Abstract
Immune-related molecular and genetic pathways that are connected to colorectal cancer (CRC) and lifestyles in postmenopausal women are incompletely characterized. In this study, we examined the role of pro-inflammatory biomarkers such as C-reactive protein (CRP) and interleukin-6 (IL-6) in those pathways. Through selection of the best predictive single-nucleotide polymorphisms (SNPs) and lifestyles, our goal was to improve the prediction accuracy and ability for CRC risk. Using large cohort data of postmenopausal women from the Women’s Health Initiative Database for Genotypes and Phenotypes Study, we previously conducted a genome-wide association (GWA) for a CRP and IL-6 gene-behavioral interaction study. For the present study, we added GWA-SNPs from outside GWA studies, resulting in a total of 152 SNPs. Together with 41 selected lifestyles, we performed a 2-stage multimodal random survival forest analysis with generalized multifactor dimensionality reduction approach to construct CRC risk profiles. Overall and in obesity strata (by body mass index, waist circumference, waist-to-hip ratio, exercise, and dietary fat intake), we identified the best predictive genetic markers in inflammatory cytokines and lifestyles. Across the strata, 2 SNPs (ONECUT2 rs4092465 and HNF4A rs1800961) and 1 lifestyle factor (relatively short-term past use of oral contraceptives) were the most common and strongest predictive markers for CRC risk. The risk profile that combined those variables exhibited synergistically increased risk for CRC; this pattern appeared more strongly in obese and inactive subgroups. Our results may contribute to improved predictability for CRC and suggest genetically targeted lifestyle interventions for women carrying the inflammatory-risk genotypes, reducing CRC risk.
Keywords: Random survival forest, generalized multifactor dimensionality reduction, inflammatory cytokines, C-reactive protein, interleukin-6, oral contraceptive, endogenous estrogen, obesity, colorectal cancer, postmenopausal women
Introduction
Chronic inflammation is a critical factor involved in the pathogenesis of obesity-attributable cancers such as colorectal cancer (CRC) from tumor initiation to progression [1,2]. In particular, CRC in postmenopausal women ages 50 years and older accounts for most (approximately 90%) of newly diagnosed CRC patients and related deaths [3], contributing to the third ranking of CRC in cancer incidence and mortality among women of the United States and Westernized countries [4,5]. CRC is indeed an inflammatory-associated disease, being seen as high risk among individuals with inflammatory bowel disease [6] or high levels of the inflammatory cytokines such as C-reactive protein (CRP) and interleukin-6 (IL-6) [7-11].These pro-inflammatory cytokines reflect different molecular pathways in acute and chronic immune responses but may be interconnected in carcinogenesis as shown in in vitro and in vivo studies [2,12-16]. In detail, CRP, a major acute-phase reactant and biomarker of chronic low-grade inflammation partially induced by IL-6, elevates the mRNA expression of genes (e.g., LOX-1) important to CRC development in CRC cell lines [12]. IL-6, upregulated by macrophages and adipose tissue, itself exhibits high mRNA expression and immunoreactivity in the CRC tissue, epithelium, and stroma [13]. Further, both inflammatory markers alter the gut microbiome, gradually forming a microenvironment that is essential to colorectal carcinogenesis [14-16]. In addition, both biomarkers exhibit higher plasma levels or mRNA expression in adipose tissue of CRC patients [17,18] and in the colon of obese individuals, accompanied by precancerous changes in the transcriptome [19], indicating that obesity-modified inflammatory pathways are associated with colorectal tumorigenesis.
Thus, the genetic variants involved in those biomarkers’ functional and structural regulation are potentially implicated in the causal pathway of inflammatory-associated CRC development that interacts with obesity factors. Earlier genomic epidemiology studies for associations between CRP/IL-6-related genetic variants and CRC risk are limited and showed inconsistent results [20-24], with only a slight effect on CRC risk [25]. The gene-phenotype pathways of CRP and IL-6 may not link to each other alone, but may also be connected to lifestyle pathways, thus being modulated by obesity (overall and visceral) [26-34], obesity-related lifestyles including lipid metabolism [34,35], a high-fat diet, exercise level, smoking, and alcohol consumption [26,36-43]. Our previous genome-wide association (GWA) study [44] of CRP and IL-6 addressed this pleiotropic effect of those biomarkers on the gene-phenotype relationship and revealed greater relationships between single-nucleotide polymorphisms (SNPs) and phenotypes among overall and viscerally obese, physically inactive, and high dietary-fat subgroups, suggesting the role of obesity in regulating the inflammatory gene-phenotype pathway. Further, the genomic pathways between CRP/IL-6 and CRC can be modified by obesity factors, suggesting that CRP/IL-6 (genotypes and phenotypes) in conjunction with obesity influence the risk of CRC (Figure S1, yellow lines). For this reason, studying how obesity factors modify the effects of genes and phenotypes, contributing to increased CRC susceptibility, is important to promote genetically targeted interventions in primary cancer prevention efforts. However, no studies thus far have examined these key pro-inflammatory cytokines in relation to CRC at the genome-wide level by incorporating a wide range of obesity-related lifestyle factors and different fat distributions of obesity status.
We hoped to address these gaps by focusing on postmenopausal women, a population vulnerable to inflammation [45], obesity, and CRC. By using a large cohort of postmenopausal women from the Women’s Health Initiative Database for Genotypes and Phenotypes (WHI dbGaP) Study, we previously performed a GWA gene-environment (G×E) interaction study with meta-analysis of subGWAs for CRP and IL-6 by evaluating interactions with obesity factors. We identified a total of 88 top GWA SNPs overall and in obesity strata [44]. In the present study, we have extended the scope of modeled SNPs by adding another 68 SNPs associated with CRP and IL-6 from earlier GWA studies that focused on European ancestry with independent replications [28,29,46,47]. We examined the relationships of these top GWA SNPs with primary CRC risk overall and in the obesity strata in which the SNPs were initially identified for the association with CRP/IL-6 in our previous GWA G×E study. This allowed us to elucidate a hypothetical empirical pathway in which a substantial proportion of the GWA SNPs in CRP and IL-6 affects CRC risk through interactions with specific lifestyle factors, and thus may contribute to understanding of the genomic immune-related etiologic pathways connected to CRC and lifestyles.
In this study, we hoped to improve the CRC prediction accuracy and ability by better characterizing the genetic architecture of the inflammatory biomarkers with incorporation of modifiable and non-modifiable risk factors. We examined the top GWA SNPs together with 41 selected lifestyles by performing a 2-stage multimodal random survival forest (RSF) analysis and generated their predictive value and accuracy for CRC. RSF, a nonparametric tree-based ensemble learning method, is one of the prediction models that has outperformed the traditional models in terms of clinical accuracy [48-52]. In particular, the RSF accounts for nonlinearity and high-order interactions among variables [53,54] and thus may provide a more accurate risk estimation. Further, we applied a generalized multifactor dimensionality reduction (GMDR) approach and characterized high-order gene-gene interactions, selecting the best genetic prediction model [55-58]. With the strongest influential SNPs and lifestyle factors selected by the RSF and GMDR, we finally constructed prediction models for CRC and calculated the combined and joint effects of genotypes and lifestyles on CRC development. We ultimately tested the hypothesis that the most-predictive genetic and lifestyle factors in combination synergistically increase the predictability of CRC risk.
Material and methods
Study population
The present study included healthy postmenopausal women from the WHI Harmonized and Imputed GWA Studies (GWASs) that were coordinated to contribute to a joint effort of imputation and harmonization for GWASs within the 2 WHI study arms, Clinical Trials and Observational Studies. Details of the study designs and rationale are described elsewhere [59,60], but briefly, healthy women were enrolled in the WHI study from 1993 through 1998 at 40 clinical centers across the U.S. if they met the following eligibility criteria: 50-79 years old, postmenopausal, expected to stay near the clinical centers for at least 3 years after enrollment, and able to provide written informed consent. Participants were further eligible for the WHI dbGaP study if they had met eligibility requirements for submission to the dbGaP and provided DNA samples. Under the dbGaP accession (phs000200.v12.p3), the Harmonization and Imputation GWASs consist of 6 subGWASs (Tables S1A and S1B). In our previous GWA G×E study, we initially included 16,088 women who reported their race or ethnicity as non-Hispanic white (Figure S2) and, by applying the exclusion criteria (i.e., diabetes history; genetic data duplications; first- and second-degree relatives; and genetic quality control [QC] based on principal components), left 10,798 women. In the present study, additional exclusion was made for those with a follow-up period of less than 1 year and/or any cancer diagnosis present at screening, leaving a total of 10,142 women (94% of the eligible women in the GWAS). These women had been followed through August 29, 2014, with a mean of 16 years of follow-up; 737 (7%) of them had developed primary CRC. The Institutional Review Boards of each WHI-participating clinical center and the University of California, Los Angeles, approved this study.
Data collection and CRC outcome
The WHI coordinating centers had collected participant information via self-administered questionnaire and periodically performed data quality assurance. For the purpose of our analysis, we initially selected 41 variables assessed at screening on the basis of their association with inflammation and CRC through a literature review [1,2,17-19,26,34-43,61-64], followed by preliminary analyses such as univariate and stepwise multiple regressions and a multicollinearity test. Those examined variables are as follows: demographic (age, education, and marital status) and socioeconomic factors (family income and employment); family history of diabetes and CRC; medical (hypertension, high cholesterol, cardiovascular disease, and depressive symptoms) and reproductive histories (hysterectomy, one or both ovaries removed, ages at menarche and menopause, pregnancy, breast feeding, oral contraceptive [OC] use, and exogenous estrogen [E] only and E plus progestin [E+P] use); lifestyles (physical activity and cigarette smoking); and daily diet (dietary energy, alcohol, total sugar, fiber, fruit, and vegetable consumption; percentage of calories from protein, carbohydrates, saturated fatty acids [SFA], monounsaturated FA [MFA], and polyunsaturated FA [PFA]). The anthropometric variables height, weight, and waist and hip circumferences had been measured by trained staff and were further included in our analysis.
The CRC outcomes were determined via a centralized review of medical charts and pathology/cytology reports by a committee of physicians. Cancer sites were recorded according to the National Cancer Institute’s Surveillance, Epidemiology, and End-Results guidelines [65]. The time from enrollment to primary CRC development, censoring, or study end point was measured and calculated in years.
Genotyping and laboratory methods
Genotyped data were extracted from the WHI dbGaP GWASs database, normalized to the reference panel GRCh37, and imputed using 1000 Genomes reference panels [60]. Details of the data-cleaning process have been previously discussed [44,60,66]. Briefly, the SNPs’ harmonization was checked via pairwise concordance in all samples across the GWASs. The initial data QC step filtered SNPs with a missing call rate of > 2% and a Hardy-Weinberg equilibrium of P < 1E-04. In the second QC step, SNPs with Ȓ 2 ≥ 0.6 imputation quality were included [67], but individuals with a KING kinship estimate > 0.088 were excluded [68].
Blood samples from participants who had fasted for at least 8 hours had been collected at baseline by trained phlebotomists. Serum levels of CRP were analyzed via a high-sensitivity immunoturbidimetric assay (Kamiya Biomedical Company) and of IL-6 by the Quantitative Sandwich Enzyme Immunoassay technique (Quantikine HS Immunoassay Kit; R&D Systems, Inc., Minneapolis, MN), with median inter-assay coefficients of variation of 2.3% and 12.4%, respectively.
Statistical analysis
Participants’ characteristics at baseline and allele frequencies by CRC were examined via unpaired 2-sample t tests (for continuous variables) and chi-squared tests (for categorical variables). If continuous variables were skewed or had outliers, the Wilcoxon rank-sum test was conducted. Our earlier GWAS evaluated obesity factors as an effect modifier via a formal interaction test and stratifications defined by body mass index (BMI; 30 kg/m2 cutoff), waist circumference (WST; 88 cm), waist-to-hip ratio (WHR; 0.85), metabolic equivalents (METs; 10·hours/week), and percentage of calories from SFA (9%). The testing results from each sub-GWAS were combined via a meta-analysis assuming a fixed effects model. In the present study, we excluded 1 SNP from the 88 SNPs in our previous study due to high missing proportion and examined their association with CRC in a particular lifestyle setting in which the SNPs were identified. Of another 68 SNPs obtained from other GWASs, 3 SNPs were also excluded due to high missing values and were analyzed both overall and in subgroups.
We performed the RSF analysis on the quality adjusted data. The RSF uses bootstrapping to generate samples using about 60% of the original dataset and grows a tree from each sample via a splitting rule to maximize differences in survival rate across daughter nodes. The tree-building process is repeated numerous times (n=5,000 in this study) and aggregated in a forest of trees for prediction [48,69]. An ensemble cumulative hazard estimate was computed from each tree and averaged over all trees for each individual, and that estimate was used to calculate a predicted cumulative CRC incidence rate. By using this ensemble estimate and creating the out-of-bag (OOB) data from the remaining 40% of the original data, the OOB concordance index (C-index) was calculated, which is a measure of prediction performance similar to the area under the receiver operating characteristic (AUROC) curve [69,70]. Each variable’s ranking was determined according to its prediction ability for CRC via 2 prediction parameters: 1) minimal depth (MD), in which variables that have a small MD split the tree close to the root, thus being considered highly predictive and 2) variable importance (VIMP), on the basis of permutation strategy using the OOB C-index, in which variables that have greater VIMPs are more predictive [53].
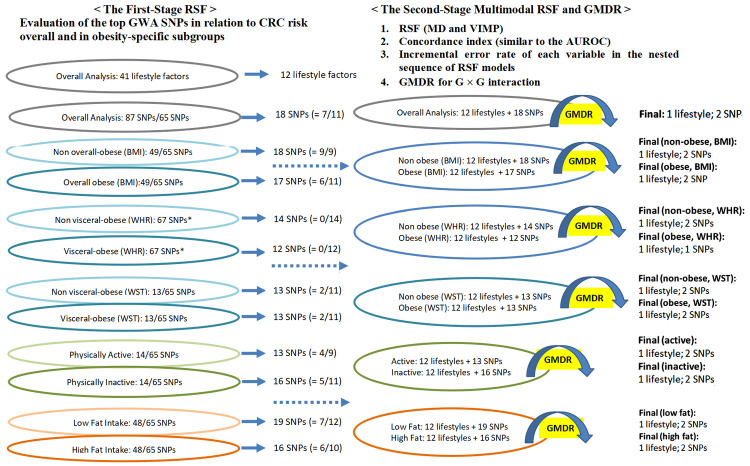
A 2-stage RSF was performed (Figure 1). In the first stage, we conducted separate RSF analyses on SNPs (overall and in obesity strata) and lifestyles. With only those SNPs and lifestyles that had a significantly low MD and high VIMP, we performed the second RSF with a multimodal approach: overall and in obesity strata 1) comparing MD and VIMP values in the plot, 2) calculating the OOB C-index from the nested RSF model, and 3) computing the incremental error rate of each variable in the nested sequence RSF models and from the top variable, calculating a dropping error rate. This approach allowed us to exclude from the outset the SNPs and lifestyles that were not significantly associated with CRC, resulting in increased statistical power and an adjusted type I error rate [48]. Additionally, we applied a GMDR approach, which is described elsewhere [55-57]. Briefly, the GMDR reduces high-dimensional multifactor prediction to a single dimension by the ratio of high vs. low risk, and it detects the best gene-gene interaction model. It generates key prediction parameters, such as testing balance accuracy (TBA), cross-validation consistency (CVC), and sign p value. The model with the highest TBA, CVC 10/10, and P < 0.05 based on 1,000-times permutation testing was considered the best model.
Figure 1.
Two-stage random survival forest (RSF) and generalized multifactor dimensionality reduction (GMDR). (BMI, body mass index; CRC, colorectal cancer; GWA, genome-wide association; MD, minimal depth; SNP, single-nucleotide polymorphism; WHR, waist-to-hip ratio; WST, waist circumference; VIMP, variable of importance. * WHR subgroups combined 2 our GWA and 65 outside GWA SNPs).
We further performed multiple Cox proportional hazards regressions with an assumption test via a Schoenfeld residual plot and r evaluation to obtain hazard ratios (HRs) and 95% confidence intervals (CIs) for the single and combined effects of SNPs and lifestyle factors on CRC, by adjusting for covariates (Table 1). A 2-tailed p value < 0.05 was considered statistically significant with multiple-comparison corrections by the Benjamini-Hochberg method [71]. R v.3.6.3. (survival, survivalROC, randomForestSRC, ggRandomForests, gamlss, ggsurvplot, and forestplot packages) and GMDR v.1.0. were used.
Table 1.
Characteristics of participants, stratified by CRC
| Characteristic | Participants without CRC (n=9,405) | Participants with CRC (n=737) | ||
|---|---|---|---|---|
|
|
|
|||
| n | (%) | n | (%) | |
| Age in years, mean (SD) | 67 | (6.66) | 66 | (6.57)* |
| Education | ||||
| ≤ High school | 3,409 | (36.2) | 220 | (29.9)* |
| > High school | 5,996 | (63.8) | 517 | (70.1) |
| Marital status | ||||
| Currently not married | 3,649 | (38.8) | 288 | (39.1) |
| Currently married | 5,756 | (61.2) | 449 | (60.9) |
| Family income | ||||
| < $35,000 | 4,253 | (45.2) | 315 | (42.7) |
| ≥ $35,000 | 5,152 | (54.8) | 422 | (57.3) |
| Employment | ||||
| Currently employed (full- or part-time) | 6,900 | (73.4) | 523 | (71.0) |
| Currently not employed | 2,505 | (26.6) | 214 | (29.0) |
| Cardiovascular disease ever | ||||
| No | 7,995 | (85.0) | 610 | (82.8) |
| Yes | 1,410 | (15.0) | 127 | (17.2) |
| Hypertension ever | ||||
| No | 6,506 | (69.2) | 487 | (66.1) |
| Yes | 2,899 | (30.8) | 250 | (33.9) |
| Family history of CRC | ||||
| No | 7,932 | (84.3) | 610 | (82.8) |
| Yes | 1,473 | (15.7) | 127 | (17.2) |
| Depressive symptom† | ||||
| < 0.06 | 8,724 | (92.8) | 666 | (90.4)* |
| ≥ 0.06 | 681 | (7.2) | 71 | (9.6) |
| METs·hour·week-1, mean (SD)¶ | 10.95 | (12.84) | 11.49 | (12.73) |
| METs·hour·week-1 ¶ | ||||
| ≥ 10.0 | 3,881 | (41.3) | 322 | (43.7) |
| < 10.0 | 5,524 | (58.7) | 415 | (56.3) |
| Cigarettes smoked per day | ||||
| Never smoked | 5,018 | (53.4) | 380 | (51.6) |
| < 15 | 2,386 | (25.4) | 185 | (25.1) |
| ≥ 15 | 2,001 | (21.3) | 172 | (23.3) |
| Years of regular smoking | ||||
| Never smoked | 5,018 | (53.4) | 380 | (51.6) |
| < 5 | 510 | (5.4) | 43 | (5.8) |
| 5-9 | 524 | (5.6) | 37 | (5.0) |
| 10 + | 3,353 | (35.7) | 277 | (37.6) |
| Dietary alcohol per day in g, mean (SD) | 6.12 | (11.45) | 6.35 | (11.92) |
| % calories from carbohydrates, mean (SD) | 49.01 | (8.69) | 49.37 | (8.91) |
| Dietary total sugars in g, mean (SD) | 98.88 | (43.73) | 100.02 | (42.93) |
| % calories from SFA, median (range) | 11.34 | (2.22-32.39) | 11.44 | (2.60-26.77) |
| % calories from SFA€ | ||||
| < 9.0 % | 2,121 | (22.6) | 169 | (22.9) |
| ≥ 9.0 % | 7,284 | (77.4) | 568 | (77.1) |
| % calories from MFA, mean (SD) | 12.71 | (3.26) | 12.56 | (3.22) |
| % calories from PFA, mean (SD) | 6.83 | (2.09) | 6.80 | (2.04) |
| Height in cm, mean (SD) | 161.9 | (6.00) | 162.5 | (6.07)* |
| Weight in kg, mean (SD) | 72.99 | (14.79) | 72.98 | (14.10) |
| BMI in kg/m2, mean (SD) | 27.80 | (5.36) | 27.61 | (5.19) |
| BMI¥ | ||||
| < 30.0 | 6,613 | (70.3) | 538 | (73.0) |
| ≥ 30.0 | 2,792 | (29.7) | 199 | (27.0) |
| Waist circumference in cm, mean (SD) | 86.72 | (12.86) | 87.3 | (12.30) |
| Waist circumference¥ | ||||
| ≤ 88 | 5,574 | (59.3) | 424 | (57.5) |
| > 88 | 3,831 | (40.7) | 313 | (42.5) |
| Hip circumference in cm, mean (SD) | 106.5 | (11.16) | 106.6 | (10.87) |
| Waist-to-hip ratio, mean (SD) | 0.813 | (0.073) | 0.8184 | (0.074) |
| Waist-to-hip ratio¥ | ||||
| ≤ 0.85 | 6,702 | (71.3) | 520 | (70.6) |
| > 0.85 | 2,703 | (28.7) | 217 | (29.4) |
| Age at menopause in years, mean (SD) | 48 | (6.20) | 49 | (6.26) |
| Total months of breastfeeding | ||||
| 1-6 | 3,363 | (35.8) | 287 | (38.9)* |
| 7-12 | 4,451 | (47.3) | 357 | (48.4) |
| > 13 | 1,591 | (16.9) | 93 | (12.6) |
| Oral contraceptive duration in years, mean (SD) | 6.71 | (3.54) | 5.16 | (3.10)* |
| Oral contraceptive duration£ | ||||
| < 5.1 | 2,745 | (29.2) | 381 | (51.7)* |
| ≥ 5.1 | 6,660 | (70.8) | 356 | (48.3) |
| Exogenous estrogen use (E-only) in years | ||||
| Never | 6,588 | (70.0) | 488 | (66.2)* |
| < 5 | 1,312 | (14.0) | 106 | (14.4) |
| 5 to < 10 | 476 | (5.1) | 54 | (7.3) |
| ≥ 10 | 1,029 | (10.9) | 89 | (12.1) |
| Exogenous estrogen use (E+P) in years | ||||
| Never | 7,753 | (82.4) | 567 | (76.9)* |
| < 5 | 900 | (9.6) | 86 | (11.7) |
| 5 to < 10 | 394 | (4.2) | 42 | (5.7) |
| ≥ 10 | 358 | (3.8) | 42 | (5.7) |
BMI, body mass index; CRC, colorectal cancer; E, estrogen; E+P, estrogen + progestin; MET, metabolic equivalent; MFA, monounsaturated fatty acids; PFA, polyunsaturated fatty acids; RSF, random survival forest; SFA, saturated fatty acids.
P < 0.05, chi-squared or Wilcoxon’s rank-sum test.
Depression scales were estimated using a short form of the Center for Epidemiologic Studies Depression Scale.
Physical activity was estimated via recreational physical activity combining walking and mild, moderate, and strenuous physical activity.
Each activity was assigned a MET value corresponding to intensity; the total MET·hours·week-1 was calculated by multiplying the MET level for the activity by the hours exercised per week and summing the values for all activities. The total MET was stratified into 2 groups, with 10 METs as the cutoff according to current American College of Sports Medicine and American Heart Association recommendations [97].
Percent calories from SFA was classified by 9%, addressing low sample power (i.e., containing a quarter in one side) and adherent to the American Heart Association and American College of Cardiology dietary guidelines, which are aligned with the 2015-2020 Dietary Guidelines for Americans to help cardiovascular and metabolic diseases reductions [98].
BMI, waist circumference, and waist-to-hip ratio were categorized at 30 kg/m2, 88 cm, and 0.85, respectively, where those cutoff levels or higher fall within the overall or visceral obese range (https://www.cdc.gov/obesity/adult/defining.html; [99]).
Duration of oral contraceptive use was stratified at 5.1 years, where the cutoff level or higher fall within the high-risk group in the RSF model.
Results
Participants’ characteristics at screening according to CRC development (Table 1) and the allele frequencies of 152 GWA CRP/IL-6 SNPs for each WHI subGWAS (Tables S1A and S1B) are displayed. Participants who developed CRC were likely to be younger, highly educated, more depressed, and taller. They also tended to have shorter breastfeeding periods and shorter durations of past OC use but higher frequencies and longer durations of E-only and E+P use.
Two-stage multimodal RSF and GMDR
We analyzed the 152 GWA SNPs (one set of 87 from our GWAS and another set of 65 from outside GWASs) and 41 selected lifestyle factors by implementing the 2-stage RSF and GMDR (Figure 1) to identify the most predictive genetic and lifestyle markers with the highest predictability and lowest prediction error for CRC risk. In the first stage of RSF (Figure S3), we calculated the 2 predicted values, MD and VIMP, and plotted to compare them; they use different prediction algorithms, so we expected the variables’ ranking to be somewhat different. Separately, for each set of GWA SNPs and the 41 lifestyles, we identified the best predictive genetic and lifestyle factors on the basis of the agreement with high ranks in both MD and VIMP (Figures 1 and S3) as follows: 12 of 41 lifestyles; 18 of 152 SNPs overall (in detail, 7 from our GWAs and 11 from outside GWASs); 18 and 17 of 114 SNPs (BMI < 30 and ≥ 30, respectively); 14 and 12 of 67 SNPs (WHR ≤ 0.85 and > 0.85); 13 and 13 of 78 SNPs (WST ≤ 88 and > 88); 13 and 16 of 79 SNPs (METs ≥ 10 and < 10); and 19 and 16 of 113 SNPs (SFA < 9 and ≥ 9).
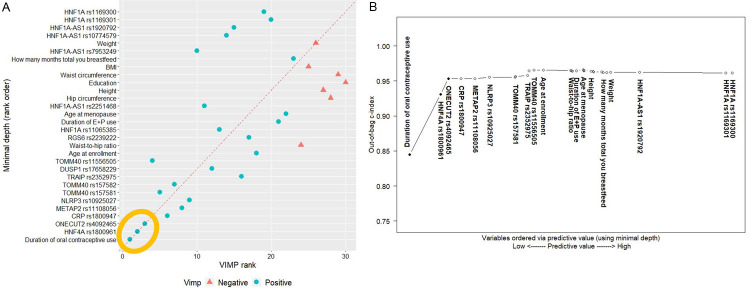
The 12 lifestyles and selected SNPs together, overall and in the obesity strata, were carried over to the second stage of multimodal RSF to generate risk profiles with the most predictive variables that account for both genetic and lifestyle factors. Particularly, in the overall group, we first calculated the 2 measures MD and VIMP (Table 2) and plotted them (Figure 2A); the dashed red line reflects the agreement of the 2 measures. Both measures in agreement with high ranks revealed that 2 SNPs (HNF4A rs1800961 and ONECUT2 rs4092465) and 1 lifestyle (past OC use) were the best predictive variables for CRC risk. Next, the C-index (i.e., the AUROC) was computed from the nested RSF model (Table 2) and plotted (Figure 2B), where variables were ranked by MD. From that, we identified the same set of top variables (2 SNPs and 1 lifestyle). Those top variables substantially improved the C-index prediction accuracy (AUROC=0.95), whereas others did not, suggesting the complementary prediction ability of the C-index. Further, we estimated a dropping error rate for each variable in the nested sequence of the RSF models (Table 2), identifying once again the same top 3 variables as the strongest contributors that dropped the error rate, thus substantially improving the prediction accuracy. Finally, we applied the GMDR approach (Table S2) and determined the best gene-by-gene interaction model; the 2-factor model including the top 2 SNPs was the most predictive, with the highest TBA of 0.7019 and CVC of 10/10 (P < 0.001).
Table 2.
The second stage of random survival forest analysis: predictive value of variables in overall analysis
| Variable* | Minimal Depth† | VIMP | C-index | Error¶ | Drop Error§ |
|---|---|---|---|---|---|
| Duration of oral contraceptive use | 1.9450 | 0.0467 | 0.8449 | 0.1551 | 0.3449 |
| HNF4A rs1800961 | 2.5412 | 0.0263 | 0.9308 | 0.0692 | 0.0859 |
| ONECUT2 rs4092465 | 2.6928 | 0.0179 | 0.9534 | 0.0466 | 0.0226 |
| CRP rs1800947 | 2.9376 | 0.0115 | 0.9533 | 0.0467 | -0.0001 |
| METAP2 rs11108056 | 3.2086 | 0.0102 | 0.9534 | 0.0466 | 0.0001 |
| NLRP3 rs10925027 | 3.4894 | 0.0073 | 0.9554 | 0.0446 | 0.0020 |
| TOMM40 rs157581 | 3.9874 | 0.0119 | 0.9552 | 0.0448 | -0.0002 |
| TOMM40 rs157582 | 3.9934 | 0.0104 | 0.9562 | 0.0438 | 0.0011 |
| TRAIP rs2352975 | 4.2272 | 0.0027 | 0.9580 | 0.0420 | 0.0017 |
| DUSP1 rs17658229 | 4.2598 | 0.0047 | 0.9647 | 0.0353 | 0.0067 |
| TOMM40 rs11556505 | 4.3526 | 0.0123 | 0.9657 | 0.0343 | 0.0011 |
| Age at enrollment | 4.5316 | 0.0015 | 0.9654 | 0.0346 | -0.0003 |
| Waist-to-hip ratio | 5.0664 | 0.0000 | 0.9650 | 0.0350 | -0.0005 |
| RGS6 rs2239222 | 5.0824 | 0.0017 | 0.9642 | 0.0358 | -0.0007 |
| HNF1A rs11065385 | 5.0992 | 0.0041 | 0.9642 | 0.0358 | 0.0000 |
| Duration of E+P use | 5.1748 | 0.0009 | 0.9647 | 0.0353 | 0.0005 |
| Age at menopause | 5.3086 | 0.0003 | 0.9658 | 0.0342 | 0.0011 |
| HNF1A-AS1 rs2251468 | 5.3192 | 0.0057 | 0.9652 | 0.0348 | -0.0006 |
| Hip circumference | 5.3238 | -0.0001 | 0.9647 | 0.0353 | -0.0005 |
| Height | 5.4572 | -0.0001 | 0.9641 | 0.0359 | -0.0006 |
| Education | 5.5004 | -0.0002 | 0.9634 | 0.0366 | -0.0007 |
| Waist circumference | 5.5066 | -0.0002 | 0.9629 | 0.0371 | -0.0005 |
| BMI | 5.6638 | -0.0001 | 0.9627 | 0.0373 | -0.0002 |
| Total months of breastfeeding | 5.6970 | 0.0003 | 0.9621 | 0.0379 | -0.0006 |
| HNF1A-AS1 rs7953249 | 5.7660 | 0.0060 | 0.9618 | 0.0382 | -0.0004 |
| Weight | 5.8404 | -0.0001 | 0.9622 | 0.0378 | 0.0005 |
| HNF1A-AS1 rs10774579 | 6.3998 | 0.0037 | 0.9623 | 0.0377 | 0.0001 |
| HNF1A-AS1 rs1920792 | 6.4012 | 0.0037 | 0.9624 | 0.0376 | 0.0001 |
| HNF1A rs1169301 | 8.0714 | 0.0010 | 0.9617 | 0.0383 | -0.0007 |
| HNF1A rs1169300 | 8.1956 | 0.0010 | 0.9616 | 0.0384 | -0.0001 |
BMI, body mass index; C-index, concordance index; E+P, exogenous estrogen + progestin; VIMP, variable of importance.
Variables are ordered by minimal depth.
Predictive value of variable was assessed via minimal depth in the nested random survival forest models.
A lower value is likely to have a greater impact on prediction.
The incremental error rate of each variable was estimated in the nested sequence of models starting with the top variable, followed by the model with the top 2 variables, then the model with the top 3 variables, and so on.
For example, the third error rate was estimated from the third nested model (including the first, second, and third variables).
The drop error rate was estimated by the difference between the error rates from the nested models with a prior and the corresponding variable.
For example, the drop error rate of the second variable was estimated by the difference between the error rates from the first and second nested models. The error rate for the null model is set at 0.5; thus, the drop error rate for the first variable was obtained by subtracting the error rate (0.3449) from 0.5.
Figure 2.
Overall analysis: the second stage of random survival forest (RSF) analysis with 18 single-nucleotide polymorphisms and 12 behavioral factors selected from the first stage of RSF. A. Comparison of minimal depth and VIMP rankings. (BMI, body mass index; E+P, exogenous estrogen + progestin; VIMP, variable of importance. Note: The 3 variables within the gold ellipse were identified as the most influential predictors. B. Out-of-bag concordance index (C-index). (Improvement in the out-of-bag C-index was observed when the top 3 variables [●] were added to the model, whereas other variables [○] did not further improve the accuracy of prediction).
We continued to apply those 2-stage multimodal RSF (Tables S3A, S3B, S3C, S3D, S3E, S3F, S3G, S3H, S3I, S3J and Figures S4, S5, S6, S7, S8) and GMDR (Table S2) methods to each of the obesity strata (BMI, WHR, WST, MET, and SFA), and throughout the strata, determined the same top 3 variables detected from the overall analysis as the best predictive markers, except in the viscerally obese subgroup (WHR > 0.85), in which only 1 SNP (ONECUT2 rs4092465) was identified as the best marker.
Combined and joint effects of the most predictive SNPs and lifestyle factor on CRC risk
Using the RSF model, we accounted for confounding factors and the nonlinearity of each variable and estimated the cumulative incidence rate of CRC (Figure 3). For the purpose of study analysis, we used this non-linear adjusted incidence rate to categorize the genotypes of each SNP that were originally continuous variables with the following risk genotypes (Figure 3A-C): CRP rs1800947 GG, ONECUT2 rs4092465 GA, and HNF4A rs1800961 TT. Also, by using a cutoff-value diverging incidence rate of a variable (Figure 3D), we defined a high-risk lifestyle group as having < 5 years of past OC use, and further analyzed that as a binary variable. With the most predictive GMDR-modeled SNPs and risk lifestyle overall and in the obesity strata, we developed multivariate models predicting CRC risk (Tables S4A and S4B); the results indicated a stronger individual effect of 1 SNP (ONECUT2 rs4092465 GA) than the other SNP and the risk lifestyle on CRC risk across the strata, even after adjusting for confounding factors.
Figure 3.
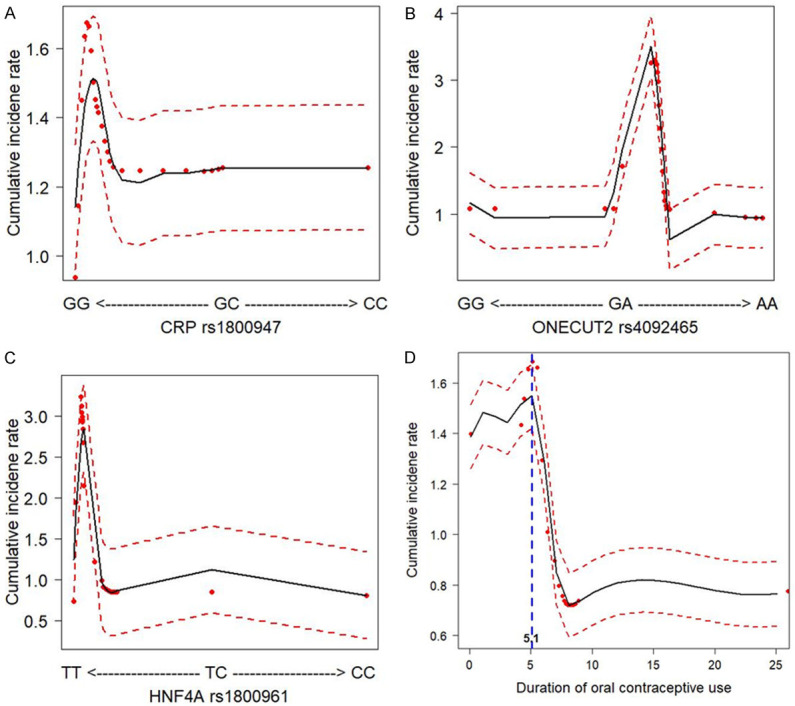
Cumulative colorectal cancer incidence rate for the 4 most influential variables (3 SNPs and 1 behavioral factor) based on random survival forest analyses. (SNPs, single-nucleotide polymorphisms. Dashed red lines indicate 95% confidence intervals).
The 2 top SNPs and the top risk lifestyle yielded different patterns when tested in combination or jointly for the association with CRC risk. For example, in the overall analysis, the top 2 SNPs were combined with the top risk lifestyle (< 5 years of past OC use) (Table 3). Compared with the lowest-risk group (i.e., low risk for genotypes and lifestyle), the moderate-risk (i.e., high risk of either genotypes or lifestyle) and the highest-risk groups (i.e., high risk of both genotypes and lifestyle) had about 4 times and 17 times the excessive risk, respectively, suggesting a gene-lifestyle dose-response relationship (Table 3). Next, we tested for the joint effect of past OC use with the risk genotypes of the 2 SNPs on CRC risk (Table 4). When the 2 SNPs were combined, their effect on CRC risk was not much different from the individual effect of ONECUT2 rs4092465. However, when stratified by past OC use, the shorter-duration users (high risk: < 5.1 years) with the 2 risk alleles had 3 times higher risk for CRC than the longer-duration users (low risk: ≥ 5 years) with the same 2 risk alleles, and further, 17 times greater risk than the longer-duration users with null or 1 risk allele. This indicates a significant joint effect of past OC use with the risk genotypes on CRC risk in both additive and multiplicative interaction models (G×E: HR=1.98, P=0.003). Multiple testing corrections were made to control the false-discovery rate. In the BMI strata (Tables 3 and 4), the non-overall obese group yielded similar results to those from the overall analysis, but the overall-obese group displayed stronger combined and joint effects of the risk genotypes and past OC use in both additive and multiplicative models (G×E: HR=1.54, P=0.332); these results suggest the potential existence of the BMI-modified inflammatory gene-lifestyle pathway predicting CRC risk.
Table 3.
Combined effect of past OC use and risk genotypes (ONECUT2 rs4092465 GA; HNF4A rs1800961 TT) on CRC risk overall and in BMI strata
| n£ | Risk genotype + past OC use | ||
|---|---|---|---|
|
| |||
| Total n | HR† (95% CI) | p * | |
| <Overall group> | |||
| 0 | 3,559 | reference | |
| 1 | 4,949 | 4.40 (3.32-5.83) | < 2e-16 |
| 2 | 1,634 | 17.54 (13.22-23.28) | < 2e-16 |
| p trend | < 2e-16 | ||
| <Non-overall obese group, BMI < 30 kg/m2 (n=7,151)> | |||
| 0 | 2,594 | reference | |
| 1 | 3,501 | 4.23 (3.08-5.82) | < 2e-16 |
| 2 | 1,056 | 17.41 (12.62-24.02) | < 2e-16 |
| p trend | < 2e-16 | ||
| <Overall obese group, BMI ≥ 30 kg/m2 (n=2,991)> | |||
| 0 | 965 | reference | |
| 1 | 1,448 | 5.08 (2.77-9.30) | 1.37e-07 |
| 2 | 578 | 19.96 (10.91-36.51) | < 2e-16 |
| p trend | < 2e-16 | ||
BMI, body mass index; CI, confidence interval; CRC, colorectal cancer; HR, hazard ratio; OC, oral contraceptive. Numbers in bold face are statistically significant.
The combined number of risk genotypes and behavioral factors was based on 1) risk genotypes defined as 0 (low risk: none or 1 risk allele) and 1 (high risk: 2 risk alleles) and 2) behavioral factors defined as 0 (low risk: past OC use ≥ 5.1 years) and 1 (high risk: past OC use < 5.1 years).
The ultimate number of combined risk genotypes and behavioral factors was defined as 0 (low risk for genotypes and behaviors), 1 (high risk for either genotypes or behaviors), and 2 (high risk for both genotypes and behaviors).
Multivariate regression was adjusted by age at enrollment, education, BMI (in overall group), height and weight (in BMI strata), waist-to-hip ratio, age at menopause, total months of breastfeeding, and exogenous estrogen plus progestin.
p values were adjusted to correct for multiple testing via the Benjamini-Hochberg approach.
Table 4.
Joint effect of past OC use with risk genotypes (ONECUT2 rs4092465 GA; HNF4A rs1800961 TT) on CRC risk overall and in BMI strata
| n | Total | Past OC use ≥ 5.1 years | Past OC use < 5.1 years | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| HR† (95% CI) | p* | n | HR† (95% CI) | p * | n | HR† (95% CI) | p * | |
| <Overall group> | ||||||||
| Risk genotypes£ | ||||||||
| 0 | reference | 3,559 | reference | 1,492 | 1.59 (1.04-2.43) | 0.03415 | ||
| 1 | 7.39 (5.93-9.20) | < 2e-16 | 3,457 | 5.46 (4.11-7.25) | < 2e-16 | 1,634 | 17.15 (12.92-22.76) | < 2e-16 |
| p trend | < 2e-16 | |||||||
| <Non-overall obese group, BMI < 30 kg/m2 (n=7,151)> | ||||||||
| Risk genotypes£ | ||||||||
| 0 | reference | 2,594 | reference | 946 | 1.52 (0.92-2.53) | 0.10148 | ||
| 1 | 7.07 (5.48-9.12) | < 2e-16 | 2,555 | 5.14 (3.73-7.07) | < 2e-16 | 1,056 | 17.05 (12.36-23.53) | < 2e-16 |
| p trend | < 2e-16 | |||||||
| <Overall obese group, BMI ≥ 30 kg/m2 (n=2,991)> | ||||||||
| Risk genotypes£ | ||||||||
| 0 | reference | 965 | reference | 546 | 1.89 (0.83-4.30) | 0.12766 | ||
| 1 | 8.40 (5.43-12.97) | < 2e-16 | 902 | 6.69 (3.64-12.31) | 1e-09 | 578 | 19.50 (10.66-35.68) | < 2e-16 |
| p trend | < 2e-16 | |||||||
BMI, body mass index; CI, confidence interval; CRC, colorectal cancer; HR, hazard ratio; OC, oral contraceptive. Numbers in bold face are statistically significant.
Multivariate regression was adjusted by age at enrollment, education, BMI (in overall group), height and weight (in BMI strata), waist-to-hip ratio, age at menopause, total months of breastfeeding, OC use (in total analysis), and exogenous estrogen plus progestin.
p values were adjusted to correct for multiple testing via the Benjamini-Hochberg approach.
The number of risk genotypes was defined on the basis of Kaplan-Meier analysis as follows: 0 (none or 1 risk allele) and 1 (2 risk alleles).
Further, we examined the combined and joint effects of past OC use with the risk genotypes on CRC risk in the other obesity strata, and determined that the risk genotypes in combination (Table S5) or jointly (Table S6) associated with OC use displayed a synergistic effect on CRC risk; particularly in the METs strata, the gene-lifestyle combined and joint effect on cancer appeared more strongly in the physically inactive group (Figure 4).
Figure 4.
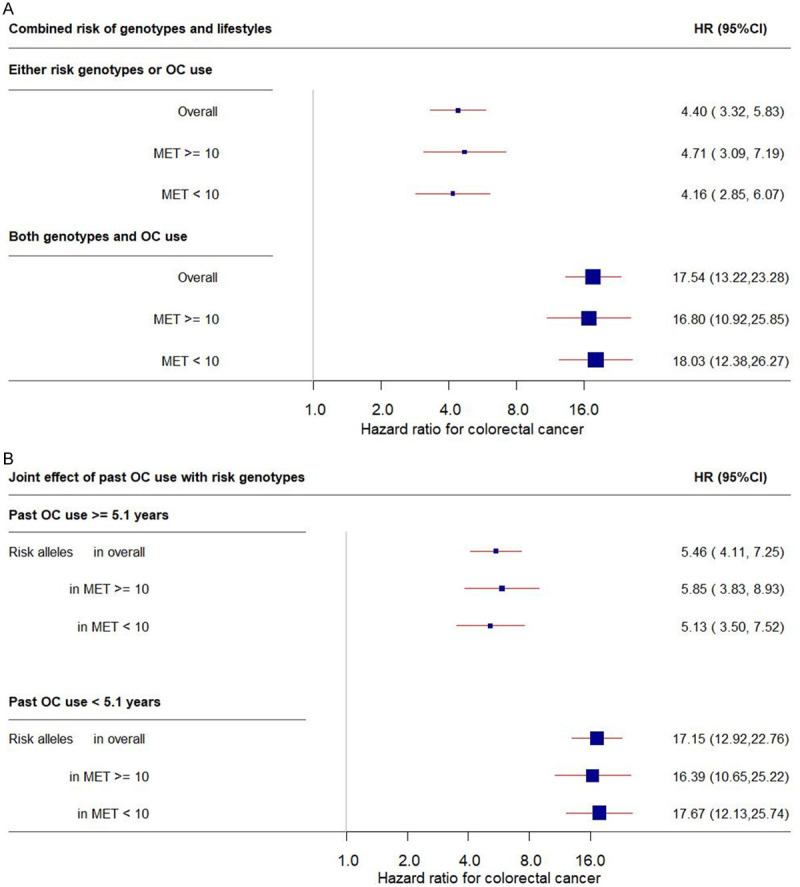
Forest plot of the combined (A) and joint (B) effect of past OC use and risk genotypes on CRC risk overall and in MET subgroups. Plot (A) shows the independent and combined effect of risk genotypes and OC use on CRC risk, and Plot (B) shows the joint tests for risk genotypes with OC use, presented as the 95% CIs (indicated with red lines) and the estimates (proportional to the size of the blue squares). The analyzed risk genotypes included ONECUT2 rs4092465 GA and HNF4A rs1800961 TT. (CI, confidence interval; CRC, colorectal cancer; HR, hazard ratio; MET, metabolic equivalent; OC, oral contraceptive).
Discussion
An increasing number of population-based human genomic studies have incorporated environmental factors in cancer molecular causal pathways. Elucidating the role of lifestyle factors in modifying the gene and phenotype association, thus influencing the risk of CRC, may improve the predictability for CRC and facilitate the development of personalized genetically targeted lifestyle interventions for primary cancer prevention efforts. Our multimodal RSF and GMDR approaches determined the best genetic markers in inflammatory cytokines and the best risk lifestyle predictive for CRC development. The most common predictors across the obesity strata are 2 SNPs (ONECUT2 rs4092465 and HNF4A rs1800961) and 1 lifestyle factor (relatively short-term past use of OC). The risk profiles that combined those genetic and lifestyle markers exhibited a synergistically increased risk for CRC, and this pattern appeared more strongly in obese subgroups.
ONECUT2 encodes the second member of the ONECUT family of DNA-binding transcription factors, characterized by a single cut domain and a specific homeodomain, and its phenotypes have been linked to CRP and stroke [72,73]. ONECUT2, as an angiogenic and epithelial-mesenchymal transition (EMT) marker, plays a key role in the oncogenesis of several cancers, including hepatocellular carcinoma (HCC) [74] and ovarian [73], breast [75], and prostate cancers [76]. With regard to CRC, ONECUT2 is involved in the EMT and the migration and invasion of CRC cells, and it acts as a tumor promoter [77], although the colorectal carcinogenic mechanism is not fully determined. Our genomic study initially detected 1 SNP near ONECUT2 for the association with CRP at the GWA level and its strong association with CRC risk, suggesting the effect of the genetic aberration in this transcription factor on colorectal tumorigenesis. Notably, the effect of this SNP on CRC risk appeared much stronger when it was combined and jointly interacted with the cumulative exposure to estrogen, warranting future biologic mechanism study on the inflammatory-sex hormone interaction in colorectal carcinogenesis.
HNF4A encodes hepatocyte nuclear factor 4 alpha, a nuclear transcription factor that controls the expression of other genes such as HNF1A, and it plays a role in the maturation of liver, kidney, and intestine [78,79]. Its phenotypes include CRP [32,45,80,81] and high-density lipoprotein [82], and mutations in this gene have been associated with maturity-onset diabetes of the young type 1, type 2 diabetes, ulcerative colitis, and Crohn’s disease [82,83]. HNF4A expression has antitumor activity in several cancer cell lines, such as lung carcinoma [84,85], head and neck squamous cell carcinoma [86], esophageal adenocarcinoma [87], and HCC [88,89]. Also, the ectopic expression of HNF4A inhibited CRC cells’ proliferation, invasion, and migration by G2/M cell-phase arrest and promoted apoptosis through its effect on the Wnt/B-catenin signaling pathway [90]. Further, HNF4A protects the intestinal mucosa against inflammation by blocking the IL6R/STAT3 pathway [83]. Therefore, downregulation of HNF4A expression is crucial in the aggravation of CRC. As supported by these previous studies, the minor allele of the HNF4A SNP in our study, both individually and in combination with the ONECUT2 SNP, presented a strong effect on increased risk for CRC. Further, considering the positive correlation between the HNF4A genetic score and BMI [91], our finding of the greater impact of the SNPs on CRC risk in the BMI-obese and MET-inactive subgroups is biologically compelling. Additionally, among obese or diabetic individuals (i.e., those with chronic low-grade inflammatory diseases), HNF4A has hepatic cross-talk with sex hormones such as sex hormone-binding globulin [92,93], potentially influencing cancer initiation and progress, although the underlying mechanism is uncertain. Our study indicates that the HNF4A/ONECUT2 SNPs combined with past OC use synergistically increase CRC risk, and that this pattern is more profound in obese subgroups; this may provide a scientific basis for future mechanistic study.
Lifetime cumulative exposure to estrogen, particularly past use of OC in postmenopausal women, has been considered a protective factor for CRC risk, as shown in in vivo and in vitro studies reporting that estrogen upregulates a p53 cell-cycle regulator, leading to the inhibition of CRC cell growth [94,95]. Our RSF-based estimation of the CRC cumulative incidence rate for OC use accounted for its nonlinearity, showing that cancer risk increased with up to 5 years of OC use but dropped thereafter. The past use of OC, when combined with inflammatory SNPs, increased cancer risk in a gene-lifestyle dose response-associated manner, implying the existence of inflammatory-sex hormone cross-talk in colorectal carcinogenesis.
In the early 1980s, OC formulations had high estrogen concentration, but that has since been changed [96]. We did not have data available on OC types. Because CRC risk can be dependent on different OC preparations, our study should be further validated with data incorporating information on OC estrogen concentration. We also had no data on CRC molecular subtypes, warranting future independent studies with data on the tumor molecular features. Further, our study population was restricted to non-Hispanic white postmenopausal women, so our findings should not be generalized to other populations. Despite the strong benefits from the 2-stage multimodal approaches, they are noisy tasks, leading to the over-fit model in small subgroups; thus, a replication study with a large sample size is requested.
In this study, the GWA SNPs in pro-inflammatory cytokines exhibit synergistically increased risk for CRC in combination with lifetime cumulative exposure to estrogen and this pattern is more profound in obese/inactive subgroups. Our results call for molecular studies to examine inflammatory gene signatures and their expressions aberrantly presenting in their downstream signaling pathways in relation to CRC by incorporating the effect of estrogen and obesity. Our study may contribute to an improved prediction ability for CRC risk and suggest genetically targeted lifestyle interventions for women carrying the inflammatory-risk genotypes, thus reducing CRC risk.
Acknowledgements
This study was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number K01NR017852 and a University of California Cancer Research Coordinating Committee grant (CRN-18-522722). The data for this project were provided by the WHI program, which is funded by the National Heart, Lung, and Blood Institute, the National Institutes of Health, and the U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C. The datasets used for the analyses described in this manuscript were obtained from dbGaP at http://www.ncbi.nlm.nih.gov/sites/entrez?db=gap through dbGaP accession (phs000200.v11.p3).
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Disis ML. Immune regulation of cancer. J. Clin. Oncol. 2010;28:4531–4538. doi: 10.1200/JCO.2009.27.2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Cancer Society. Colorectal Cancer Facts & Figures 2017-2019. Atlanta: American Cancer Society, Inc.; 2017. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2017-2019.pdf. [Google Scholar]
- 4.American Cancer Society. Cancer Fact and Figures, 2020. Atlanta: American Cancer Society, Inc.; https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf. [Google Scholar]
- 5.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 6.Pohl C, Hombach A, Kruis W. Chronic inflammatory bowel disease and cancer. Hepatogastroenterology. 2000;47:57–70. [PubMed] [Google Scholar]
- 7.Erlinger TP, Platz EA, Rifai N, Helzlsouer KJ. C-reactive protein and the risk of incident colorectal cancer. JAMA. 2004;291:585–590. doi: 10.1001/jama.291.5.585. [DOI] [PubMed] [Google Scholar]
- 8.Prizment AE, Anderson KE, Visvanathan K, Folsom AR. Association of inflammatory markers with colorectal cancer incidence in the atherosclerosis risk in communities study. Cancer Epidemiol Biomarkers Prev. 2011;20:297–307. doi: 10.1158/1055-9965.EPI-10-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toriola AT, Cheng TY, Neuhouser ML, Wener MH, Zheng Y, Brown E, Miller JW, Song X, Beresford SA, Gunter MJ, Caudill MA, Ulrich CM. Biomarkers of inflammation are associated with colorectal cancer risk in women but are not suitable as early detection markers. Int J Cancer. 2013;132:2648–2658. doi: 10.1002/ijc.27942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ho GY, Wang T, Gunter MJ, Strickler HD, Cushman M, Kaplan RC, Wassertheil-Smoller S, Xue X, Rajpathak SN, Chlebowski RT, Vitolins MZ, Scherer PE, Rohan TE. Adipokines linking obesity with colorectal cancer risk in postmenopausal women. Cancer Res. 2012;72:3029–3037. doi: 10.1158/0008-5472.CAN-11-2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ho GY, Wang T, Zheng SL, Tinker L, Xu J, Rohan TE, Wassertheil-Smoller S, Xue X, Augenlicht LH, Peters U, Phipps AI, Strickler HD, Gunter MJ, Cushman M. Circulating soluble cytokine receptors and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 2014;23:179–88. doi: 10.1158/1055-9965.EPI-13-0545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghazi-Khanloosani M, Bandegi AR, Kokhaei P, Barati M, Pakdel A. CRP and LOX-1: a mechanism for increasing the tumorigenic potential of colorectal cancer carcinoma cell line. Pathol Oncol Res. 2019;25:1467–1475. doi: 10.1007/s12253-018-0507-4. [DOI] [PubMed] [Google Scholar]
- 13.Cui G, Yuan A, Sun Z, Zheng W, Pang Z. IL-1beta/IL-6 network in the tumor microenvironment of human colorectal cancer. Pathol Res Pract. 2018;214:986–992. doi: 10.1016/j.prp.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 14.Liu L, Tabung FK, Zhang X, Nowak JA, Qian ZR, Hamada T, Nevo D, Bullman S, Mima K, Kosumi K, da Silva A, Song M, Cao Y, Twombly TS, Shi Y, Liu H, Gu M, Koh H, Li W, Du C, Chen Y, Li C, Li W, Mehta RS, Wu K, Wang M, Kostic AD, Giannakis M, Garrett WS, Hutthenhower C, Chan AT, Fuchs CS, Nishihara R, Ogino S, Giovannucci EL. Diets that promote colon inflammation associate with risk of colorectal carcinomas that contain fusobacterium nucleatum. Clin Gastroenterol Hepatol. 2018;16:1622–1631. e3. doi: 10.1016/j.cgh.2018.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Yu X, Yu E, Wang N, Cai Q, Shuai Q, Yan F, Jiang L, Wang H, Liu J, Chen Y, Li Z, Jiang Q. Changes in gut microbiota and plasma inflammatory factors across the stages of colorectal tumorigenesis: a case-control study. BMC Microbiol. 2018;18:92. doi: 10.1186/s12866-018-1232-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Proença MA, Biselli JM, Succi M, Severino FE, Berardinelli GN, Caetano A, Reis RM, Hughes DJ, Silva AE. Relationship between Fusobacterium nucleatum, inflammatory mediators and microRNAs in colorectal carcinogenesis. World J Gastroenterol. 2018;24:5351–5365. doi: 10.3748/wjg.v24.i47.5351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castellano-Castillo D, Morcillo S, Clemente-Postigo M, Crujeiras AB, Fernandez-Garcia JC, Torres E, Tinahones FJ, Macias-Gonzalez M. Adipose tissue inflammation and VDR expression and methylation in colorectal cancer. Clin Epigenetics. 2018;10:60. doi: 10.1186/s13148-018-0493-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Himbert C, Ose J, Nattenmüller J, Warby CA, Holowatyj AN, Böhm J, Lin T, Haffa M, Gigic B, Hardikar S, Scherer D, Zielske L, Schrotz-King P, Kölsch T, Siegel EM, Shibata D, Ulrich A, Schneider M, Hursting SD, Kauczor HU, Ulrich CM. Body fatness, adipose tissue compartments, and biomarkers of inflammation and angiogenesis in colorectal cancer: the colocare study. Cancer Epidemiol Biomarkers Prev. 2019;28:76–82. doi: 10.1158/1055-9965.EPI-18-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfalzer AC, Leung K, Crott JW, Kim SJ, Tai AK, Parnell LD, Kamanu FK, Liu Z, Rogers G, Shea MK, Garcia PE, Mason JB. Incremental elevations in TNFalpha and IL6 in the human colon and procancerous changes in the mucosal transcriptome accompany adiposity. Cancer Epidemiol Biomarkers Prev. 2018;27:1416–1423. doi: 10.1158/1055-9965.EPI-18-0121. [DOI] [PubMed] [Google Scholar]
- 20.Fang D, Ye Y. C-reactive protein gene rs1205 polymorphism is not associated with the risk of colorectal cancer. Biosci Rep. 2017;37:BSR20170872. doi: 10.1042/BSR20170872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang BZ, Tsilidis KK, Smith MW, Hoffman-Bolton J, Visvanathan K, Platz EA, Joshu CE. Polymorphisms in genes related to inflammation and obesity and colorectal adenoma risk. Mol Carcinog. 2018;57:1278–1288. doi: 10.1002/mc.22842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu JJ, Wang ZT, Zhong J. Lack of association between the interleukin 6 gene -174G>C polymorphism and colorectal cancer: evidence from a meta-analysis. Genet Mol Res. 2013;12:2205–14. doi: 10.4238/2013.July.8.2. [DOI] [PubMed] [Google Scholar]
- 23.Banday MZ, Balkhi HM, Sameer AS, Chowdri NA, Haq E. Strong association of interleukin-6 -174G/C promoter single nucleotide polymorphism with a decreased risk of colorectal cancer in ethnic Kashmiri population: a case control study. Tumour Biol. 2017;39:1010428317695940. doi: 10.1177/1010428317695940. [DOI] [PubMed] [Google Scholar]
- 24.Landi S, Moreno V, Gioia-Patricola L, Guino E, Navarro M, de Oca J, Capella G, Canzian F Bellvitge Colorectal Cancer Study Group. Association of common polymorphisms in inflammatory genes interleukin (IL)6, IL8, tumor necrosis factor alpha, NFKB1, and peroxisome proliferator-activated receptor gamma with colorectal cancer. Cancer Res. 2003;63:3560–3566. [PubMed] [Google Scholar]
- 25.Wang X, Dai JY, Albanes D, Arndt V, Berndt SI, Bézieau S, Brenner H, Buchanan DD, Butterbach K, Caan B, Casey G, Campbell PT, Chan AT, Chen Z, Chang-Claude J, Cotterchio M, Easton DF, Giles GG, Giovannucci E, Grady WM, Hoffmeister M, Hopper JL, Hsu L, Jenkins MA, Joshi AD, Lampe JW, Larsson SC, Lejbkowicz F, Li L, Lindblom A, Le Marchand L, Martin V, Milne RL, Moreno V, Newcomb PA, Offitt K, Ogino S, Pharoah PDP, Pinchev M, Potter JD, Rennert HS, Rennert G, Saliba W, Schafmayer C, Schoen RE, Schrotz-King P, Slattery ML, Song M, Stegmaier C, Weinstein SJ, Wolk A, Woods MO, Wu AH, Gruber SB, Peters U, White E. Mendelian randomization analysis of C-reactive protein on colorectal cancer risk. Int J Epidemiol. 2019;48:767–780. doi: 10.1093/ije/dyy244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amaral WZ, Krueger RF, Ryff CD, Coe CL. Genetic and environmental determinants of population variation in interleukin-6, its soluble receptor and C-reactive protein: insights from identical and fraternal twins. Brain Behav Immun. 2015;49:171–181. doi: 10.1016/j.bbi.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fried SK, Bunkin DA, Greenberg AS. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: depot difference and regulation by glucocorticoid. J Clin Endocrinol Metab. 1998;83:847–850. doi: 10.1210/jcem.83.3.4660. [DOI] [PubMed] [Google Scholar]
- 28.Ligthart S, Vaez A, Võsa U, Stathopoulou MG, Ligthart S, Vaez A, Võsa U, Stathopoulou MG, de Vries PS, Prins BP, Van der Most PJ, Tanaka T, Naderi E, Rose LM, Wu Y, Karlsson R, Barbalic M, Lin H, Pool R, Zhu G, Macé A, Sidore C, Trompet S, Mangino M, Sabater-Lleal M, Kemp JP, Abbasi A, Kacprowski T, Verweij N, Smith AV, Huang T, Marzi C, Feitosa MF, Lohman KK, Kleber ME, Milaneschi Y, Mueller C, Huq M, Vlachopoulou E, Lyytikäinen LP, Oldmeadow C, Deelen J, Perola M, Zhao JH, Feenstra B LifeLines Cohort Study; Amini M CHARGE Inflammation Working Group. Lahti J, Schraut KE, Fornage M, Suktitipat B, Chen WM, Li X, Nutile T, Malerba G, Luan J, Bak T, Schork N, Del Greco M F, Thiering E, Mahajan A, Marioni RE, Mihailov E, Eriksson J, Ozel AB, Zhang W, Nethander M, Cheng YC, Aslibekyan S, Ang W, Gandin I, Yengo L, Portas L, Kooperberg C, Hofer E, Rajan KB, Schurmann C, den Hollander W, Ahluwalia TS, Zhao J, Draisma HHM, Ford I, Timpson N, Teumer A, Huang H, Wahl S, Liu Y, Huang J, Uh HW, Geller F, Joshi PK, Yanek LR, Trabetti E, Lehne B, Vozzi D, Verbanck M, Biino G, Saba Y, Meulenbelt I, O’Connell JR, Laakso M, Giulianini F, Magnusson PKE, Ballantyne CM, Hottenga JJ, Montgomery GW, Rivadineira F, Rueedi R, Steri M, Herzig KH, Stott DJ, Menni C, Frånberg M, St Pourcain B, Felix SB, Pers TH, Bakker SJL, Kraft P, Peters A, Vaidya D, Delgado G, Smit JH, Großmann V, Sinisalo J, Seppälä I, Williams SR, Holliday EG, Moed M, Langenberg C, Räikkönen K, Ding J, Campbell H, Sale MM, Chen YI, James AL, Ruggiero D, Soranzo N, Hartman CA, Smith EN, Berenson GS, Fuchsberger C, Hernandez D, Tiesler CMT, Giedraitis V, Liewald D, Fischer K, Mellström D, Larsson A, Wang Y, Scott WR, Lorentzon M, Beilby J, Ryan KA, Pennell CE, Vuckovic D, Balkau B, Concas MP, Schmidt R, Mendes de Leon CF, Bottinger EP, Kloppenburg M, Paternoster L, Boehnke M, Musk AW, Willemsen G, Evans DM, Madden PAF, Kähönen M, Kutalik Z, Zoledziewska M, Karhunen V, Kritchevsky SB, Sattar N, Lachance G, Clarke R, Harris TB, Raitakari OT, Attia JR, van Heemst D, Kajantie E, Sorice R, Gambaro G, Scott RA, Hicks AA, Ferrucci L, Standl M, Lindgren CM, Starr JM, Karlsson M, Lind L, Li JZ, Chambers JC, Mori TA, de Geus EJCN, Heath AC, Martin NG, Auvinen J, Buckley BM, de Craen AJM, Waldenberger M, Strauch K, Meitinger T, Scott RJ, McEvoy M, Beekman M, Bombieri C, Ridker PM, Mohlke KL, Pedersen NL, Morrison AC, Boomsma DI, Whitfield JB, Strachan DP, Hofman A, Vollenweider P, Cucca F, Jarvelin MR, Jukema JW, Spector TD, Hamsten A, Zeller T, Uitterlinden AG, Nauck M, Gudnason V, Qi L, Grallert H, Borecki IB, Rotter JI, März W, Wild PS, Lokki ML, Boyle M, Salomaa V, Melbye M, Eriksson JG, Wilson JF, Penninx BWJH, Becker DM, Worrall BB, Gibson G, Krauss RM, Ciullo M, Zaza G, Wareham NJ, Oldehinkel AJ, Palmer LJ, Murray SS, Pramstaller PP, Bandinelli S, Heinrich J, Ingelsson E, Deary IJ, Mägi R, Vandenput L, van der Harst P, Desch KC, Kooner JS, Ohlsson C, Hayward C, Lehtimäki T, Shuldiner AR, Arnett DK, Beilin LJ, Robino A, Froguel P, Pirastu M, Jess T, Koenig W, Loos RJF, Evans DA, Schmidt H, Smith GD, Slagboom PE, Eiriksdottir G, Morris AP, Psaty BM, Tracy RP, Nolte IM, Boerwinkle E, Visvikis-Siest S, Reiner AP, Gross M, Bis JC, Franke L, Franco OH, Benjamin EJ, Chasman DI, Dupuis J, Snieder H, Dehghan A, Alizadeh BZ. Genome analyses of >200,000 individuals identify 58 loci for chronic inflammation and highlight pathways that link inflammation and complex disorders. Am J Hum Genet. 2018;103:691–706. doi: 10.1016/j.ajhg.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dehghan A, Dupuis J, Barbalic M, Bis JC, Eiriksdottir G, Lu C, Pellikka N, Wallaschofski H, Kettunen J, Henneman P, Baumert J, Strachan DP, Fuchsberger C, Vitart V, Wilson JF, Paré G, Naitza S, Rudock ME, Surakka I, de Geus EJ, Alizadeh BZ, Guralnik J, Shuldiner A, Tanaka T, Zee RY, Schnabel RB, Nambi V, Kavousi M, Ripatti S, Nauck M, Smith NL, Smith AV, Sundvall J, Scheet P, Liu Y, Ruokonen A, Rose LM, Larson MG, Hoogeveen RC, Freimer NB, Teumer A, Tracy RP, Launer LJ, Buring JE, Yamamoto JF, Folsom AR, Sijbrands EJ, Pankow J, Elliott P, Keaney JF, Sun W, Sarin AP, Fontes JD, Badola S, Astor BC, Hofman A, Pouta A, Werdan K, Greiser KH, Kuss O, Meyer zu Schwabedissen HE, Thiery J, Jamshidi Y, Nolte IM, Soranzo N, Spector TD, Völzke H, Parker AN, Aspelund T, Bates D, Young L, Tsui K, Siscovick DS, Guo X, Rotter JI, Uda M, Schlessinger D, Rudan I, Hicks AA, Penninx BW, Thorand B, Gieger C, Coresh J, Willemsen G, Harris TB, Uitterlinden AG, Järvelin MR, Rice K, Radke D, Salomaa V, Willems van Dijk K, Boerwinkle E, Vasan RS, Ferrucci L, Gibson QD, Bandinelli S, Snieder H, Boomsma DI, Xiao X, Campbell H, Hayward C, Pramstaller PP, van Duijn CM, Peltonen L, Psaty BM, Gudnason V, Ridker PM, Homuth G, Koenig W, Ballantyne CM, Witteman JC, Benjamin EJ, Perola M, Chasman DI. Meta-analysis of genome-wide association studies in >80 000 subjects identifies multiple loci for C-reactive protein levels. Circulation. 2011;123:731–738. doi: 10.1161/CIRCULATIONAHA.110.948570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doumatey AP, Chen G, Tekola Ayele F, Zhou J, Erdos M, Shriner D, Huang H, Adeleye J, Balogun W, Fasanmade O, Johnson T, Oli J, Okafor G, Amoah A, Eghan BA, Agyenim-Boateng K, Acheampong J, Adebamowo C, Gerry NP, Christman MF, Adeyemo A, Rotimi CN. C-reactive protein (CRP) promoter polymorphisms influence circulating CRP levels in a genome-wide association study of African Americans. Hum Mol Genet. 2012;21:3063–3072. doi: 10.1093/hmg/dds133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ridker PM, Pare G, Parker A, Zee RY, Danik JS, Buring JE, Kwiatkowski D, Cook NR, Miletich JP, Chasman DI. Loci related to metabolic-syndrome pathways including LEPR, HNF1A, IL6R, and GCKR associate with plasma C-reactive protein: the women’s genome health study. Am J Hum Genet. 2008;82:1185–1192. doi: 10.1016/j.ajhg.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reiner AP, Beleza S, Franceschini N, Auer PL, Robinson JG, Kooperberg C, Peters U, Tang H. Genome-wide association and population genetic analysis of C-reactive protein in African American and Hispanic American women. Am J Hum Genet. 2012;91:502–512. doi: 10.1016/j.ajhg.2012.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prizment AE, Folsom AR, Dreyfus J, Anderson KE, Visvanathan K, Joshu CE, Platz EA, Pankow JS. Plasma C-reactive protein, genetic risk score, and risk of common cancers in the atherosclerosis risk in communities study. Cancer Causes Control. 2013;24:2077–2087. doi: 10.1007/s10552-013-0285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu M, Lee MH, Mak VW, Tomlinson B. Effect of central obesity, low high-density lipoprotein cholesterol and C-reactive protein polymorphisms on C-reactive protein levels during treatment with Rosuvastatin (10 mg Daily) Am J Cardiol. 2010;106:1588–1593. doi: 10.1016/j.amjcard.2010.07.044. [DOI] [PubMed] [Google Scholar]
- 35.Wu S, Hsu LA, Teng MS, Lin JF, Chou HH, Lee MC, Wu YM, Su CW, Ko YL. Interactive effects of C-reactive protein levels on the association between APOE variants and triglyceride levels in a Taiwanese population. Lipids Health Dis. 2016;15:94. doi: 10.1186/s12944-016-0262-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fraser A, May M, Lowe G, Rumley A, Smith GD, Ebrahim S, Lawlor DA. Interleukin-6 and incident coronary heart disease: results from the British Women’s Heart and Health Study. Atherosclerosis. 2009;202:567–572. doi: 10.1016/j.atherosclerosis.2008.04.048. [DOI] [PubMed] [Google Scholar]
- 37.Winters-Stone KM, Wood LJ, Stoyles S, Dieckmann NF. The effects of resistance exercise on biomarkers of breast cancer prognosis: a pooled analysis of three randomized trials. Cancer Epidemiol Biomarkers Prev. 2018;27:146–153. doi: 10.1158/1055-9965.EPI-17-0766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lynch BM, Friedenreich CM, Winkler EA, Healy GN, Vallance JK, Eakin EG, Owen N. Associations of objectively assessed physical activity and sedentary time with biomarkers of breast cancer risk in postmenopausal women: findings from NHANES (2003-2006) Breast Cancer Res Treat. 2011;130:183–194. doi: 10.1007/s10549-011-1559-2. [DOI] [PubMed] [Google Scholar]
- 39.van Gemert WA, May AM, Schuit AJ, Oosterhof BY, Peeters PH, Monninkhof EM. Effect of weight loss with or without exercise on inflammatory markers and adipokines in postmenopausal women: the SHAPE-2 trial, a randomized controlled trial. BMC Public Health. 2016;25:799–806. doi: 10.1158/1055-9965.EPI-15-1065. [DOI] [PubMed] [Google Scholar]
- 40.Rojo-Martínez G, Soriguer F, Colomo N, Calle A, Goday A, Bordiú E, Delgado E, Menéndez E, Ortega E, Urrutia I, Girbés J, Castaño L, Catalá M, Gaztambide S, Valdés S di@bet.es study group. Factors determining high-sensitivity C-reactive protein values in the Spanish population. Di@bet.es study. Eur J Clin Invest. 2013;43:1–10. doi: 10.1111/eci.12002. [DOI] [PubMed] [Google Scholar]
- 41.Dias JA, Wirfalt E, Drake I, Gullberg B, Hedblad B, Persson M, Engström G, Nilsson J, Schiopu A, Fredrikson GN, Björkbacka H. A high quality diet is associated with reduced systemic inflammation in middle-aged individuals. Atherosclerosis. 2015;238:38–44. doi: 10.1016/j.atherosclerosis.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 42.Bermudez EA, Rifai N, Buring JE, Manson JE, Ridker PM. Relation between markers of systemic vascular inflammation and smoking in women. Am J Cardiol. 2002;89:1117–1119. doi: 10.1016/s0002-9149(02)02284-1. [DOI] [PubMed] [Google Scholar]
- 43.Stewart SH, Mainous AG 3rd, Gilbert G. Relation between alcohol consumption and C-reactive protein levels in the adult US population. J Am Board Fam Pract. 2002;15:437–42. [PubMed] [Google Scholar]
- 44.Jung SY, Scott P, Papp J, Sobel E, Pellegrini M, Yu H, et al. Genome-wide association analysis of pro-inflammatory cytokines and gene-lifestyle interaction for invasive breast cancer risk: the WHI dbGaP Study. Submitted and Reviewed for Publication. 2020 doi: 10.1158/1940-6207.CAPR-20-0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ellis J, Lange EM, Li J, Dupuis J, Baumert J, Walston JD, Keating BJ, Durda P, Fox ER, Palmer CD, Meng YA, Young T, Farlow DN, Schnabel RB, Marzi CS, Larkin E, Martin LW, Bis JC, Auer P, Ramachandran VS, Gabriel SB, Willis MS, Pankow JS, Papanicolaou GJ, Rotter JI, Ballantyne CM, Gross MD, Lettre G, Wilson JG, Peters U, Koenig W, Tracy RP, Redline S, Reiner AP, Benjamin EJ, Lange LA. Large multiethnic Candidate Gene Study for C-reactive protein levels: identification of a novel association at CD36 in African Americans. Hum Genet. 2014;133:985–995. doi: 10.1007/s00439-014-1439-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schick UM, Auer PL, Bis JC, Lin H, Wei P, Pankratz N, Lange LA, Brody J, Stitziel NO, Kim DS, Carlson CS, Fornage M, Haessler J, Hsu L, Jackson RD, Kooperberg C, Leal SM, Psaty BM, Boerwinkle E, Tracy R, Ardissino D, Shah S, Willer C, Loos R, Melander O, Mcpherson R, Hovingh K, Reilly M, Watkins H, Girelli D, Fontanillas P, Chasman DI, Gabriel SB, Gibbs R, Nickerson DA, Kathiresan S, Peters U, Dupuis J, Wilson JG, Rich SS, Morrison AC, Benjamin EJ, Gross MD, Reiner AP Cohorts for Heart and Aging Research in Genomic Epidemiology; National Heart, Lung, and Blood Institute GO Exome Sequencing Project. Association of exome sequences with plasma C-reactive protein levels in >9000 participants. Hum Mol Genet. 2015;24:559–571. doi: 10.1093/hmg/ddu450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Prasad G, Giri AK, Basu A, Tandon N, Bharadwaj D. Genomewide association study for C-reactive protein in Indians replicates known associations of common variants. J Genet. 2019;98:20. [PubMed] [Google Scholar]
- 48.Chung RH, Chen YE. A two-stage random forest-based pathway analysis method. PLoS One. 2012;7:e36662. doi: 10.1371/journal.pone.0036662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Montazeri M, Beigzadeh A. Machine learning models in breast cancer survival prediction. Technol Health Care. 2016;24:31–42. doi: 10.3233/THC-151071. [DOI] [PubMed] [Google Scholar]
- 50.Pang H, Lin A, Holford M, Enerson BE, Lu B, Lawton MP, Floyd E, Zhao H. Pathway analysis using random forests classification and regression. Bioinformatics. 2006;22:2028–2036. doi: 10.1093/bioinformatics/btl344. [DOI] [PubMed] [Google Scholar]
- 51.Chang JS, Yeh RF, Wiencke JK, Wiemels JL, Smirnov I, Pico AR, Tihan T, Patoka J, Miike R, Sison JD, Rice T, Wrensch MR. Pathway analysis of single-nucleotide polymorphisms potentially associated with glioblastoma multiforme susceptibility using random forests. Cancer Epidemiol Biomarkers Prev. 2008;17:1368–1373. doi: 10.1158/1055-9965.EPI-07-2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gawel SH, Lucht M, Gomer H, Treado P, Christensen IJ, Nielsen HJ, Davis GJ Danish Research Group on Early Detection of Colorectal Cancer. Evaluation of algorithm development approaches: development of biomarker panels for early detection of colorectal lesions. Clin Chim Acta. 2019;498:108–115. doi: 10.1016/j.cca.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 53.Mogensen UB, Ishwaran H, Gerds TA. Evaluating random forests for survival analysis using prediction error curves. J Stat Softw. 2012;50:1–23. doi: 10.18637/jss.v050.i11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hamidi O, Poorolajal J, Farhadian M, Tapak L. Identifying important risk factors for survival in kidney graft failure patients using random survival forests. Iran J Public Health. 2016;45:27–33. [PMC free article] [PubMed] [Google Scholar]
- 55.Lou XY, Chen GB, Yan L, Ma JZ, Zhu J, Elston RC, Li MD. A generalized combinatorial approach for detecting gene-by-gene and gene-by-environment interactions with application to nicotine dependence. Am J Hum Genet. 2007;80:1125–1137. doi: 10.1086/518312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hou TT, Lin F, Bai S, Cleves MA, Xu HM, Lou XY. Generalized multifactor dimensionality reduction approaches to identification of genetic interactions underlying ordinal traits. Genet Epidemiol. 2019;43:24–36. doi: 10.1002/gepi.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xu HM, Xu LF, Hou TT, Luo LF, Chen GB, Sun XW, Lou XY. GMDR: versatile software for detecting gene-gene and gene-environment interactions underlying complex traits. Curr Genomics. 2016;17:396–402. doi: 10.2174/1389202917666160513102612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu HM, Xu LF, Hou TT, Luo LF, Chen GB, Sun XW, Lou XY. GMDR: versatile software for detecting gene-gene and gene-environment interactions underlying complex traits. 2019. http: //ibi.zju.edu.cn/software/GMDR/download.html. [DOI] [PMC free article] [PubMed]
- 59.Design of the Women’s Health Initiative clinical trial and observational study. The Women’s Health Initiative Study Group. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 60.NCBI: WHI Harmonized and Imputed GWAS Data. A sub-study of Women’s Health Initiative. 2019. https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000746.v3.p3.
- 61.Golkhalkhali B, Rajandram R, Paliany AS, Ho GF, Wan Ishak WZ, Johari CS, Chin KF. Strain-specific probiotic (microbial cell preparation) and omega-3 fatty acid in modulating quality of life and inflammatory markers in colorectal cancer patients: a randomized controlled trial. Asia Pac J Clin Oncol. 2018;14:179–191. doi: 10.1111/ajco.12758. [DOI] [PubMed] [Google Scholar]
- 62.Miranda DO, Anatriello E, Azevedo LR, Cordeiro JFC, Peria FM, Flória-Santos M, Pereira-da-Silva G. Elevated serum levels of proinflammatory cytokines potentially correlate with depression and anxiety in colorectal cancer patients in different stages of the antitumor therapy. Cytokine. 2018;104:72–77. doi: 10.1016/j.cyto.2017.09.030. [DOI] [PubMed] [Google Scholar]
- 63.Nielsen FH. Dietary magnesium and chronic disease. Adv Chronic Kidney Dis. 2018;25:230–235. doi: 10.1053/j.ackd.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 64.Cho YA, Lee J, Oh JH, Chang HJ, Sohn DK, Shin A, Kim J. Inflammatory dietary pattern, IL-17F genetic variant, and the risk of colorectal cancer. Nutrients. 2018;10:724. doi: 10.3390/nu10060724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.National Cancer Institute. SEER Program: Comparative Staging Guide For CancerJune. 1993. https://seer.cancer.gov/archive/manuals/historic/comp_stage1.1.pdf.
- 66.Jung SY, Mancuso N, Yu H, Papp J, Sobel E, Zhang ZF. Genome-wide meta-analysis of gene-environmental interaction for insulin resistance phenotypes and breast cancer risk in postmenopausal women. Cancer Prev Res (Phila) 2019;12:31–42. doi: 10.1158/1940-6207.CAPR-18-0180. [DOI] [PubMed] [Google Scholar]
- 67.Schumacher FR, Al Olama AA, Berndt SI, Benlloch S, Ahmed M, Saunders EJ, Dadaev T, Leongamornlert D, Anokian E, Cieza-Borrella C, Goh C, Brook MN, Sheng X, Fachal L, Dennis J, Tyrer J, Muir K, Lophatananon A, Stevens VL, Gapstur SM, Carter BD, Tangen CM, Goodman PJ, Thompson IM Jr, Batra J, Chambers S, Moya L, Clements J, Horvath L, Tilley W, Risbridger GP, Gronberg H, Aly M, Nordström T, Pharoah P, Pashayan N, Schleutker J, Tammela TLJ, Sipeky C, Auvinen A, Albanes D, Weinstein S, Wolk A, Håkansson N, West CML, Dunning AM, Burnet N, Mucci LA, Giovannucci E, Andriole GL, Cussenot O, Cancel-Tassin G, Koutros S, Beane Freeman LE, Sorensen KD, Orntoft TF, Borre M, Maehle L, Grindedal EM, Neal DE, Donovan JL, Hamdy FC, Martin RM, Travis RC, Key TJ, Hamilton RJ, Fleshner NE, Finelli A, Ingles SA, Stern MC, Rosenstein BS, Kerns SL, Ostrer H, Lu YJ, Zhang HW, Feng N, Mao X, Guo X, Wang G, Sun Z, Giles GG, Southey MC, MacInnis RJ, FitzGerald LM, Kibel AS, Drake BF, Vega A, Gómez-Caamaño A, Szulkin R, Eklund M, Kogevinas M, Llorca J, Castaño-Vinyals G, Penney KL, Stampfer M, Park JY, Sellers TA, Lin HY, Stanford JL, Cybulski C, Wokolorczyk D, Lubinski J, Ostrander EA, Geybels MS, Nordestgaard BG, Nielsen SF, Weischer M, Bisbjerg R, Røder MA, Iversen P, Brenner H, Cuk K, Holleczek B, Maier C, Luedeke M, Schnoeller T, Kim J, Logothetis CJ, John EM, Teixeira MR, Paulo P, Cardoso M, Neuhausen SL, Steele L, Ding YC, De Ruyck K, De Meerleer G, Ost P, Razack A, Lim J, Teo SH, Lin DW, Newcomb LF, Lessel D, Gamulin M, Kulis T, Kaneva R, Usmani N, Singhal S, Slavov C, Mitev V, Parliament M, Claessens F, Joniau S, Van den Broeck T, Larkin S, Townsend PA, Aukim-Hastie C, Gago-Dominguez M, Castelao JE, Martinez ME, Roobol MJ, Jenster G, van Schaik RHN, Menegaux F, Truong T, Koudou YA, Xu J, Khaw KT, Cannon-Albright L, Pandha H, Michael A, Thibodeau SN, McDonnell SK, Schaid DJ, Lindstrom S, Turman C, Ma J, Hunter DJ, Riboli E, Siddiq A, Canzian F, Kolonel LN, Le Marchand L, Hoover RN, Machiela MJ, Cui Z, Kraft P, Amos CI, Conti DV, Easton DF, Wiklund F, Chanock SJ, Henderson BE, Kote-Jarai Z, Haiman CA, Eeles RA Profile Study; Australian Prostate Cancer BioResource (APCB); IMPACT Study; Canary PASS Investigators; Breast and Prostate Cancer Cohort Consortium (BPC3); PRACTICAL (Prostate Cancer Association Group to Investigate Cancer-Associated Alterations in the Genome) Consortium; Cancer of the Prostate in Sweden (CAPS); Prostate Cancer Genome-wide Association Study of Uncommon Susceptibility Loci (PEGASUS); Genetic Associations and Mechanisms in Oncology (GAME-ON)/Elucidating Loci Involved in Prostate Cancer Susceptibility (ELLIPSE) Consortium. Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nat Genet. 2018;50:928–936. doi: 10.1038/s41588-018-0142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Manichaikul A, Mychaleckyj JC, Rich SS, Daly K, Sale M, Chen WM. Robust relationship inference in genome-wide association studies. Bioinformatics. 2010;26:2867–2873. doi: 10.1093/bioinformatics/btq559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ishwaran H, Kogalur UB, editors. Random Survival Forests for R. 2007. https://pdfs.semanticscholar.org/951a/84f0176076fb6786fdf43320e8b27094dcfa.pdf. [DOI] [PMC free article] [PubMed]
- 70.Harrell FE Jr, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982;247:2543–2546. [PubMed] [Google Scholar]
- 71.Wiens BL, Dmitrienko A, Marchenko O. Selection of hypothesis weights and ordering when testing multiple hypotheses in clinical trials. J Biopharm Stat. 2013;23:1403–1419. doi: 10.1080/10543406.2013.834920. [DOI] [PubMed] [Google Scholar]
- 72.Gene Card: Human Gene Database: One Cut Homeobox 2. 2020. https://www.genecards.org/cgi-bin/carddisp.pl?gene=ONECUT2.
- 73.Lu T, Wu B, Yu Y, Zhu W, Zhang S, Zhang Y, Guo J, Deng N. Blockade of ONECUT2 expression in ovarian cancer inhibited tumor cell proliferation, migration, invasion and angiogenesis. Cancer Sci. 2018;109:2221–2234. doi: 10.1111/cas.13633. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 74.Zhang J, Cheng J, Zeng Z, Wang Y, Li X, Xie Q, Guo J, Deng N. Comprehensive profiling of novel microRNA-9 targets and a tumor suppressor role of microRNA-9 via targeting IGF2BP1 in hepatocellular carcinoma. Oncotarget. 2015;6:42040–42052. doi: 10.18632/oncotarget.5969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang K, Wang YW, Wang YY, Song Y, Zhu J, Si PC, Ma R. Identification of microRNA biomarkers in the blood of breast cancer patients based on microRNA profiling. Gene. 2017;619:10–20. doi: 10.1016/j.gene.2017.03.038. [DOI] [PubMed] [Google Scholar]
- 76.Guo H, Ci X, Ahmed M, Hua JT, Soares F, Lin D, Puca L, Vosoughi A, Xue H, Li E, Su P, Chen S, Nguyen T, Liang Y, Zhang Y, Xu X, Xu J, Sheahan AV, Ba-Alawi W, Zhang S, Mahamud O, Vellanki RN, Gleave M, Bristow RG, Haibe-Kains B, Poirier JT, Rudin CM, Tsao MS, Wouters BG, Fazli L, Feng FY, Ellis L, van der Kwast T, Berlin A, Koritzinsky M, Boutros PC, Zoubeidi A, Beltran H, Wang Y, He HH. ONECUT2 is a driver of neuroendocrine prostate cancer. Nat Commun. 2019;10:278. doi: 10.1038/s41467-018-08133-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sun Y, Shen S, Liu X, Tang H, Wang Z, Yu Z, Li X, Wu M. MiR-429 inhibits cells growth and invasion and regulates EMT-related marker genes by targeting Onecut2 in colorectal carcinoma. Mol Cell Biochem. 2014;390:19–30. doi: 10.1007/s11010-013-1950-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.HNF4A hepatocyte nuclear factor 4 alpha. Genetics Home Reference. 2020. https://www.ncbi.nlm.nih.gov/gene/3172.
- 79.Darsigny M, Babeu JP, Seidman EG, Gendron FP, Levy E, Carrier J, Darsigny M, Babeu JP, Seidman EG, Gendron FP, Levy E, Carrier J, Perreault N, Boudreau F. Hepatocyte nuclear factor-4alpha promotes gut neoplasia in mice and protects against the production of reactive oxygen species. Cancer Res. 2010;70:9423–9433. doi: 10.1158/0008-5472.CAN-10-1697. [DOI] [PubMed] [Google Scholar]
- 80.López-Mejías R, Genre F, Remuzgo-Martínez S, González-Juanatey C, Robustillo-Villarino M, Llorca J, Corrales A, Vicente E, Miranda-Filloy JA, Magro C, Tejera-Segura B, Ramírez Huaranga MA, Pina T, Blanco R, Alegre-Sancho JJ, Raya E, Mijares V, Ubilla B, Mínguez Sánchez MD, Gómez-Vaquero C, Balsa A, Pascual-Salcedo D, López-Longo FJ, Carreira P, González-Álvaro I, Rodríguez-Rodríguez L, Fernández-Gutiérrez B, Ferraz-Amaro I, Castañeda S, Martín J, González-Gay MA. Influence of elevated-CRP level-related polymorphisms in non-rheumatic Caucasians on the risk of subclinical atherosclerosis and cardiovascular disease in rheumatoid arthritis. Sci Rep. 2016;6:31979. doi: 10.1038/srep31979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ligthart S, de Vries PS, Uitterlinden AG, Hofman A CHARGE Inflammation working group. Franco OH, Chasman DI, Dehghan A. Pleiotropy among common genetic loci identified for cardiometabolic disorders and C-reactive protein. PLoS One. 2015;10:e0118859. doi: 10.1371/journal.pone.0118859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gene Card: human gene database: hepatocyte nuclear factor 4 alpha. 2020. https://www.genecards.org/cgi-bin/carddisp.pl?gene=HNF4A.
- 83.Babeu JP, Boudreau F. Hepatocyte nuclear factor 4-alpha involvement in liver and intestinal inflammatory networks. World J Gastroenterol. 2014;20:22–30. doi: 10.3748/wjg.v20.i1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yang YC, Fu WP, Zhang J, Zhong L, Cai SX, Sun C. rs401681 and rs402710 confer lung cancer susceptibility by regulating TERT expression instead of CLPTM1L in East Asian populations. Carcinogenesis. 2018;39:1216–1221. doi: 10.1093/carcin/bgy084. [DOI] [PubMed] [Google Scholar]
- 85.Selvaraj G, Kaliamurthi S, Kaushik AC, Khan A, Wei YK, Cho WC, Gu K, Wei DQ. Identification of target gene and prognostic evaluation for lung adenocarcinoma using gene expression meta-analysis, network analysis and neural network algorithms. J Biomed Inform. 2018;86:120–134. doi: 10.1016/j.jbi.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 86.Tentu S, Nandarapu K, Muthuraj P, Venkitasamy K, Venkatraman G, Rayala SK. DHQZ-17, a potent inhibitor of the transcription factor HNF4A, suppresses tumorigenicity of head and neck squamous cell carcinoma in vivo. J Cell Physiol. 2018;233:2613–2628. doi: 10.1002/jcp.26139. [DOI] [PubMed] [Google Scholar]
- 87.Rogerson C, Britton E, Withey S, Hanley N, Ang YS, Sharrocks AD. Identification of a primitive intestinal transcription factor network shared between esophageal adenocarcinoma and its precancerous precursor state. Genome Res. 2019;29:723–736. doi: 10.1101/gr.243345.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li MM, Tang YQ, Gong YF, Cheng W, Li HL, Kong FE, Guan XY, Ma NF, Liu M. Development of an oncogenic dedifferentiation SOX signature with prognostic significance in hepatocellular carcinoma. BMC Cancer. 2019;19:851. doi: 10.1186/s12885-019-6041-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Takashima Y, Horisawa K, Udono M, Ohkawa Y, Suzuki A. Prolonged inhibition of hepatocellular carcinoma cell proliferation by combinatorial expression of defined transcription factors. Cancer Sci. 2018;109:3543–3553. doi: 10.1111/cas.13798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yao HS, Wang J, Zhang XP, Wang LZ, Wang Y, Li XX, Jin KZ, Hu ZQ, Wang WJ. Hepatocyte nuclear factor 4alpha suppresses the aggravation of colon carcinoma. Mol Carcinog. 2016;55:458–472. doi: 10.1002/mc.22294. [DOI] [PubMed] [Google Scholar]
- 91.Shabana , Shahid SU, Hasnain S. Use of a gene score of multiple low-modest effect size variants can predict the risk of obesity better than the individual SNPs. Lipids Health Dis. 2018;17:155. doi: 10.1186/s12944-018-0806-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Salva-Pastor N, Chavez-Tapia NC, Uribe M, Nuno-Lambarri N. Understanding the association of polycystic ovary syndrome and non-alcoholic fatty liver disease. J Steroid Biochem Mol Biol. 2019;194:105445. doi: 10.1016/j.jsbmb.2019.105445. [DOI] [PubMed] [Google Scholar]
- 93.Simo R, Barbosa-Desongles A, Lecube A, Hernandez C, Selva DM. Potential role of tumor necrosis factor-alpha in downregulating sex hormone-binding globulin. Diabetes. 2012;61:372–382. doi: 10.2337/db11-0727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Slattery ML, Potter JD, Curtin K, Edwards S, Ma KN, Anderson K, Schaffer D, Samowitz WS. Estrogens reduce and withdrawal of estrogens increase risk of microsatellite instability-positive colon cancer. Cancer Res. 2001;61:126–130. [PubMed] [Google Scholar]
- 95.Issa JP. Colon cancer: it’s CIN or CIMP. Clin Cancer Res. 2008;14:5939–5940. doi: 10.1158/1078-0432.CCR-08-1596. [DOI] [PubMed] [Google Scholar]
- 96.Martínez ME, Grodstein F, Giovannucci E, Colditz GA, Speizer FE, Hennekens C, Rosner B, Willett WC, Stampfer MJ. A prospective study of reproductive factors, oral contraceptive use, and risk of colorectal cancer. Cancer Epidemiol. 1997;6:1–5. [PubMed] [Google Scholar]
- 97.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 98.Van Horn L, Carson JA, Appel LJ, Burke LE, Economos C, Karmally W, Lancaster K, Lichtenstein AH, Johnson RK, Thomas RJ, Vos M, Wylie-Rosett J, Kris-Etherton P American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council. Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) guidelines: a scientific statement from the American Heart Association. Circulation. 2016;134:e505–e529. doi: 10.1161/CIR.0000000000000462. [DOI] [PubMed] [Google Scholar]
- 99.Waist Circumference and Waist-Hip Ratio. The World Health Organization. 2011. https://apps.who.int/iris/bitstream/handle/10665/44583/9789241501491_eng.pdf;jsessionid=587F1A4B31954337F34F1A84F063AB0E?sequence=1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.