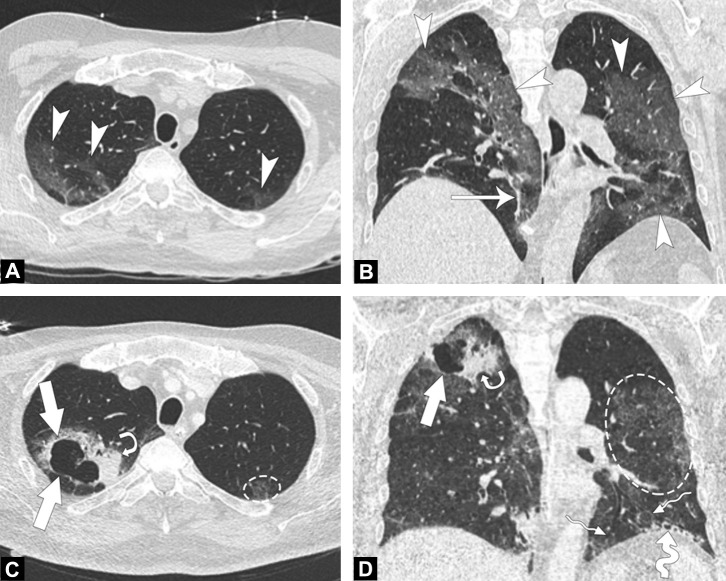
A 62-year-old man was hospitalized in intensive care unit for severe Covid-19 pneumonia confirmed by reverse-transcriptase polymerase chain reaction positivity on oropharyngeal swabs. At initial examination, arterial blood pressure was within the normal range (100/76 mmHg) but tachyarrhythmia (heart rate, 120/min), tachypnea (respiratory rate, 38/min) and low oxygen saturation at 82% were found. Body temperature was 38.1 °C. Supplemental oxygen (15 L/min) was insufficient to restore oxygen saturation above 90% and sedation and orotracheal intubation were required. Laboratory tests revealed hemoglobin concentration of 16.8 g/dL, platelet count of 306 × 109/L, leucocyte count of 13.5 × 109/L and fibrinogen serum level of 6.13 g/L. Procalcitonin serum level was not elevated. Initial low dose computed tomography examination (CT) [1] was strongly suggestive of COVID-19 pneumonia (Fig. 1A and B). Repeated cultures from bronchoalveolar lavage were positive for methicillin-sensitive-Staphylococcus-aureus, Pseudomonas-Aeruginosa and Klebsiella-Pneumonia. The patient was given meropenem, tobramycin and ciprofloxacin with gradual improvement of symptoms. Follow-up CT examination showed thin-walled large cavity within consolidation of the right upper lobe (Fig. 1C and D). Additional bacteriological tests were positive for Aspergillus-niger on bronchoalveolar fluid and aspergillus antigenemia. Antifungal treatment (amphotericin B then voriconazole) was added, followed by a favorable clinical course. Typical CT patterns of COVID-19 pneumonia are well known, but lung cavitation remains uncommon [2]. It might be explained by viral damage to the alveolar walls leading to pneumatoceles. Bacterial and fungal superinfections can also be observed.
Fig. 1.
Chest CT examinations obtained at day 1 and day 20 in a 62-year-old man with severe COVID-19 pneumonia. A, B, CT images in the axial (A) and coronal (B) planes in lung window obtained at day 1 of hospitalization reveal ground glass opacities (arrowheads) and linear consolidations (arrow). C, D, Follow-up CT images in the axial (C) and coronal (D) planes in lung window at the same level than in A & B, obtained at day 20 of hospitalization in intensive care unit demonstrate a large cavitation (arrows) and evolution towards consolidation of ground glass opacities (curved arrow) in the right upper lobe, interlobular septal thickening resulting in left upper lobe crazy paving appearance (dotted circle), cystic changes (large wave arrow) and traction bronchiectasis (thin wave arrows).
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patient(s) and/or volunteers.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
CRediT authorship contribution statement
Amine Ammar: conceptualization, writing - original draft preparation, visualization. Jean-Luc Drapé: supervision, writing - review & editing. Marie-Pierre Revel: supervision, writing - review & editing, validation.
References
- 1.Ludes C., Labani A., Severac F., Jeung M.Y., Leyendecker P., Roy C. Ultra-low-dose unenhanced chest CT: prospective comparison of high kV/low mA versus low kV/high mA protocols. Diagn Interv Imaging. 2019;100:85–93. doi: 10.1016/j.diii.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 2.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101:263–268. doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]