Abstract
Rationale
COVID-19 is likely to be stigmatized. The people of Hubei province perceived courtesy and affiliate stigma due to the geographic linkage to COVID-19. Perceived courtesy stigma refers to the perception of stigma of people who are associated with COVID-19 (e.g., the geographic linkage). Affiliate stigma is the internalization and psychological responses of perceived courtesy stigma among the associates.
Objective
The current study aims to reveal different patterns of perceived courtesy and affiliate stigma among people who are at high risk of contagion of COVID-19, and to examine the possible risk factors.
Method
A sample including 2813 adults who located in Hubei Province, China (female: n = 2,184, 77.64%; male: n = 629, 22.36%; mean age = 37.85 years, SD = 6.61 years, range = 18–63 years) were employed in the current study, using latent profile analysis for searching stigma profiles.
Results
Three profiles of stigma were found: the “Denier” (35.98%), “Confused moderate” (48.13%) and “Perceiver” (15.89%) displaying the low, moderate and high level of perceived courtesy and affiliate stigma, respectively. Multinomial logistic regression analyses revealed that generally people with a high level of education, perceived threats, anxiety symptoms, and familiarity with quarantined cases have a high likelihood to be distributed into the “Perceiver”.
Discussion and Conclusions
Our findings highlight the issues of COVID-19-related stigma and provide evidence for launching effective health actions to promote a cohesive society and culture of health. The media can transmit scientific knowledge, promote positive interactions and social cohesion between the stigmatized group and the dominant group, and create spaces for stories that nurture group identification among the implicated people. Future studies should use more representative sample and improve the measures.
Keywords: COVID-19, Stigma, Courtesy stigma, Affiliate stigma, Latent profile analysis, Hubei
Highlights
-
•
People at high risk of contagion of COVID-19 may experience stigma.
-
•
Stigma may concern perceived courtesy and/or affiliate stigma.
-
•
Three distinct profiles of stigma were identified.
-
•
Risk factors were measured at the interface of individuals and the community.
1. Introduction
On January 30, 2020, the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) as a pandemic and a Public Health Emergency of International Concern (PHEIC). COVID-19 is likely to be stigmatized (Bagcchi, 2020). The stigma associated with diseases can drive individual and societal burdens. Disease-related stigma can cause suffering to those who are stigmatized; these individuals may reduce their help-seeking behaviors, thus increasing the challenge for public health efforts to combat the disease or condition (Jarlais et al., 2006; Link and Phelan, 2006). Stigma may generate an adverse influence (e.g., burnout) to professional health care workers, volunteers, families, and communities who may be associated with the infected patients (Smith Morris, 2017). For affected areas and countries, the stigma can cause economic loss, regional discrimination, and racism (Budhwani and Sun, 2020; Messer et al., 2006). Thus, stigma is an important issue for all people in the battle against COVID-19.
1.1. COVID-19 stigma
Stigma has been defined as an attribute or characteristic that conveys a social identity, which is devalued in a particular social context (Gilbert et al., 1998, p. 505). The disease characteristics (e.g., the severity and contagion) may drive the COVID-19 stigma (Crandall, 1991). The person-to-person transmission chains, relatively long incubation period and some asymptomatic cases of COVID-19 triggered great fear among the public that the virus is highly contagious, fatal, and uncontrollable (Tian et al., 2020; World Health Organization, 2020; Wu and McGoogan, 2020). The occurrence of transmission in family, community, and healthcare settings may also strengthen the feelings of threats and risks. COVID-19 poses a public health risk and increases the susceptibility of most individuals without any hygienic precaution (e.g., wearing a mask, physical distancing, and thoroughly cleaning hands) to be infected. These have caused people to revert to instinctual behavioral responses, in which people naturally avoid and isolate individuals and groups who are likely to be infected with COVID-19 (e.g., people who live in or have traveled to Hubei province), as a defense against infectious diseases (Faulkner et al., 2004). Avoidance behavior objectively reduces exposure to risk, but it may also end up stigmatizing people, places, or things (Johnson, 2019; Reluga et al., 2019).
Moreover, the stigma affects not only individuals with the stigmatizing attributes (e.g., people who have COVID-19) but also those who are associated with them (e.g., family members, service providers, and community members). The stigma-in-association has been labeled courtesy stigma, which refers to the perceived and experienced stigma of the associates from the general public toward themselves (Goffman, 1963). The internalization of stigma among associates of chastised attributes has been defined as affiliate stigma, which describes the extent of self-stigmatization and the corresponding cognitive (e.g., low self-worth), affective (e.g., feeling shame), and behavioral responses (e.g., self-denigration) of the associates (Mak and Cheung, 2008; Mitter et al., 2019; Shi et al., 2019).
Such associations may be based on genetic, contagion, moral, ethnic, and/or geographical reasons (Lee et al., 2005). The phenomenon of courtesy stigma due to the perceived linkage between infectious diseases and the geographic areas has been observed in residents of Amoy Gardens, the first officially recognized site of the community outbreak of SARS in Hong Kong (Lee et al., 2005). During the outbreak of COVID-19, Hubei is the region affected worst by the coronavirus within China, with approximately 65,000 people who acquired COVID-19 and 3000 deaths. The people of Hubei province have perceived courtesy and affiliate stigma due to the geographic linkage to COVID-19.
Targeted individuals may perceive different patterns and levels of courtesy and affiliate stigma, such as someone susceptible to courtesy and affiliate stigma and others who are not. These variations may be due to a lack of acceptance of the stigmatized identity, or a psychological mechanism, by which the individual attempts to maintain self-worth or individual coping strategies (Ali et al., 2012; Festinger, 1954). Previous studies often use variable-centered approaches, which may mask the heterogeneous profiles of potentially infected individuals (e.g., Hubei people). Latent profile analysis (LPA) is a person-centered approach, which is a data-driven statistical protocol that identifies clusters among individuals through Maximum Likelihood (ML) estimation (Bauer and Curran, 2004). The present study aims to reveal different patterns of perceived courtesy and affiliate stigma among Hubei people, using LPA to group the target individuals into different profiles, each of which contains individuals who are similar to each other and different from individuals in other profiles (B. O. Muthén and Muthén, 2000).
1.2. Risk factors for COVID-19 stigma
The second purpose of this study is to specify which risk factors are related to which profile. Pescosolido, Martin, Lang, and Olafsdottir (2008) have synthesized the variety of theoretical influences on stigma and promoted the cross-discipline Framework Integrating Normative Influences on Stigma (FINIS), which posits several possible triggers of stigma at the interface of the community and individual levels.
At the individual level, social and disease characteristics combine to shape the evaluation of the probability that a person can be easily identified by others as a person getting illness (Pescosolido et al., 2008). Researchers have called for an analysis of the relationship between social characteristics (e.g., gender and age) and COVID-19 stigma (Logie, 2020). FINIS also points out that individuals could experience self-stigma through social psychological and cognitive processes (e.g., anxiety and attribution of the disease). At the community level, information about COVID-19 learned from media context (e.g., exposure) will be a source of stigmatization, which influences people's judgments when they encounter situations related to COVID-19 (Pescosolido et al., 2008). Particularly, heavy media users construct their view of what people and places are like through information learned from media (Pescosolido et al., 2008). In addition to media exposure, the real-life exposure (i.e., “contact” with persons with diseases) has been thought to be a potential risk factor at the meso-level and is expected to have direct effects on stigma (Pescosolido et al., 2008). Therefore, along with FINIS, we examine the demographics, perceived threats, attribution of the disease, and anxiety symptoms as the individual level of risk factors, and media exposure, media engagement, and familiarity with the quarantined cases as the community-level risk factors.
In sum, the present study focuses on identifying the profiles of perceived courtesy and affiliate stigma connected to COVID-19 among the population who identify themselves as Hubei people, who is not treating for COVID-19 (i.e., tested positive for COVID-19 by medical laboratory and under treatment) and presumptive for COVID-19 (i.e., met clinical criteria and epidemiologic evidence with no confirmatory laboratory testing). This study also aims at examining the risk factors for different profiles. The study of the stigma connected to COVID-19 can be salient, as it can provide a reference for stigma research and policymakers, and facilitate health professionals in taking further steps to empower and support the vulnerable populations and their families and communities during such a global pandemic.
2. Method
2.1. Data collection
The data of the present study were a subset of an online survey named Social Cognition and Behavior Investigation of COVID-19. This survey aimed to investigate how people were perceiving and coping with the COVID-19 threats, including people located in Wuhan, other cities in Hubei with the exclusion of Wuhan, and other cities outside of Hubei. The data were collected during the peak period (i.e., 31st Jan to Feb 8, 2020) of the COVID-19 outbreak in Mainland China. The characteristics of COVID-19 rendered most individuals without any hygienic precaution potentially infected. All participants were recruited by convenience sampling through public social media (e.g., WeChat and Tencent QQ) relying on the research team's networks with the local community. Convenient sampling through social media is a typical and common method in studies on public health emergencies (Elrggal et al., 2018; Maity et al., 2015). In total, 7058 participants (male = 2,157, female = 4901; mean age = 26.06, SD = 12.91, range = 8 to 72) voluntarily participated in the investigation. Ethics approval was obtained from the Human Subjects Ethics Sub-Committee of School of Social and Public Administration, East China University of Science and Technology. The informed written consent of the participant was obtained by clicking the AGREE button before the completion of the investigation. The questionnaire was written in Chinese. Participants did not receive any incentive.
2.2. Participants
The participants of the study were potentially COVID-19-infected individuals who: a) were over 18 years; b) residence in Hubei with Internet Protocol addresses showing Wuhan and other cities in Hubei province; and c) identified themselves as Hubei people. Those who claimed that they were treating for, presumptive for, and have recovered from COVID-19 were excluded. The final sample used in the present study included 2813 adults (female: n = 2,184, 77.64%; male: n = 629, 22.36%; mean age = 37.85 years, SD = 6.61 years, range = 18–63 years). Most of the participants received education above junior school level, reporting middle socioeconomic status (mean = 4.99, SD = 1.83) and good health status (mean = 4.02, SD = 0.77). The details of the demographic information of the current sample can be found in Table 1 .
Table 1.
Sample characteristics (N = 2813).
|
n |
% |
|
|---|---|---|
| M ± SD | Range | |
| Age | 37.66 ± 6.56 | 18–63 |
| Sex | ||
| Male | 629 | 22.36% |
| Female | 2184 | 77.64% |
| Identity | ||
| Wuhan people | 935 | 33.24% |
| Hubei people | 1878 | 66.76% |
| Education level | ||
| Primary School and below | 170 | 6.04% |
| Junior School | 786 | 27.94% |
| High School | 864 | 30.71% |
| Bachelor and above | 993 | 35.30% |
| Subjective socioeconomic status | ||
| 1 (Lowest) | 213 | 7.57% |
| 2 | 99 | 3.52% |
| 3 | 226 | 8.03% |
| 4 | 239 | 8.50% |
| 5 | 967 | 34.38% |
| 6 | 591 | 21.01% |
| 7 | 268 | 9.53% |
| 8 | 167 | 5.94% |
| 9 | 20 | 0.71% |
| 10 (Highest) | 23 | 0.82% |
| Self-reported general health | ||
| Very poor | 4 | 0.14% |
| Poor | 42 | 1.49% |
| Normal | 656 | 23.32% |
| Good | 1308 | 46.50% |
| Very good | 803 | 28.55% |
2.3. Measures
As no existing measure could assess the variables that we were interested in within the context of the COVID-19 outbreak, a multidisciplinary research group (including researchers in social work, sociology, and psychology) conducted an extensive literature review, and selected the following measures and items that a) matched the factors in the FINIS (Pescosolido et al., 2008), including the individual-level risk factors (i.e., the demographics, perceived threats, attribution of the disease, and anxiety symptoms), and community-level risk factors (i.e., media exposure, media engagement, and familiarity with the quarantined cases); b) had been used in previous studies of similar contexts (i.e., the measure of perceived threats [Cronbach's α = 0.89] and media exposure and engagement which had been used in MERS-CoV, as well as the item of attribution of the disease which had been used in SARS); c) had been culturally adapted to the Chinese population with good psychometric properties (i.e., the Generalized Anxiety Disorder-2 and the Chinese Courtesy Stigma Scale had been validated in Chinese samples). Measures that had not been used in Standard Chinese speaking populations before (i.e., items of stigma, perceived threats, and media exposure and engagement) were translated to Simplified Chinese through a standard and validated translation process (e.g., forward- and back-translation, cognitive interviews, expert discussions) to guarantee that the translation was easily and unambiguously understood in the Chinese population (Beaton et al., 2000; Li et al., 2020a).
2.4. COVID-19 stigma
Perceived courtesy stigma. Perceived courtesy stigma was assessed using five items selected from a subscale (i.e., concern with public attitudes) of the revised HIV Stigma Scale (Berger et al., 2001), and adapted to the context of the present study. The items mainly describe the awareness of social disqualification (e.g., Because the COVID-19 outbreak took place in Wuhan/Hubei, Wuhan/Hubei people are rejected when others learn that they are Wuhan/Hubei people), and negative change in social identity (e.g., Because the COVID-19 outbreak took place in Wuhan/Hubei, most people regard Wuhan/Hubei people as a plague). The five items assess individuals’ typical levels of perceived courtesy stigma, namely, “Disgusting”, “Rejected”, “Plague”, “Uncomfortable” and “Outcasts”. The participants responded to a four-point Likert scale (1 = strongly disagree to 4 = strongly agree), asking the extent to which they agreed with each statement, with a higher score indicating a higher level of perceived courtesy stigma. The internal consistency was good for the perceived courtesy stigma measure in the present study (Cronbach's α = 0.93). The factor loadings were higher than 0.80.
Affiliate stigma. The affiliate stigma was measured by five items adapted from the subscale (i.e., self-perceived stigma) of the Chinese Courtesy Stigma Scale that was designed to measure the stigma perceived by people who had the undesirable attribute (e.g., people who lived with HIV patients) (Liu et al., 2014). Five items (i.e., “Estranged”, “Blamed”, “Shamed”, “No Strong Point” and “Discriminated” ) relevant to the context of COVID-19 were selected, measuring negative changes in self-concept (e.g., Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel shamed and self-blame) and emotional reactions (e.g., Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel people will no longer see my strong point). Participants reported the extent to which they agreed with each item and rated this response on a four-point Likert scale (1 = strongly disagree to 4 = strongly agree). A higher score indicated a higher level of affiliate stigma. In the present study, Cronbach's α was 0.86. The factor loadings were higher than 0.66.
2.5. Risk factors
According to FINIS, risk factors were measured at the interface of individuals and the community. At the individual level, demographic characteristics and perceived threats, including susceptibility and severity, and the attribution of the disease and anxiety symptoms were assessed. At the community level, media exposure, media engagement, and familiarity with quarantined cases of COVID-19 were assessed.
Demographic Characteristics. The participants answered questions about their background, including their sex, age, and education level. The respondents were asked to place themselves on a ladder from one to ten in terms of their subjective relative rank of socioeconomic status (SES). The participants indicated the present state of their health on a single-item five-point Likert scale from 0 (very bad) to 5 (very good).
Perceived threats of COVID-19. Eight items regarding perceived susceptibility (four items) and severity (four items) were adapted from a previous study in the context of the MERS-CoV outbreak (Yoo et al., 2016) to measure the perceived threats of COVID-19. The participants reported their perceptions of COVID-19-related susceptibility (e.g., “COVID-19 infection could happen anytime to anyone, even a healthy individual”) and severity (e.g., “COVID-19 causes death quickly”) on a five-point scale (1 = strongly disagree to 5 = strongly agree) with a higher score indicating a higher level of perceived threats. In the present study, the Cronbach's α was 0.84 and 0.82 for susceptibility and severity, respectively.
Attribution of the disease. Two items were used to measure the two aspects of controllability attributions directly (i.e., personal responsibility to the disease: “COVID-19 patients are responsible for their own infection;” blame the infected individuals: “It is the COVID-19 patients' own fault that they have the disease”). The two items were developed according to Weiner's (1993) attribution theory and a previous study regarding SARS (Mak et al., 2006). Participants were asked whether they agreed with the statements on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree), with higher scores indicating greater personal responsibility and more blame.
COVID-19-related anxiety symptoms. The Chinese version of the Generalized Anxiety Disorder-2 (GAD-2; Luo et al., 2019; Plummer et al., 2016) was adopted to assess the extent to which participants had suffered from COVID-19-related anxiety symptoms in the past 14 days. The original GAD-2 has been widely used across different cultures, including Chinese people (Luo et al., 2019; Plummer et al., 2016). Participants responded on a four-point Likert scale (0 = not at all to 3 = nearly every day). The items were “I am feeling nervous, anxious, or on edge” and “I am not able to stop or control worrying.” The total score ranged from 0 to 6, while a cut-off point of 3 was recommended to identify GAD-2 (Luo et al., 2019; Plummer et al., 2016). In the current study, Cronbach's α was 0.80.
Media context. Two single items that were adapted from a previous study in the context of the MERS-CoV outbreak (Yoo et al., 2016) directly measured two aspects of media context: “How often have you heard or seen comments, questions, pictures, videos, or other information about COVID-19 after the Chinese authorities closed off Wuhan?” for media exposure; “How often do you post or share comments, questions, pictures, videos, or other information about COVID-19 after the Chinese authorities closed off Wuhan?” for media engagement. Responses for media exposure and engagement were based on a six-point scale (1 = never to 6 = very often).
Familiarity with quarantined cases of COVID-19. A binary item that asked whether the respondent knew someone who was quarantined was employed to assess the familiarity of participants with quarantined cases of COVID-19. The responses were coded as 1 = yes and 2 = no.
3. Results
3.1. Latent profile analysis
To search for the stigma profiles of Hubei people in the outbreak of COVID-19, the present study used cross-sectional data to conduct a Latent Profile Analysis (LPA) based on all the items of perceived courtesy and affiliate stigma. To test the most appropriate number of profiles, the following statistical criteria were used: Akaike's information criterion (AIC); Bayesian Information Criterion (BIC); Vuong-Lo-Mendell-Rubin adjusted likelihood ratio (VLMR); bootstrapped likelihood ratio (BLRT), and entropy value. Low BIC and AIC values indicated a better quality of the resulting statistical model (Weisberg, 2005). Entropy denoted how well individuals were classified, with an entropy value greater than 0.80 showing a relatively high accuracy of classification (Lubke and Muthén, 2007). Significant VLMR and BLRT indicated that classes were statistically different between each other in the model (L. K. Muthén and Muthén, 2010). Mplus 7 was used to conduct the LPA.
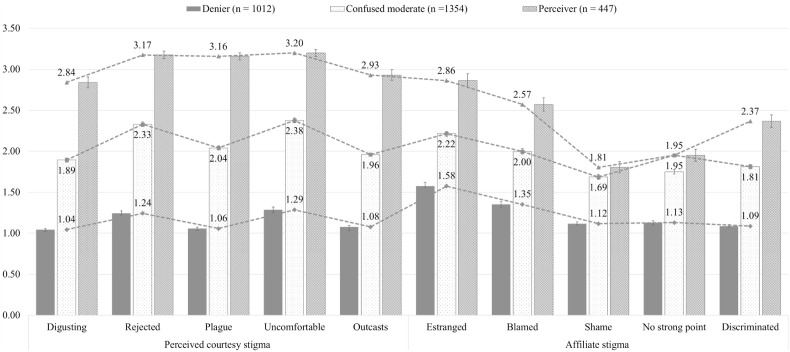
Three comparable solutions of LPA are shown in Table 2 and depicted graphically with means of each item in Fig. 1 . Grouping individuals into three profiles was the best solution for the current sample. The three-profile solution (AIC = 48247.57, BIC = 48497.14, VLMR < 0.001, BLRT < 0.001) fit the data significantly better than the four-profile solution (AIC = 46078.27, BIC = 46393.19, VLMR = 0.15, BLRT = 0.15). Moreover, it showed a lower AIC and BIC than the two-profile model (AIC = 52602.06, BIC = 52786.27, VLMR < 0.001, BLRT < 0.001).
Table 2.
Latent profile analysis of participants’ responses to questions regarding stigma (N = 2813).
| Model | Log | AIC | BIC | Entropy | VLMR | BLRT |
|---|---|---|---|---|---|---|
| 2-profile | −26270.03 | 52602.06 | 52786.27 | 0.94 | <0.001 | <0.001 |
| 3-profile | −24081.79 | 48247.57 | 48497.14 | 0.94 | < 0.001 | < 0.001 |
| 4- profile | −22986.13 | 46078.27 | 46393.19 | 0.94 | .15 | .15 |
Note. Log = log-likelihood; AIC = Akaike's information criterion; BIC = Bayesian Information Criterion; VLMR = Vuong-Lo-Mendell-Rubin adjusted likelihood ratio test; BLRT = bootstrapped likelihood ratio test.
Bold indicates “best” fit for each respective statistic.
Fig. 1.
The Three-Profile Model of Stigma (N = 2813). Note. Perceived courtesy stigma refers to the experience and perception of stigma of people who associated with COVID-19 (e.g., the geographic linkage); Affiliate stigma is the internalization of perceived courtesy stigma among the associates; the “Denier”, “Confused moderate” and “Perceiver” profile include individuals who perceived the low, moderate, high level of perceived courtesy and affiliate stigma, respectively.
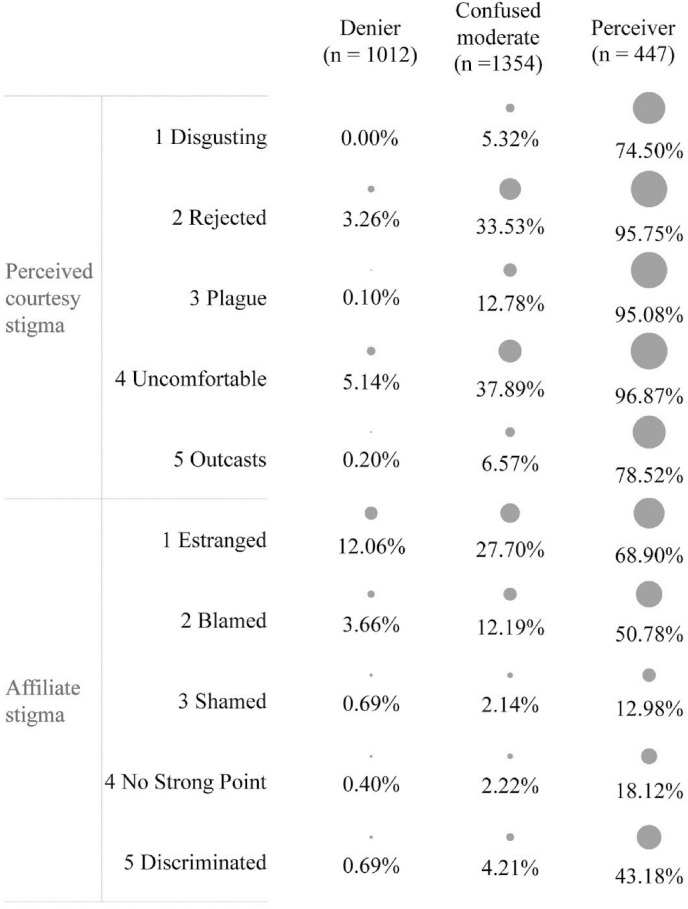
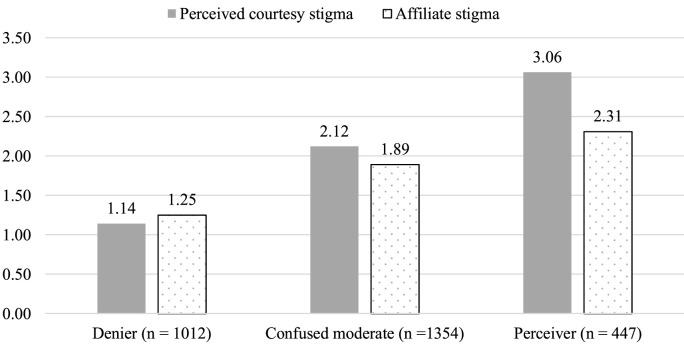
Profile characteristics according to participants’ responses on each item can be found in Table 3 . We further collapsed all individual items of perceived courtesy and affiliate stigma into dichotomies (“Strongly agree” and “Agree” coded as 1; “Strongly disagree” and “Disagree” coded as 0). The percentage of endorsement of a stigmatizing response of participants in different profiles was presented in Fig. 2 , which may be helpful to search for the backbone (i.e., core sentiments) underlying perceived courtesy and affiliate stigma. Three profiles are all homogeneous, which means no varying combinations of levels of perceived courtesy stigma and affiliate stigma was observed. Fig. 3 shows the mean levels of perceived courtesy and affiliate stigma for each of the three profiles.
Table 3.
Profile characteristics according to participants’ response on each item.
| Denier (n = 1012) |
Confused moderate (n = 1354) |
Perceiver (n = 447) |
|||
|---|---|---|---|---|---|
| Responsea | % | % | % | ||
| Perceived courtesy stigma | |||||
| 1 Disgusting | Because the COVID-19 outbreak took place in Wuhan/Hubei, most people think that Wuhan/Hubei people are disgusting. | 1 | 95.55%b | 16.17% | 4.03% |
| 2 | 4.45% | 78.51% | 21.48% | ||
| 3 | 0.00% | 5.10% | 60.85% | ||
| 4 | 0.00% | 0.22% | 13.65% | ||
| 2 Rejected | Because the COVID-19 outbreak took place in Wuhan/Hubei, Wuhan/Hubei people are rejected when others learn that they are Wuhan/Hubei people. | 1 | 78.95% | 1.70% | 0.45% |
| 2 | 17.79% | 64.77% | 3.80% | ||
| 3 | 3.16% | 32.42% | 73.60% | ||
| 4 | 0.10% | 1.11% | 22.15% | ||
| 3 Plague | Because the COVID-19 outbreak took place in Wuhan/Hubei, most people regard Wuhan/Hubei people as a plague. | 1 | 94.27% | 8.86% | 0.00% |
| 2 | 5.63% | 78.36% | 4.92% | ||
| 3 | 0.10% | 12.63% | 74.27% | ||
| 4 | 0.00% | 0.15% | 20.81% | ||
| 4 Uncomfortable | Because the COVID-19 outbreak took place in Wuhan/Hubei, most people are uncomfortable around someone from Wuhan/Hubei. | 1 | 76.68% | 2.07% | 0.00% |
| 2 | 18.18% | 60.04% | 3.13% | ||
| 3 | 4.94% | 35.97% | 73.83% | ||
| 4 | 0.20% | 1.92% | 23.04% | ||
| 5 Outcasts | Because the COVID-19 outbreak took place in Wuhan/Hubei, most Wuhan/Hubei people are treated as outcasts. | 1 | 92.39% | 11.00% | 2.68% |
| 2 | 7.41% | 82.42% | 18.79% | ||
| 3 | 0.20% | 6.20% | 61.30% | ||
| 4 | 0.00% | 0.37% | 17.23% | ||
| Affiliate stigma | |||||
| 1 Estranged | Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel estranged by people around me. | 1 | 56.92% | 9.90% | 7.38% |
| 2 | 31.03% | 62.41% | 23.71% | ||
| 3 | 9.58% | 23.93% | 44.07% | ||
| 4 | 2.47% | 3.77% | 24.83% | ||
| 2 Blamed | Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel blamed by people around me. | 1 | 69.17% | 14.03% | 10.07% |
| 2 | 27.17% | 73.78% | 39.15% | ||
| 3 | 2.87% | 10.64% | 34.23% | ||
| 4 | 0.79% | 1.55% | 16.55% | ||
| 3 Shamed | Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel shamed and self-blame. | 1 | 89.33% | 33.68% | 35.79% |
| 2 | 9.98% | 64.18% | 51.23% | ||
| 3 | 0.40% | 1.85% | 9.62% | ||
| 4 | 0.30% | 0.30% | 3.36% | ||
| 4 No Strong Point | Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel people will no longer see my strong point. | 1 | 87.45% | 27.40% | 27.96% |
| 2 | 12.15% | 70.38% | 53.91% | ||
| 3 | 0.30% | 2.07% | 13.20% | ||
| 4 | 0.10% | 0.15% | 4.92% | ||
| 5 Discriminated | Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel discriminated and people kept away from me. | 1 | 92.00% | 23.34% | 14.54% |
| 2 | 7.31% | 72.45% | 42.28% | ||
| 3 | 0.69% | 3.77% | 35.12% | ||
| 4 | 0.00% | 0.44% | 8.05% | ||
Note.
1 = strongly disagree; 2 = disagree; 3 = agree; 4 = strongly agree.
Bold: the highest percentage among the responses of each item. Between-group differences were statistical significant for all items (p < .001).
Fig. 2.
The percentage of endorsement of a stigmatizing response of participants in different profiles (N = 2813). Note. Items of perceived courtesy and affiliate stigma were collapsed into dichotomies (“Strongly agree” and “Agree” coded as 1; “Strongly disagree” and “Disagree” coded as 0). Size of circle corresponds to percentage agreeing on each item in each profile.
Fig. 3.
Mean levels of perceived courtesy and affiliate stigma for each of the three profiles (N = 2813).
The first profile can be called the “Denier” (35.98%, n = 1012). The majority of this group selected the least stigmatizing option (i.e., strongly disagree) on each item of stigma (56.92%–95.55%). “Estranged” appeared to be a backbone of stigma in this profile (see Table 3 and Fig. 2). The “Denier” indicated the lowest levels of perceived courtesy stigma (mean = 1.14, SD = 0.23) and affiliate stigma (mean = 1.25, SD = 0.35).
The second profile was labeled as the “Confused moderate” (48.13%, n = 1354). The “Confused moderate” scored the middle stigmatizing option (i.e., disagree: 60.04%–82.42%) in each item of stigma. The core sentiments underlying perceived courtesy and affiliate stigma were “Uncomfortable”, “Rejected”, and “Estranged” (see Table 3 and Fig. 2). The “Confused moderate” reported moderate degree on perceived courtesy stigma (mean = 2.12, SD = 0.26) and affiliate stigma (mean = 1.89, SD = 0.39).
The third profile, the “Perceiver”, had 447 (15.89%) individuals, who had perceived the highest levels of courtesy (mean = 3.06, SD = 0.40) and affiliate stigma (mean = 2.31, SD = 0.60), with 50.78%–95.75% scoring the more stigmatizing options (i.e., “agree” or “strongly agree”). Exceptions were “feel shame and self-blame,” “feel uneasy to get along with people around me,” and “have been discriminated,” with 12.98%, 18.12%, and 43.18% of members selecting the more stigmatizing options, respectively. The core sentiments were “Uncomfortable” , “Rejected”, and “Plague” (see Table 3 and Fig. 2).
3.2. ANOVA analysis
To validate the identified profiles, the stigma indicators were compared among different profiles of participants using ANOVA in SPSS 25. The post hoc tests were conducted using Fisher's least significant difference (LSD) test. The results of the ANOVA showed significant main effects for all groups in stigma indicators across the three profiles [perceived courtesy stigma: F (2, 2810) = 8065.64, p < .001; affiliate stigma: F (2, 2810) = 1203.82, p < .001]. The pairwise comparisons among the three profiles were also statistically significant.
3.3. Multinomial logistic regression analysis
Once the final cluster profiles were identified, the probability of being a member of a particular class was input as the dependent variable in a multinomial logistic regression. The model fitness was estimated using a likelihood ratio test (Agresti, 2018; Anderson and Rutkowski, 2008). All risk factors were simultaneously incorporated in the fully adjusted multinomial logistic regression model. Poisson distributions were normally approximated to calculate the 95% confidence intervals (CI). SPSS 25 was used for data analysis. Statistical significance was set at p < .05.
Taking the “Perceiver” as the reference profile, the “Denier” and the “Confused moderate” were compared with it. The results of the multinomial logistic regression are presented in Table 4 . Only the significant effects were interpreted with indices.
Table 4.
Multinomial logistic regression modelling results for the three profiles (N = 2813).
| Mean /N |
SD /% |
B | Wald | p | aOR | 95% Confidence Interval for aOR |
||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Denier | ||||||||
| Individual Level | ||||||||
| Sex | ||||||||
| Male (code = 1) | 228 | 22.53% | 0.07 | 0.20 | .65 | 1.07 | 0.80 | 1.44 |
| Female (code = 2) | 784 | 77.47% | 0 | |||||
| Age | 37.79 | 6.61 | 0.00 | 0.30 | .58 | 1.01 | 0.99 | 1.02 |
| Education level | 2.89 | 0.95 | −0.30 | 18.28 | < .001 | 0.74 | 0.65 | 0.85 |
| Subjective socioeconomic status | 5.11 | 1.86 | 0.09 | 7.09 | .01 | 1.10 | 1.02 | 1.17 |
| Self-reported general health | 4.1 | 0.77 | 0.15 | 3.64 | .06 | 1.16 | 1.00 | 1.36 |
| Perceived susceptibility of COVID-19 | 2.34 | 1.04 | −0.13 | 4.05 | .04 | 0.88 | 0.78 | 1.00 |
| Perceived severity of COVID-19 | 2.79 | 1.06 | −0.27 | 17.14 | < .001 | 0.77 | 0.67 | 0.87 |
| Attribution of responsibility | 3.23 | 1.34 | 0.04 | 0.61 | .43 | 1.04 | 0.94 | 1.15 |
| Attribution of blame | 1.58 | 0.9 | −0.17 | 5.67 | .02 | 0.84 | 0.73 | 0.97 |
| Anxiety symptoms | 2.54 | 1.9 | −0.29 | 68.56 | < .001 | 0.75 | 0.70 | 0.80 |
| Community Level | ||||||||
| Media exposure | 5.07 | 1.21 | 0.04 | 0.50 | .48 | 1.04 | 0.93 | 1.16 |
| Media engagement | 3.43 | 1.77 | −0.01 | 0.06 | .81 | 0.99 | 0.92 | 1.07 |
| Familiarity with quarantined cases | ||||||||
| Yes (code = 1) | 66 | 6.52% | −0.83 | 18.41 | < .001 | 0.44 | 0.30 | 0.64 |
| No (code = 2) | 946 | 93.48% | 0 | |||||
| Confused moderate | ||||||||
| Individual Level | ||||||||
| Sex | ||||||||
| Male (code = 1) | 314 | 23.19% | 0.11 | 0.54 | .46 | 1.11 | 0.84 | 1.47 |
| Female (code = 2) | 1040 | 76.81% | 0 | |||||
| Age | 38.04 | 6.5 | 0.01 | 1.22 | .27 | 1.01 | 0.99 | 1.03 |
| Education level | 2.96 | 0.92 | −0.16 | 5.59 | .02 | 0.85 | 0.75 | 0.97 |
| Subjective socioeconomic status | 4.96 | 1.78 | 0.05 | 2.79 | .10 | 1.05 | 0.99 | 1.12 |
| Self-reported general health | 3.98 | 0.76 | −0.01 | 0.01 | .91 | 0.99 | 0.86 | 1.15 |
| Perceived susceptibility of COVID-19 | 2.53 | 0.93 | −0.01 | 0.06 | .81 | 0.99 | 0.88 | 1.11 |
| Perceived severity of COVID-19 | 2.98 | 0.93 | −0.15 | 6.26 | .01 | 0.86 | 0.76 | 0.97 |
| Attribution of responsibility | 3.21 | 1.17 | −0.03 | 0.34 | .56 | 0.97 | 0.88 | 1.07 |
| Attribution of blame | 1.77 | 0.88 | 0.08 | 1.42 | .23 | 1.08 | 0.95 | 1.23 |
| Anxiety symptoms | 2.94 | 1.71 | −0.17 | 27.89 | < .001 | 0.84 | 0.79 | 0.90 |
| Community Level | ||||||||
| Media exposure | 4.94 | 1.18 | −0.11 | 4.03 | .04 | 0.90 | 0.81 | 1.00 |
| Media engagement | 3.54 | 1.66 | 0.04 | 1.58 | .21 | 1.05 | 0.98 | 1.12 |
| Familiarity with quarantined cases | ||||||||
| Yes (code = 1) | 135 | 9.97% | −0.44 | 6.78 | .01 | 0.65 | 0.47 | 0.90 |
| No (code = 2) | 1219 | 90.03% | 0 | |||||
Note. The reference category is: Perceiver; aOR = Adjusted Odds Ratio.
“Denier” vs. “Perceiver.” The results show that the odds of being distributed to “Perceiver” were greater for those who reported high levels of education (aOR = 0.74; 95% CI: 0.64, 0.85), perceived threats of COVID-19 (severity: aOR = 0.77; 95% CI: 0.68, 0.87; susceptibility: aOR = 0.88; 95% CI: 0.78, 1.00), attribution of blame (aOR = 0.84; 95% CI: 0.73, 0.97), and anxiety symptoms (aOR = 0.75; 95% CI: 0.70, 0.80). Individuals with a high level of SES (aOR = 1.10; 95% CI: 1.02, 1.17) are likely to be distributed to the “Denier”. Compared with individuals who did not report their familiarity with quarantined cases of COVID-19, those who reported such familiarity were about twice as likely to be a member of the “Perceiver” (aOR = 0.44; 95% CI: 0.30, 0.64).
“Confused moderate” vs. “Perceiver.” The results show that a high level of education (aOR = 0.85; 95% CI: 0.75, 0.97), perceived severity of COVID-19 (aOR = 0.86; 95% CI: 0.76, 0.97), anxiety symptoms (aOR = 0.84; 95% CI: 0.79, 0.90), and media exposure (aOR = 0.90; 95% CI: 0.81, 1.00) were significantly associated with a high probability of being a member of the “Perceiver.” Compared with individuals who did not report their familiarity with quarantined cases of COVID-19, those who reported such familiarity were more likely to be a member of the “Perceiver” (aOR = 0.65; 95% CI: 0.47, 0.90).
4. Discussion
This study identified the three distinct profiles among Hubei people: “Denier,” “Confused moderate,” and “Perceiver.” Generally, people with a high level of education, perceived threats, anxiety symptoms, and familiarity with quarantined cases have a high likelihood to be distributed into the “Perceiver” category.
4.1. Three profiles of perceived courtesy and affiliate stigma
The current study found three patterns of perceived courtesy and affiliate stigma: “Denier,” “Confused moderate,” and “Perceiver,” each of which was significantly different from the others. The “Denier” (35.98%) indicated the lowest levels of perceived courtesy and affiliate stigma. They were significantly healthier than the other profiles and reported the lowest level of risk factors, including perceived threats, attribution of blame, anxiety symptoms, and familiarity with quarantined cases. The majority of participants in our sample were categorized into the “Confused moderate” (48.13%). They scored relatively high in stigma indicators (i.e., perceived courtesy and affiliate stigma). They mostly agreed with the attribution that the people who have COVID-19 were responsible for contracting the disease. Moreover, they reported little exposure to media. The “Perceiver” should be given increased attention despite being the smallest profile (15.89%). The “Perceiver” displayed the highest perceived courtesy and affiliate stigma among the three profiles, which reported a significantly high level of risk factors than other profiles, including high education levels, perceived threats, anxiety symptoms, and familiarity with quarantined cases and low SES.
No discordant patterns (e.g., a high level of perceived courtesy stigma and low level of affiliate stigma) were found in our sample. This result was consistent with the assertion of Modified Labeling Theory that public stigmatization can have a negative influence on a person's internal sense of self (Link et al., 1989), and also in line with other studies which demonstrated the congruence between courtesy and affiliate stigma (Mak and Kwok, 2010; Vogel et al., 2013). Thus, there may be an interlocking psychological response that those who are at high risk of contagion may perceive courtesy stigma and then internalized it. However, regarding the affiliate stigma of the “Perceiver”, only 12.98% and 18.12% of the participants selected the stigmatizing options (i.e., “agree” or “strongly agree”) of “feel shame and self-blame” and “people will no longer see my strong point,” respectively. Most participants of the “Perceiver” might have realized that, although they were under a salient stigmatizing condition (e.g., feel estranged, blamed, and discriminated), the stigmatizing behaviors of others were illegitimate (Corrigan and Watson, 2002). Hence, their self-esteem might remain intact and they would show righteous anger (e.g., “Yes, I am Hubei people, who is at high risk of contagion, but I am not ashamed!”) (Corrigan and Watson, 2002), instead of negative cognition and emotion responses.
4.2. Profiles and corresponding risk factors
Demographic characteristics. According to FINIS, we estimated the influence of demographics, which combine with the illness characteristics to drive stigma. Our study found that SES might be a risk factor for perceiving perceived courtesy and affiliate stigma. Members of the “Denier” with a low level of SES had a higher likelihood to be a member of the “Perceiver”. Our findings were consistent with previous studies, showing that low-SES individuals appeared vulnerable to experience perceived courtesy and affiliate stigma (Chiu et al., 2013; Yang, 2015). These individuals might lack resources (e.g., money, power, beneficial social connections, and healthy advantages) to protect their social identity and minimize the consequences of infection from COVID-19 once it occurred (Hatzenbuehler et al., 2013; Link and Phelan, 1995). We also found that the “Denier” and “Confused moderate” who reported a high level of education had a high likelihood to be distributed into the “Perceiver”. This can be explained in two aspects. First, well-educated individuals may be more sensitive to the behaviors of others and perceive these behaviors as rejection and discrimination (Phelan et al., 1998). Second, the result may be influenced by the mental health status of individuals. A recent survey among Chinese people has found that people with higher education tend to report more mental health problems (e.g., anxiety and depression) (Graham et al., 2017), making them more vulnerable to perceive greater stigma. Our findings would intrigue some questions for future studies under the pandemic circumstance: which indicator of socioeconomic status can be a better predictor of stigma; or whether gaps between subjective and objective socioeconomic status could influence individual's psychological processes like in many other circumstances (Kim et al., 2014; Kim and Park, 2015).
Social psychological process. FINIS also proposed social psychological and cognitive factors as risk factors for stigma. The odds of being distributed to the “Perceiver” were greater for those who in the “Denier” with a high level of perceived threats, along with “Confused moderate” members with a high level of perceived severity. At the early stage of COVID-19, on account of the unknown cause and possible fatal outcome of the disease, the uncertainty about objective risks may amplify the perceived health risks and anxiety (Strekalova, 2017), which may be accompanied by social isolation and stigmatization (Leppin and Aro, 2009). Moreover, we also found that members of the “Denier” who reported a higher level of attribution of blame, were more likely to be distributed to the “Perceiver”. This likelihood might be due to the attribution bias that people believed, in which the associates (e.g., all Hubei people) shared the same character flaws as the discredited people who engaged in taboo activities (e.g., consumption of wildlife), triggering the COVID-19 outbreak (R. A. Smith, Zhu and Quesnell, 2016).
Media context. As FINIS suggested, media and real-life exposure are critical elements of community context where stigma embeds in. For the “Confused moderate”, frequent media exposure increased the likelihood of being a member of the “Perceiver”. As the global media reported dramatic stories from China using “Chinese Virus” or “Wuhan Virus” as the name of COVID-19, the stigmatization of people who potentially acquired COVID-19 emerged early in the outbreak. Hence, a higher level of receiving information from the media increases the possibility of picking up prejudicial and stereotypical information, thus increasing the perceived stigmatization. Moreover, great media exposure can increase perceived threats (Yoo et al., 2016), which contributes to the stigma.
Social network characteristics. For the “Denier”, familiarity with people who have been quarantined, as a source of real-life exposure to COVID-19, played a significant role in perceiving courtesy and affiliate stigma. We found that those who reported familiarity with quarantined cases of COVID-19 were twice as likely to be a member of the “Perceiver”. The quarantined cases suffered from the stigma of illness (Brooks et al., 2020), and the stigma would extend to those who were familiar with them (Corrigan and Nieweglowski, 2019). The familiarity with groups already prone to infection could exacerbate the perceived courtesy and affiliate stigma because of their association (Corrigan and Nieweglowski, 2019).
4.3. Limitations
A notable limitation is that our sample is reflective of a middle-class, middle-aged, well-educated, female, and healthy population residing in Hubei. Fast person-to-person transmission of the coronavirus hinders traditional community-based national sampling surveys and the face-to-face data collection. Conducting an online survey is feasible and safe. However, limited access to the internet could result in the undersampling of old adults and people with lower SES (Hong et al., 2017). The predominantly middle-aged adults in the sample may be because our data were collected relying on the research team's networks with local communities. We believe that higher female participation in our study may be due to the gender differences in response behaviors, which has been found in survey responses in different populations and settings (Galea and Tracy, 2007; Sax et al., 2003; W. G. Smith, 2008). Another online survey during the peak period of the COVID-19 outbreak also reported the higher rate of female responders (65.70%) compared with male responders (Zhong et al., 2020).
To investigate whether our findings can be applied to a demographically-representative community sample, a subsample (n = 824) was created and analyzed through randomly reducing the data to match the census records in important dimensions of demographics, namely, sex (male vs. female), age (range: 35–54), and residence (Wuhan city vs. other cities). The census data of Hubei Province and Wuhan city were obtained from reports by the National Bureau of Statistics (2011) and Statistics Bureau of Wuhan Municipality (2011). Similar results were observed in the demographically-representative community sample (see in supplementary documents). Nevertheless, future research should interpret our findings with caution. An online survey is a mixed picture, so future researchers should consider using more efficient methods (such as multilevel regression and post-stratification) to address the issue of representativeness (Salganik, 2019).
Another limitation lies in the measures we used in the study. Since our work has been done in a short time, the measures and results can only reveal small pieces of the whole COVID-19 stigma issue. Liu et al. (2014) point out two dimensions of courtesy stigma, namely ‘‘public stigma’’ and ‘‘self-perceived stigma’’, while we have focused only on the latter. Affective and cognitive responses of affiliate stigma were involved in our study, lacking measures of behavioral responses (e.g., withdrawal) (Mak and Cheung, 2008). Future study should employ measures which could map well onto the conceptualization of health-related stigma in different contexts. For the risk factors, more community-level factors should be considered. For example, the recommended practices of public policy (e.g., physical distancing and travel restrictions) could facilitate stigmatization on Hubei people (He et al., 2020; Logie and Turan, 2020).
5. Conclusions
Our study presents testimonies of the stigma issues of COVID stigma which is a social challenge to health and wellbeing and requires expertise from different fields to engage together and promote a cohesive society and culture of health (Berezin and Lamont, 2016). Health professionals must provide mental health services to tackle mental health problems and COVID-19 stigma timely and simultaneously, due to the potential knock-on effect and vicious circle between mental health problems and COVID-19 stigma. We found that demographic characteristics (e.g., SES and education) and individuals’ social-psychological processes (e.g., anxiety symptoms and perceived threats) can be possible predictors of COVID-19 stigma among Hubei people. The emerging COVID-19 stigma (e.g., perceived courtesy stigma) may, in turn, risk increasing mental health problems (e.g., anxiety and post-traumatic stress disorder) for the implicated groups (Li et al., 2020b). Therefore, awareness should be raised in the public to seek psychological assistance to ameliorate unnecessary anxiety and panic reactions (Bagcchi, 2020). Keeping daily routine and contact with families and friends are also advised to help people sense of control and obtain emotional supports. Moreover, the identification of different profiles of perceived courtesy and affiliate stigma may facilitate guiding the effective prevention and intervention actions with wider applicability across divergent groups.
The media context may contribute to COVID-19 stigma initially, but it can also function as an essential channel to reduce stigma. First, scientific knowledge and its credibility can ease fears and anxiety among the public and create empathy among the dominant public (Clair et al., 2016). Therefore, the media can transmit scientific and up-to-date knowledge about COVID-19 and explicit messages about the harms of stigma articulated by credible officials and expertise. People should be recommended to access sources of scientific knowledge from national and international official websites (e.g., CDC and WHO), reliable television channels, and journals. Second, positive interactions occur when the potential stigmatizer shift their beliefs and attitudes towards the stigmatized group, which can, in turn, mitigate stigma (Clair et al., 2016). The media can provide platforms for improving attitudes and social cohesion and solidarity among the public. For example, Chinese public media has kept broadcasting stories of ordinary Wuhan residents about their sacrifice and resilience in the battle against COVID-19, describing Wuhan as a city of hero and the people of Wuhan as grassroots heroes. These stories redefining the stigmatized group may help to promote positive interactions between the dominant group and the stigmatized population (e.g., Wuhan and Hubei people) (Clair et al., 2016). The government of Hong Kong employed Together, We Fight the Virus as their slogan in almost all publicity channels related to COVID-19, such as press conferences, advertisements, and psychoeducational and stigma-reduction materials. This may promote social cohesion and solidarity which in turn, facilitates better health and less stigma (Berezin and Lamont, 2016). Moreover, during the lockdown period, videos of Hubei people encouraging one another from their balconies circulated on social media which can help the outsiders understanding the struggles and create a sense of community and solidarity among Hubei people (Logie, 2020). These stories can promote group identification among the implicated people, shielding them from internalizing stigma and maintaining their self-esteem (Corrigan and Watson, 2002). Therefore, people who are isolated are advised to share their stories of isolation in the media in ways of pictures, blogs, vlogs, and live streaming.
This study has enrolled a large sample to evaluate the heterogeneity of perceived courtesy and affiliate stigma among people who are potentially infected with COVID-19 and examined the influence of contextual risk factors for stigma. This study is the first research to use LPA to assess the stigma toward people who are at high risk of contagion and in the worst affected area in the context of COVID-19. Our hope is that our findings intrigue other researchers in discussing stigma in the context of a worldwide pandemic.
CRediT author statement
He Bu: Conceptualization, Methodology, Formal analysis, Writing - original draft. Wenjie Duan: Conceptualization, Methodology, Resources, Writing - review & editing, Supervision, Project administration. Zheng Chen: Investigation, Resources, Project administration.
Acknowledgement
The authors thank our participants and all people of Hubei province, for the role they played in this battle against this coronavirus.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.113425.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agresti A. John Wiley & Sons; New York, NY: 2018. An Introduction to Categorical Data Analysis. [Google Scholar]
- Ali A., Hassiotis A., Strydom A., King M. Self stigma in people with intellectual disabilities and courtesy stigma in family carers: a systematic review. Res. Dev. Disabil. 2012;33(6):2122–2140. doi: 10.1016/j.ridd.2012.06.013. [DOI] [PubMed] [Google Scholar]
- Anderson C.J., Rutkowski L. Multimomial logistic regression. In: Osborne J., editor. Best Practices in Quantitative Methods. Sage Publications; Thousand Oaks, CA: 2008. pp. 390–409. [Google Scholar]
- Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020;20(7):782. doi: 10.1016/S1473-3099(20)30498-9. 782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer D.J., Curran P.J. The integration of continuous and discrete latent variable models: potential problems and promising opportunities. Psychol. Methods. 2004;9(1):3–29. doi: 10.1037/1082-989X.9.1.3. [DOI] [PubMed] [Google Scholar]
- Beaton D.E., Bombardier C.G.F., Ferraz M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- Berezin M., Lamont M. Mutuality, mobilization, and messaging for health promotion: toward collective cultural change. Soc. Sci. Med. 2016;165:201–205. doi: 10.1016/j.socscimed.2016.07.040. [DOI] [PubMed] [Google Scholar]
- Berger B.E., Ferrans C.E., Lashley F.R. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res. Nurs. Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budhwani H., Sun R. Creating COVID-19 stigma by referencing the novel coronavirus as the “Chinese virus” on Twitter: quantitative analysis of social media data. J. Med. Internet Res. 2020;22(5):e19301. doi: 10.2196/19301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu M.Y.L., Yang X., Wong F.H.T., Li J.H., Li J. Caregiving of children with intellectual disabilities in China – an examination of affiliate stigma and the cultural thesis. J. Intellect. Disabil. Res. 2013;57(12):1117–1129. doi: 10.1111/j.1365-2788.2012.01624.x. [DOI] [PubMed] [Google Scholar]
- Clair M., Daniel C., Lamont M. Destigmatization and health: cultural constructions and the long-term reduction of stigma. Soc. Sci. Med. 2016;165:223–232. doi: 10.1016/j.socscimed.2016.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P.W., Nieweglowski K. How does familiarity impact the stigma of mental illness? Clin. Psychol. Rev. 2019;70:40–50. doi: 10.1016/j.cpr.2019.02.001. [DOI] [PubMed] [Google Scholar]
- Corrigan P.W., Watson A.C. The paradox of self-stigma and mental illness. Clin. Psychol. Sci. Pract. 2002;9(1):35–53. doi: 10.1093/clipsy.9.1.35. [DOI] [Google Scholar]
- Crandall C.S. Multiple stigma and AIDS: illness stigma and attitudes toward homosexuals and IV drug users in AIDS-related stigmatization. J. Community Appl. Soc. Psychol. 1991;1(2):165–172. doi: 10.1002/casp.2450010210. [DOI] [Google Scholar]
- Elrggal M.E., Karami N.A., Rafea B., Alahmadi L., Al Shehri A., Alamoudi R. Evaluation of preparedness of healthcare student volunteers against Middle East respiratory syndrome coronavirus (MERS-CoV) in Makkah, Saudi Arabia: a cross-sectional study. J. Publ. Health. 2018;26(6):607–612. doi: 10.1007/s10389-018-0917-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner J., Schaller M., Park J.H., Duncan L.A. Evolved disease-avoidance mechanisms and contemporary xenophobic attitudes. Group Process. Intergr. Relat. 2004;7(4):333–353. doi: 10.1177/1368430204046142. [DOI] [Google Scholar]
- Festinger L. A theory of social comparison processes. Hum. Relat. 1954;7(2):117–140. doi: 10.1177/001872675400700202. [DOI] [Google Scholar]
- Galea S., Tracy M. Participation rates in epidemiologic studies. Ann. Epidemiol. 2007;17(9):643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Gilbert D.T., Fiske S.T., Lindzey G. Oxford University Press; New York: 1998. The Handbook of Social Psychology. [Google Scholar]
- Goffman E. Prentice Hall; NJ: 1963. Stigma: Notes on the Management of Spoiled Identity. [Google Scholar]
- Graham C., Zhou S., Zhang J. Happiness and health in China: the paradox of progress. World Dev. 2017;96:231–244. doi: 10.1016/j.worlddev.2017.03.009. [DOI] [Google Scholar]
- Hatzenbuehler M.L., Phelan J.C., Link B.G. Stigma as a fundamental cause of population health inequalities. Am. J. Publ. Health. 2013;103(5):813–821. doi: 10.2105/ajph.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J., He L., Zhou W., Nie X., He M. Discrimination and social exclusion in the outbreak of COVID-19. Int. J. Environ. Res. Publ. Health. 2020;17(8):2933. doi: 10.3390/ijerph17082933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong Y.A., Zhou Z., Fang Y., Shi L. The digital divide and health disparities in China: evidence from a national survey and policy implications. J. Med. Internet Res. 2017;19(9):e317. doi: 10.2196/jmir.7786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarlais D.C.D., Galea S., Tracy M., Tross S., Vlahov D. Stigmatization of newly emerging infectious diseases: AIDS and SARS. Am. J. Publ. Health. 2006;96(3):561–567. doi: 10.2105/ajph.2004.054742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson B.B. Hazard avoidance, symbolic and practical: the case of Americans' reported responses to Ebola. J. Risk Res. 2019;22(3):346–363. doi: 10.1080/13669877.2017.1378252. [DOI] [Google Scholar]
- Kim J.-H., Lee S.G., Shin J., Park E.-C. Impact of the gap between socioeconomic stratum and subjective social class on depressive symptoms: unique insights from a longitudinal analysis. Soc. Sci. Med. 2014;120:49–56. doi: 10.1016/j.socscimed.2014.09.001. [DOI] [PubMed] [Google Scholar]
- Kim J.-H., Park E.-C. Impact of socioeconomic status and subjective social class on overall and health-related quality of life. BMC Publ. Health. 2015;15(1):783. doi: 10.1186/s12889-015-2014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Chan L.Y.Y., Chau A.M.Y., Kwok K.P.S., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppin A., Aro A.R. Risk perceptions related to SARS and Avian Influenza: theoretical foundations of current empirical research. Int. J. Behav. Med. 2009;16(1):7–29. doi: 10.1007/s12529-008-9002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., Bu H., Duan W. 2020. A brief measure of courtesy and affiliate stigma on COVID-19 [Manuscript submitted for publication] [Google Scholar]
- Li Y., Duan W., Chen Z. Latent profiles of the comorbidity of post-traumatic stress disorder and generalized anxiety disorder among children and adolescents who are potentially infected with COVID-19. Child. Youth Serv. Rev. 2020;116 doi: 10.1016/j.childyouth.2020.105235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Cullen F.T., Struening E., Shrout P.E., Dohrenwend B.P. A modified labeling theory approach to mental disorders: an empirical assessment. Am. Socio. Rev. 1989;54(3):400–423. doi: 10.2307/2095613. [DOI] [Google Scholar]
- Link B.G., Phelan J.C. Social conditions as fundamental causes of disease [Extra Issue] J. Health Soc. Behav. 1995 doi: 10.2307/2626958. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J.C. Stigma and its public health implications. Lancet. 2006;367(9509):528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Liu H., Xu Y., Sun Y., Dumenci L., Seedat S. Measuring hiv stigma at the family level: psychometric assessment of the Chinese Courtesy Stigma Scales (CCSSs) PloS One. 2014;9(3) doi: 10.1371/journal.pone.0092855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H. Lessons learned from HIV can inform our approach to COVID-19 stigma. J. Int. AIDS Soc. 2020;23(5):e25504. doi: 10.1002/jia2.25504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Turan J.M. How do we balance tensions between COVID-19 public health responses and stigma mitigation? Learning from hiv research. AIDS Behav. 2020;24(7):2003–2006. doi: 10.1007/s10461-020-02856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubke G., Muthén B.O. Performance of factor mixture models as a function of model size, covariate effects, and class-specific parameters. Struct. Equ. Model. 2007;14(1):26–47. [Google Scholar]
- Luo Z., Li Y., Hou Y., Zhang H., Liu X., Qian X. Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: a validation study and meta-analysis. Gen. Hosp. Psychiatr. 2019;60:50–56. doi: 10.1016/j.genhosppsych.2019.07.008. [DOI] [PubMed] [Google Scholar]
- Maity H., Stansilaus R.P., Krishan A., Riya M., Zadeh V.R., Mudgal P.P., Arunkumar G. An online survey to assess awareness of ebola virus disease. Clin. Microbiol. Newsl. 2015;37(15):123–125. doi: 10.1016/j.clinmicnews.2015.07.004. [DOI] [Google Scholar]
- Mak W.W.S., Cheung R.Y.M. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J. Appl. Res. Intellect. Disabil. 2008;21(6):532–545. doi: 10.1111/j.1468-3148.2008.00426.x. [DOI] [Google Scholar]
- Mak W.W.S., Kwok Y.T.Y. Internalization of stigma for parents of children with autism spectrum disorder in Hong Kong. Soc. Sci. Med. 2010;70(12):2045–2051. doi: 10.1016/j.socscimed.2010.02.023. [DOI] [PubMed] [Google Scholar]
- Mak W.W.S., Mo P.K.H., Cheung R.Y.M., Woo J., Cheung F.M., Lee D. Comparative stigma of HIV/AIDS, SARS, and tuberculosis in Hong Kong. Soc. Sci. Med. 2006;63(7):1912–1922. doi: 10.1016/j.socscimed.2006.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer K.D., Schulze W.D., Hackett K.F., Cameron T.A., McClelland G.H. Can stigma explain large property value losses? The psychology and economics of superfund. Environ. Resour. Econ. 2006;33(3):299–324. doi: 10.1007/s10640-005-3609-x. [DOI] [Google Scholar]
- Mitter N., Ali A., Scior K. Stigma experienced by families of individuals with intellectual disabilities and autism: a systematic review. Res. Dev. Disabil. 2019;89:10–21. doi: 10.1016/j.ridd.2019.03.001. [DOI] [PubMed] [Google Scholar]
- Muthén B.O., Muthén L.K. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin. Exp. Res. 2000;24(6):882–891. doi: 10.1111/j.1530-0277.2000.tb02070.x. [DOI] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. [Computer software and manual]; Los Angeles,CA: Authors: 2010. Mplus User's Guide. Version 6. [Google Scholar]
- National Bureau of Statistics Tabulation on the 2010 population census of the People's Republic of China. 2011. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm
- Pescosolido B.A., Martin J.K., Lang A., Olafsdottir S. Rethinking theoretical approaches to stigma: a Framework integrating normative influences on stigma (FINIS) Soc. Sci. Med. 2008;67(3):431–440. doi: 10.1016/j.socscimed.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J.C., Bromet E.J., Link B.G. Psychiatric illness and family stigma. Schizophr. Bull. 1998;24(1):115–126. doi: 10.1093/oxfordjournals.schbul.a033304. [DOI] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatr. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Reluga T.C., Smith R.A., Hughes D.P. Dynamic and game theory of infectious disease stigmas. J. Theor. Biol. 2019;476:95–107. doi: 10.1016/j.jtbi.2019.05.020. [DOI] [PubMed] [Google Scholar]
- Salganik M.J. Princeton University Press; Princeton & Oxford: 2019. Bit by Bit: Social Research in the Digital Age. [Google Scholar]
- Sax L.J., Gilmartin S.K., Bryant A.N. Assessing response rates and nonresponse bias in web and paper surveys. Res. High. Educ. 2003;44(4):409–432. doi: 10.1023/A:1024232915870. [DOI] [Google Scholar]
- Shi Y., Shao Y., Li H., Wang S., Ying J., Zhang M. Correlates of affiliate stigma among family caregivers of people with mental illness: a systematic review and meta-analysis. J. Psychiatr. Ment. Health Nurs. 2019;26(1–2):49–61. doi: 10.1111/jpm.12505. [DOI] [PubMed] [Google Scholar]
- Smith Morris C. Epidemiological placism in public health emergencies: ebola in two Dallas neighborhoods. Soc. Sci. Med. 2017;179:106–114. doi: 10.1016/j.socscimed.2017.02.036. [DOI] [PubMed] [Google Scholar]
- Smith R.A., Zhu X., Quesnell M. Stigma and health/risk communication. Oxford Research Encyclopedia of Communication. 2016 doi: 10.1093/acrefore/9780190228613.013.96. [DOI] [Google Scholar]
- Smith W.G. Does gender influence online survey participation? A record-linkage analysis of university faculty online survey response behavior. ERIC Document Reproduction Service. 2008 https://scholarworks.sjsu.edu/cgi/viewcontent.cgi?article=1003&context=elementary_ed_pub Retrieved Sep 07, 2020, from. [Google Scholar]
- Statistics Bureau of Wuhan Municipality . China Statistics Press; Beijing: 2011. Wuhan Statistical Yearbook 2011. [Google Scholar]
- Strekalova Y.A. Health risk information engagement and amplification on social media:News about an emerging pandemic on facebook. Health Educ. Behav. 2017;44(2):332–339. doi: 10.1177/1090198116660310. [DOI] [PubMed] [Google Scholar]
- Tian S., Hu N., Lou J., Chen K., Kang X., Xiang Z. Characteristics of COVID-19 infection in Beijing. J. Infect. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel D.L., Bitman R.L., Hammer J.H., Wade N.G. Is stigma internalized? The longitudinal impact of public stigma on self-stigma. J. Counsel. Psychol. 2013;60(2):311. doi: 10.1037/a0031889. [DOI] [PubMed] [Google Scholar]
- Weiner B. On sin versus sickness. A theory of perceived responsibility and social motivation. Am. Psychol. 1993;48(9):957. doi: 10.1037/0003-066X.48.9.957. [DOI] [PubMed] [Google Scholar]
- Weisberg S. vol. 528. John Wiley & Sons; 2005. (Applied Linear Regression). [Google Scholar]
- World Health Organization . 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf Retrieved from. [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Yang X. No Matter How I Think, it Already Hurts: self-stigmatized feelings and face concern of Chinese caregivers of people with intellectual disabilities. Journal of Intellectual Disabilities. 2015;19(4):367–380. doi: 10.1177/1744629515577909. [DOI] [PubMed] [Google Scholar]
- Yoo W., Choi D.-H., Park K. The effects of SNS communication: how expressing and receiving information predict MERS-preventive behavioral intentions in South Korea. Comput. Hum. Behav. 2016;62:34–43. doi: 10.1016/j.chb.2016.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong B.-L., Luo W., Li H.-M., Zhang Q.-Q., Liu X.-G., Li W.-T., Li Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int. J. Biol. Sci. 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.