Abstract
Stent underexpansion is frequently observed in calcified coronary lesions and increases the risk of future adverse cardiac events. Current plaquemodification techniques might not be suitable when calcium deposition is circumferential and deep inside the vessel wall. We report a case during which coronary lithoplasty was used as an adjuvant therapy to improve severe stent underexpansion after failed atherectomy and high‐pressure non‐compliant balloon dilatations.
Keywords: calcified coronary lesions, coronary lithoplasty, plaque modification, shockwave balloon, stent expansion
1. INTRODUCTION
Heavily calcified coronary lesions often lead to suboptimal stent deployment, increasing the risk of adverse cardiac events, including in‐stent restenosis and stent thrombosis.1, 2 Available plaque‐modifying devices rely on tissue compression or tissue debulking to modify the underlying plaque before stent placement.3 However, some calcified plaques remain resistant to these devices due to deep concentric calcium depositions; in this particular scenario, coronary lithoplasty might play an important role. Here, we present a case supporting the use of coronary lithoplasty after conventional plaque‐modification techniques have failed.
2. CASE PRESENTATION
A 82‐year‐old man with history of hypertension, type 2 diabetes mellitus, percutaneous coronary intervention (PCI) of the right coronary artery (RCA), coronary artery bypass grafting, and a left ventricular ejection fraction of 25% presented with progressive class III angina. Diagnostic coronary angiography revealed chronic total occlusions of the RCA and left circumflex, and a left anterior descending coronary artery (LAD) with a heavily calcified high‐grade stenosis (minimal lumen diameter of 0.35 mm and diameter stenosis of 81%) (Figure 1a). The left internal mammary arterial graft to the LAD showed a significant stenosis proximal to the anastomosis. Subsequent PCI of the proximal LAD was performed with rotational atherectomy (1.5 mm burr) and pre‐dilatation with a non‐compliant (NC) 3.0 mm balloon (20 atm); an Onyx DES 3.5 × 38 mm was implanted and despite post‐dilatation with NC 3.5 mm balloon (24 atm), significant stent underexpansion persisted.(Figure 1b,c). Optical coherence tomography (OCT) showed concentric thick deep calcification and a minimal lumen area (MLA) of 1.72 mm2 (Figure 2a–c asterisks). A 2.5 × 12 mm shockwave balloon (Shockwave Medical, Inc., Fremont, CA) was positioned, inflated to 4 atm and eight coronary lithoplasty therapies were applied; then, the balloon was inflated to 6 atm to enhance balloon compliance, however, still no full expansion was noticed (Figure 3a). Further post‐dilatation was performed with a 3.5 mm NC balloon (22 atm) resulting in complete stent expansion (Figure 3b,c). Post‐PCI OCT showed multiple calcium cracks along the circumference and an MLA of 4.86 mm2 (Figure 4a–c arrows). The procedure finalized without complications.
Figure 1.
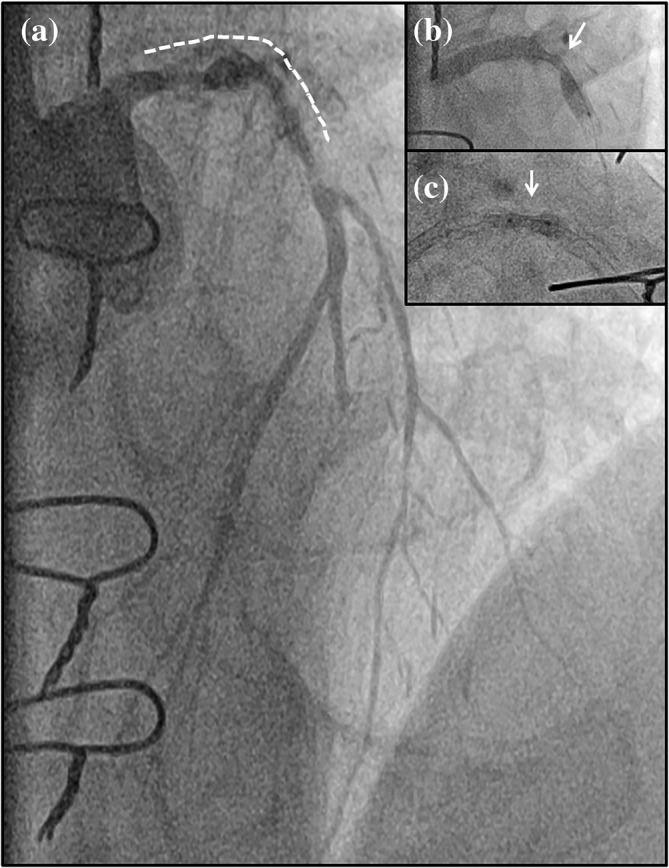
Angiography pre‐lithoplasty. (a) Angiography pre‐intervention, cranial view of the left descending coronary artery; (b) Persistent stent underexpansion (arrow); (c) Post‐dilatation with non‐compliant balloon showing balloon underexpansion (arrow)
Figure 2.
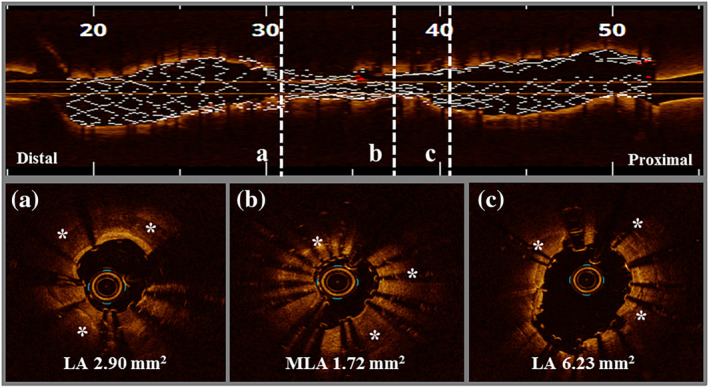
Optical coherence tomography pre‐lithoplasty. Optical coherence tomography of the left anterior descending coronary artery pre‐lithoplasty showing circumferential deep calcification (asterisks). Longitudinal view (upper row). Transversal view (bottom row). LA, lumen area; MLA, minimal lumen area [Color figure can be viewed at wileyonlinelibrary.com]
Figure 3.
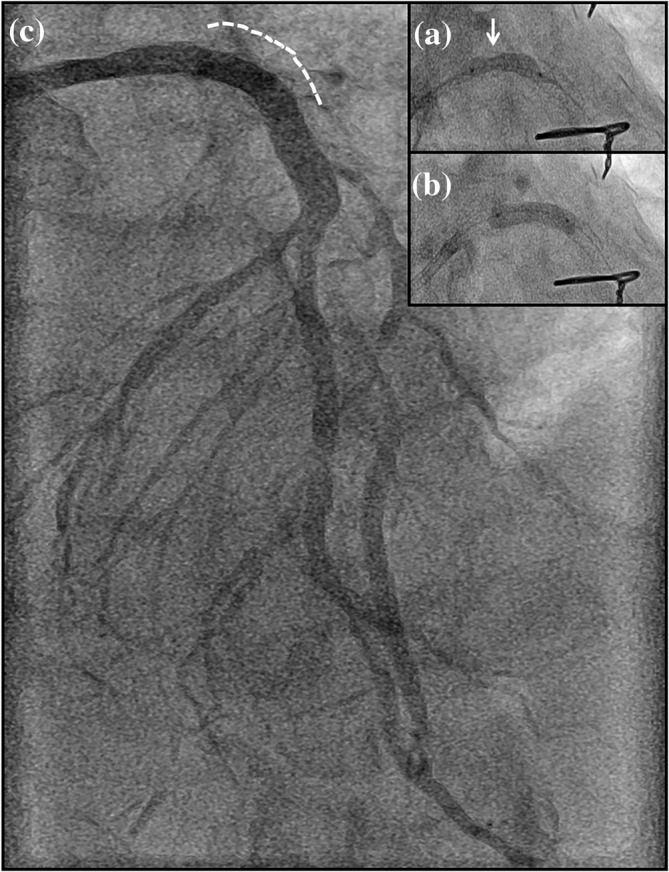
Angiography post‐lithoplasty. (a) Lithoplasty balloon with slightly incomplete expansion after eight lithoplasty therapies (arrow); (b) Post‐lithoplasty non‐compliant balloon dilatation showing complete balloon expansion; (c) Angiography final result, cranial view of the left descending coronary artery
Figure 4.
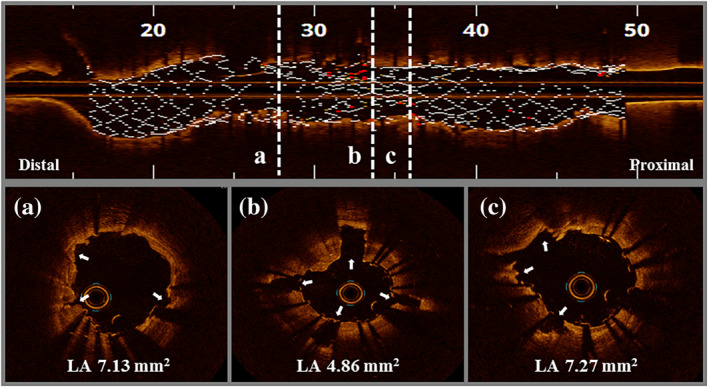
Optical coherence tomography post‐lithoplasty. Optical coherence tomography of the left anterior descending coronary artery post‐intervention showing deep calcium cracks (arrows). Longitudinal view (upper row). Transversal view (bottom row). LA, lumen area [Color figure can be viewed at wileyonlinelibrary.com]
3. DISCUSSION
Calcified coronary lesions increase the risk of suboptimal PCI results and future adverse cardiac events.2 The success of preparation of heavily calcified lesions strongly depends on extend and localization of calcium. Moreover, rotational atherectomy proved to be less efficacious in case of deep, thick, and concentric calcifications. The Shockwave Coronary Rx Lithoplasty® System (Shockwave Medical, Inc.) conversely is capable of creating multiple calcium fractures through the vessel wall by delivering unfocused acoustic pulse waves. An OCT substudy reported deep dissections in 12.9% of the cases after lithoplasty therapy, revealing its effect in deep calcium depositions, of note, following stenting, no edge dissections were observed, an neither any signs of flow impairment, abrupt vessel closure, or perforations reported, which overall illustrates the safety of the technique.4
Although typically used to prepare heavily calcified lesions pre‐stenting, previous case reports described the successful and safe off‐label use of the technology to improve stent underexpansion.5, 6 As demonstrated in our case, deep concentric calcifications did not suffer significant modification after conventional plaque‐modification techniques, resulting in persistent severe stent underexpansion. It was only after coronary lithoplasty application that NC balloons could be fully expanded.
Despite the fact that no important complications have been reported so far, more data are needed to further assess the safety and efficacy of this technique in underexpanded stents. In the meantime, the lithoplasty therapy could be considered as a bailout technique in those situations.
4. CONCLUSION
The present case supports the use of coronary lithoplasty as an adjuvant therapy to efficiently disrupt circumferential deep calcification, event after failed rotablation.
Tovar Forero MN, Van Mieghem NM, Daemen J. Stent underexpansion due to heavy coronary calcification resistant to rotational atherectomy: A case for coronary lithoplasty? Catheter Cardiovasc Interv. 2020;96:598–600. 10.1002/ccd.28641
REFERENCES
- 1. Lee MS, Shah N. The impact and pathophysiologic consequences of coronary artery calcium deposition in percutaneous coronary interventions. J Invasive Cardiol. 2016;28(4):160‐167. [PubMed] [Google Scholar]
- 2. Albrecht D, Kaspers S, Fussl R, Hopp HW, Sechtem U. Coronary plaque morphology affects stent deployment: assessment by intracoronary ultrasound. Cathet Cardiovasc Diagn. 1996;38(3):229‐235. [DOI] [PubMed] [Google Scholar]
- 3. Farag M, Costopoulos C, Gorog DA, Prasad A, Srinivasan M. Treatment of calcified coronary artery lesions. Expert Rev Cardiovasc Ther. 2016;14(6):683‐690. [DOI] [PubMed] [Google Scholar]
- 4. Ali ZA, Brinton TJ, Hill JM, et al. Optical coherence tomography characterization of coronary lithoplasty for treatment of calcified lesions: first description. JACC Cardiovasc Imaging. 2017;10(8):897‐906. [DOI] [PubMed] [Google Scholar]
- 5. Tovar Forero MN, Wilschut J, Van Mieghem NM, Daemen J. Coronary lithoplasty: a novel treatment for stent underexpansion. Eur Heart J. 2019;40(2):221. [DOI] [PubMed] [Google Scholar]
- 6. Ali ZA, McEntegart M, Hill JM, Spratt JC. Intravascular lithotripsy for treatment of stent underexpansion secondary to severe coronary calcification. Eur Heart J. 2020;41(3):485–486. [DOI] [PubMed] [Google Scholar]


