Abstract
Objective
To compare labor patterns in pregnancies affected by fetal anomalies to low-risk singletons.
Study Design
Labor data from the Consortium on Safe Labor, a multicenter retrospective study from 19 U.S. hospitals, including 98,674 low-risk singletons compared with 6,343 pregnancies with fetal anomalies were analyzed. Repeated-measures analysis constructed mean labor curves by parity, gestational age, and presence of fetal anomaly in women who reached full dilation. Interval-censored regression analysis adjusted for covariables was used to determine the median traverse times for labor progression.
Results
Labor curves for all groups indicated slower labor progress for patients with fetal anomalies. The most significant trends in median traverse times were observed in the preterm nulliparous and term multiparous groups. The median traverse times from 4 cm to complete dilation in the preterm nulliparous control versus anomaly groups were 5.0 and 5.4 hours (p < 0.0001).
Conclusion
Labor proceeds at a slower rate in pregnancies affected by anomalies.
Keywords: fetal anomalies, labor progress, labor curves, chromosome abnormalities
Approximately 3% of live births are affected by major congenital malformations or anomalies in the United States.1 While the diagnosis of a fetal anomaly is not typically thought to be associated with increased obstetric risk, little research has been done evaluating obstetric outcomes and labor patterns in pregnancies affected by fetal anomalies. Much of the original research looking at labor patterns excluded pregnancies affected by fetal anomalies in the analyses.2–8 Using a contemporary cohort of patients, Zhang et al evaluated labor progression but again excluded gravidas with fetal anomalies.2 Thus, there is little evidence guiding labor management for this subset of women.
Pregnancies affected by fetal anomalies have historically been associated with certain obstetric considerations such as malpresentation, which in turn leads to increased cesarean section rates.9,10 One retrospective study concluded that in pregnancies with major congenital cardiac anomalies, there were higher rates of nonreassuring fetal status and emergency cesarean delivery (CD).11 Rossi et al looked specifically at fetal cyanotic cardiac anomalies and showed higher rates of cesarean section, preterm delivery, small for gestational age, and abnormal fetal heart tones.10 There is a paucity of data in regard to anomalies and labor other than cardiac anomalies.
The present study sought to determine if labor progress is altered in pregnancies affected by fetal anomalies. A better understanding of labor progression and obstetric risk factors in women with pregnancies affected by fetal malformations may provide guidance for physicians managing labor for this vulnerable subset of patients.
Materials and Methods
Using data from the Consortium on Safe Labor, containing data from more than 200,000 deliveries collected from 19 U.S. hospitals from 2002 to 2008, we obtained labor information for women with pregnancies affected by fetal anomalies and compared them with low-risk singleton gestations.2,3 The Consortium on Safe Labor is a Eunice Kennedy Shriver National Institute of Child Health and Human Development sponsored dataset that was meant to represent a contemporary group of women to help define labor and delivery characteristics. The data were obtained from 12 clinical centers across 9 American College of Obstetricians and Gynecologists districts. The majority of the births occurred from 2005 to 2007 (87%). The cohort includes both term and preterm women (>23 weeks). Detailed description of the dataset is provided elsewhere.2,3 The Institutional Review Boards at all participating sites approved this study.
Information from a total of 228, 668 deliveries is provided in the dataset. In the current study, the following inclusion criteria were used: liveborn, singleton gestation ≥24 and ≤42 weeks with induced or spontaneous labor, defined as those who had a vaginal delivery or those who had at least two cervical exams in the database. Deliveries were excluded for multiple gestation, still birth, history of cesarean section, trial of labor with <2 vaginal exams, missing data or repeated measures, and diagnosis of placenta previa/accreta (Fig. 1). Approximately 6% of the women contributed more than one delivery to the dataset. The first delivery for these women was used to avoid intrapersonal correlation.
Fig. 1.
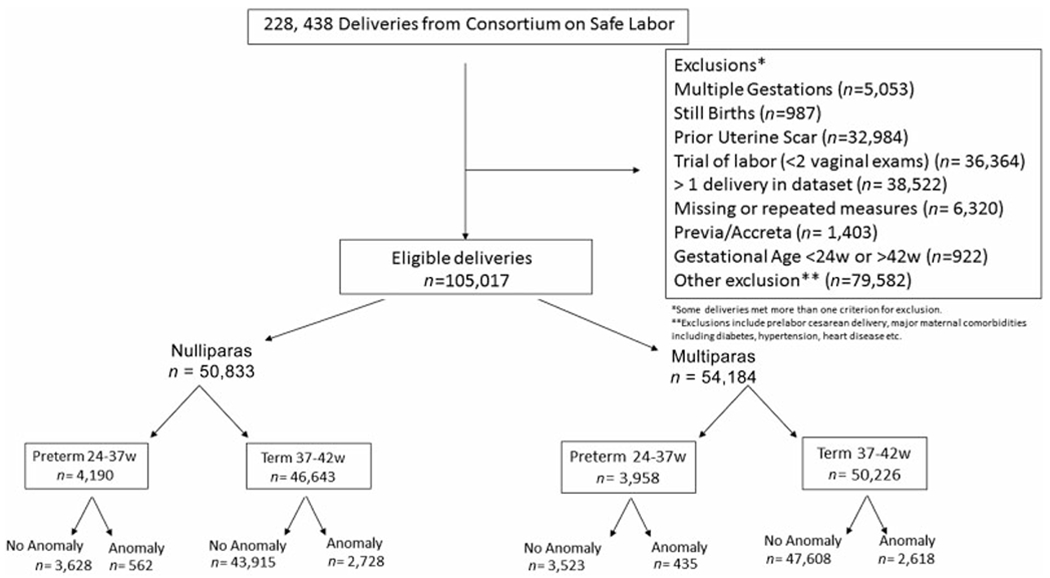
Diagram of patient selection. Total patients in consortium were divided after exclusions applied into nulliparas and multiparas and then by presence of anomaly. All exclusions listed in figure.
There were 105,017 deliveries meeting inclusion criteria and evaluated in the present study, including 6,373 women with fetal anomalies. Anomalies were defined as major congenital anomalies by system and included International Classification of Diseases (ICD)-9 diagnosis codes 740–758 (nervous system ICD-9—740–742, eye, ear, face, and neck ICD-9—743–744, circulatory system ICD-9—745–747, respiratory system ICD-9—748, digestive system ICD-9—749–751, genital organs ICD-9—752, urinary system ICD-9—753, musculoskeletal system ICD-9—754–756, integument ICD-9—757, and other ICD-9—759) and major chromosome anomalies (ICD-9—758) (Supplementary Table S1, available in the online version). The cohort was divided into those with anomalies, the study group versus the controls, those without, and then further divided into the following subgroups: preterm (delivery occurred at 24–366/7 weeks’ gestation) and term (≥37 and ≤42 weeks’ gestation) and by parity, nulliparous, and multiparous groups (Fig. 1).
Demographics and maternal characteristics between anomaly and control groups were compared using Pearson’s chi-square test and analysis of variance. Descriptive variables including maternal age, race, body mass index (BMI), gestational age, pregestational diabetes, cervical dilation and effacement at admission, augmentation, induction, operative vaginal delivery, epidural anesthesia, CD, and birth weight were analyzed and are shown in Tables 1 and 2.
Table 1.
Maternal demographics and labor characteristics nulliparas
| Preterm | Term | |||||
|---|---|---|---|---|---|---|
| No anomaly | Anomaly | p-Value | No anomaly | Anomaly | p-Value | |
| n = 3,628 | n = 562 | n = 43,915 | n = 2,728 | |||
| Maternal age, y, mean (SD) | 24.7 (6.2) | 24.4 (6.4) | 0.24 | 25.2 (6.0) | 25.5 (6.1) | 0.0009 |
| Maternal BMI | 24.1 (5.6) | 25.2 (6.4) | 0.0006 | 24.0 (5.3) | 24.2 (5.2) | 0.04 |
| Race, n (%) | ||||||
| White | 1,715 (50) | 239 (45) | 0.01 | 23,002 (55) | 1,207 (46) | <0.0001 |
| Black | 848 (25) | 171 (32) | 7,862 (19) | 689 (26) | ||
| Hispanic | 612 (18) | 89 (17) | 7,351 (18) | 400 (15) | ||
| Asian | 171 (5) | 22 (4) | 2,409 (6) | 240 (9) | ||
| Other | 79 (2) | 11 (2) | 997 (2) | 65 (3) | ||
| Gestational age, wk, mean (SD) | 34.5 (2.6) | 32.2 (4.0) | <0.0001 | 39.4 (1.1) | 39.4 (1.2) | 0.0003 |
| Dilation at admission, cm, mean (SD) | 2.8 (2.4) | 2.9 (2.6) | 0.34 | 3.0 (2.1) | 3.0 (2.1) | 0.20 |
| Effacement at admission, n (%), mean (SD) | 71.3 (28.7) | 68.4 (30.2) | 0.03 | 75.9 (23.1) | 74.6 (24.1) | 0.01 |
| No. of cervical exams, mean (SD) | 6.7 (3.6) | 6.2 (4.0) | 0.0007 | 7.7 (3.4) | 7.6 (3.5) | 0.10 |
| Induction, n (%) | 1,349 (37) | 197 (35) | 0.33 | 19,589 (45) | 1,233 (45) | 0.55 |
| Augmentation, n (%) | 1,073 (68) | 129 (51) | <0.0001 | 12,837 (72) | 715 (61) | <0.0001 |
| Epidural analgesia, n (%) | 2,072 (67) | 264 (54) | <0.0001 | 29,006 (77) | 1,793 (78) | 0.15 |
| Operative vaginal delivery, n (%) | 249 (7) | 29 (5) | 0.13 | 4,586 (10) | 263 (10) | 0.18 |
| Cesarean delivery, n (%) | 684 (19) | 165 (29) | <0.0001 | 9,475 (22) | 734 (27) | <0.0001 |
| Cesarean performed for labor abnormality, n (%) | 626 (17) | 153 (27) | <0.0001 | 9,393 (21) | 730 (27) | <0.0001 |
| Birth weight, g, mean (SD) | 2,406.4 (621.0) | 1,893.9 (767.0) | <0.0001 | 3,328.8 (436.5) | 3,303.1 (460.7) | 0.003 |
Abbreviations: BMI, body mass index; SD, standard deviation.
Table 2.
Maternal demographics and labor characteristics multiparas
| Preterm | Term | |||||
|---|---|---|---|---|---|---|
| No anomaly | Anomaly | p-Value | No anomaly | Anomaly | p-Value | |
| n = 3,523 | n = 435 | n = 47,608 | n = 2,618 | |||
| Maternal age, y, mean (SD) | 28.5 (5.8) | 28.7 (5.9) | 0.47 | 29.3 (5.4) | 29.3 (5.5) | 0.96 |
| Maternal BMI | 25.2 (6.0) | 25.6 (6.1) | 0.23 | 25.1 (5.6) | 25.3 (5.9) | 0.05 |
| Race, n (%) | ||||||
| White | 1,622 (48) | 198 (47) | 0.30 | 29,950 (57) | 1,203 (48) | <0.0001 |
| Black | 927 (27) | 123 (29) | 8,024 (18) | 626 (25) | ||
| Hispanic | 649 (19) | 83 (20) | 8,714 (19) | 433 (17) | ||
| Asian | 132 (4) | 9(2) | 1,804 (4) | 183 (7) | ||
| Other | 76 (3) | 6 (1) | 993 (2) | 70 (3) | ||
| Gestational age, wk, mean (SD) | 34.8 (2.3) | 32.7 (3.8) | <0.0001 | 39.2 (1.1) | 39.1 (1.1) | 0.0001 |
| Dilation at admission, cm, mean (SD) | 3.7 (2.4) | 3.7 (2.7) | 0.92 | 3.9 (2.2) | 3.9 (2.2) | 0.69 |
| Effacement at admission, n (%), mean (SD) | 71.4 (25.5) | 69.0 (27.4) | 0.08 | 75.1 (21.1) | 74.6 (21.3) | 0.29 |
| No. of cervical exams, mean (SD) | 6.2 (3.4) | 5.5 (3.4) | <0.0001 | 6.4 (2.9) | 6.4 (3.1) | 0.77 |
| Induction, n (%) | 1,018 (29) | 126 (29) | 0.98 | 19,758 (42) | 1,093 (42) | 0.80 |
| Augmentation, n (%) | 1,136 (68) | 112 (54) | <0.0001 | 12,415 (67) | 643 (58) | <0.0001 |
| Epidural analgesia, n (%) | 1,824 (60) | 205 (54) | 0.0013 | 28,703 (70) | 1,555 (72) | 0.08 |
| Operative vaginal delivery, n (%) | 78 (2) | 7 (2) | 0.41 | 1,686 (4) | 82 (3) | 0.27 |
| Cesarean delivery, n (%) | 299 (9) | 89 (20) | <0.0001 | 2,115 (5) | 174 (7) | <0.0001 |
| Cesarean performed for labor abnormality, n (%) | 284 (8) | 84 (19) | <0.0001 | 2,104 (4) | 171 (7) | <0.0001 |
| Birth weight, g, mean (SD) | 2,555.6 (595.9) | 2,082.0 (793.1) | <0.0001 | 3,402.9 (436.3) | 3,378.6 (472.0) | 0.005 |
Abbreviations: BMI, body mass index; SD, standard deviation.
Variables considered in the statistical analysis described later included maternal age, race, BMI, gestational age, parity, pregestational diabetes, cervical dilation on admission (in centimeters), and induction or augmentation of labor. These independent variables were selected because they have been shown to affect labor progression.12,13
A repeated-measures analysis with an eighth-degree polynomial model was used to construct mean labor curves by parity and gestational age using cervical dilation in centimeters. For the labor curves, the starting point was set as the time when the patient first reached 10 cm (time = 0) and the time was calculated backward. The curves were created as previously described and only included gravidas who reached 10 cm.2 The labor curves begin after 3 cm dilation so as to allow for model convergence. Those who were admitted with more advanced cervical dilation were included as long as they had greater than two cervical exams in the dataset. Women who required CD were excluded in this analysis as previously described.2 PROC MIXED (SAS software, version 9.4; SAS Institute Inc, Cary, NC) was used.2,3
To evaluate duration of labor, an interval censored regression analysis was used to determine median traverse times (the time from progression from 1 cm of dilation to the next) starting at 3 cm to complete dilation as well as the total time from 4 cm dilation to 10 cm dilation.2 The median and 95th percentile were calculated for the first stage of labor for both the study and control groups (Tables 3–6). Traverse times are computed assuming the labor data are normally distributed.2 The median traverse times were adjusted for age, race, BMI, gestational age, induction, augmentation, epidural (first stage only), vaginal delivery, and birth weight. PROC LIFEREG (SAS software, version 9.4; SAS Institute Inc) was used to evaluate traverse times at each centimeter of dilation, as well as total duration of labor between anomalous and nonanomalous groups.2,3 The times for second stage of labor were also calculated for all groups in patients with and without an epidural and included in the traverse tables. A p-value of <0.05 was considered statistically significant.
Table 3.
Adjusted duration of labor in preterm nulliparas by presence of fetal anomaly with median traverse times reported as hours (95th percentile)
| No anomaly (N = 3,628) | Anomaly (N = 562) | p-Value for trend | |
|---|---|---|---|
| Cervical dilation, cm | |||
| 3–4 | 4.8 (14.4) | 5.8 (18.8) | 0.002 |
| 4–5 | 4.3 (12.8) | 4.6 (13.8) | 0.002 |
| 5–6 | 4.0 (12.4) | 4.0 (12.9) | <0.0001 |
| 6–7 | 3.5 (10.6) | 2.2 (10.2) | 0.58 |
| 7–8 | 2.7 (8.0) | 3.7 (11.1) | 0.001 |
| 8–9 | 2.0 (5.2) | 1.8 (5.1) | 0.13 |
| 9–10 | 1.5 (4.1) | 1.8 (6.0) | 0.002 |
| 4–10 | 5.0 (14.2) | 5.4(16.7) | <0.0001 |
| Second stage without epidural | 0.4 (2.4) | 0.3 (2.1) | 0.20 |
| Second stage with epidural | 0.8 (3.1) | 0.9 (4.4) | <0.005 |
Note: Adjusted model controlled for age, BMI, race, induction, augmentation, epidural (first stage only), and birth weight.
Table 6.
Adjusted duration of labor (hours) in term multiparas by presence of fetal anomaly with median traverse times reported as hour (95th percentile)
| No anomaly (N = 47,608) | Anomaly (N = 2,618) | p-Value for trend | |
|---|---|---|---|
| Cervical dilation, cm | |||
| 3–4 | 3.4 (9.4) | 3.4 (10.4) | <0.0001 |
| 4–5 | 2.5 (6.7) | 3.1 (7.2) | 0.010 |
| 5–6 | 2.5 (6.4) | 2.5 (6.2) | <0.0001 |
| 6–7 | 2.1 (5.6) | 1.8 (5.0) | <0.0001 |
| 7–8 | 1.7 (4.5) | 1.8 (3.8) | <0.0001 |
| 8–9 | 1.5 (4.1) | 1.6 (4.8) | 0.92 |
| 9–10 | 1.1 (3.4) | 1.1 (3.5) | 0.007 |
| 4–10 | 3.7 (9.6) | 3.7 (10.1) | 0.009 |
| Second stage without epidural | 0.2 (1.0) | 0.2 (1.0) | 0.65 |
| Second stage with epidural | 0.4 (1.6) | 0.3(1.5) | 0.42 |
Note: Adjusted model controlled for age, BMI, race, induction, augmentation, epidural (first stage only), and birth weight.
Results
The descriptive characteristics of the deliveries included in the current study are presented in Tables 1 and 2. The entire Consortium on Safe Labor database included 228,668 deliveries. After exclusions described earlier, 6,373 pregnancies were included in the anomaly groups and 98,674 were included in the low-risk, singleton control groups (Fig. 1). Three per cent of the total deliveries had recorded fetal anomalies that met our inclusion criteria for this analysis. This number is in line with the national averages indicating an adequate population sampling.1 Nulliparas made up 50,833 (48%) of the current study and control population. Multiparas represented 54,184 (52%) of the population. In the nulliparous group, there were 3,628 who were preterm controls without anomalies and 562 study women with anomalies. In the multiparous group, there were 3,523 preterm control patients without anomalies and 435 study women with anomalies. There were 43,915 nulliparous term control patients without anomalies and 2,728 study women with anomalies (Fig. 1). There were 47,608 multiparous term control patients without anomalies and 2,618 term study group patients with anomalies (Fig. 1).
Significantly higher rates of CD in anomalous study pregnancies were seen across all subgroups. In the preterm group, the rates were 19 versus 29% (p < 0.0001) in nulliparous women and 9 versus 20% (p < 0.0001) in multiparous women for the control and anomalous study pregnancies, respectively (Tables 1 and 2). In the term group, the CD rates for nulliparas were 22 versus 27% (p < 0.0001) and for multiparas 5 versus 7% (p < 0.0001) for control and anomalous study patients, respectively (Tables 1 and 2). The gestational ages and birth weights were also significantly lower in the anomalous groups as might be expected (Tables 1 and 2).
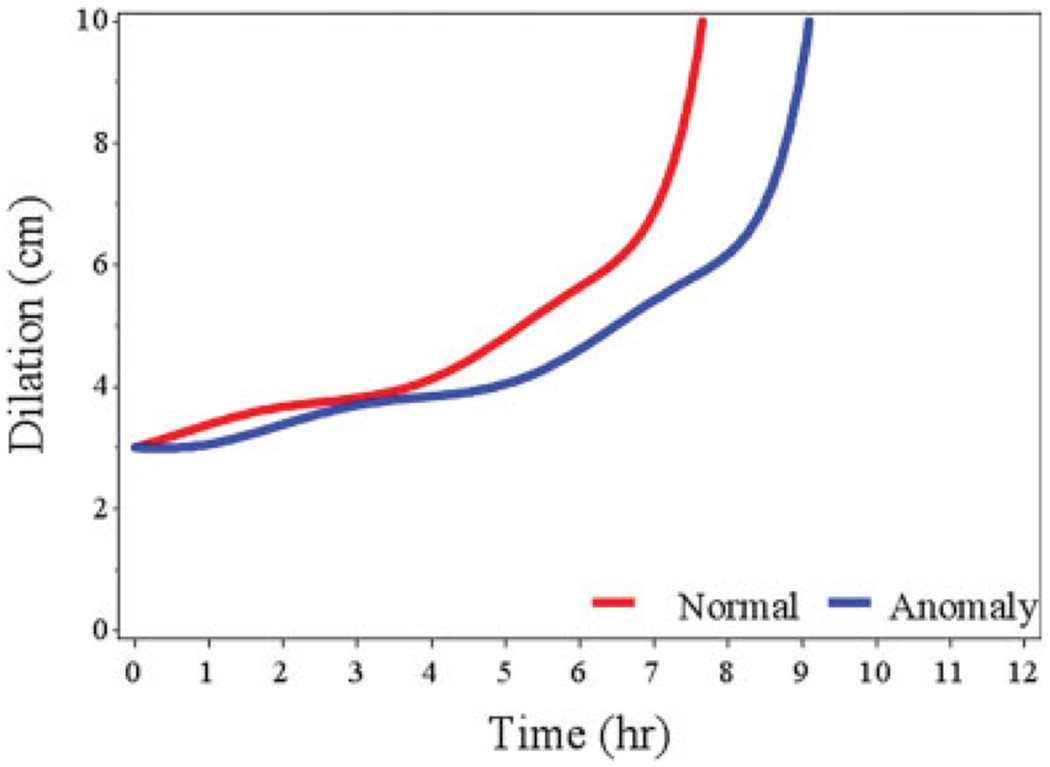
Figs. 2 to 5 illustrate the mean labor curves for the anomalous study women (blue) and nonanomalous controls (red), by nulliparity and multiparity and by preterm and term deliveries who reached 10 cm dilation. For all groups, the curves indicate that labor proceeded at a slower rate for women with pregnancies affected by fetal anomalies. There is a more dramatic difference noted in the curves for the preterm groups.
Fig. 2.
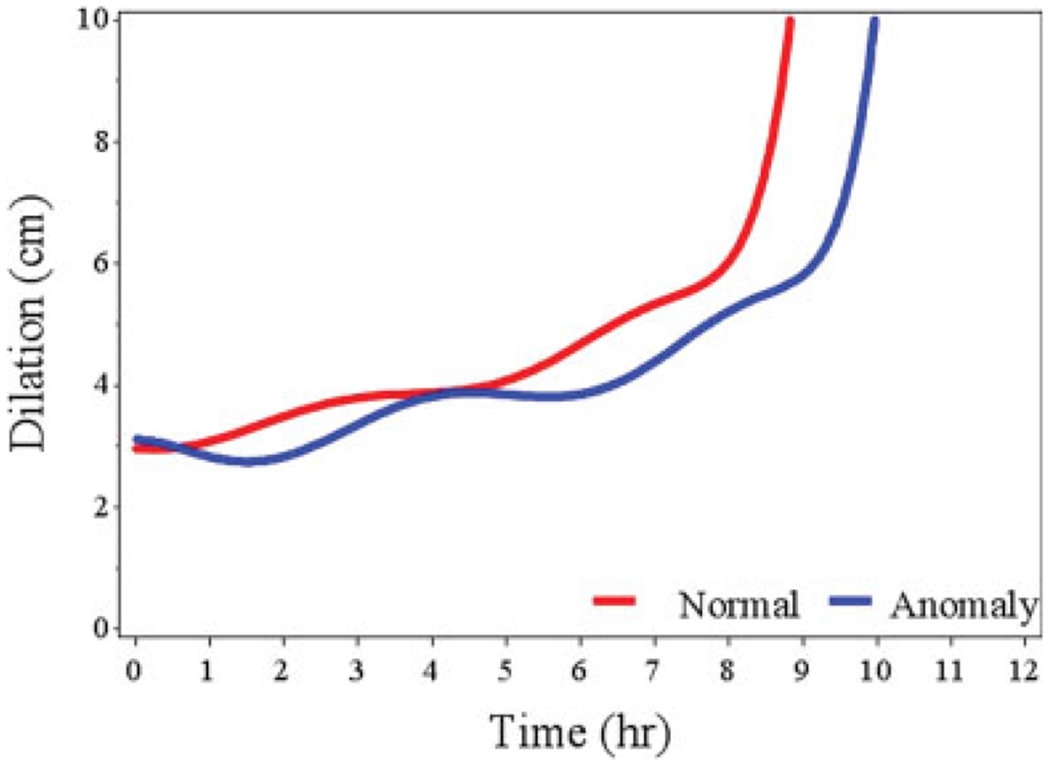
Labor curves for preterm multiparous women with dilation in centimeters on the y-axis and time in hours. Blue curve represents anomaly group and red curve represents control group.
Fig. 5.
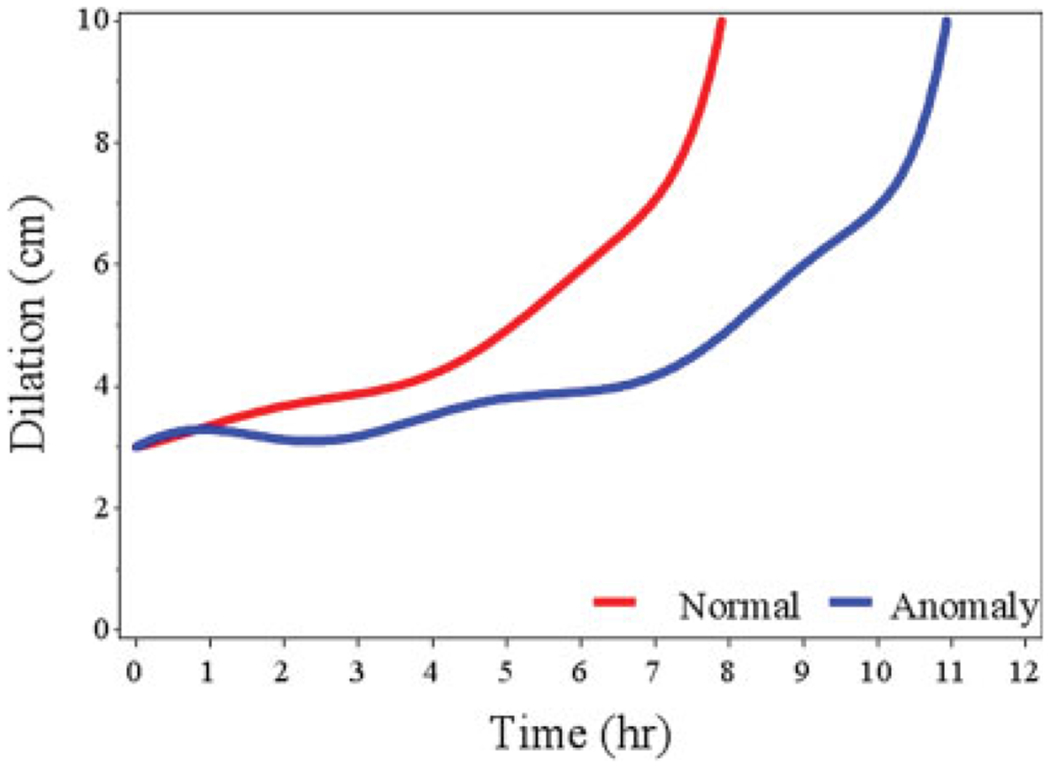
Labor curves for preterm nulliparous women with dilation in centimeters on the y-axis and time in hours. Blue curve represents anomaly group and red curve represents control group.
The curves for all groups also demonstrate a clear inflection point at 6 cm dilation, with a steep increase in the slope of the line after 6 cm dilation indicating the onset of active labor. Labor curves for spontaneous versus induced and augmented labors for nulliparas and multiparas were also generated for preterm, term, anomalies, and no anomalies with similar results, slower labor progress in the women with anomalies Supplementary Figs. 1–4, available in the online version.
The median traverse time from 4 cm to complete dilation in the preterm nulliparous patients was 5.4 versus 5.0 hours for the anomaly versus the control group (p < 0.0001, Table 3). For the preterm multiparous group, the median traverse time from 4 to 10 cm were 4.0 and 4.1 hours for the anomaly versus control group (p = 0.39, Table 4). Many of the centimeter to centimeter dilation times in the preterm groups were significantly different and trended toward longer labors in the anomaly patients (Tables 3 and 4). The latent phase times from 3 to 6 cm dilation for all groups took longer in the anomalous groups compared with the nonanomalous groups and was found to be significantly different in the traverse tables (Tables 3–6). This effect is also observed on the labor curves themselves showing longer times from dilation of 3 to 6 cm in anomalous and nonanomalous pregnancies (Figs. 2–5).
Table 4.
Adjusted duration of labor in preterm multiparas by presence of fetal anomaly with median traverse times reported as hours (95th percentile)
| No anomaly (N = 3,523) | Anomaly (N = 435) | p-Value for trend | |
|---|---|---|---|
| Cervical dilation, cm | |||
| 3–4 | 4.6 (14.9) | 4.3 (10.7) | 0.24 |
| 4–5 | 3.6 (10.1) | 4.0 (8.5) | <0.0001 |
| 5–6 | 3.6 (11.5) | 3.8 (16.9) | <0.0001 |
| 6–7 | 2.5 (6.9) | 4.7 (16.1) | <0.0001 |
| 7–8 | 1.8 (5.9) | 2.0 (4.1) | 0.13 |
| 8–9 | 1.3 (3.4) | 1.1 (2.2) | <0.0001 |
| 9–10 | 0.7 (2.0) | 1.2 (2.7) | 0.02 |
| 4–10 | 4.1 (12.6) | 4.0 (12.9) | 0.05 |
| Second stage without epidural | 0.1 (0.9) | 0.1 (1.6) | 0.96 |
| Second stage with epidural | 0.3 (1.3) | 0.3(1.4) | 0.51 |
Note: Adjusted model controlled for age, BMI, race, induction, augmentation, epidural (first stage only), and birth weight.
For the term groups, the total time to progress from 4 cm to complete dilation was longer in pregnancies affected by fetal anomalies in both unadjusted and adjusted models; however, this was only found to be significant in the multiparous term patients (adjusted data, Tables 5 and 6, and unadjusted data not shown).
Table 5.
Adjusted duration of labor (hours) in term nulliparas by presence of fetal anomaly with median traverse times reported as hours (95th percentile)
| No anomaly (N = 43,915) | Anomaly (N = 2,728) | p-Value for trend | |
|---|---|---|---|
| Cervical dilation, cm | |||
| 3–4 | 4.0 (10.6) | 4.1 (11.6) | 0.005 |
| 4–5 | 3.7 (8.7) | 3.7 (8.3) | 0.001 |
| 5–6 | 3.2 (7.4) | 3.1 (7.0) | <0.0001 |
| 6–7 | 2.9 (6.4) | 2.7 (5.9) | 0.61 |
| 7–8 | 2.5 (6.0) | 2.5 (5.7) | 0.002 |
| 8–9 | 2.2 (5.2) | 1.9 (4.9) | <0.0001 |
| 9–10 | 1.5 (3.7) | 2.0 (4.3) | <0.0001 |
| 4–10 | 5.2 (12.4) | 5.4 (13.5) | 0.39 |
| Second stage without epidural | 0.7 (3.2) | 0.7 (3.2) | 0.81 |
| Second stage with epidural | 1.3 (4.1) | 1.3(4.0) | 0.39 |
Note: Adjusted model controlled for age, BMI, race, induction, augmentation, epidural (first stage only), and birth weight.
The traverse tables indicate there were no significant differences in the length of second stage of labor between patients who had anomalies versus those who did not with and without epidurals except in the preterm nulliparous patients with an epidural, and this difference does not seem clinically relevant (Tables 3–6).
Comment
In this large, multicenter study of contemporary labor patterns across the United States, labor progressed at a slower rate for patients with pregnancies affected by fetal anomalies in all groups when compared with low-risk nonanomalous singleton gravidas, as shown in the labor curves (Figs. 2–5). The median traverse times from 4 to 10 cm dilation were significantly longer for the preterm nulliparous and the term multiparous patients (Tables 3 and 6) though clinically not much different. The centimeter to centimeter median traverse times between groups trended toward slower labor progress in the patients with anomalies. The computed traverse times suggest that these findings are independent of important covariables known to influence labor progress such as age, race, BMI, induction, augmentation, and birth weight. An inflection point at 6 cm was noted for both preterm and term anomalous studies and nonanomalous control gestations.
Of note, the times to reach 10 cm differ among the labor curves (Figs. 2–5) and the median traverse times (Tables 3–6) because the labor curves included only patients who reached 10 cm dilation, whereas the traverse times included patients who underwent intrapartum CD.
There have been no prior studies that we could locate evaluating labor progress in the specific cohort of patients with fetal anomalies. There are known labor complications specific to particular anomalies that may explain the findings of slower labor in the current study.14 For example, hydrocephalus likely causes labor protraction if the fetal head size creates cephalopelvic disproportion.15 Congenital anomalies and major chromosome abnormalities have a higher risk of malpresentation which may protract labor and affect risk for CD.16 Shipp et al found an association of the ultrasound finding of hyperextension of the fetal head in labor with possible congenital anomalies, which can lead to difficult protracted labors.17 De la Vega and Verdiales reported a high incidence of emergency cesarean section in pregnancies with unrecognized major chromosomal anomalies.18 The current study also observed an increased cesarean rate among pregnancies with fetal anomalies. Given the increased risk in pregnancies affected by fetal anomalies for labor complications, it is important to note, based on the current study, the naturally slower labor progress in these patients.
Another important finding of the present study is an inflection point in the labor curves at 6 cm, which indicates the onset of active labor. This was seen in all curves and is consistent with previous labor curve studies for term pregnancies. The preterm nulliparous group also appears to have an inflection point at ~6 cm dilation. Feghali et al evaluated labor progress in a cohort of preterm patients undergoing induction of labor and noted an inflection point at 4 to 6 cm dilation across preterm women grouped by gestational age.19 This is in agreement with our findings, although it may differ slightly for nulliparous preterm labors in that our labor curves may indicate a longer latent period for this specific group. This finding is present regardless of the presence of fetal anomaly and can aide obstetricians in labor management for these patients. However, across groups, the latent period is longer in anomalous pregnancies as indicated by the labor curves, as well as the traverse tables with the centimeter to centimeter times from 3 to 6 cm being significantly different among groups evaluated. Preterm women with an anomalous fetus in preterm labor or undergoing induction should be managed with patience in this stage to achieve active phase of labor before considering labor dystocia and CD.
There are limitations to the present study. The labor curves in the present study represent spontaneous and augmented or induced labors; however, the curves were created starting at 3 cm dilation in an attempt to exclude those patients in early latent labor and also in an attempt to replicate the likely cohort of women in labor presenting for management at most institutions today. Today, the onset of active labor is considered closer to 6 cm dilation which is likely a shift from the time of the Consortium on Safe Labor data collection period. Future research is needed to address the specific differences in latent labor between anomalous and nonanomalous pregnancies. The labor curves indicate longer times for latent labor in anomalous pregnancies; however, the data are limited by the low number of cervical exams performed in the latent period. To evaluate the effect that augmentation and induction have on labor progress in the present study, similar curves were created for the augmented and induced labors separately for each of the groups and compared with those included in the current study and showed similar results (Supplementary Figs. 1–4, available in the online version). Augmented and induced laboring patients in our cohort who did not influence the labor curves dramatically were therefore included in our analysis. The interpretation of the labor curves should also take into account the possibility for differences in labor management of patients with anomalous pregnancies, for example, physicians may be more or less aggressive with infusion rates of oxytocin depending on the anomaly and expected outcome. Differences in management of labor and dosing schedules could certainly influence the results of labor progress; however, the cohort evaluated in the present study included spontaneous labor as well as induced and augmented because no difference was seen in the results of the curves when the augmented/induced patients were considered separately to attempt to eliminate this bias. The present study also excluded patients who had <2 cervical exams during their labor course, and this may create bias in excluding some patients who had fast labors. However, the Consortium on Safe Labor dataset is robust in nature and one of the largest datasets containing labor progress information.
We were also unable to further investigate labor curves and progress based on specific fetal anomalies or by specific chromosome abnormality. The dataset includes groupings by ICD-9 diagnosis codes which do differentiate by system (Supplementary Table S1, available in the online version); however, the Consortium dataset includes all major congenital anomalies and chromosome aberrations in one group.
While the dataset is robust in nature, it was collected retrospectively and this must be considered with the interpretation of the data. Labor management, especially with the updates from the subsequent care consensus, Safe prevention of the primary cesarean delivery published in 2012 may have already significantly changed how labor is managed at most institutions today compared with labor management during the collection period of the Consortium on Safe Labor dataset.20,21
However, the Consortium on Safe Labor remains the largest and most contemporary labor cohort dataset available. It is representative of a diverse pregnancy cohort in the United States and also represents multiple labor and delivery settings including both large academic and community hospitals dispersed throughout the country.
The strengths of this study are that this is the first study to evaluate labor patterns in this specific cohort of patients with fetal anomalies. We have observed this cohort as being high risk for CD, as have others previously.10,22 Information about labor progress and noting slower labor progress in patients with fetal anomalies should be taken into consideration before performing cesarean section for arrest disorders. Our analysis was also the first to include both preterm and term patients and compare labor progress in both groups while controlling for important confounders.
In conclusion, the results of the current study indicate that special attention should be given to this unique cohort of patients with pregnancies affected by fetal anomalies to mitigate risk of poor obstetric outcomes, as their labors progress at a slower rate than those not affected by fetal anomalies. Pregnancies affected by fetal anomalies also remain high risk for CD. Generalizable to all patients, with and without anomalous pregnancies, was an inflection point at 6 cm dilation in preterm labor cohorts indicating a clear starting point for the transition from latent to active labor, similar to term women. This is important to take into consideration while managing preterm labor to allow for preparedness among teams caring for the preterm neonate.
Supplementary Material
Fig. 3.
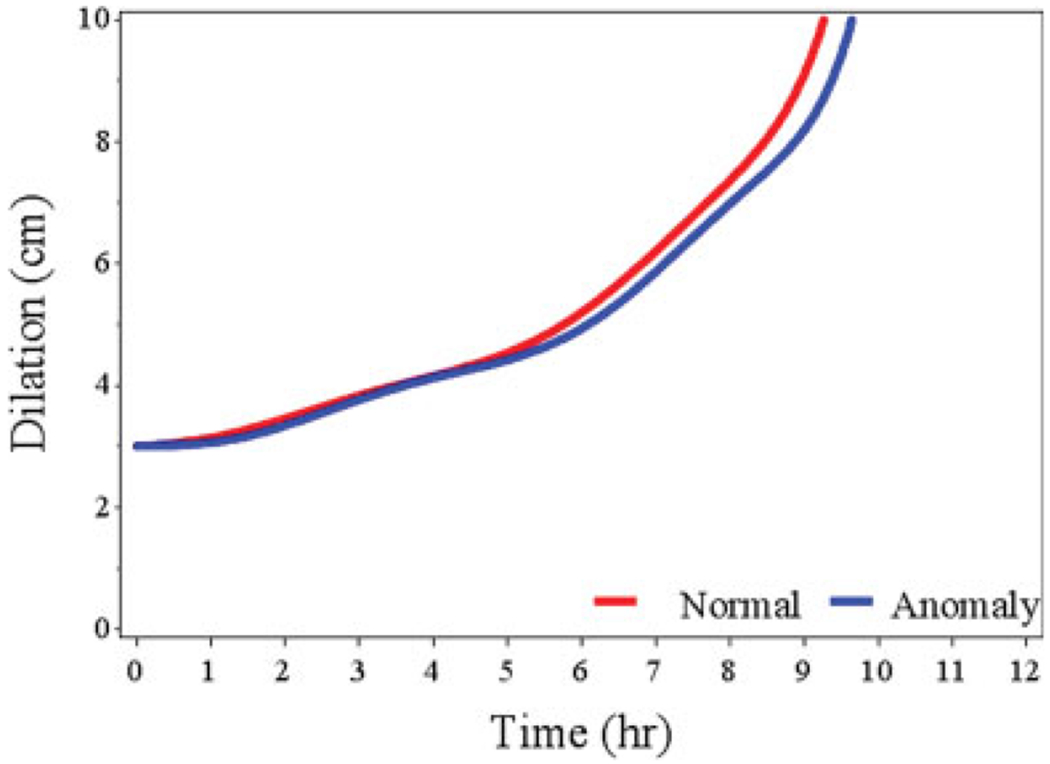
Labor curves for term nulliparous women with dilation in centimeters on the y-axis and time in hours. Blue curve represents anomaly group and red curve represents control group.
Fig. 4.
Labor curves for term multiparous women with dilation in centimeters on the y-axis and time in hours. Blue curve represents anomaly group and red curve represents control group.
Footnotes
Conflict of Interest
None declared.
References
- 1.National Center for Health and Statistics. Birth defects monitoring program. NCfHSBdm. Available at: www.marchofdimes.org/peristats. Accessed February 29, 2016
- 2.Zhang J, Landy HJ, Branch DW, et al. ; Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol 2010;116(06):1281–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang J, Troendle J, Reddy UM, et al. ; Consortium on Safe Labor. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol 2010;203(04):326.e1–326.e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang J, Troendle JF, Yancey MK. Reassessing the labor curve in nulliparous women. Am J Obstet Gynecol 2002;187(04):824–828 [DOI] [PubMed] [Google Scholar]
- 5.Albers LL. The duration of labor in healthy women. J Perinatol 1999;19(02):114–119 [DOI] [PubMed] [Google Scholar]
- 6.Kilpatrick SJ, Laros RK Jr. Characteristics of normal labor. Obstet Gynecol 1989;74(01):85–87 [PubMed] [Google Scholar]
- 7.Neal JL, Lowe NK, Ahijevych KL, Patrick TE, Cabbage LA, Corwin EJ. “Active labor” duration and dilation rates among low-risk, nulliparous women with spontaneous labor onset: a systematic review. J Midwifery Womens Health 2010;55(04):308–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedman E The graphic analysis of labor. Am J Obstet Gynecol 1954;68(06):1568–1575 [DOI] [PubMed] [Google Scholar]
- 9.Sharshiner R, Silver RM. Management of fetal malpresentation. Clin Obstet Gynecol 2015;58(02):246–255 [DOI] [PubMed] [Google Scholar]
- 10.Rossi RM, Divanovic A, DeFranco EA. Obstetric outcomes associated with fetal cyanotic congenital heart disease. Am J Perinatol 2018 [DOI] [PubMed] [Google Scholar]
- 11.Walsh CA, MacTiernan A, Farrell S, et al. Mode of delivery in pregnancies complicated by major fetal congenital heart disease: a retrospective cohort study. J Perinatol 2014;34(12):901–905 [DOI] [PubMed] [Google Scholar]
- 12.Zaki MN, Hibbard JU, Kominiarek MA. Contemporary labor patterns and maternal age. Obstet Gynecol 2013;122(05):1018–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kominiarek MA, Vanveldhuisen P, Hibbard J, et al. ; Consortium on Safe Labor. The maternal body mass index: a strong association with delivery route. Am J Obstet Gynecol 2010;203(03):264.e1–264.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craigo SD. Indicated preterm birth for fetal anomalies. Semin Perinatol 2011;35(05):270–276 [DOI] [PubMed] [Google Scholar]
- 15.Clark SL, DeVore GR, Platt LD. The role of ultrasound in the aggressive management of obstructed labor secondary to fetal malformations. Am J Obstet Gynecol 1985;152(08):1042–1044 [DOI] [PubMed] [Google Scholar]
- 16.Mostello D, Chang JJ, Bai F, et al. Breech presentation at delivery: a marker for congenital anomaly? J Perinatol 2014;34(01):11–15 [DOI] [PubMed] [Google Scholar]
- 17.Shipp TD, Bromley B, Benacerraf B. The prognostic significance of hyperextension of the fetal head detected antenatally with ultrasound. Ultrasound Obstet Gynecol 2000;15(05):391–396 [DOI] [PubMed] [Google Scholar]
- 18.de la Vega A, Verdiales M. High incidence of emergency cesarean section among fetuses with unrecognized chromosomal abnormalities. P R Health Sci J 2001;20(04):347–349 [PubMed] [Google Scholar]
- 19.Feghali M, Timofeev J, Huang CC, et al. Preterm induction of labor: predictors of vaginal delivery and labor curves. Am J Obstet Gynecol 2015;212(01):91.e1–91.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol 2012;120(05):1181–1193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists (College); Society for Maternal-Fetal Medicine. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 2014;210(03):179–193 [DOI] [PubMed] [Google Scholar]
- 22.Dotters-Katz SK, Humphrey WM, Senz KL, Lee VR, Shaffer BL, Caughey AB. The effects of Turner syndrome, 45,X on obstetric and neonatal outcomes: a retrospective cohort evaluation. Am J Perinatol 2016;33(12):1152–1158 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


