Abstract
Purpose
Coronavirus disease-19 (COVID-19) was firstly reported in December 2019 in Wuhan, China and soon after, the number of cases increased rapidly worldwide. As of May 2, 2020, more than 3,000,000 confirmed cases have been reported world. In Macao, there were 45 confirmed COVID-19 cases until May 2, 2020.
Material and Methods
In this study, we summarized the radiological features of these cases and analyzed relationship between the clinical characteristics and radiological findings. We retrospectively analyzed the imaging manifestations of the 45 cases with COVID-19 in Macao, focusing on identifying and characterizing the most common radiological findings of COVID-19. We retrospectively analyze the relationship between the clinical features and radiological finding of COVID-19 pneumonia.
Results
This study showed that chest CT manifestations of COVID-19 were multiple ground-glass densities in both lungs. It is dominated by bilateral peripheral subpleural distribution, which may be accompanied by consolidation, interlobular septa thickening, and adjacent pleura thickening. As the disease progresses, it can manifest as consolidation of the lungs in CT scan. We also found the age, smoking and hypertension may be risk factor for predicting the severity of COVID-19 in radiology.
Conclusion
COVID-19 should be diagnosed based on the clinical feature, nCoV PCR test and radiological manifestation. The main manifestation of COVID-19 is peripheral ground glass opacity. Age, smoking and hypertension may be used to predict the severity of COVID-19. Chest CT is the important radiological method for screening and detecting COVID-19 patients.
Keywords: Coronavirus disease 2019, COVID-19, SARS-CoV-2, Tomography, X-Ray computed, Pneumonia
1. Introduction
In December 2019, cases of unexplained pneumonia were reported in Wuhan, Hubei Province, China. The pathogen isolated from the airway epithelial cells of the infected patients was preliminarily determined to be a new type of coronavirus by the laboratory etiology test [1]. The coronavirus was named severe acute respiratory syndrome coronavirus 2 (SARS−COV-2) and the disease was named as Coronavirus disease-19 (COVID-19) by the World Health Organization (WHO). On January 20, 2020, the National Health Commission issued announcement No.1 to include the novel coronavirus pneumonia into the class B infectious diseases stipulated in Law of the People's Republic of China on the Prevention and Treatment of Infectious Diseases, and adopt the prevention and control measures for class A infectious diseases. On January 22, 2020, the first case of COVID-19 was confirmed in Macao. As of May 2, 2020, a total of 45 COVID-19 cases have been diagnosed in Macao. It has been recently confirmed that SARS−COV-2 infection is the definitive cause of COVID-19. SARS−COV-2 is a member of the genus β−COronavirus, which is one of the genera of coronaviruses. Coronavirus is an enveloped single-stranded RNA virus found in human, many other mammals and birds. The virus is associated with lung, liver, central nervous system and intestinal diseases. However, the natural host of SARS−COV-2 has not been determined [2]. Coronaviruses belong to the family Coronaviridae and the order Nidovarales. There are six known coronaviruses related to human diseases, in which severe acute respiratory syndrome coronavirus (SARS CoV) and Middle East respiratory syndrome coronavirus (MERS CoV) are zoonoses and sometimes cause fatal illness. The other four spread widely in human society and can cause mild upper respiratory infections.
In this study, we aimed to analyze the imaging characteristics further explore the relationship between the clinical features and the radiological findings.
2. Materials and methods
A total of 45 COVID-19 patients admitted to our hospital from January 22, 2020 to May 2, 2020 were enrolled in this study. Their real time polymerase chain reaction (PCR) test results were positive for 2019-nCoV. Demographic characteristics (age, gender, clinical information) were collected and shown in Table 1. 44 cases of them have history of traveling abroad, 1 Macao resident had contact history of COVID-19 patient locally. This study was approved by the ethical committee of our hospital.
Table 1.
Demographic Characteristics (N = 45).
| Characteristics | N | Percentage (%) |
|---|---|---|
| Age (years) | ||
| Mean ± SD | 48.4 ± 16.5 | |
| Sex | ||
| Male | 26 | 58 |
| Female | 19 | 42 |
| Race | ||
| East Asian | 35 | 78 |
| Hispanic | 5 | 11 |
| Southeast Asian | 5 | 11 |
| Travelling history | ||
| Australia | 1 | 2.2 |
| Cambodia | 1 | 2.2 |
| China | 9 | 20 |
| Indonesia | 3 | 6.7 |
| Ireland | 1 | 2.2 |
| Macao | 1 | 2.2 |
| Philippines | 5 | 11.1 |
| Portugal | 4 | 8.9 |
| Spain | 1 | 2.2 |
| Thailand | 1 | 2.2 |
| United Kingdom | 15 | 33.3 |
| United State of America (USA) | 3 | 6.8 |
| Symptoms | ||
| Fever | 28 | 62.2 |
| Cough | 16 | 35.6 |
| Runny nose | 6 | 13.3 |
| Sore throat | 6 | 13.3 |
| Diarrhea | 3 | 6.6 |
| Myalgia | 3 | 6.6 |
| Headache | 2 | 4.4 |
| Anosmia | 1 | 2.2 |
| Fatigue | 1 | 2.2 |
| Abdominal pain | 1 | 2.2 |
| Asymptomatic | 8 | 10 |
All patients were performed with 1.25 mm and 5 mm slice thickness on Revolution CT (GE medical Systems, Milwaukee, WI). All chest computed tomography (CT) images were reviewed and interpreted by well-trained radiologists independently in our hospital. The following CT signs of each patient was evaluated: 1) ground glass opacity (GGO), 2) consolidation, 3) the number of lobes involved by the GGO or consolidation, 4) other pulmonary abnormality such as cavitation, nodules, pleural effusion, thoracic lymphadenopathy, potential lung diseases such as emphysema, fibrosis etc.
The follow-up chest imaging was evaluated and compared with the initial images. In addition, COVID-19 patients were divided into two groups based on the initial chest imaging: positive radiological finding and negative radiological group. Positive radiological finding was defined as the presence of GGO and/or consolidation in the initial chest CT scan. Negative radiological finding was defined as the absence of GGO and/or consolidation.
We also interpreted the chest CT of each patient with CT severity score. Each lung lobe was graded: 0: no involvement; 1: < 5% involvement; 2: 5 %–25 % involvement; 3: 26 %–49 % involvement; 4: 50 %–75 % involvement; 5: > 75 % involvement. The total score of the five lung lobes is the lesion score of each patient with the range of 0 (no involvement) to 25 (maximum involvement). The data was analyzed using Shapiro-Wilk test and chi-square test. A p less than 0.05 was considered statistically significant.
3. Results
A total of 45 patients (26 male and 19 female) were enrolled in this study with a mean age of 34.4 ± 16.5 years. Demographic characteristic (age, gender, clinical information) was shown in the Table 1. 44 patients had a history of traveling and 1 had a history of close contact with one confirmed patients who was the Macao resident and had no traveling history. Of these patients, fever is the most common symptoms (28 patients), followed by cough (16 patients). Other symptoms including headache, dizziness, diarrhea and other upper respiratory symptoms were also noted in our cases. In addition, there were eight cases in our study who were asymptomatic but they were close contactors. All of the 45 patients were diagnosed with COVID-19 by the 2019 nCoV PCR test and were admitted to our hospital for further treatment.
3.1. GGO and consolidation
All COVID-19 patients were performed the chest CT after diagnosis. The average CT severity score of the initial images was 3.47. In the 45 cases, 21 cases had no significant GGO or consolidation in the initial chest CT scan. The other 24 cases were found the presence of GGO (Fig. 1) in which, 2 cases had both GGO and consolidation, while 22 had only GGO (Table 2).
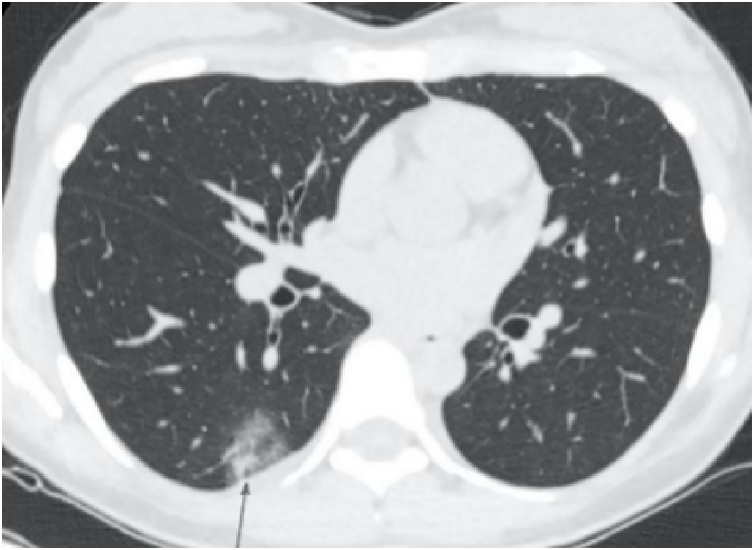
Fig. 1.
An axial non-contract chest CT (first time) of 29-year-old female with COVID demonstrating ground glass opacity in the subpleural region of right lower pulmonary lobe.
Table 2.
Initial Chest CT Findings of COVID-19 Patients.
| Initial Chest CT Finding | N | Percentage (%) |
|---|---|---|
| GGO and consolidation | ||
| Absence of both GGO and consolidation | 21 | 46.7 |
| Presence of GGO | 22 | 48.9 |
| Presence of GGO with Consolidation | 2 | 4.4 |
| Presence of consolidation without GGO | 0 | |
| Number of lobes involved | ||
| None | 21 | 46.7 |
| One | 4 | 8.9 |
| Two | 9 | 20 |
| Three | 2 | 4.4 |
| Four | 2 | 4.4 |
| Five | 7 | 15.6 |
| More than 2 lobes involved | 20 | 44.4 |
| Bilateral lungs involved | 16 | 35.6 |
| Location of Lobe Involvement | ||
| Left upper lobe | 13 | 28.9 |
| Left lower lobe | 18 | 40 |
| Right upper lobe | 12 | 26.7 |
| Right middle lobe | 10 | 22.2 |
| Right lower lobe | 18 | 40 |
| Opacification distribution and Patterns | ||
| Round morphology | 22 | 48.9 |
| Linear opacities | 1 | 2.2 |
| Crazy paving pattern | 1 | 2.2 |
| Peripheral distribution | 24 | 53.3 |
| Cavitation | 0 | |
| Other findings | ||
| Separate pulmonary nodules | 4 | 8.8 |
| Hilar lymphadenopathy | 1 | 2.2 |
| Pleural effusion | 2 | 4.4 |
| Pulmonary emphysema | 3 | 6.6 |
| Pulmonary fibrosis | 4 | 8.8 |
GGO = ground glass opacities.
3.2. Opacification distribution and patterns
As mentioned before, 21 cases were found negative radiological finding in the initial chest CT scan. In the positive radiological finding group, 20 of the 24 cases were found to have at least two involvement, 4 with only one segment involved which mainly concentrated in the lower pulmonary lobe (2 were found the involvement in the left lower lobe and 2 in the right lower lobe), and 7 of them showed involvement in all of the five lobes (Table 2).
In the initial chest CT examination, there were 16 cases of bilateral lungs involvement. The most common lobe involvement were right upper lobe and left lower lobe, both of which were 18 cases, accounted for 75 % of the total 24 chest CT abnormal cases, followed by the left upper lobe, accounting for 51.2 % (13 of 24), while the right middle lobe is the least, accounting for 41.7 % (10 of 24) (Table 2).
In patterns of opacities, 22 of the 24 patients with positive radiological finding showed round morphology. 1 case showed a linear opacity and 1 showed a crazy-paving pattern. 24 cases of abnormal chest CT demonstrated peripheral distribution. In our case, there were 4 cases with pulmonary nodules, 1 case with hilar lymphadenopathy, 2 cases with mild pleural effusion, 3 cases with emphysema and 4 cases with pulmonary fibrosis (Table 2).
3.3. Follow-up chest imaging
Besides the initial chest CT, all COVID-19 cases were performed 2 follow-up chest CT scans. The average interval between the first and second CT scan was 5.7 days. The average CT severity score of the first and second follow-up chest CT were 5.89 and 3.12, respectively. Of the 21 cases with normal chest CT at the initial scan, 6 cases detected several GGOs in the both lungs at the follow-up chest CTs (Fig. 2) and the remaining 15 had no GGO or consolidation. All follow-up chest CT showed mild progression in 12 patients during admission, mainly manifested by the enlargement of lesions and/or the expansion of the combined scope (Fig. 3, Fig. 5). One case was detected with thickened interlobular and intralobular septa (crazy paving pattern) in the first follow-up CT (Fig. 6). Compared with first follow-up chest CT, the second revealed that 11 patients had improved lung involvement, showing smaller lesions or completely absorption (Fig. 4) and 10 cases appeared the fibrotic stripes in both of their lungs (Table 3).
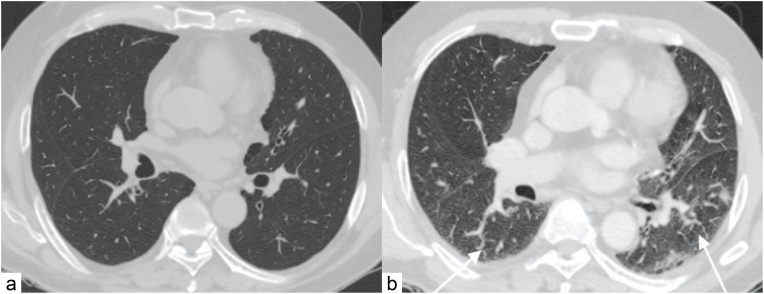
Fig. 2.
(a) An axial non-contrast chest CT (1 st time) of 66-year-old male with COVID-19 demonstrated normal. (b) An axial chest CT of the same patient performed 3 days after admission due to clinical condition progression, showing several new GGOs appeared in the both lungs, predominately in the left lung (white arrows).
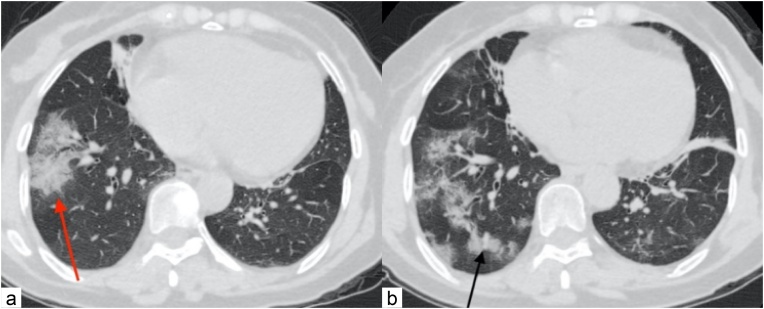
Fig. 3.
(a) Axial noncontract chest CT (1 st time) of 64-year-old female with COVID-19, demonstrating a few quasi-circular GGOs in the right lung (red arrow). (b) Axial noncontract chest CT of the same patient 9 days after admission due to progression of the illness demonstrated the GGO increased in quantity and expansion of lung involvement (black arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
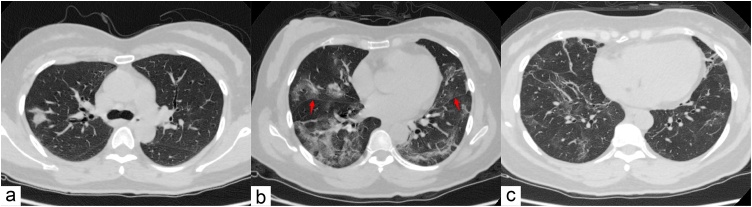
Fig. 5.
(a) Axial noncontract chest CT of a 57-year-old male with COVID-19 showed a few ground glass opacities (GGO) in the both lower pulmonary lobes and left lingular lobe. (b) Axial noncontract chest CT of this patient after 7 days of treatment indicated both the size and quantity of the aforementioned GGO had increased. (c) The chest CT after 23 days of treatment suggested the GGO were absorbed and a few fibrotic stripes were noted in the previous regions of both lungs.
Fig. 6.
(a) Axial noncontract chest CT of a 50-year-old female with COVID-19 displayed several ground glass opacities (GGO) in the whole lungs. (b) The CT performed 8 days after hospitalization showed the consolidation of the involved lung parenchyma, thickness of interlobular and intralobular septa (crazy paving pattern) noted (arrow). (c) CT after 40 days of hospitalization showed the aforementioned consolidation and GGO were almost absorbed and some fibrotic stripes were noted at the both lungs.
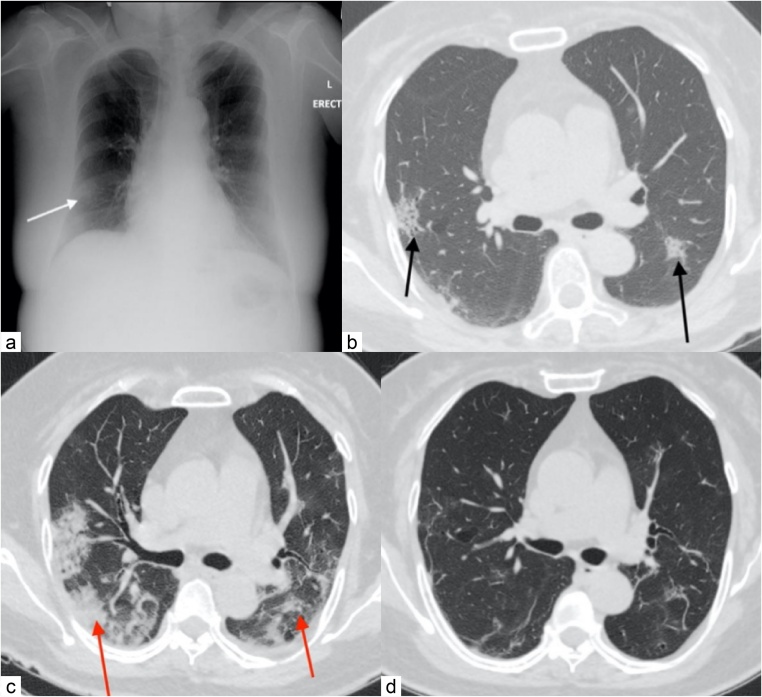
Fig. 4.
(a) Erect chest radiography of 57-year-old female with COVID-19 demonstrated a focal opacity in the right lower lung zone (white arrow). (b) Axial noncontract chest CT (1 st time) of the same patient showed a few GGOs in the both lungs (black arrows). (c) Axial noncontract chest CT of the same patient 10 days after admission due to progression of the disease demonstrated GGOs increased in quantity and size, accompanied with consolidation (red arrows). (d) Axial noncontract chest CT of this patient after 21days of treatment demonstrated the aforementioned the GGO and consolidation absorbed, and some fibrotic stripes noted in the corresponding region of the both lungs. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Table 3.
Follow up CT Findings of COVID-19 patients.
| Follow up CT Finding | 1st follow up CT | 2nd follow up CT |
|---|---|---|
| Normal | 15 | 15 |
| Increased and progression | 17 | 1 |
| Decreased and regression of involved region | 13 | 8 |
| Completed absorption | 0 | 11 |
| Fibrotic stripes | 0 | 10 |
| Total | 45 | 45 |
CT = computed tomography.
3.4. Risk factor prediction
The patients were categorized into positive radiological finding and negative radiological group. The demographic characteristics of these two groups were analyzed to explore the potential risk factor of the COVID-19. The results indicated the age might be a risk factor for severity of the pneumonia. The mean age of patients with positive radiological finding was 43.79 ± 15.15, which was significantly higher than that of the patients with positive radiological finding (23.62 ± 10.50) (p < 0.05). There was no significant difference in the gender and race between these two groups (Table 4). The symptoms between two groups also showed no significant difference in statistics (Table 5). In underlying disease analysis, we found that smoking might be related to the severity of the COVID-19 pneumonia (p < 0.05). The severity of COVID-19 in hypertension patients was also higher than that without hypertension (p < 0.05). Diabetes mellitus and dyslipidemia were not related to the severity of COVID-19 pneumonia (Table 6).
Table 4.
Relationship between Demographic Characteristics and Radiological Findings of COVID-19 Patients.
| Factor | Negative radiological finding group (n = 21) | Positive radiological finding group (n = 24) | P |
|---|---|---|---|
| Age | 23.62 ± 10.50 | 43.79 ± 15.15 | 0.000 |
| Gender | |||
| M | 12 (57.1 %) | 14 (58.3 %) | 0.936 |
| F | 9 (42.9 %) | 10 (41.7 %) | |
| Race | |||
| East Asian | 14 (66.7 %) | 21 (87.5 %) | 0.188 |
| Hispanic | 4 (19.0 %) | 1 (4.2 %) | |
| Southeast Asian | 3 (14.3 %) | 2 (8.3 %) |
Table 5.
Relationship between Symptoms and Radiological Findings of COVID-19 patients.
| Factor | Negative radiological finding group (n = 21) | Positive radiological finding group (n = 24) | P | |
|---|---|---|---|---|
| Abdominal pain | No | 21 (100.0 %) | 23 (95.8 %) | 1.000 |
| Yes | 0 (0.0 %) | 1 (4.2 %) | ||
| Anosmia | No | 20 (95.2 %) | 24 (100.0 %) | 0.467 |
| Yes | 1 (4.1 %) | 0 (0.0 %) | ||
| Cough | No | 16 (76.2 %) | 13 (54.2 %) | 0.124 |
| Yes | 5 (23.8 %) | 11 (45.8 %) | ||
| Dizziness | No | 21 (100.0 %) | 23 (95.8 %) | 1.000 |
| Yes | 0 (0.0 %) | 1 (4.2 %) | ||
| Diarrhea | No | 21 (100.0 %) | 21 (87.5 %) | 0.236 |
| Yes | 0 (0.0 %) | 3 (12.5 %) | ||
| Fatigue | No | 21 (100.0 %) | 23 (95.8 %) | 1.000 |
| Yes | 0 (0.0 %) | 1 (4.2 %) | ||
| Fever | No | 7 (33.3 %) | 10 (41.7 %) | 0.565 |
| Yes | 14 (66.7 %) | 14 (58.3 %) | ||
| Headache | No | 19 (90.5 %) | 24 (100.0 %) | 0.212 |
| Yes | 2 (9.5 %) | 0 (0.0 %) | ||
| Muscle pain | No | 20 (95.2 %) | 22 (91.7 %) | 1.000 |
| Yes | 1 (4.1 %) | 2 (8.3 %) | ||
| Runny nose | No | 18 (85.7 %) | 21 (87.5 %) | 1.000 |
| Yes | 3 (14.3 %) | 3 (12.5 %) | ||
| Skin rash | No | 19 (90.5 %) | 24 (100.0 %) | 0.212 |
| Yes | 2 (9.5 %) | 0 (0.0 %) | ||
| Sore throat | No | 16 (76.2 %) | 23 (95.8 %) | 0.135 |
| Yes | 5 (23.8 %) | 1 (4.2 %) | ||
| Toothache | No | 20 (95.2 %) | 24 (100.0 %) | 0.467 |
| Yes | 1 (4.1 %) | 0 (0.0 %) | ||
| Asymptomatic | No | 16 (76.2 %) | 21 (87.5 %) | 0.549 |
| Yes | 5 (23.8 %) | 3 (12.5 %) | ||
Table 6.
Relationship between Chronic Illness and Radiological Findings of COVID-19 Patients.
| Factor | Negative radiological finding group (n = 21) | Positive radiological finding group (n = 24) | P | |
|---|---|---|---|---|
| Smoking | No | 20 (95.2 %) | 16 (66.7 %) | 0.043 |
| Yes | 1 (4.8 %) | 8 (33.3 %) | ||
| Diabetes mellitus | No | 21 (100.0 %) | 20 (83.3 %) | 0.151 |
| Yes | 0 (0.0 %) | 4 (16.7 %) | ||
| Hypertension | No | 21 (100.0 %) | 18 (79.2 %) | 0.043 |
| Yes | 0 (0.0 %) | 6 (20.8 %) | ||
| Hepatitis B infection | No | 21 (100.0 %) | 23 (95.8 %) | 1.000 |
| Yes | 0 (0.0 %) | 1 (4.2 %) | ||
| Dyslipidemia | No | 21(100.0 %) | 21 (87.5 %) | 0.236 |
| Yes | 0 (0.0 %) | 3 (12.5 %) | ||
4. Discussion
The COVID-19 has spread rapidly throughout China and around the world in two months since its occurrence in Wuhan in December 2019. As of May 2, 2020, the number of confirmed infections in the world has exceeded 3,000,000 and the number of deaths has exceeded 200,000 [3]. This disease mainly affects the epithelial cells of the upper respiratory tract and in severe cases can lead to respiratory failure. Besides medical history, physical examination and virological test (2019 nCoV PCR), radiological examination is also important.
Radiological examination is one of the quick and convenient methods for the diagnosis of COVID-19. Chest radiograph is a fast and simple imaging method. Some reports indicated that chest X-ray examination had a high rate of misdiagnosis for lesions in the early stage or changes in ground glass density [4]. In some medical settings with high incidence of COVID-19 but limited resources, chest radiographs could be used as the first-line screening tool [5]. Huang C et al. summarized and the clinical characteristics of 41 newly diagnosed patients in Wuhan and published the article in the LANCET journal which indicated the laboratory confirmed COVID-19 caused serious diseases similar to the clinical SARS. In the study, 13 of 41 (32 %) were admitted to hospital and 6 (15 %) died. In addition, abnormalities in chest CT were found in 41 patients with pneumonia which mainly was the abnormal opacities in bilateral lungs of each patient [6]. The advantage of CT, especially the high resolution computed tomography (HRCT), is that it has high spatial resolution and not affected by structures other than layers. It uses post-processing techniques to display the details of the lesion in multiple planes and directions. Therefore, CT examination plays an important role in the diagnosis of new viral pneumonia, and the basis of clinical diagnosis is included in the National Health and Health Commission's “Pneumonitis Diagnosis and Treatment Program for New Coronavirus Infection (fifth version)” [7].
A recent paper published by Shi et al. pointed out that the chest radiography showed no abnormality, bronchitis or bronchiolitis that showed bilateral bronchial thickening and interstitial infiltration at the early stage of the disease [8]. While the lesions were obvious, multiple patchy or patchy opacities appeared in both lungs and the lesions were serious, there were diffuse consolidation detected in both lungs. In our study, the chest radiography of 8 cases were normal but their chest CT showed GGO. 10 cases were detected the patchy opacities in chest radiography and chest CT confirmed GGO in their both lungs. We believe that chest radiography in the early stage of COVID-19 is not specific.
Guan et al. published an article recently reporting the CT features of COVID-19 [4]. COVID-19 can be classified into 4 stages that based on the COVID treatment guideline (fifth edition) that published by National Health and Health Commission on 5 Feb 2020: early, common, severe and fetal stage [7]. Common manifestations: single or multiple lung multiple, patchy or segmental GGO, grid-like texture in most lesions (cobblestone sign); the lesions distributed along the bronchial vascular sub-pleural in the base of the lung are predominant, with air bronchus signs, with or without lobular septal thickening, a small number with interlobular pleural thickening, and very few with a small amount of pleural and/or pericardial effusion.
Chung et al. analyzed the chest CT of 21 cases with COVID-19 and summarized the CT features which showed that 12 cases had GGO and 6 had consolidation. Besides, they found that most of these cases had more than two lung lobe involvement (15 of 21, 71 %) and bilateral lung involvement (16 of 21, 76 %) [5]. A study analyzing 50 COVID-19 cases by Song et al. found bilateral GGO in peripheral region (85 %) and posterior region of lungs (82 %). They also investigated the consolidation of patient who had been sick more than 5 days and the results showed the older the patients had, the more consolidation they had [9].
Lomoro et al. published an article recently which evaluated chest imaging manifestations of 58 COVID-19 patients with the conventional radiology, chest ultrasound and chest CT. Chest CT showed bilateral and multilobar GGO have predominately peripheral distribution. They also pointed out some other imaging features including crazy paving pattern, fibrous stripes, subpleural lines, architectural distortion and air bronchogram sign. Besides, enlarged lymph node and pleural effusion were observed in their study. In addition, chest ultrasound showed diffuse B line and subpleural consolidation in the patients [10].
In our study, there were 22 cases with GGO in the initial chest CT, 2 cases of which had both GGO and consolidation. We also found that the bilateral lower lobes were the most common affected lobes (40 %). Multiple GGO with peripheral distribution could be found in 16 of our patients. 22 cases showed round morphology, 6 showed linear opacities and 1 showed crazy paving pattern. Other pulmonary abnormalities were found in our patients, such as pulmonary nodule, pleural effusion, pulmonary emphysema, pulmonary fibrosis and hilar lymphadenopathy (Table 2). There was no death in our study.
The correlation of the clinical features with radiological findings was further analyzed in our study. Age was found to be a potential risk factor of the severity of the COVID-19. The age of patients with imaging manifestations was significantly higher than that without imaging manifestations (43.79 ± 15.15 vs 23.62 ± 10.50, p < 0.05). The relationship between the symptoms and radiological finding was not statistically significant, but the chest CT findings of 3 asymptomatic cases were positive. In addition, smoking and hypertension might be used to predict the severity of pneumonia in radiology (p < 0.05). Smoking may damage the alveolar epithelial cells, leading to the loss of protection in airway.
We also found the chest CT might be the better radiological modality for the follow up evaluation. The follow-up chest radiography in our study suggested 5 cases improved because of the opacities regression and the follow-up chest CT showed the aforementioned GGO in previous CT was still noted but the size and extent were reduced. CT can also be applied to patients with renal insufficiency, especially in patient with CKD stage 4 or below. Jajodia et al. found chest CT was very useful for assessing the severity and progression of COVID-19, especially in moderated and severe cases due to the high mortality rate in these two groups. However, it was not recommended in the asymptomatic and mild COVID-19. In addition, they also pointed out that chest CT could be used to evaluate the complication of COVID-19 such as bacterial superinfection, pulmonary effusion and heart failure [11]. In our study, there were 17 patients developing progression of GGO or consolidation in the first follow-up CT and 16 of them showed regression of GGO in the second follow up. One patient presented with mild symptoms on the first day of the hospitalization and subsequently developed shortness of breath and hypoxemia. The patient was then transferred to ICU and the chest CT showed consolidation with interlobar thickening. Patient recovered well after adjustment of treatment. The chest CT before discharge showed GGO and consolidation were almost absorbed and there were a few fibrotic stripes in the both lungs.
The main feature of COVID-19 is GGO, but it is not specific. It must be distinguished from other infectious and non-infectious lung diseases. 1) Other viral pneumonia manifests as diffuse GGO. It is difficult to distinguish COVID-19 from the viral pneumonia in radiology and clinical practice [12,13]. 2) Bacterial pneumonia manifests as a small piece of opacity distributed along the bronchi, which can fuse into a large focus or large piece of consolidation [14]. 3) Non-infectious lesions need to be distinguished from cryptogenic organizing pneumonia (COP). COP lesions are characteristically distributed peripherally or around the bronchi. The lower lobe of the lungs is more susceptible and the density can change from ground glass to consolidation [15,16].
There are some limitations in our research. Firstly, the sample is small (45 patients). In addition, the CT follow-up interval is short and lack of long term follow up, because some patients return to their hometown and miss follow up. Secondly, the number of severe cases is less and most are mild cases, so there is no comparison severe infections and mild infections. Thirdly, there are several pediatric patients in this study. Finally, no lung biopsy can be used to study the correlation between radiological and pathological findings.
In summary, the diagnosis of COVID-19 is mainly based on clinical history, exposure history, and 2019 nCoV PCR examination. But radiological examination is also an important modality. The imaging characteristics of COVID-19 chest CT is multiple GGO or accompanied by consolidation. The fibrotic stripes and complete absorption may indicate a good prognosis. Although 2019 nCoV PCR test is the current gold standard for diagnosis of COVID-19, more literature has found more "false negative" cases [17]. Therefore, COVID-19 need to be accurately diagnosed combining various aspects. Age, smoking and hypertension may be the risk factors and the potential indicators for predicting the severity of the disease, but more cases are needed to prove the accuracy. In addition, CT scan is a good radiological modality for screening and detecting the progression of COVID-19, especially in high risk, asymptomatic cases.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
This study was approved by the ethical committee of the Centro Hospitalar Conde de São Januário and consent form was waived as it was retrospective.
CRediT authorship contribution statement
Chon Man Ieong: Conceptualization, Date curation, Writing - original draft, Writing - review & editing. Xi Xu: Conceptualization, Visualization, Investigation, Writing - review & editing. Soi Chau Kong: Supervision, Writing - review & editing. Liangping Luo: Methodology, Software, Validation.
Declaration of Competing Interest
The authors do not have any competing interests to declare.
References
- 1.Xu X., Chen P., Wang J., Feng J., Zhou H., Li X., Zhong W., Hao P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020;63:457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization, Novel Coronavirus (2019-nCov). https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200502-covid-19-sitrep-103.pdf?sfvrsn=d95e76d8_4, (accessed 2 May, 2020).
- 4.Guan H., Xiong Y., Shen N., Fan Y., Shao J., Li H., Li X., Hu D., Zhu W., Jin Z. Clinical and thin-section CT features of patients with 2019-nCoV-pneumonia in Wuhan. Radiologic Practice. 2020:125–130. doi: 10.13609/j.cnki.1000-0313.2020.02.001. [DOI] [Google Scholar]
- 5.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., Cui J., Xu W., Yang Y., Fayad Z.A., Jacobi A., Li K., Li S., Shan H. CT imaging features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Health and Health Commission . 2020. Pneumonia Diagnosis and Treatment Plan for New Coronavirus Infection (fifth Version)http://www.nhc.gov.cn/yzygj/s7653p/202002/3b09b894ac9b4204a79db5b8912d4440/files/7260301a393845fc87fcf6dd52965ecb.pdf (accessed 5 Feb. 2020) [Google Scholar]
- 8.Shi H., Han X., Fan Y., Liang B., Yang F., Han P. Radiologic features of patients with 2019-nCoV infection. J. Clin. Interv. Radiol. Isvir. 2020;39:8–11. doi: 10.13437/j.cnki.jcr.20200206.002. [DOI] [Google Scholar]
- 9.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H., Ling Y., Jiang Y., Shi Y. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lomoro P., Verde F., Zerboni F., Simonetti I., Borghi C., Fachinetti C., Natalizi A., Martegani A. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur. J. Radiol. Open. 2020;7:100231. doi: 10.1016/j.ejro.2020.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jajodia A., Ebner L., Heidinger B., Chaturvedi A., Prosch H. Imaging in corona virus disease 2019 (COVID-19)—a scoping review. Eur. J. Radiol. Open. 2020;7:100237. doi: 10.1016/j.ejro.2020.100237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koo H.J., Lim S., Choe J., Choi S.-H., Sung H., Do K.-H. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38:719–739. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 13.Franquet T. Imaging of pulmonary viral pneumonia. Radiology. 2011;260:18–39. doi: 10.1148/radiol.11092149. [DOI] [PubMed] [Google Scholar]
- 14.Garg M., Prabhakar N., Gulati A., Agarwal R., Dhooria S. Spectrum of imaging findings in pulmonary infections. Part 1: bacterial and viral. Pol. J. Radiol. 2019;84:205–213. doi: 10.5114/pjr.2019.85812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee K.S., Kullnig P., Hartman T.E., Müller N.L. Cryptogenic organizing pneumonia: CT findings in 43 patients. Am. J. Roentgenol. 1994;162:543–546. doi: 10.2214/ajr.162.3.8109493. [DOI] [PubMed] [Google Scholar]
- 16.Ujita M., Renzoni E.A., Veeraraghavan S., Wells A.U., Hansell D.M. Organizing pneumonia: perilobular pattern at thin-section CT. Radiology. 2004;232:757–761. doi: 10.1148/radiol.2323031059. [DOI] [PubMed] [Google Scholar]
- 17.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. 200343. [DOI] [PMC free article] [PubMed] [Google Scholar]