared with patients without DM. Prior work has shown similar gaps in the treatment of this high-risk group of patients. A recent analysis of trends in statin use among a large group of patients included in the four recommended treatment groups by the 2013 ACC/AHA cholesterol guidelines revealed that while the use of statins increased from 2009 to 2015, only approximately one third of primary prevention patients with DM and ASCVD risk ≥7.5% were treated with a high intensity statin and two-thirds of patients with DM and ASCVD risk <7.5% were treated with at least a moderate intensity statin.14 Other studies have similarly shown low proportions of patients with DM treated in accordance to guideline recommended statin therapy.15-17
Statin intolerance is commonly cited as a reason for statin under treatment. However, we observed that the majority of untreated DM patients reported never being offered or prescribed a statin previously. The self-reported patient data likely represents several layers of potential improvement – not only in clinician prescribing but also in areas of communication between a patient and clinician regarding the use or non-use of statin therapy. Both these scenarios, however, indicate that clinicians may play a key role in the lack of guideline-adherent care. We also found that patients with DM were more likely to report concerns regarding statin safety; but only a minority of patients stopped statin therapy due to side effects, and the frequency of side effects did not differ between patients with and without DM. While prior symptoms can also influence a patient’s willingness to re-attempt statin therapy, in our study, the majority of patients indicated for but not currently treated with a statin were willing to consider statin therapy again in the future. Together, these findings further highlight the importance of shared clinician and patient decision making with personalized education regarding the benefit to risk ratio of statin therapy being key to these discussions.
We hypothesized that glycemic control amongst patients with DM might correlate with greater adherence to evidence-based care, including prescription of guideline recommended statin intensity. However, we observed no difference in treatment with statin therapy among patients with well-controlled versus poorly controlled DM. While the gaps in statin therapy do not appear to be any more pronounced in those patients with HgbA1C ≥7%, we did find that patients with well-controlled DM (HgbA1C <7%) had more favorable lipid profiles in general. Patients with well-controlled DM had lower triglyceride levels and higher HDL-C among both primary and secondary prevention populations as well as lower LDL-C levels in primary prevention patients. Given no difference in overall treatment with statin therapy, this improved overall lipid profile may be a marker of general health and management of comorbidities.
Statin under treatment may be explained by either or both patient and clinician factors. Prior work from the PALM registry showed that clinician beliefs regarding the benefits and risks associated with statin therapy were associated with guideline adherent statin treatment of patients as well as achieved LDL-C levels.18 By examining patient reported responses in this study, we found that there were significant differences in the self-perceptions and beliefs of patients with DM who did or did not receive guideline recommended intensities of statin treatment. Patients who received guideline-recommended statin intensities rated themselves at higher risk for CV events and were more likely to report that the reason they were taking a statin was to reduce this risk than patients who received less than guideline recommended statin intensity or no statin. Prior work has similarly shown these gaps in the application of guideline recommendations for the treatment of blood lipid levels among patients with DM. Interventions have largely focused on the clinician aspect of statin prescribing. However, our study suggests that understanding how clinicians may more effectively engage patients in the discussion of individual CV risk and statin therapy use is also critical to increase guideline-compliant care of these high-risk patients. Further work across levels of care, from patient and clinician focused to broad system-level interventions, is likely necessary to improve this engagement and the guideline-recommended lipid treatment for patients with DM.
Limitations
We acknowledge several limitations associated with our study. First, given the cross-sectional nature of our study, we were unable to assess trends in the treatment of blood lipid levels over time or determine the causality or directionality of the observed associations. We used the most recent available HgbA1C value from chart review. As these values can vary over time, the single value may not fully reflect the overall glycemic control for each patient. For patients on a statin at the time of their study visit, core lab LDL-C values were reflective of this treatment and ASCVD risk was calculated using blood lipid levels while on statin therapy. Given that calculation of ASCVD risk while on statin therapy will decrease the 10-year risk, it is probable that some of the patients with active statin treatment and ASCVD risk of <7.5% may have had an ASCVD risk ≥7.5% prior to the initiation of statin therapy. Further, guideline-recommended treatment with a statin was based on definitions from the 2013 ACC/AHA guideline. While 74.2% of clinicians from the PALM registry reported use of the ACC/AHA guideline as their primary tool for lipid management19, use of other guideline recommendations may have contributed to some of the treatment results we observed. Additionally, there are minor differences in determining high intensity statin treatment for primary prevention patients with DM between the ACC/AHA 2013 and 2018 guidelines. Given that this analysis was completed using data collected in 2015, we utilized the active recommendation at that time. Finally, given the observational nature of our study, clinician rationale for lipid management, including shared-decision making discussions between patients and clinicians, was not available.
Conclusions
In the PALM registry, we found ongoing large gaps in the use of statins among patients with and without DM. Despite objective and patient-reported assessment of higher risk, patients with DM were less likely to receive guideline-recommended statin intensities as compared with patients without DM, driven primarily by under treatment of high-risk primary prevention DM patients. Those patients with DM treated with a guideline-recommended statin intensity were more likely to believe they were at high CV risk and that statins can reduce CV risk than under-treated patients. These insights may form the basis of both clinician and patient-facing interventions to optimize guideline-directed treatment of these high-risk patients.
Supplementary Material
Acknowledgments
Sources of Funding
This study was supported by Sanofi and Regeneron Pharmaceuticals who contributed to the design of the study and interpretation of the data but were not involved in the conduct of the study, the data analysis, nor the decision to publish.
Conflict of Interest Disclosures
A Lowenstern: Dr. Lowenstern reports funding through NIH T-32 training grant #5 T32 HL069749–14.
S Li: Ms. Li reports no relevant disclosures.
SS Virani: Dr. Virani reports research support from ADA/AHA/ VA; honorarium from ACC as the Associate Editor for Innovations, ACC.org.
AM Navar: Dr. Navar is supported by the NIH, NHLBI K01HL133416–01 and reports research support from Amgen, Sanofi, and Regeneron; consulting fees from Amgen and Sanofi.
Z Li: Dr. Li reports no relevant disclosures
JG Robinson: Dr. Robinson reports research support from Amarin, Amgen, Astra-Zeneca, Eli Lilly, Esai, Glaxo-Smith Kline, Merck, Pfizer, Regeneron/Sanofi, Takeda; consultant for Amgen, Eli Lilly, Merck, Pfizer, Regeneron/Sanofi.
VL Roger: Dr. Roger reports no relevant disclosures.
AC Goldberg: Dr. Goldberg reports research support from Amarin, Amgen, Pfizer, Merck, Regeneron/Sanofi, IONIS, Genzyme/Isis, and Regeneron, Madrigal, and Arisaph; consulting for Optum Rx, Regeneron/Sanofi, and Esperion; honorarium for editorial work Merck Manual.
A Koren: Dr. Koren reports employment with Sanofi.
MJ Louie: Dr. Louie reports employment with Regeneron Pharmaceuticals, Inc.; ownership interest in Regeneron Pharmaceuticals, Inc.
ED Peterson: Dr. Peterson reports research support from Eli Lilly, Janssen, Merck; Consulting from AstraZeneca, Bayer, Boehringer Ingelheim, Genentech, Janssen, Merck, and Sanofi Aventis.
TY Wang: Dr. Wang reports research support from AstraZeneca, Daiichi Sankyo, Eli Lilly, Gilead, Glaxo SmithKline, Regeneron, Sanofi; consultant/advisory/education from Bristol Myers Squibb, Astra Zeneca, Eli Lilly, Premier, Inc.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2017. [Google Scholar]
- 2.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS and Gregg EW. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29:1263–8. [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS and Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–200. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Council on E, Prevention Statistics C and Stroke Statistics S. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 5.Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF and Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36:2271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong ND, Patao C, Wong K, Malik S, Franklin SS and Iloeje U. Trends in control of cardiovascular risk factors among US adults with type 2 diabetes from 1999 to 2010: comparison by prevalent cardiovascular disease status. Diab Vasc Dis Res. 2013;10:505–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr., Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr., Tomaselli GF and American College of Cardiology/American Heart Association Task Force on Practice G. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–45. [DOI] [PubMed] [Google Scholar]
- 8.Standards of medical care in diabetes−-2015: summary of revisions. Diabetes Care. 2015;38 Suppl:S4. [DOI] [PubMed] [Google Scholar]
- 9.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr., Sperling L, Virani SS and Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2018:CIR0000000000000625. [Google Scholar]
- 10.Navar AM, Wang TY, Goldberg AC, Robinson JG, Roger VL, Wilson PF, Virani SS, Elassal J, Lee LV, Webb LE and Peterson E. Design and rationale for the Patient and Provider Assessment of Lipid Management (PALM) registry. American heart journal. 2015;170:865–71. [DOI] [PubMed] [Google Scholar]
- 11.Turner RC, Millns H, Neil HA, Stratton IM, Manley SE, Matthews DR and Holman RR. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ. 1998;316:823–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cholesterol Treatment Trialists C, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J and Collins R. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jellinger PS, Smith DA, Mehta AE, Ganda O, Handelsman Y, Rodbard HW, Shepherd MD, Seibel JA, Dyslipidemia ATFfMo and Prevention of A. American Association of Clinical Endocrinologists’ Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis: executive summary. Endocr Pract. 2012;18:269–93. [DOI] [PubMed] [Google Scholar]
- 14.Harrison TN, Scott RD, Cheetham TC, Chang SC, Hsu JY, Wei R, Ling Grant DS, Boklage SH, Romo-LeTourneau V and Reynolds K. Trends in Statin Use 2009–2015 in a Large Integrated Health System: Pre- and Post-2013 ACC/AHA Guideline on Treatment of Blood Cholesterol. Cardiovasc Drugs Ther. 2018;32:397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pokharel Y, Gosch K, Nambi V, Chan PS, Kosiborod M, Oetgen WJ, Spertus JA, Ballantyne CM, Petersen LA and Virani SS. Practice-Level Variation in Statin Use Among Patients With Diabetes: Insights From the PINNACLE Registry. J Am Coll Cardiol. 2016;68:1368–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gu A, Kamat S and Argulian E. Trends and disparities in statin use and low-density lipoprotein cholesterol levels among US patients with diabetes, 1999–2014. Diabetes Res Clin Pract. 2018;139:1–10. [DOI] [PubMed] [Google Scholar]
- 17.Chamberlain AM, Cohen SS, Killian JM, Monda KL, Weston SA and Okerson T. Lipid-Lowering Prescription Patterns in Patients With Diabetes Mellitus or Cardiovascular Disease. Am J Cardiol. 2019;124:995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowenstern A, Navar AM, Li S, Virani SS, Goldberg AC, Louie MJ, Lee LV, Peterson ED and Wang TY. Association of Clinician Knowledge and Statin Beliefs With Statin Therapy Use and Lipid Levels (A Survey of US Practice in the PALM Registry). Am J Cardiol. 2019;123:1011–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lowenstern A, Li S, Navar AM, Virani S, Lee LV, Louie MJ, Peterson ED and Wang TY. Does clinician-reported lipid guideline adoption translate to guideline-adherent care? An evaluation of the Patient and Provider Assessment of Lipid Management (PALM) registry. American heart journal. 2018;200:118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


