Abstract
Objectives
To determine the effect of a free smartphone application (TCPRLink) that provides real-time monitoring and audiovisual feedback on chest compressions (CC) on trained layperson telephone-assisted cardiopulmonary resuscitation (T-CPR) performance.
Design
A manikin-based randomised controlled study.
Setting
This study was conducted at a multidisciplinary university and a community centre in China.
Participants
One hundred and eighty-six adult participants (age 18–65 years) with T-CPR training experience were randomly assigned to the TCPRLink (n=94) and T-CPR (n=92) groups with age stratification.
Interventions
We compared the participants’ performance for 6 min of CC in a simulated T-CPR scenario both at the baseline and after 3 months.
Primary and secondary outcome measures
The primary outcomes were the CC rate and proportion of adequate CC rate (100–120 min−1). The secondary outcomes included the proportion of participants counting the CC rhythm, time to first CC, CC depth, hands-off time and CC full-release ratio.
Results
Participants in the TCPRLink feedback group more consistently performed CC with higher rate, both initially and 3 months later (median 111 (IQR 109–113) vs 108 (103–112) min−1, p=0.002 and 111 (109–113) vs 108 (105–112) min−1, p<0.001, respectively), with less need to count the rhythm (21.3% vs 41.3%, p=0.003% and 7% vs 22.6%, p=0.004, respectively) compared with the T-CPR group. There were no significant differences in time to the first CC, hands-off time or CC full-release ratio. Among 55–65 year group, the CC depth was deeper in the TCPRLink group than in the TCPR group (47.1±9.6 vs 38.5±8.7 mm, p=0.001 and 44.7±10.1 vs 39.3±10.8 mm, p=0.07, respectively).
Conclusions
The TCPRLink application improved T-CPR quality in trained laypersons to provide more effective CCs and lighten the load of counting out the CC with the dispatcher in a simulated T-CPR scenario. Further investigations are required to confirm this effectiveness in real-life resuscitation attempts.
Keywords: accident & emergency medicine, public health, telemedicine
Strengths and limitations of this study.
The effectiveness of a real-time feedback smartphone application (TCPRLink) was evaluated in a telephone-assisted cardiopulmonary resuscitation (T-CPR) simulation among participants from the Chinese general population.
Trained adult laypersons (age range 18–65 years) participated in this study to facilitate the identification of discrepancies in T-CPR performance among different age groups.
The study included a 3-month follow-up T-CPR performance test to investigate the participants’ skill retention.
The Hawthorn effect could not be excluded in the simulation scenario, with the possibility of a motivation bias.
Introduction
Bystander-provided immediate and adequate cardiopulmonary resuscitation (CPR) can directly impact patient outcomes following an out-of-hospital cardiac arrest.1–3 The updated guidelines of the American Heart Association (AHA) and European Resuscitation Council (ERC) state that telephone-assisted CPR (T-CPR) has a positive effect on the entire resuscitation process by getting more callers to start CPR and through coaching the callers to provide effective CPR.4 5 Despite significant advances in the T-CPR instructions during the resuscitation procedures, here exists a blind zone between the dispatcher and caller. The dispatcher is voice connected to the caller via the phone, but is unable to see the patient and evaluate the quality of bystander CPR. Therefore, new strategies to address this challenge are needed.
The ubiquitous presence and utilisation of smartphones suggest a novel opportunity to improve resuscitation care through the measurement of bystander CPR metrics.6–12 In a recent statement from the AHA and ERC, the use of digital strategies, such as mobile devices, was encouraged to provide bystanders with an accelerometer to measure CPR metrics.13 14 In adherence to these guidelines, an audiovisual smartphone application (TCPRLink) was developed to facilitate high-quality bystander-provided CPR and assist the dispatcher to evaluate the CPR quality in real time.15 The TCPRLink application utilises the smartphone front camera to detect chest compressions (CC) and displays the CC rate to the bystanders and simultaneously sends the real-time CC rate and the time without compressions via the internet to a monitor that is in front of the dispatcher.
This study was conducted to evaluate the effectiveness of the TCPRLink application with real-time audiovisual feedback in dispatcher-assisted CPR during a cardiac arrest simulation. We hypothesised that this smartphone-based CC rate feedback application would improve the quality of CPR in the general population compared with the use of conventional T-CPR instructions.
Methods
Study design and ethics
This study was a simulation-based randomised experimental trial that was carried out from 1 September 2018 to 30 May 2019. All participants were verbally informed about the purpose of the study and provided written informed consent. They were informed that their T-CPR performance would be tested and video-recorded in a simulated scenario after training and, again, 3 months later.
Study population
We randomly recruited 186 participants from those who participated in the ‘WeCan CPR’ training programme16 an initiative of the China Resuscitation Academy. College students and adult laypersons (age range 18–65 years) who had completed the training programme within 1 week were eligible for study enrolment. Physicians, nurses, dispatchers and other healthcare professionals were excluded from the study.
The WeCan CPR course is a video-based, 1-hour training programme on applying dispatcher-telephone-guided CPR training in combination with practical and basic CPR training that is targeted at potential bystanders. Participants learn how to call the emergency dispatch centre, follow the procedure of the T-CPR instructions and perform hands-only CPR. All trainees performed at least 550 CC on instrumented feedback manikins (QCPR Classroom, Laerdal Medical, Norway) during the training.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting or dissemination of our research.
Randomisation
Randomisation was stratified by age groups (18–24, 25–54 and 55–65 years) and conducted to ensure equal distribution of participants across study arms. Participants were randomised into either the control arm (conventional T-CPR group) or interventional arm (T-CPR with the TCPRLink group). All participants were informed the purpose of the study, which was to assess the impact of the TCPRLink App on resuscitation performance, and were not blinded to the study-arm allocation due to the nature of the intervention.
TCPRLink application
TCPRLink (University of Stavanger and Laerdal Medical, Norway) is a free, CPR audiovisual feedback smartphone application that was designed to measure the CC rate and hands-off time and to provide feedback to the bystander and the dispatcher. The accuracy and validation of the TCPRLink app has been demonstrated earlier.17
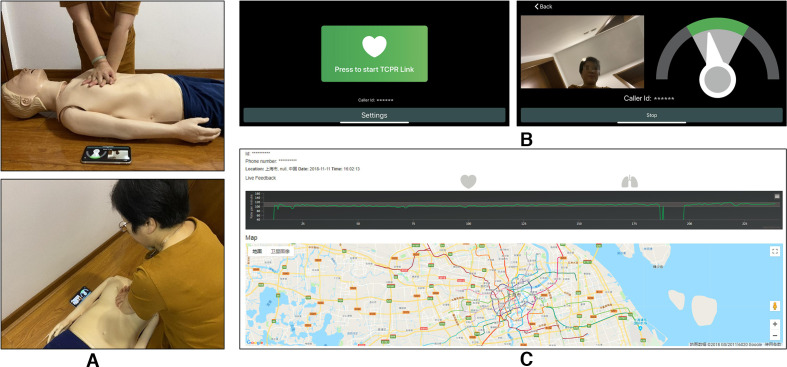
The illustration of the application in use is presented in figure 1. By clicking the ‘Press to start TCPR Link’ button, the application activates the speaker, establishes a telephone connection with the dispatcher, activates the TCPRLink app which captures and analyses the CPR movement via the front facing camera of the smartphone in real time, and simultaneously sends the location and real-time compression data to a web server which is available for the dispatcher (web server: http://tcprlink.azurewebsites.net/?_country=china).
Figure 1.
The illustration of TCPRLink application in use. (A) Illustration photo of TCPRLink in use in a simulated T-CPR situation. (B) Screenshots of TCPRLink. Front page to the left and bystander feedback example to the right. (C) Screenshot of the web server available for the dispatcher. T-CPR, telephone-assisted cardiopulmonary resuscitation.
At the bystander interface, a speedometer displayed on the smartphone screen next to a preview frame allows the bystander to keep track of the CC rate, which is obtained by analysing body movement. Thus, the individual receives real-time objective feedback via the speedometer (with the indicator in the green or yellow range of 100–120 and <100 or >120 compressions/min, respectively).
Similarly, at the dispatcher’s interface, real-time objective feedback is presented during the emergency call via a sliding window from a website presented on a computer screen that shows the history and progression of the CC rate. Guided by the indicator on web server, the dispatcher can further guide the bystander-rendered CC rate through direct instructions to ‘push faster’, ‘push slower’ or ‘don’t stop’.
Study procedures
The T-CPR performance of all participants was evaluated twice. The first evaluation (phase I test) was conducted within 1 week of WeCanCPR training in a cardiac arrest T-CPR simulated scenario, and the second occurred 3 months later (phase II test) and corresponded to the same setting as the initial test.
The simulations were performed in a quiet, isolated, designated room with a manikin placed on the floor. Individuals were asked to enter the room alone, make an emergency call to an assigned phone number and try their best to rescue the manikin in a cardiac arrest T-CPR simulated scenario. T-CPR instructions were strictly standardised using the Medical Priority Dispatch System (MPDS V.12.1, Salt Lake City, USA) out-of-hospital cardiac arrest (OHCA) dispatch protocol.18 One dispatcher who had 6 years of T-CPR experience from working at the local emergency dispatch centre acted as dispatcher in the simulation.
During T-CPR calls, individuals were asked for their current address, patient’s age and gender, patient’s consciousness level and breathing status in accordance with the MPDS protocol. Then, individuals were instructed by the dispatcher to activate the speaker and place their phone on the floor by the manikin. The dispatcher followed a standard procedure to initiate CPR and let the participant perform hands-only CPR for 6 min. For encouragement, the dispatcher counted the CC rhythm with the participants and said ‘good job, push harder’ every 30 s during the simulation.
For the conventional T-CPR group, the participants received no visual feedback from the smartphone and were guided only by the dispatcher instructions. For the TCPRLink group, individuals were asked to call for help using the TCPRLink app. The participants’ behaviour and performance during the simulation exercise were recorded by a separate video camera that faced towards the manikin and was located 80 cm above the ground and 1.5 m away for a panoramic shot.
Outcome measures
The primary outcomes measured were the CC rate and the proportion of the adequate CC meeting the guideline-recommended rate (100–120 min−1)19 20 during 6 min of hands-only CPR. The secondary outcomes were CC depth, the proportion of CC with the adequate CC depth (5–6 cm), the proportion of CC with complete recoil (complete release recoil of the chest between compressions) and the absolute hands-off time (the sum of all periods during which there was no hand compression of the chest) during the 6 min of hands-only CC. The abovementioned parameters of CCs effectiveness were monitored using the proprietary software for the ResusciAnne QCPR manikin (Laerdal Medical, Norway).
The video recording of the simulation scenario was used to evaluate individual participant behaviours, including the communication with the dispatcher (counting the CC rhythms with the dispatcher) and time to first CC (time interval from call connection to first CC). We documented the age, sex, education level, self-reported body weight and height of all participants.
Sample size estimation
The sample size calculation was followed to sequentially recruit 68 participants (34 in the TCPRLink group with 12, 11 and 11 participants in the 18–24, 25–54 and 55–65 years age range, respectively, and 34 in the T-CPR group with 11, 12 and 11 participants in the 18–24, 25–54 and 55–65 years age range, respectively) in the phase I test. A change in the proportion of adequate CC by >5% was considered to be a relevant difference. With a statistical power of 90% and two-sided alpha level of 0.05, the minimum numbers of participants required in the TCPRLink/T-CPR group among the different age groups were 20 (18–24 years), 26 (25–54 years) and 18 (55–65 years), respectively. Considering the possibility of 20% loss to follow-up and the participants’ availability, we recruited 54, 75 and 57 participants in the age ranges of 18–24, 25–54 and 55–65 years, respectively.
Statistical analysis
Data are presented as frequencies with percentages for categorical variables and mean±SD or median (IQR; M (P25−P75)) for continuous variables. Normal distribution was confirmed using the Kolmogorov–Smirnov test. Intergroup differences in the outcomes for the categorical variables were assessed using the χ2 or Fisher’s exact test. Independent Student’s t-tests were conducted to explore the effect of the intervention for continuous variables with normal distribution and Mann–Whitney U-test was used for variables with non-parametric distribution between the control and intervention arm. All analyses were conducted using SPSS V.22.0. All p-values were two-sided, and p<0.05 was considered to be statistically significant.
Results
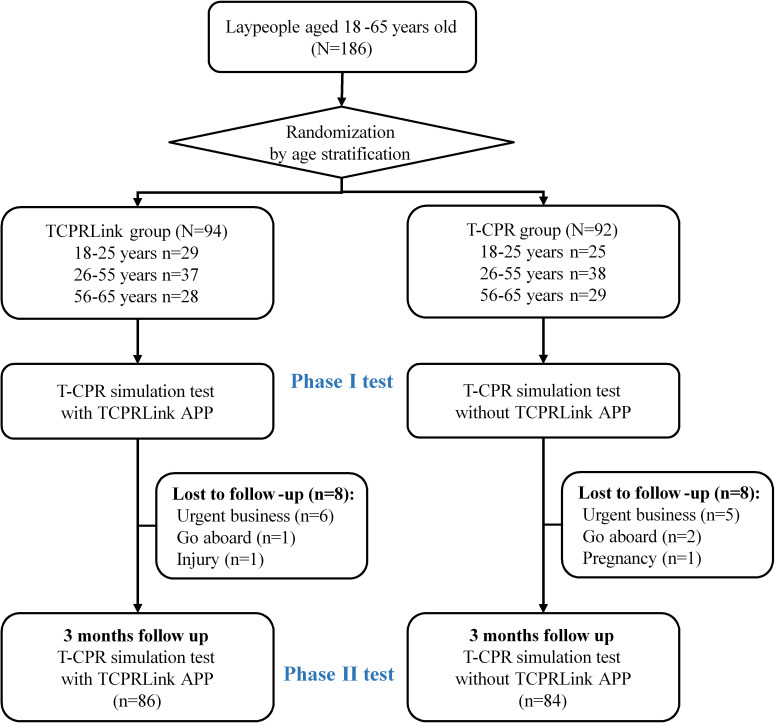
A total of 186 participants (94 in T-CPR with TCPRLink group and 92 in conventional T-CPR group) were included in this study. The demographic characteristics are shown in table 1. Age, gender, education level and body mass index did not differ between the groups. Eight participants in each study arm were lost to follow-up after the initial test (figure 2).
Table 1.
Demographic characteristics of the participants
| Total (n=186) |
TCPRLink group (n=94) |
T-CPR group (n=92) |
|
| Male (n, %) | 83 (44.6) | 42 (44.7) | 41 (44.6) |
| Age, years | |||
| 18–24 | 54 (27.0) | 29 (30.9) | 25 (27.2) |
| 25–54 | 75 (37.5) | 37 (39.4) | 38 (41.3) |
| 55–65 | 57 (28.5) | 28 (29.8) | 29 (31.5) |
| Education status (n, %) | |||
| ≤High school/junior college | 68 (36.6) | 30 (31.9) | 38 (41.3) |
| College | 75 (40.3) | 44 (46.8) | 31 (33.7) |
| Masters and PhD | 43 (23.1) | 20 (21.3) | 23 (25.0) |
| Height, m, mean±SD | 1.68±0.1 | 1.67±0.1 | 1.68±0.1 |
| Weight, kg, mean±SD | 64.5±11.4 | 63.3±10.3 | 65.6±12.4 |
| BMI, kg/m2, mean±SD | 22.9±3.1 | 22.7±2.8 | 23.0±3.4 |
BMI, body mass index; T-CPR, telephone-assisted cardiopulmonary resuscitation.
Figure 2.
Flow diagram of the participants. T-CPR, telephone-assisted cardiopulmonary resuscitation.
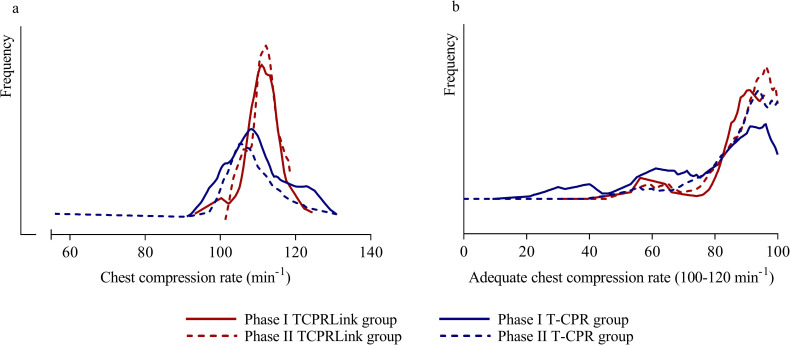
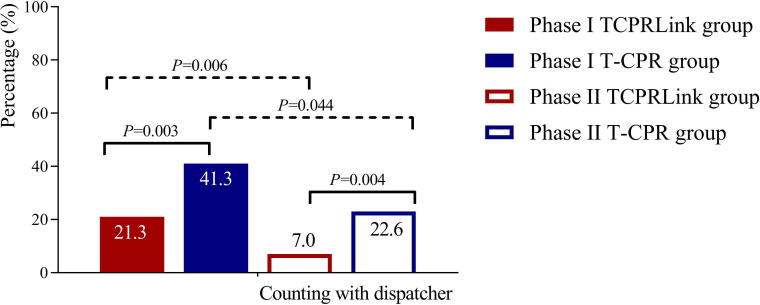
During the 6 min of hands-only CPR, individuals in the TCPRLink group performed CC with a higher rate, both initially (median 111 (IQR 109–113) vs 108 (103–112) min−1, p=0.002) and at the 3-month retest (111 (109–113) vs 108 (105–112) min−1, p<0.001), compared with the conventional T-CPR group, respectively (table 2 and figure 3). In the TCPRLink group where the CC rate speedometer was displayed, individuals were less likely to count out the CC rhythms with the dispatcher (21.3% vs 41.3%, p=0.003% and 7% vs 22.6%, p=0.004, respectively) (table 2 and figure 4). Hands-off times, CC full-release ratio and time to first CC did not statistically differ between the study groups either initially or at 3 months follow-up.
Table 2.
Participants’ CPR performance assessment in the T-CPR simulation scenario
| T-CPR performance | Phase I (n=186) | Phase II (n=170) | ||||
| TCPRLink group (n=94) |
T-CPR group (n=92) |
P-value | TCPRLink group (n=86) |
T-CPR group (n=84) |
P-value | |
| Counting with the dispatcher (n, %) | 20 (21.3) | 38 (41.3) | 0.003 | 6 (7.0) | 19 (22.6) | 0.004 |
| Time from call connected to: (seconds, mean±SD) | ||||||
| Cardiac arrest identification | 98.2±12.8 | 99.1±16.9 | 0.68 | 101.7±13.0 | 104.2±15.0 | 0.25 |
| First chest compression | 143.6±17.8 | 140.0±25.8 | 0.27 | 149.7±16.6 | 146.0±20.2 | 0.19 |
| CPR parameters (M (P25−P75) or mean±SD) | ||||||
| Total number of compressions | 661 (643–674) | 648 (615–674) | 0.035 | 661 (644–675) | 646 (630–667) | 0.002 |
| Average compression rate (min−1) | 111 (109–113) | 108 (103–112) | 0.002 | 111 (109–113) | 108 (105–112) | <0.001 |
| Percentage of adequate rate (100–120 min−1, %) | 96 (89–98) | 82 (50–97) | <0.001 | 95 (78–98) | 93 (67–97) | 0.11 |
| Average compression depth (mm) | 45.4±8.8 | 43.6±8.8 | 0.17 | 43.9±9.1 | 42.9±11.5 | 0.59 |
| Percentage of adequate depth (50–60 mm, %) | 20 (3–74) | 12 (0–51) | 0.14 | 17 (4–54) | 13 (0–57) | 0.26 |
| Percentage of fully released (%) | 97 (72–100) | 97 (69–100) | 0.79 | 95 (54–100) | 96 (51–100) | 0.40 |
| Average hands-off time (s) | 0 (0–1) | 0 (0–1) | 0.24 | 0 (0–1) | 0 (0–1) | 0.72 |
Phase I tests were cardiopulmonary resuscitation (CPR) performance and capabilities assessment using the telephone-assisted CPR (T-CPR) simulation scenario among individuals who have undergone CPR training with/without the TCPRLink application.
Phase II tests were CPR skill retention assessments among individuals with/without TCPRLink application after 3 months.
T-CPR, telephone-assisted cardiopulmonary resuscitation.
Figure 3.
Distribution of the chest compression rate and the proportion of the adequate chest compression rate (100–120 min−1) in TCPRLink group and T-CPR group. Phase I test was conducted in T-CPR trained individuals with/without TCPRLink App after inclusion. Phase II test was conducted in the same individuals with/without TCPRLink App after 3 months. T-CPR, telephone-assisted cardiopulmonary resuscitation.
Figure 4.
Counting with dispatcher in TCPRLink group and T-CPR group. Phase I test was conducted in T-CPR trained individuals with/without TCPRLink App after inclusion. Phase II test was conducted in the same individuals with/without TCPRLink App after 3 months. T-CPR, telephone-assisted cardiopulmonary resuscitation.
The depth of CCs in the TCPRLink group was significantly deeper in the age group of 55–65 years (47.1±9.6 vs. 38.5±8.7 mm, p=0.001) than in the control group in the phase I test (table 3). However, the CC depth showed a tendency to be deeper in TCPRLink group but the difference was not statistically significant in the phase II test conducted 3 months later (44.7±10.1 vs 39.3±10.8 mm, p=0.07; table 4).
Table 3.
Age-stratified comparison of the participants’ CPR performance in the TCPRLink and T-CPR groups (phase I)
| TCPR performance | Age 18–24 years | Age 25–54 years | Age 55–65 years | ||||||
| TCPRLink group (n=29) |
T-CPR group (n=25) |
P value | TCPRLink group (n=37) |
T-CPR group (n=38) |
P value | TCPRLink group (n=28) |
T-CPR group (n=29) |
P value | |
| Counting with the dispatcher (n, %) | 9 (31.0) | 12 (48.0) | 0.20 | 7 (18.9) | 19 (50.0) | 0.005 | 4 (14.3) | 7 (4.1) | 0.35 |
| Time from call connection to: (s, mean±SD) | |||||||||
| Cardiac arrest identification | 98.9±13.5 | 96.4±19.5 | 0.58 | 97.0±13.2 | 98.2±14.0 | 0.72 | 98.9±12.0 | 102.7±17.8 | 0.36 |
| First chest compression | 141.4±20.2 | 137.8±26.8 | 0.57 | 143.6±17.7 | 135.9±26.9 | 0.14 | 145.8±15.4 | 147.1±22.5 | 0.79 |
| CPR parameters (M (P25−P75) or mean±SD) | |||||||||
| Total number of compression | 663 (640–671) | 650 (608–666) | 0.21 | 659 (653–677) | 652 (632–674) | 0.29 | 659 (640–676) | 640 (612–672) | 0.14 |
| Average compression rate (min−1) | 111 (108–113) | 108 (101–112) | 0.03 | 111 (109–114) | 109 (106–113) | 0.12 | 110 (107–113) | 107 (103–113) | 0.06 |
| Percentage of adequate rate (100–120 min−1, %) | 95 (88–99) | 82 (50–96) | 0.01 | 97 (90–98) | 89 (51–97) | 0.006 | 95 (88–97) | 71 (48–95) | 0.003 |
| Average compression depth (mm) | 41.8±7.8 | 43.1±6.6 | 0.49 | 46.9±8.2 | 47.8±8.1 | 0.67 | 47.1±9.6 | 38.5±8.7 | 0.001 |
| Percentage of adequate depth (50–60 mm, %) | 8 (0–28) | 12 (4–33) | 0.37 | 25 (9–84) | 37 (7–86) | 0.92 | 45 (1–99) | 1 (0–14) | 0.002 |
| Percentage of fully released (%) | 100 (95–100) | 100 (96–100) | 0.66 | 98 (79–100) | 95 (57–99) | 0.24 | 71 (5–100) | 96 (37–100) | 0.13 |
| Average hands-off time (s) | 0 (0–2) | 0 (0–1) | 0.24 | 0 (0–1) | 0 (0–0) | 0.45 | 0 (0–1) | 0 (0–1) | 0.92 |
Phase I tests were conducted for the evaluation of CPR performance and capabilities assessment using a telephone-assisted CPR (T-CPR) simulation scenario among individuals who have undergone CPR training with/without the TCPRLink application.
Table 4.
Age-stratified comparison of the participants’ CPR performance between the TCPRLink and T-CPR groups (phase II)
| TCPR performance | Age 18–24 years | Age 25–54 years | Age 55–65 years | ||||||
| TCPRLink group (n=29) |
T-CPR group (n=23) |
P value | TCPRLink group (n=31) |
T-CPR group (n=34) |
P value | TCPRLink group (n=26) |
T-CPR group (n=27) |
P value | |
| Counting with the dispatcher (n, %) | 2 (6.9) | 4 (17.4) | 0.40 | 4 (12.9) | 12 (35.3) | 0.036 | 0 (0) | 3 (11.1) | 0.24 |
| Time from call connected to: (seconds, mean±SD) | |||||||||
| Cardiac arrest identification | 99.8±16.0 | 100.4±16.3 | 0.89 | 103.8±13.6 | 103.0±11.9 | 0.82 | 101.4±7.3 | 108.9±16.7 | 0.04 |
| First chest compression | 148.4±20.1 | 144.2±25.5 | 0.52 | 153.2±17.3 | 143.6±13.9 | 0.018 | 146.8±9.8 | 150.4±21.9 | 0.45 |
| CPR parameters (M (P25−P75) or mean±SD) | |||||||||
| Total number of compressions | 658 (643–678) |
639 (605–653) |
0.004 | 665 (653–675) | 648 (640–668) | 0.09 | 663 (644–676) | 643 (627–680) | 0.32 |
| Average compression rate (min−1) | 111 (109–113) |
107 (101–110) | <0.001 | 112 (109–113) | 109 (107–112) | 0.06 | 111 (107–114) | 109 (105–114) | 0.28 |
| Percentage of adequate rate (100–120 min−1, %) | 96 (82–99) | 82 (60–98) |
0.08 | 95 (78–98) |
95 (84–97) | 0.64 | 92 (77–98) | 90 (70–97) | 0.61 |
| Average compression depth (mm) | 41.7±8.2 | 43.7±14.1 | 0.55 | 45.2±9.0 | 45.4±9.6 | 0.92 | 44.7±10.1 | 39.3±10.8 | 0.07 |
| Percentage of adequate depth (50–60 mm, %) | 10 (2–32) | 10 (0–54) | 0.92 | 19 (7–55) | 22 (2–81) | 0.97 | 19 (3–68) | 2 (0–24) | 0.04 |
| Percentage of fully released compressions (%) | 100 (92–100) | 99 (91–100) | 0.52 | 93 (15–100) | 90 (44–99) | 0.65 | 68 (33–100) | 89 (24–99) | 0.84 |
| Average hands-off time (s) | 0 (0–2) | 0 (0–1) | 0.16 | 0 (0–1) | 0 (0–1) | 0.48 | 0 (0–0) | 0 (0–0) | 0.89 |
Phase II tests were conducted for the evaluation of CPR performance and capabilities assessment using telephone-assisted CPR (T-CPR) simulation scenario among individuals who have received CPR training with/without a TCPRLink application at 3 months after the training.
T-CPR, telephone-assisted cardiopulmonary resuscitation.
Discussion
This study evaluated a novel, digital invention that integrated an audiovisual feedback smartphone application and a web-based system, thereby combining real-time dispatcher instructions and real-time feedback to ensure the appropriate quality of CPR. We compared the quality of T-CPR performed by potential bystander-rescuers in the age range of 18–65 years in a cardiac arrest simulation scenario with or without the smartphone application. The results of this study showed that real-time, audiovisual feedback using a smartphone application and web-based system in combination with dispatcher instructions augmented the interaction between dispatchers and bystanders with a resultant positive effect on the quality of bystander-rendered CPR.
Dispatchers may coach callers to perform CPR, although they rely on audio communication alone to understand what is happening. With no other means of feedback, depending on the dispatcher’s instructions may lead to lower quality CC and more hands-off time.21 Several experimental manikin studies have demonstrated the potential benefits and drawbacks of video-assisted communication between rescuers and dispatchers compared with that of the conventional audio-instructed practice with regard to the CC rate and hand position.22–26 In a recent study that compared the real-world effects of video-instructed or audio-instructed T-CPR on the resuscitation outcomes, video-instructed T-CPR caused no delay in initiating CC although it was not associated with improvement in the survival rates.27
In dispatch-assisted instructions, the smartphone has secured a role as a promising carrier to improve video resuscitation care with its wide availability and high communication capabilities. Several diversified, advanced smartphone applications have been developed for integration into the links of the chain of survival and have feasibly created a strengthened ‘Mobile chain of survival’28 as shown previously. One kind of application guides users in their CPR procedures via text and pictures or provides video examples of CPR with metronomic guidance that a bystander could watch before or during an actual resuscitation.6 8 Another application provides measurement of CPR quality and feedback based on motion-sensing which require the user to place the phone on the patient’s chest or hold it between the rescuer’s hands while performing CPR.9–12 However, these previous smartphone solutions have neglected the potential to leverage the dispatcher’s involvement and, therefore, may be less suitable for real-life emergencies as the phone connection may be accidentally lost when using the phone as a CPR feedback device.
Given its salient differences with regard to the other smartphone applications, the TCPRLink application could improve the effectiveness of T-CPR, both on the dispatcher instruction and bystander operation aspects. The TCPRLink application uses the smartphone front facing camera for continuous quality improvement through real-time feedback for the bystander and the dispatcher. Dispatcher could monitor the hands-off time and encourage the bystander to continue CPR when they experience fatigue. Therefore, this application may be suitable for real-world emergencies when considering the prolonged time to call the dispatch centre and start CC, and that phone connection may be accidentally lost wmhen using the phone as a CPR feedback device.10
As the risk of OHCA increases with age,29 30 older adults are more likely to be bystanders when their spouse or a family member experiences a cardiac arrest. The CPR capability of older adults has always been a significant concern. Another study that evaluated the effectiveness of a smartphone CPR application showed that participants aged over 60 years could not sustain long-duration CPR.9 However, in contrast with the results of that study, our study showed that TCPR Link app used with dispatcher assistance caused extra stimulus among seniors aged 55–65 as indicated by the subgroup analysis, with comparable quality of CPR with that of the younger participants during the 6 min of hands-only CPR. Moreover, providing a feasible CPR feedback devices for seniors might be an appropriate approach to increase both their ability and also their willingness and confidence to do CPR.9 When guided by the TCPRLink application, the CC rate and depth of CPR performed by older participants were both better and in adherence to the guidelines when compared with that in the conventional T-CPR group. These data suggest that, with the two-way metric of CPR quality and dispatcher encouragement, older participants performed CPR equally well as did the younger generation.
Counting aloud is the the most common method by which the dispatcher can ensure an appropriate CC rate in T-CPR. Without feedback from the rescuer, the dispatcher’s understanding of the rescuer’s situation is poor.31 Interestingly, we found that visual guidance of the CC rate from the speedometer on the smartphone reduced the need to count the number of CC aloud to maintain an appropriate rate. Thus, rescuers could expend more energy on compression and less on counting. Furthermore, a lesser need for counting in the dispatcher’s protocol leaves more time to coach for compression depth and avoiding leaning. Contrary to the common concern that the use of mobile devices or smartphone applications to improve CPR quality might cause a delay in the initiation of CCs,8 10 the time to the first CC in the TCPRLink group was not prolonged as compared with that in the conventional T-CPR group in this study.
Nevertheless, some limitations of this study need to be mentioned. On the one hand, this study was implemented in a simulated environment which may not reflect the real-world scenario. The Hawthorn effect could not be excluded under the simulation scenario, and could result in a motivation bias. Therefore, this study followed a realistic approach to the simulation of bystander CPR in a cardiac arrest scenario. We invited a senior dispatcher who worked in the emergency dispatch centre to portray the T-CPR scenario. On the other hand, a manikin may not represent the diversity of patients’ chests and the changes in chest resistance during extended CPR. Finally, we recruited voluntary participants aged between 18 and 65 years who attended the ‘WeCan CPR’ training project. Therefore, the participants of this study might have had a selection bias as they had a positive willingness and knowledge of CPR training. We found that elderly individuals older than 65 years were less likely to participate, considering their physical capacity. The mean age of participants was nearly 40 years, which might not be the representative age for bystanders in real life.
Conclusions
The TCPRLink smartphone application provides real-time feedback to both rescuer and dispatcher to enable more effective CC and lighten the load of counting out the CC with the dispatcher in a simulated T-CPR scenario. Further investigations are required to confirm the effectiveness of this application in the real-life resuscitation scenario.
Supplementary Material
Acknowledgments
We would like to acknowledge the participants from Shanghai Jiao Tong University and the Chaoyang community for their time and active involvement in this study.
Footnotes
XD and LZ contributed equally.
Contributors: LZ conceptualised the study. XD and LZ performed the data collection and analysis. XD and LZ contributed to manuscript writing. LZ, HM, TSB and Z-JZ provided administrative advice and consultation. HM, TSB and Z-JZ critically revised the final version. All authors approved the final version of the manuscript.
Funding: This research was funded by the National Natural Science Foundation of China (Grant No. 81703303); Shanghai Municipal Government Pujiang Research Development Program (Grant No. 17PJC070); HeartRescue Project China Program; and Innovative Research Team of High-level Local Universities in Shanghai.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: All of the authors declare that they have no potential or actual conflicts of interest. HM and TSB are employees at Laerdal Medical. The manufacturer (Laerdal Medical, Norway) does not have any conflicts of interest with regard to the trial or in the interpretation of the results.
Patient consent for publication: Not required.
Ethics approval: The study protocol was approved by the Joint Research Ethics Board of the Shanghai Jiao Tong University Schools of Public Health and Nursing (approval ID SJUPN-201714).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. Kern KB, Hilwig RW, Berg RA, et al. . Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation 2002;105:645–9. 10.1161/hc0502.102963 [DOI] [PubMed] [Google Scholar]
- 2. Steen S, Liao Q, Pierre L, et al. . The critical importance of minimal delay between chest compressions and subsequent defibrillation: a haemodynamic explanation. Resuscitation 2003;58:249–58. 10.1016/S0300-9572(03)00265-X [DOI] [PubMed] [Google Scholar]
- 3. Meaney PA, Bobrow BJ, Mancini ME, et al. . Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation 2013;128:417–35. 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed] [Google Scholar]
- 4. Panchal AR, Berg KM, Cabañas JG, et al. . 2019 American heart association focused update on systems of care: Dispatcher-Assisted cardiopulmonary resuscitation and cardiac arrest centers: an update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2019;140:e895–903. 10.1161/CIR.0000000000000733 [DOI] [PubMed] [Google Scholar]
- 5. Perkins GD, Handley AJ, Koster RW, et al. . European resuscitation Council guidelines for resuscitation 2015: section 2. Adult basic life support and automated external defibrillation. Resuscitation 2015;95:81–99. 10.1016/j.resuscitation.2015.07.015 [DOI] [PubMed] [Google Scholar]
- 6. Semeraro F, Taggi F, Tammaro G, et al. . iCPR: a new application of high-quality cardiopulmonary resuscitation training. Resuscitation 2011;82:436–41. 10.1016/j.resuscitation.2010.11.023 [DOI] [PubMed] [Google Scholar]
- 7. Zapletal B, Greif R, Stumpf D, et al. . Comparing three CPR feedback devices and standard BLS in a single rescuer scenario: a randomised simulation study. Resuscitation 2014;85:560–6. 10.1016/j.resuscitation.2013.10.028 [DOI] [PubMed] [Google Scholar]
- 8. Sakai T, Kitamura T, Nishiyama C, et al. . Cardiopulmonary resuscitation support application on a smartphone - randomized controlled trial. Circ J 2015;79:1052–7. 10.1253/circj.CJ-14-1258 [DOI] [PubMed] [Google Scholar]
- 9. Plata C, Stolz M, Warnecke T, et al. . Using a smartphone application (PocketCPR) to determine CPR quality in a bystander CPR scenario - A manikin trial. Resuscitation 2019;137:87–93. 10.1016/j.resuscitation.2019.01.039 [DOI] [PubMed] [Google Scholar]
- 10. Paal P, Pircher I, Baur T, et al. . Mobile phone-assisted basic life support augmented with a metronome. J Emerg Med 2012;43:472–7. 10.1016/j.jemermed.2011.09.011 [DOI] [PubMed] [Google Scholar]
- 11. Eaton G, Renshaw J, Gregory P, et al. . Can the British heart Foundation PocketCPR application improve the performance of chest compressions during bystander resuscitation: a randomised crossover manikin study. Health Informatics J 2018;24:14–23. 10.1177/1460458216652645 [DOI] [PubMed] [Google Scholar]
- 12. Kovic I, Lulic I, Lulic D. A new method of investigating the Ergonomics of visual cardiopulmonary resuscitation (CPR) feedback delivery. Resuscitation 2012;83:e191–2. 10.1016/j.resuscitation.2012.05.023 [DOI] [PubMed] [Google Scholar]
- 13. Perkins GD, Handley AJ, Koster RW, et al. . European resuscitation Council guidelines for resuscitation 2015: section 2. adult basic life support and automated external defibrillation. Resuscitation 2015;95:81–99. 10.1016/j.resuscitation.2015.07.015 [DOI] [PubMed] [Google Scholar]
- 14. Kleinman ME, Goldberger ZD, Rea T, et al. . 2017 American heart association focused update on adult basic life support and cardiopulmonary resuscitation quality: an update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2018;137:e7–13. 10.1161/CIR.0000000000000539 [DOI] [PubMed] [Google Scholar]
- 15. Meinich-Bache Øyvind, Engan K, Birkenes TS, et al. . Real-Time chest compression quality measurements by smartphone camera. J Healthc Eng 2018;2018:6241856–56. 10.1155/2018/6241856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The WeCan CPR training program in China. Available: https://www.globalresuscitationalliance.org/wp-content/uploads/2019/12/China_Community_Training.pdf2019 [Accessed 1 May 2020].
- 17. Meinich-Bache Øyvind, Engan K, Birkenes TS, et al. . Real-Time chest compression quality measurements by smartphone camera. J Healthc Eng 2018;2018:6241856–12. 10.1155/2018/6241856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medical Priority Dispatch System (version 12.1.3) Salt Lake City, Utah, USA: 2008. [Google Scholar]
- 19. Monsieurs KG, Nolan JP, Bossaert LL, et al. . European resuscitation Council guidelines for resuscitation 2015: section 1. executive summary. Resuscitation 2015;95:1–80. 10.1016/j.resuscitation.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 20. Neumar RW, Shuster M, Callaway CW, et al. . Part 1: Executive summary: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132:S315–67. 10.1161/CIR.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 21. Birkenes TS, Myklebust H, Neset A, et al. . Quality of CPR performed by trained bystanders with optimized pre-arrival instructions. Resuscitation 2014;85:124–30. 10.1016/j.resuscitation.2013.09.015 [DOI] [PubMed] [Google Scholar]
- 22. Lin Y-Y, Chiang W-C, Hsieh M-J, et al. . Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation 2018;123:77–85. 10.1016/j.resuscitation.2017.12.010 [DOI] [PubMed] [Google Scholar]
- 23. Lee JS, Jeon WC, Ahn JH, et al. . The effect of a cellular-phone video demonstration to improve the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation as compared with audio coaching. Resuscitation 2011;82:64–8. 10.1016/j.resuscitation.2010.09.467 [DOI] [PubMed] [Google Scholar]
- 24. Stipulante S, Delfosse A-S, Donneau A-F, et al. . Interactive videoconferencing versus audio telephone calls for dispatcher-assisted cardiopulmonary resuscitation using the ALERT algorithm: a randomized trial. Eur J Emerg Med 2016;23:418–24. 10.1097/MEJ.0000000000000338 [DOI] [PubMed] [Google Scholar]
- 25. Bolle SR, Scholl J, Gilbert M. Can video mobile phones improve CPR quality when used for dispatcher assistance during simulated cardiac arrest? Acta Anaesthesiol Scand 2009;53:116–20. 10.1111/j.1399-6576.2008.01779.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Johnsen E, Bolle SR. To see or not to SEE—Better dispatcher-assisted CPR with video-calls? A qualitative study based on simulated trials. Resuscitation 2008;78:320–6. 10.1016/j.resuscitation.2008.04.024 [DOI] [PubMed] [Google Scholar]
- 27. Lee SY, Song KJ, Shin SD, et al. . Comparison of the effects of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation on resuscitation outcomes after out-of-hospital cardiac arrest. Resuscitation 2020;147:12–20. 10.1016/j.resuscitation.2019.12.004 [DOI] [PubMed] [Google Scholar]
- 28. Kovic I, Lulic I. Mobile phone in the chain of survival. Resuscitation 2011;82:776–9. 10.1016/j.resuscitation.2011.02.014 [DOI] [PubMed] [Google Scholar]
- 29. Sasson C, Rogers MAM, Dahl J, et al. . Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63–81. 10.1161/CIRCOUTCOMES.109.889576 [DOI] [PubMed] [Google Scholar]
- 30. Wissenberg M, Lippert FK, Folke F, et al. . Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 2013;310:1377–84. 10.1001/jama.2013.278483 [DOI] [PubMed] [Google Scholar]
- 31. Johnsen E, Bolle SR. To see or not to see--better dispatcher-assisted CPR with video-calls? A qualitative study based on simulated trials. Resuscitation 2008;78:320–6. 10.1016/j.resuscitation.2008.04.024 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.