Hospitals have made substantial investments in advertising for cancer services in recent years, totaling over $200 million in 2016 alone.1,2 Advertisements promoting cancer centers are unavoidable in the U.S. They hang on highway billboards and air during prime-time programming. Some advertisements claim superior outcomes, others highlight access to clinical trials, and many present heartwarming patient stories that may be non-representative.3 Data suggest that patients are highly aware of advertisements and likewise influenced by them.4 Decades of research demonstrate wide and consistent variations in cancer care outcomes between U.S. hospitals.5,6 While patients might wish to select their cancer provider based on objective measures of cancer care quality and outcomes,7,8 few measures are publicly available. Advertising is designed to improve cancer center recognition and attract patients in an increasingly competitive environment. It has the potential to provide valuable information about screening and treatment options, and it may benefit patients by attracting them to hospitals with the best outcomes. However, if hospital advertising for cancer services is not correlated with patient outcomes, information shared through advertising may mislead patients and generate inaccurate expectations of treatment benefit.9
We conducted an analysis to evaluate whether advertising spending for a hospital’s cancer services was associated with long-term survival outcomes of the patients with cancer treated in those centers. For the measures of advertising spending and long-term survival, we applied methods that have been described previously.9,10 We captured hospital advertising spending for cancer services in 2014 across 6 different U.S. media outlets (television, magazines, radio, newspapers, billboards, and the Internet), using data from the media-monitoring agency Kantar Media (New York, New York).9 Medicare Fee-for-Service (FFS) 100% Research Identifiable Files were used to determine hospital risk-adjusted five-year mortality ratios, including cases from 2011–12.10 We included the top 50 hospitals (or sets of hospitals) in terms of their advertising spending, accounting for over 89% of the 173 million dollars spent on cancer center advertising in 2014.
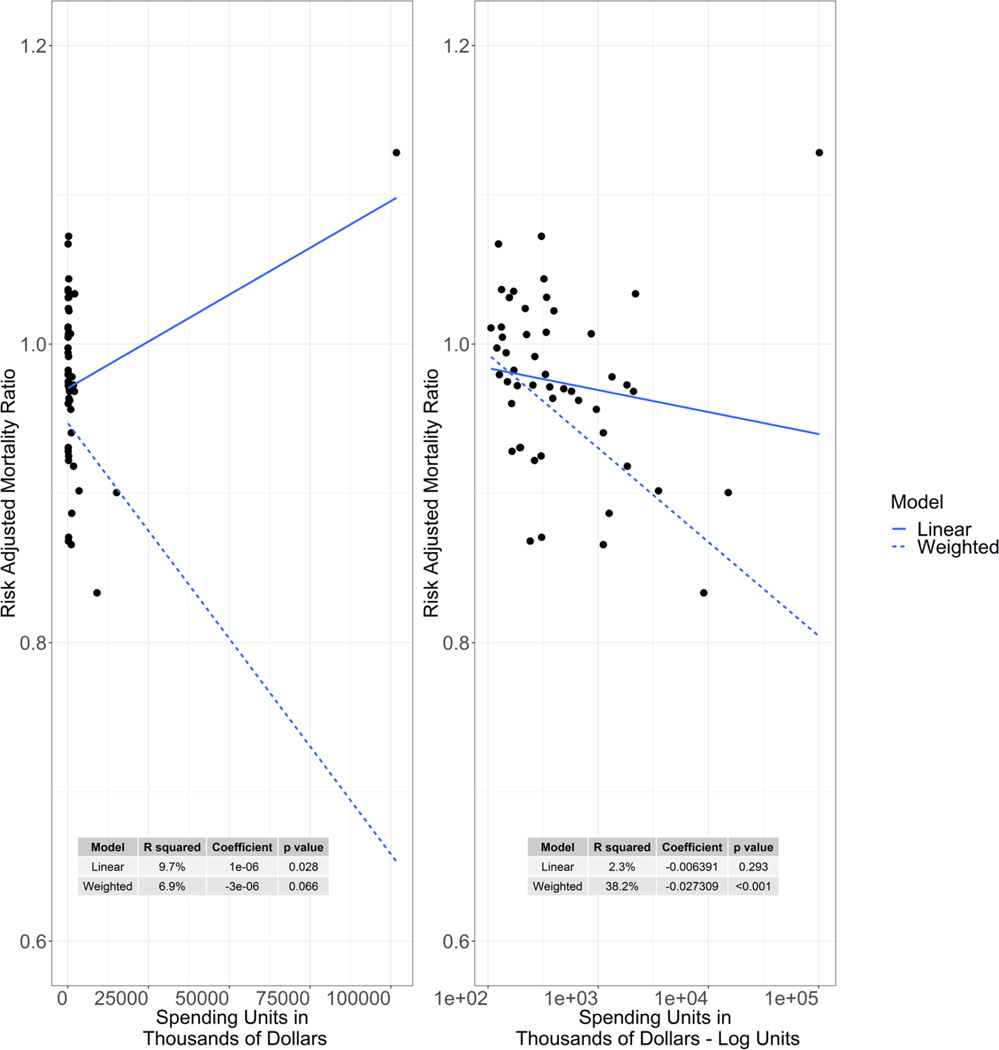
The primary test of association was a linear regression, with advertising spending as the predictor. The outcome was a risk-adjusted mortality ratio which was determined by dividing the observed number of deaths by an expected number. In brief, the 3M Clinical Risk Group (CRG) risk adjustment model in combination with adjustments for age and median income level of the zip code of residence serve to adjust for differences in patient severity and population demographics. A risk-adjusted mortality ratio below one indicates that a hospital performed better than expected, where a ratio greater than one means a hospital had higher mortality than what was expected. The R-squared from the regression model was used to see how well advertising spending explained outcomes. We conducted additional analyses that included a log transformation of the x variable (i.e., spending) and weighting of the outcome (y) variable (i.e., risk- adjusted five-year mortality) by the volume of patients at the hospital. In total, there were four models used to assess the relationship between advertising spending and risk-adjusted mortality. This study was deemed exempt research by the institutional review board of Memorial Sloan Kettering Cancer Center. The Centers for Medicare & Medicaid Services and Kantar Media granted data use approvals. Additional methodological details can be found in Appendix A.
For the top 50 hospital advertisers, the median number of FFS Medicare cancer patients treated was 764 (range: 93 to 5,945). Spending for advertising promoting cancer services was unevenly distributed across hospitals (Figure). Median spending was $305,900. The 50th hospital spent $106,300, the average hospital spent $3,064,600, and the top advertising spender, Cancer Treatment Centers of America, spent more than the other 49 hospitals combined, totaling $101,740,900. Five-year hospital risk-adjusted mortality ratio for patients with cancer ranged from 0·83 to 1·13, meaning hospitals’ mortality ratio ranged from 17% (0·83) below expected to 13% (1·13) higher than expected. Results between the four models were fairly inconsistent. Some of the models found a positive relation between advertising spending and survival outcomes; other models found a negative relation. For two of the four models, this relationship was not statistically significant. None of the models had an R2 greater than 38%, indicating that hospital advertising did not account for the majority of the variability in hospital survival outcomes. Figure 1 shows the full explanation of the model results. A list of all hospitals with spending, volume, and survival outcomes is available in the Appendix.
Figure.
Scatterplots of hospitals’ advertising spending for cancer services in 2014, compared to risk-adjusted five-year mortality for FFS Medicare beneficiaries beginning treatment in 2011–12
We found little evidence that the cancer centers to which people were most likely to be exposed through advertisements were the cancer centers with the best patient outcomes. There was considerable variation in both advertising spending and survival outcomes among the top 50 hospital advertisers. Some hospitals in our sample with excellent outcomes did not have particularly high advertising spending, and the highest-spending set of hospitals – operating as Cancer Treatment Centers of America – had notably poorer patient outcomes than the average in our sample. Patients might be inadvertently pursuing treatment choices that do not align with their intentions or preferences by assuming that advertising across national media is indicative of high-quality cancer treatment. Over the past decade, cancer centers have markedly increased the amount of consumer-directed advertising spending. Assuming current trends continue, cancer center advertising is likely to constitute a major source of patient information that may influence decisions about where cancer patients seek treatment. This would be a good thing for patients if advertising was predictive of better patient outcomes. However, our findings suggest that the relation is inconsistent and not particularly strong, with many outliers.
Some limitations should be considered when interpreting these findings. For long-term survival, we only included FFS Medicare beneficiaries, and the generalizability of this outcome to other patients is unknown. Advertising spending totals did not include spending for social media, which has been widely adopted by U.S. hospitals as a means to support hospitals’ reputations and attract patients. We also did not have data available on the content of cancer center advertisements, and were thus unable to distinguish between advertisements promoting specific cancer therapies and advertisements promoting general cancer center reputations. Our analysis was limited to cancer center advertising in the U.S., but the U.S. has the highest health care spending in the world and in recent decades there has been marked growth in spending for health care advertising.1
Hospital advertising for cancer services continues to increase in the U.S., and patients have more options for where to seek cancer care. However, cancer care quality remains uneven. Our findings suggest that cancer care advertising is not reliably valuable for patients as a surrogate of cancer care quality. The lack of correlation underscores the need for publicly available objective data on cancer centers’ patient outcomes and other measures of quality that can be easily accessed and interpreted by patients to aid in decision making. Patients, clinicians, and other stakeholders should view cancer center advertisements with scrutiny.
Supplementary Material
ACKNOWLEDGEMENTS
Funding source: P30 CA 008748 from the National Institutes of Health Core to Memorial Sloan Kettering Cancer Center
Footnotes
Disclosures:
ALS, LV, MC, DL, DMR, ED, and YS report no disclosures.
PBB reports: reports grants from Kaiser Permanente, grants from Laura and John Arnold Foundation, grants from NIH Core Grant P30 CA 008748, during the conduct of the study; personal fees from American Society for Health-System Pharmacists, personal fees from Gilead Pharmaceuticals, personal fees from WebMD, personal fees from Goldman Sachs, personal fees from Defined Health, personal fees from Vizient, personal fees from Anthem, personal fees from Excellus Health Plan, personal fees from Hematology Oncology Pharmacy Assoc, personal fees from Novartis Pharmaceuticals, personal fees from Janssen Pharmaceuticals, personal fees from Third Rock Ventures, personal fees from JMP Securities, personal fees from Genentech, personal fees from Mercer, personal fees from United Rheumatology, personal fees from Morgan Stanley, consulting fees from Foundation Medicine, consulting fees from Grail, outside the submitted work.
REFERENCES
- 1.Schwartz LM, Woloshin S. Medical marketing in the united states, 1997–2016. JAMA 2019; 321(1): 80–96. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal E. Ask Your Doctor if This Ad Is Right for You. The New York Times. 2016 February 28, 2016. [Google Scholar]
- 3.Vater LB, Donohue JM, Arnold R, White DB, Chu E, Schenker Y. What are cancer centers advertising to the public?: a content analysis. Ann Intern Med 2014; 160(12): 813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abel GA, Burstein HJ, Hevelone ND, Weeks JC. Cancer-Related Direct-to-Consumer Advertising: Awareness, Perceptions, and Reported Impact Among Patients Undergoing Active Cancer Treatment. Journal of Clinical Oncology 2009; 27(25): 4182–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA 1998; 280(20): 1747–51. [DOI] [PubMed] [Google Scholar]
- 6.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002; 346(15): 1128–37. [DOI] [PubMed] [Google Scholar]
- 7.Yang A, Chimonas S, Bach PB, Taylor DJ, Lipitz-Snyderman A. Critical Choices: What Information Do Patients Want When Selecting a Hospital for Cancer Surgery? Journal of oncology practice / American Society of Clinical Oncology 2018; 14(8): e505–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz LM, Woloshin S, Birkmeyer JD. How do elderly patients decide where to go for major surgery? Telephone interview survey. BMJ 2005; 331(7520): 821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vater LB, Donohue JM, Park SY, Schenker Y. Trends in Cancer-Center Spending on Advertising in the United States, 2005 to 2014. JAMA Intern Med 2016; 176(8): 1214–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfister DG, Rubin DM, Elkin EB, et al. Risk Adjusting Survival Outcomes in Hospitals That Treat Patients With Cancer Without Information on Cancer Stage. JAMA oncology 2015; 1(9): 1303–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.