ABSTRACT
Acute-on-chronic liver failure (ACLF) is a recently recognised and defined syndrome seen in patients with liver cirrhosis and carries a high short-term mortality in excess of 15% at 28 days. ACLF is defined by organ failures (OFs) and is distinct from simple ‘acute decompensation’ (AD) of cirrhosis. OFs involve the liver, kidney, brain, coagulation, respiratory system and the circulation, and are defined by the European Association for the Study of the Liver Chronic Liver Failure Consortium (CLIF-C) OF score. The central pathophysiological mechanism in the development of ACLF is intense systemic inflammation, which distinguishes this syndrome from AD. The most frequent precipitating event of ACLF in the western world is bacterial infection and active alcohol intake, whereas hepatitis B flare followed by sepsis and active alcohol intake are the common precipitating events in the east. In about 40% patients with ACLF, however, no precipitating event is found. The course of ACLF is dynamic and reversible, so early identification and early initiation of supportive therapy is of utmost importance. Unfortunately, to date, there is no known specific therapy for ACLF except for liver transplantation, so the treatment revolves around institution of early organ support. Most of the patients will have a clear prognosis between 3–7 days of hospitalisation. CLIF-C ACLF score is the best available prognostic score in patients with ACLF.
KEYWORDS: Acute-on-chronic liver failure, liver cirrhosis, organ failure, acute decompensation, high short-term mortality
Key points
Acute-on-chronic liver failure (ACLF) is clinically and pathophysiologically distinct syndrome which carries high short-term mortality.
The diagnosis of ACLF is made in patients with acute decompensation of liver cirrhosis with organ failure. Organ failure is defined by the Chronic Liver Failure – Sequential Organ Failure Assessment (CLIF-SOFA) score which is a modification of the SOFA score.
The prognosis of patients with ACLF is better defined by CLIF-C ACLF score as compared to Child–Pugh–Turcotte and Model for End-stage Liver Disease scores.
The mainstay of the management of patients with ACLF is organ support and treatment of the precipitating event.
Patients with ACLF have comparable survival as compared to patients without ACLF post-liver transplant.
Introduction
Acute decompensation (AD) of liver cirrhosis and acute-on-chronic liver failure (ACLF) are the two most important, yet pathophysiologically distinct, clinical entities seen in patients admitted to hospital with a complication of cirrhosis. Acute decompensation refers to the development of ascites, hepatic encephalopathy, gastrointestinal haemorrhage, or any combination of these conditions in patients with liver cirrhosis.1,2 ACLF, on the other hand, is a distinct clinical condition characterised by hepatic or extrahepatic organ failures and carries high short-term mortality in excess of 15% at 28 days.1,2 Three major features characterise this syndrome: ACLF occurs in the context of intense systemic inflammation; ACLF frequently develops in close temporal relationship with pro-inflammatory precipitating events (eg infections or alcoholic hepatitis); and ACLF is associated with single- or multiple-organ failure.
Defining ACLF
Although there is considerable heterogeneity in the definition of ACLF primarily emanating from disagreements over the stage of underlying liver disease (from non-cirrhotic chronic liver disease to decompensated cirrhosis) and whether the precipitating event is primarily hepatic or extra-hepatic, most definitions address the role of both hepatic and extra-hepatic precipitating events and include extra-hepatic organ failures (Table 1).1–3 The European definition, proposed by the European Association for the Study of the Liver – Chronic Liver Failure (EASL-CLIF) Consortium, applies to patients with acute decompensation of cirrhosis, with or without prior decompensating events and does not exclude extrahepatic precipitating events.1 The EASL-CLIF definition is based on the prospective investigation of 1,343 consecutive patients hospitalised for acute decompensation. The organ failures were identified by the modified Sequential Organ Failure Assessment (SOFA) score (Fig 1), which considers the function of the liver, kidney, brain, coagulation, circulation and respiration allowing stratification of patients in subgroups with different risks of death (Fig 2). The EASL-CLIF definition is validated in large-scale studies from Europe, Asia and the USA in different precipitating events.1,4–7
Table 1.
Variations in worldwide definitions of acute-on-chronic liver failure
| Consortium | EASL-CLIF1 | APASL2 | NACSELD3 |
|---|---|---|---|
| Diagnostic parameters | Specified criteria using CLIF-OF score(s) for OF, 28-day mortality rate >15% from AD of cirrhosis, with/without prior decompensation often caused by infection | Acute jaundice and coagulopathy, followed by ascites ±HE <4 weeks in undiagnosed or diagnosed chronic liver disease, including cirrhosis | Specified criteria for ≥2 OFs in patients with infection, at or during admission |
| Exclusion criteria | Patients admitted electively for procedures or therapy, or those with hepatocellular carcinoma outside Milan criteria, or receiving immunosuppressive therapy, with HIV or with severe chronic extrahepatic disease | Bacterial infection or previous AD | Outpatients with infection, any patient with HIV infection, prior organ transplants or disseminated malignancies |
AD = acute decompensation; ACLF = acute-on-chronic liver failure; APASL = Asian Pacific Association for the Study of the Liver; CLIF-OF = Chronic Liver Failure – Organ Failure; EASL-CLIF = European Association for the Study of the Liver – Chronic Liver Failure; HE = hepatic encephalopathy; NACSELD = North American Consortium for the Study of End-stage Liver Disease.
Fig 1.
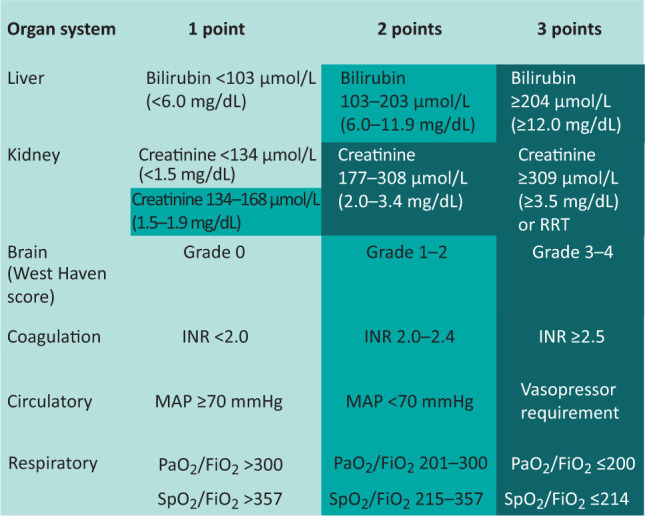
Diagnostic criteria of organ dysfunction and failure. Adapted from Moreau R, Jalan R, Gines P et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–37. FiO2 = fraction of inspired oxygen; INR = international normalised ratio; MAP = mean arterial pressure; PaO2 = partial pressure of oxygen; RRT = renal replacement therapy; SpO2 = oxygen saturation.
Fig 2.
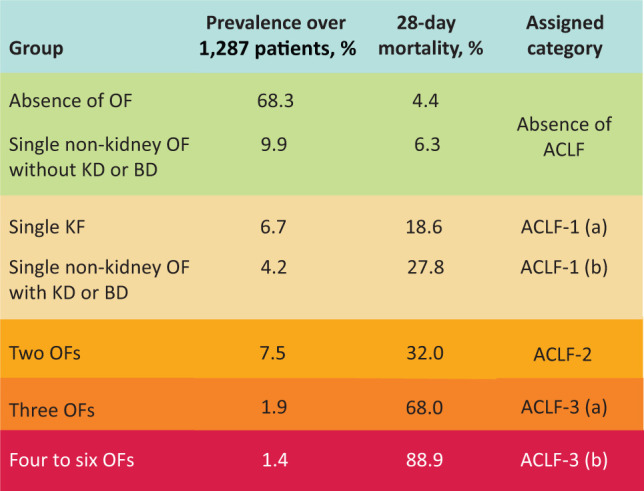
Diagnostic criteria of acute-on-chronic liver failure and their grades. Adapted from Moreau R, Jalan R, Gines P et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–37. ACLF = acute-on-chronic liver failure; BD = brain dysfunction; KD = kidney dysfunction; KF = kidney failure; OF = organ failure.
Pathophysiology of ACLF
Although the pathophysiology of ACLF is currently largely unknown, intense systemic inflammation and oxidative stress are believed to play a central and definitive role in the pathogenesis of ACLF, which distinguishes it from patients who have acute decompensation without organ failure.8 Furthermore, the extent of systemic inflammation co-relates directly with the severity of ACLF; the higher the grade of ACLF, greater the systemic inflammation.8
Recognizing ACLF: The clinical features
ACLF occurs simultaneously or very early after the acute decompensation episode. In the CANONIC study, ACLF was present in 22.6% of patients at admission and another 8.3% of patients developed ACLF during the first 2 weeks of admission.1 It is of utmost importance to recognise ACLF early and institute therapy to reverse the natural history of the disease, bacterial infection and alcoholic hepatitis are the most common precipitating events.1
The PIRO concept (predisposition, injury, response and organ involvement) helps in the early recognition of ACLF. In this example, a patient with a history of alcohol-related cirrhosis presents with fever and ascites. Laboratory investigation shows white cell count (WCC) of 16,000 /mm3 and C-reactive protein (CRP) of 59 mg/L, ascitic fluid WCC of 800 /mm3, serum total bilirubin of 318 µmol/L and prothrombin time of 35 seconds. In this patient, the predisposition is alcohol-related cirrhosis; injury is spontaneous bacterial peritonitis; response is systemic inflammation characterised by high WCC and CRP and the organs involved are liver and coagulation.
Although ACLF carries a high 28-day mortality of 32%, it has a highly variable course.1 In the prospective CANONIC study, it was found that ACLF grade 1 is potentially reversible in the majority of patients: 54.5% of patients had a reversal to no ACLF, 21% remained in ACLF grade 1 and the rest (24.5%) progressed to a higher grade of ACLF to grade 2 or 3. For patients presenting with ACLF grade 3, 32% of patients had a regression in ACLF grade while the rest (68%) remained in ACLF grade 3. Thus, ACLF as a syndrome is potentially reversible in some patients.9
Assessment of prognosis in patients with ACLF and acute decompensation
Traditionally, the prognostic assessment of patients with liver cirrhosis has been carried out by determining the severity of portal hypertension and by assessing the severity of liver disease as defined by Childs–Pugh–Turcotte (CTP) or Model for End-stage Liver Disease (MELD) score. These scores and criteria, however, fail to correctly and adequately prognosticate patients with ACLF.10 A new scoring system developed by the EASL-CLIF Consortium, the CLIF-C ACLF score, has superior performance in prediction of mortality in patients with ACLF. The CLIF-C ACLF score, which can be calculated via a free online calculator (www.efclif.com/scientific-activity/score-calculators/clif-c-aclf) is based on the CLIF-C organ failure score, age and white cell count, since these three factors are the independent predictors of mortality in patients with ACLF.1 This score was obtained from CANONIC study and has been further validated in external cohorts.11 The CLIF-C ACLF score outperforms CTP, MELD and MELD-Na scores in predicting 28-day mortality.11
Treatment of patients with ACLF
There is currently no specific therapy for ACLF. The main principles of treatment are to diagnose and treat precipitating events and provide supportive therapy. Organ support in an intensive care unit, with care overseen by physicians who are experts in liver disease management, may be of benefit for patients with life-threatening, single- or multiple-organ failure who have not responded to standard therapy.
Treating the precipitating event
Bacterial or fungal infection
The prevalence of infection, either precipitating or complicating, in patients with ACLF is over 50% and increases with the grade of ACLF.12 Although the causative organisms are most often bacteria, fungal infection is not uncommon. Anti-microbial treatment should commence as soon as possible based on suspected site involved, culture/isolation results, and local anti-microbial sensitivity patterns.
Variceal haemorrhage
An episode of variceal haemorrhage should be managed according to the updated society guidance (Baveno/EASL/American Association for the Study of Liver Diseases). The standard medical treatment includes volume restitution, a combination of safe vasoconstrictor agent (somatostatin, octreotide or terlipressin), antibiotic prophylaxis and endoscopic therapy preferably within 12 hours of presentation. Additionally, a patient presenting with haematemesis should be electively intubated. Two recently published studies show that the presence of ACLF is the single most important determinant of death in patients with variceal bleeding, and pre-emptive transjugular intrahepatic portosystemic shunt (TIPSS) as well as rescue TIPSS improves survival in patients with ACLF.13,14
Alcoholic hepatitis
Although prednisolone therapy is indicated in patients with alcoholic hepatitis, the response to prednisolone is negatively correlated with the number of organ failures at baseline.15 The added susceptibility of patients with ACLF to new infection makes it even more challenging to use steroids in these patients. A careful assessment for ongoing infection is of utmost importance in decision making for steroid therapy. The response to steroids should be assessed on day 7 with the Lille score, and if there is no response on day 7, the treatment should be discontinued.
Acute viral hepatitis or reactivation
There is no specific agent for acute viral hepatitis except for hepatitis B. In the event of hepatitis B virus infection at presentation, potent nucleotide or nucleoside analogues should be started at the earliest pending the confirmation based on viral deoxyribonucleic acid load.2
Supportive therapy
Cardiovascular and renal support
In the western world, acute kidney injury is the most common organ failure.1 Withdrawal of diuretics, volume expansion with intravenous albumin, as well as urine tests to identify whether the acute renal injury is acute tubular necrosis or type 1 hepato-renal syndrome should be undertaken.16 If there is no response to volume expansion and withdrawal of diuretics, treatment with vasoconstrictor agents should be started. The likelihood of renal response to vasoconstriction is inversely related to the number of organ failures.17 norepinephrine is the first-line vasopressor in the management of persistent shock.
Treatment of encephalopathy
The airway should be protected with elective intubation in patients with high-grade encephalopathy (grade 3/4). Lactulose therapy and concomitant use of rifaximin can lead to rapid resolution of hepatic encephalopathy; care should be taken not to induce profuse diarrhoea. Albumin dialysis can be used in patients with grade 3 or 4 hepatic encephalopathy refractory to lactulose treatment.
Extracorporeal liver support
Thus far, randomised clinical trials of extra-corporeal liver support devices have failed to show any mortality benefit in patients with ACLF. These include the albumin dialysis and an extracorporeal liver device incorporating hepatocytes compared with standard medical therapy.18,19
Liver transplantation
Liver transplantation is currently the only known and efficacious treatment for patients with ACLF. The 1-year survival rates after liver transplantation among patients with ACLF with one or two organ failures do not differ significantly from patients without organ failures. In patients with three or more organ failures, the survival post-transplantation approaches 80% as compared with survival rates of less than 20% among patients who do not undergo liver transplantation.10,20
Conclusion
ACLF has emerged to be the most common cause of inpatient death in cirrhosis, and is a major public health problem in view of the increasing rate of liver disease mortality in the UK and globally. ACLF is characterised by marked systemic inflammation and organ failure(s), usually associated with a precipitating event. The development of validated scoring systems sets the foundation for assessment of prognosis and stratifying patients for clinic.
References
- 1.Moreau R, Jalan R, Ginès P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–37. [DOI] [PubMed] [Google Scholar]
- 2.Sarin SK, Choudhury A, Sharma MK, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL): an update. Hepatol Int 2019;13:353–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bajaj J, O’Leary J, Reddy K, et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology 2014;60:250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li H, Chen LY, Zhang NN, et al. Characteristics, diagnosis and prognosis of acute-on-chronic liver failure in cirrhosis associated to hepatitis B. Sci Rep 2016;6:25487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu T, Li J, Shao L, et al. Development of diagnostic criteria and a prognostic score for hepatitis B virus-related acute-on-chronic liver failure. Gut 2018;67:2181–91. [DOI] [PubMed] [Google Scholar]
- 6.Mahmud N, Kaplan DE, Taddei TH, Goldberg DS. Incidence and mortality of acute-on-chronic liver failure using two definitions in patients with compensated cirrhosis. Hepatology 2019;69:2150–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hernaez R, Kramer JR, Liu Y, et al. Prevalence and short-term mortality of acute-on-chronic liver failure: a national cohort study from the USA. J Hepatol 2019;70:639–47. [DOI] [PubMed] [Google Scholar]
- 8.Clària J, Stauber RE, Coenraad MJ, et al. Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology 2016;64:1249–64. [DOI] [PubMed] [Google Scholar]
- 9.Gustot T, Fernandez J, García E, et al. Clinical course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology 2015;62:243–52. [DOI] [PubMed] [Google Scholar]
- 10.Sundaram V, Jalan R, Wu T, et al. Factors associated with survival of patients with severe acute-on-chronic liver failure before and after liver transplantation. Gastroenterology 2019;156:1381– 91.e3. [DOI] [PubMed] [Google Scholar]
- 11.Jalan R, Saliba F, Pavesi M, et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol 2014;61:1038–47. [DOI] [PubMed] [Google Scholar]
- 12.Fernández J, Acevedo J, Wiest R, et al. Bacterial and fungal infections in acute-on-chronic liver failure: prevalence, characteristics and impact on prognosis. Gut 2018;67:1870–80. [DOI] [PubMed] [Google Scholar]
- 13.Trebika J, Gu W, Ibanez-Samaniego L, et al. Rebleeding and mortality are increased by ACLF but reduced by pre-emptive TIPS. J Hepatol 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 14.Kumar R, Kerbert AJC, Sheikh MF, et al. Determinant of mortality in patients with cirrhosis and uncontrolled variceal bleeding. J Hepatol 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15.Sersté T, Cornillie A, Njimi H, et al. The prognostic value of acute-on-chronic liver failure during the course of severe alcoholic hepatitis. J Hepatol 2018;69:318–24. [DOI] [PubMed] [Google Scholar]
- 16.Ginès P, Schrier RW. Renal failure in cirrhosis. N Engl J Med 2009;361:1279–90. [DOI] [PubMed] [Google Scholar]
- 17.Piano S, Schmidt HH, Ariza X, et al. Association between grade of acute on chronic liver failure and response to terli pressin and albumin in patients with hepatorenal syndrome. Clin Gastroenterol Hepatol 2018;16:1792– 800.e3. [DOI] [PubMed] [Google Scholar]
- 18.Kribben A, Gerken G, Haag S, et al. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology 2012;142:782– 9.e3. [DOI] [PubMed] [Google Scholar]
- 19.Thompson J, Jones N, Al-Khafaji A, et al. Extracorporeal cellular therapy (ELAD) in severe alcoholic hepatitis: a multinational, prospective, controlled, randomized trial. Liver Transpl 2018;24:380–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Artru F, Louvet A, Ruiz I, et al. Liver transplantation in the most severely ill cirrhotic patients: a multicentre study in acute-on-chronic liver failure grade 3. J Hepatol 2017;67:708–15. [DOI] [PubMed] [Google Scholar]


