Abstract
Objectives
We aimed to study the incidence rate, predictors and outcomes of HIV care interruption (HCI) in Belgium.
Methods
We analysed data for adult patients with at least two HIV care records in the Belgian HIV cohort between 1 January 2007 and 31 December 2016. An HCI episode was defined as 1 year without an HIV care record. The HCI incidence rate was analysed using Poisson regression, return to HIV care using a cumulative incidence function with death as a competing risk, and viral load (VL) status upon return to HIV care using logistic regression.
Results
We included 16 066 patients accounting for 78 625 person‐years of follow‐up. The incidence rate of HCI was 5.3/100 person‐years [95% confidence interval (CI) 5.1–5.4/100 person‐years]. The incidence of return to HIV care after HCI was estimated at 77.5% (95% CI 75.7–79.2%). Of those who returned to care, 43.7% had a VL ≤ 200 HIV‐1 RNA copies/mL, suggesting care abroad or suboptimal care (without an HIV‐related care record) in Belgium during the HCI, and 56.3% returned without controlled VL and were therefore considered as having experienced a real gap in HIV care; they represented 2.3/100 person‐years of follow‐up. Factors individually associated with HCI were no antiretroviral therapy (ART) uptake, lower age, injecting drug use, non‐Belgian nationality, male gender, not being a man who has sex with men, a shorter time since HIV diagnosis, no high blood pressure and CD4 count < 350 cells/µL.
Conclusions
This study highlights the need to investigate return to care and viral status at return, to better understand HCI. Identified predictors can help health care workers to target patients at higher risk of HCI for awareness and support.
Keywords: HIV care, loss to follow‐up, maintenance, retention, re‐engagement
Introduction
Since the introduction of antiretroviral therapy (ART) and the resulting increase in life expectancy among HIV‐infected people [1], HIV infection has evolved to become a chronic disease requiring decades of engagement in dedicated care for more and more patients. Sustained maintenance of the patients in HIV care and on ART is crucial to ensure the best outcomes in terms of mortality and morbidity, and to reduce onward transmission [2]. Nevertheless, this is a challenge for a number of patients [3].
Retention in care is one of the key stages of the continuum of HIV care [4, 5]. In Belgium, this step is amongst those with the highest attrition [6]. Improving retention in care would therefore further support our national progress towards the Joint United Nations Programme on HIV/AIDS (UNAIDS) targets [7].
In Belgium, HIV care is well structured and mainly centralized in 12 multidisciplinary specialized care centres, the HIV reference centres (HRCs). Patients might also consult in other hospitals or in primary care. High ART uptake (> 97% in 2017) and viral load (VL) control (> 95% of those on ART) are reported for those in regular care [8]. HIV care is guided by the European AIDS Clinical Society (EACS) guidelines, which recommend a medical visit with a VL measurement every 3–6 months [9].
Studies on HIV care interruption (HCI) and loss to follow‐up in European countries have reported incidence rates of around 2.5–3.5/100 person‐years [10, 11, 12]. In a large multi‐country European cohort study, 50% of the patients had, between 1995 and 2005, a period of > 1 year without a follow‐up visit [13]. In one Belgian HRC, an incidence rate of loss to follow‐up of 5.5/100 persons each year was observed between 1999 and 2009 [14]. Comparison between studies is hampered by differing approaches for selection of the population studied and the lack of standardized definitions for ‘loss to follow‐up’ and ‘HCI’. This is partly a consequence of the diversity of situations leading to HCI, as illustrated in Fig. 1. Patients might permanently leave the national HIV care system as a result of out‐migration, or might receive care abroad before returning to care in Belgium. Alternatively, patients might have ART renewal in Belgium without HIV medical follow‐up and hence without VL records, which would be considered as suboptimal care. Finally, patients might experience a real gap in HIV care before return to care. Disentangling the diverse pathways underlying HCI will inform actions to improve long‐term maintenance in HIV care.
Fig. 1.
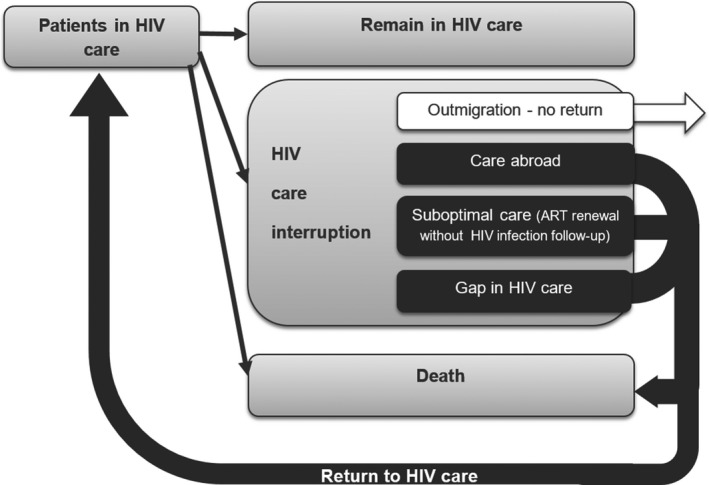
Diagram of HIV care interruption pathways. ART, antiretroviral therapy.
This study aimed to study HCI in Belgium and to better understand the drivers of the different pathways, particularly for those experiencing a real gap during their HCI in Belgium.
Methods
Study setting and population
The Belgian HIV cohort study was set up in 2007. It includes data on all HIV‐infected patients in care in Belgium collected from the AIDS reference laboratories (ARLs) and the HRCs. All VL measurements in the country are performed and reported by the ARLs. This provides a national coverage of the patients in HIV care. HRCs follow > 80% of the HIV‐infected patients in care in the country. Those not attending HRCs are mainly followed up in other hospitals and, less frequently, in primary care. A description of the Belgian HIV cohort was previously published [15].
The cohort data include a reliable unique patient identifier based on a combination of the encrypted civil registry number and a code using gender and date of birth. Nevertheless, missing or erroneous records may occur. This is more frequent for patients with HIV follow‐up outside of HRCs. We therefore focused our analysis on those in care in HRC to ensure the most reliable patient identifier.
In this study, we analysed data for patients aged ≥ 18 years, with at least two records of HIV care in HRCs between 1 January 2007 and 31 December 2016.
Data collection
Routine individual patient data are collected annually from HRCs and ARLs. Demographic information and VL results are collected from both HRCs and ARLs. Clinical and additional laboratory information is collected from HRCs.
Death data were extracted from medical records and reported by the HRCs. In addition, some HRC and ARL databases are linked to Belgium’s civil registry, allowing identification of additional deaths declared among their patients.
HIV data collection is performed by Sciensano, the Belgian Scientific Institute of Public Health, which is legally entitled to carry out HIV surveillance in Belgium (Royal Decree of 8 October 1996). The HIV surveillance was authorized by an independent administrative authority protecting privacy and personal data (https://www.autoriteprotectiondonnees.be/sites/privacycommission/files/documents/d%C3%A9lib%C3%A9ration_SS_017_2014.pdf), and approved by the ethical committee of Ghent University Hospital (RN B670201420495).
Definition of outcomes and variables
The first outcome studied was the incidence rate of HCI. An HIV care record was defined as a measurement of CD4 count or VL, or a medical visit in an HRC. The study start date was defined as 1 January 2007 for those previously in care in HRCs or as the date of first HIV care record for those entering care later. An episode of HCI was defined as the occurrence of 1 year without an HIV care record in HRCs if the patient did not die or have a VL record outside of HRCs (reported by ARLs) during this period. In the case of an HCI, data were censored at the date of the last record preceding the HCI. In the case of a VL reported outside HRCs during the 1‐year period, patients were considered as having shifted to care outside HRCs and were censored at the date of VL measurement reported by the ARL. Patients who died were censored at the date of death. If none of these events occurred, data were censored at 31 December 2016. Care records were analysed up to 31 December 2017 to ensure that there was the 1‐year period of hindsight required to define an HCI.
The second outcome studied was the cumulative incidence of return to HIV care, analysed among those presenting an HCI. The analysis period began after the first year of HCI. It was censored at the date of return to HIV care, the date of death or 31 December 2017, whichever occurred first. Return to HIV care was defined as a care record in an HRC or a VL record outside an HRC (reported by an ARL).
The third outcome studied was the VL status upon return to HIV care. Patients presenting a VL ≤ 200 copies/mL upon return to care were considered as having accessed ART during their period of HCI, either through HIV care abroad or through suboptimal care in Belgium (ART renewal without VL follow‐up). Those having a VL > 200 copies/mL were classified as having experienced a gap in care.
The following patient characteristics were assessed for their association with each outcome: gender, age, mode of HIV acquisition, nationality, time since diagnosis of HIV infection, CD4 count, ART uptake, HRC of care and year of care. Urbanization of place of residence was categorized into three levels of population density based on a European method applied to the Belgian census data [16, 17, 18]. Income data for municipality of residence was retrieved from the Belgian statistical office as the average net taxable income per capita per municipality [19]. Income was divided into three terciles. High systolic blood pressure was defined as at least one measurement > 140 mmHg during follow‐up; it was used as an indicator of higher risk of comorbidity. Smoking (at least one record of smoking during follow‐up) and obesity [at least one measurement of body mass index (BMI) > 30 kg/m2 during follow‐up] were used to identify those with an unhealthy lifestyle. Regularity of care was defined as at least one HIV care record in each semester during the year preceding censoring.
Statistical analyses
To deal with missing values among risk factors (proportion of missing values per variable reported in Table 1), multiple imputation was applied to the data prior to statistical analyses. The sas mi procedure was used to generate 10 imputed data sets (SAS Institute, Cary, NC). The imputation process included all the studied factors and the postal code as an auxiliary variable. Models for analyses of HCI, return to HIV care and VL status at return were applied to each imputed data set and parameter estimates were subsequently combined into a single set of results for each model using the sas proc mianalyze statement.
Table 1.
Sociodemographic and selected behavioural and clinical characteristics of patients in care for HIV, Belgium, 2007–2016
| Characteristic | |
|---|---|
| Sex [n = 16 026; number missing: 40 (0.2%)] | |
| Male | 10 560 (65.9) |
| Female | 5448 (34.0) |
| Other | 18 (0.1) |
| Age at baseline (n = 16 066; number missing: 0) | |
| Age (years) [mean (SD)] | 40 (11) |
| Mode of HIV acquisition [n = 14 493; number missing: 1573 (9.8%)] | |
| Heterosexual | 7571 (52.2) |
| MSM | 6091 (42.0) |
| IDU | 365 (2.5) |
| MTCT | 174 (1.2) |
| Other | 292 (2.0) |
| Nationality [n = 15 353; number missing: 713 (4.4%)] | |
| Belgian | 8209 (53.5) |
| SSA | 4488 (29.2) |
| European | 1608 (10.5) |
| Other | 1048 (6.8) |
| Time period of HIV diagnosis [n = 15 349; number missing: 717 (4.5%)] | |
| 1980–1989 | 678 (4.4) |
| 1990–1999 | 3010 (19.6) |
| 2000–2009 | 6655 (43.4) |
| 2010–2016 | 5006 (32.6) |
| Nadir CD4 count [n = 15 938; number missing: 128 (0.8%)] | |
| < 350 cells/µL | 8396 (52.7) |
| ≥ 350 cells/µL | 7542 (47.3) |
| ART status [n = 15 237; number missing: 829 (5.2%)] | |
| Ever on ART | 14 117 (92.6) |
| No ART | 1120 (7.4) |
| Systolic blood pressure [n = 9430; number missing: 6636 (41.3%)] | |
| High | 2909 (30.8) |
| Normal | 6521 (69.2) |
| Smoking [n = 8887; number missing: 7179 (44.7%)] | |
| Yes | 3472 (39.1) |
| No | 5415 (60.9) |
| BMI [n = 7565; number missing: 8501 (52.9%)] | |
| ≥ 30 (obese) | 1151 (15.2) |
| < 30 | 6414 (84.8) |
ART, antiretroviral therapy; BMI, body mass index; IDU, injecting drug use; MSM, men who have sex with men; MTCT, mother to child transmission; SD, standard deviation; SSA, sub‐Saharan African.
The incidence rate of the first HCI and associated factors were analysed with Poisson regression. Return to HIV care for those presenting an HCI was assessed using the cumulative incidence function (CIF) with death as a competing risk and associated factors were identified using cause‐specific hazard models. VL status upon return to HIV care and associated factors were analysed using logistic regression.
The variables age, time since HIV diagnosis, year of care, ART and CD4 count were considered time‐varying for the HCI analysis and stratified by Lexis expansion. For the analyses of return to HIV care and VL status upon return, their values at the time of HCI were used.
All analyses were performed in sas eg version 7.13.
Results
Population description
Over the 10‐year study period, 18 891 patients were followed for HIV in Belgium. Of these, 16 066 (85%) patients in care in the HRCs were included in the analysis, accounting for 78 625 person‐years of follow‐up. Most patients were male, and the median age at inclusion was 39 years. The reported mode of HIV acquisition was heterosexual in 52% of patients, men who have sex with men (MSM) in 42%, injecting drug use (IDU) in 3%, mother‐to‐child transmission (MTCT) in 1% and other (contaminated blood products for transfusion or haemophilia treatment) in 2%. Half (53%) of the patients were Belgians, 29% sub‐Saharan Africans, 11% non‐Belgian Europeans and 7% of other nationalities. Table 1 presents characteristics of the patients.
HIV care interruption and return to HIV care
During the study period, 4151 (25.8%) patients interrupted HIV care, 2160 (13.4%) received care outside HRCs, 417 (2.6%) died and 9338 (58.1%) were retained in care without experiencing any of those events. The incidence rate of HCI was 5.3/100 person‐years [95% confidence interval (CI) 5.1–5.4/100 person‐years].
Of those who had interrupted care for at least 1 year, 2364 (57.0%) subsequently returned to HIV care in an HRC, 421 (10.1%) returned to care outside HRCs, eight (0.2%) died and 1358 (32.5%) remained out of Belgian HIV care up to 31 December 2017. After the initial 1‐year period of HCI, the cumulative incidence of return to HIV care within a maximum period of 8 years was estimated at 77.5% (95% CI 75.7–79.2%), with 51.4% (95% CI 49.8–53.0%) and 72.4% (95% CI 70.8–73.9%) returning within, respectively, 1 and 5 years (Fig. 2). The median time to return to HIV care was 179 days [interquartile range (IQR) 50–496 years].
Fig. 2.
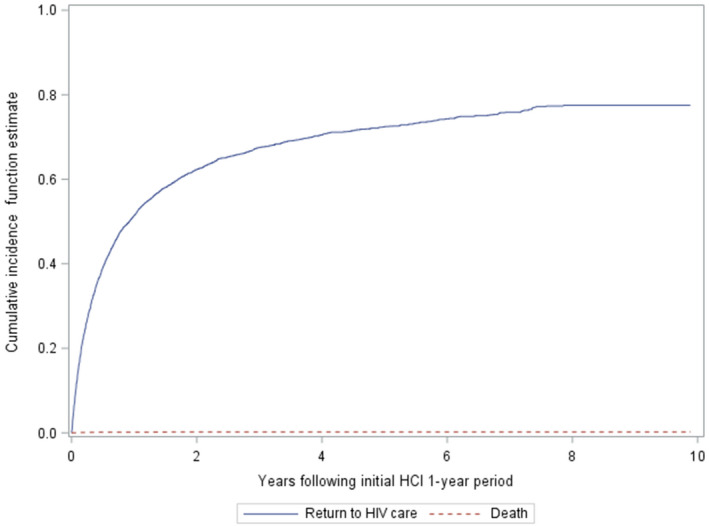
Cumulative incidence of return to HIV care and death after the initial 1‐year period of HIV care interruption (HCI) in Belgium.
A VL measurement was available upon return into HIV care for 2695 patients (97%). Of these, 1178 (43.7%) had a controlled VL, suggesting alternative access to medical care and ART during the HCI period, and 1517 (56.3%) had uncontrolled VL and were considered to have experienced a gap in HIV care.
By combining the results of the cumulative incidence model with the assessment of VL status upon return to care, incidence rates by type of HCI were estimated. The incidence rate of HCI related to out‐migration was 1.2/100 person‐years in care (22.3% × 5.3/100 person‐years). The incidence rate of HCI with care abroad or with ART renewal without VL follow‐up was 1.8/100 person‐years in care (77.5% × 43.7% × 5.3/100 person‐years). HCI with a gap in HIV care had an incidence rate of 2.3/100 person‐years in care (77.5% × 56.3% × 5.3/100 person‐years) and HCI followed by death had an incidence rate of 0.01/100 person‐years in care (0.2% × 5.3/100 person‐years).
Associated factors
After adjustment, a higher incidence rate of HCI was strongly associated with no ART uptake and moderately associated with younger age, IDU, non‐Belgian nationality, more recent HIV diagnosis and low CD4 count (Table 2). A lower incidence rate of HCI was moderately associated with female gender, being MSM and high blood pressure. Smoking, obesity, urbanization level and income of place of residence were not associated with the incidence rate of HCI. Those having regular care during the last year of observation had a higher incidence rate of HCI than others. The HCI incidence rates were lower in the period 2007–2011 compared to the following years.
Table 2.
Crude and adjusted relative risks (RRs) for HIV care interruption (HCI), for return to HIV care and for experiencing a gap during HCI, Belgium, 2007–2016
| All patients in HIV care | Patients in HCI | Patients who returned to care | ||||
|---|---|---|---|---|---|---|
| Crude RR for HCI | Adjusted RR for HCI | Crude HR for return | Adjusted* HR for return | Crude OR for gap | Adjusted* OR for gap | |
| Gender | ||||||
| Male | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Female | 1.1 (1.1–1.2) | 0.8 (0.8–0.9) | 1.2 (1.1–1.3) | 1.1 (1.0–1.3) | 1.2 (1.0–1.4) | 1.4 (1.1–1.6) |
| Age | ||||||
| 18–24 years | 3.4 (3.0–3.9) | 2.1 (1.8–2.5) | 1.1 (0.9–1.3) | 1.4 (1.1–1.6) | 6.1 (4.2–9.1) | 3.9 (2.5–6.2) |
| 25–39 years | 2.1 (1.9–2.3) | 1.6 (1.4–1.7) | 1.0 (0.9–1.1) | 1.2 (1.1–1.4) | 3.2 (2.6–4.0) | 2.5 (1.9–3.2) |
| 40–49 years | 1.4 (1.3–1.5) | 1.2 (1.1–1.3) | 1.1 (1.0–1.2) | 1.1 (1.0–1.3) | 1.8 (1.4–2.3) | 1.7 (1.3–2.1) |
| ≥ 50 years | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Mode of HIV acquisition | ||||||
| Heterosexual | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| MSM | 0.7 (0.7–0.8) | 0.7 (0.6–0.8) | 0.8 (0.8–0.9) | 0.9 (0.8–1.0) | 1.2 (1.0–1.4) | 1.1 (0.9–1.5) |
| IDU | 1.9 (1.6–2.2) | 1.5 (1.2–1.8) | 1.0 (0.8–1.2) | 1.1 (0.9–1.3) | 0.9 (0.6–1.4) | 0.8 (0.5–1.2) |
| MTCT | 1.1 (0.8–1.5) | 0.8 (0.6–1.1) | 1.5 (1.1–2.0) | 1.1 (0.8–1.6) | 1.8 (0.9–3.6) | 1.6 (0.7–3.7) |
| Other | 0.9 (0.7–1.1) | 0.9 (0.7–1.2) | 0.7 (0.5–1.0) | 0.7 (0.5–1.0) | 0.9 (0.5–1.6) | 0.9 (0.5–1.8) |
| Nationality | ||||||
| Belgian | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| SSA | 1.7 (1.6–1.9) | 1.4 (1.3–1.6) | 0.8 (0.7–0.8) | 0.7 (0.7–0.8) | 1.1 (0.9–1.3) | 1.1 (0.9–1.3) |
| European | 2.1 (1.9–2.3) | 1.8 (1.6–2.0) | 0.4 (0.4–0.5) | 0.5 (0.4–0.6) | 0.9 (0.7–1.2) | 0.7 (0.5–1.0) |
| Other | 2.0 (1.7–2.2) | 1.5 (1.3–1.7) | 0.6 (0.5–0.6) | 0.7 (0.5–0.8) | 1.0 (0.7–1.4) | 0.8 (0.6–1.2) |
| Systolic BP | ||||||
| Normal | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | 0.7 (0.7–0.8) | 0.8 (0.8–0.9) | 1.1 (1.0–1.2) | 1.0 (0.9–1.1) | 0.7 (0.6–0.9) | 0.9 (0.7–1.1) |
| Obesity | ||||||
| BMI < 30 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| BMI ≥ 30 | 1.2 (1.1–1.3) | 1.1 (1.0–1.3) | 1.1 (0.9–1.2) | 1.0 (0.9–1.1) | 1.0 (0.8–1.4) | 1.1 (0.8–1.5) |
| Smoking | ||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.0 (0.9–1.0) | 1.1 (1.0–1.2) | 1.0 (0.9–1.1) | 1.1 (0.9–1.2) | 1.1 (0.9–1.4) | 1.1 (0.8–1.4) |
| Time since HIV diagnosis | ||||||
| < 1 year | 3.2 (2.9–3.5) | 1.3 (1.1–1.4) | 0.5 (0.4–0.5) | 0.5 (0.5–0.6) | 4.4 (3.3–5.9) | 1.4 (0.7–2.0) |
| 1 to 3 years | 1.7 (1.6–1.9) | 1.0 (0.9–1.1) | 0.7 (0.6–0.7) | 0.7 (0.7–0.8) | 2.8 (2.2–3.6) | 1.1 (0.9–1.3) |
| > 3 to 10 years | 1.3 (1.2–1.4) | 1.0 (0.9–1.1) | 0.8 (0.7–0.9) | 0.8 (0.8–0.9) | 1.7 (1.4–2.0) | 2.2 (1.7–2.9) |
| > 10 years | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| CD4 count | ||||||
| ≥ 350 cells/µL | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| < 350 cells/µL | 2.4 (2.2–2.6) | 2.2 (2.0–2.4) | 0.8 (0.7–0.9) | 0.8 (0.7–0.9) | 2.1 (1.7–2.6) | 2.2 (1.7–2.9) |
| ART | ||||||
| Yes | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| No | 4.6 (4.3–4.9) | 4.4 (4.1–4.7) | 0.9 (0.9–1.0) | 1.1 (1.0–1.2) | 7.0 (5.6–8.8) | 5.3 (4.1–6.9) |
| Degree of urbanization | ||||||
| Low | 0.9 (0.8–1.0) | 0.9 (0.7–1.0) | 1.0 (0.8–1.3) | 1.1 (0.9–1.3) | 1.0 (0.7–1.4) | 1.0 (0.7–1.5) |
| Mid | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | 1.2 (1.1–1.3) | 1.0 (0.9–1.1) | 0.9 (0.8–1.1) | 1.0 (0.9–1.1) | 1.1 (0.9–1.4) | 1.1 (0.9–1.4) |
| Municipality income | ||||||
| Low | 1.2 (1.1–1.3) | 1.0 (0.9–1.2) | 0.9 (0.8–1.0) | 0.9 (0.8–1.1) | 1.0 (0.8–1.3) | 1.1 (0.8–1.4) |
| Mid | 1.1 (1.0–1.2) | 0.9 (0.8–1.0) | 1.0 (0.9–1.2) | 1.0 (0.9–1.2) | 1.0 (0.8–1.2) | 1.0 (0.8–1.3) |
| High | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Regularity of HIV care | ||||||
| Regular | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Not regular | 0.9 (0.8–1.1) | 0.8 (0.7–0.9) | 1.3 (1.1–1.5) | 1.2 (1.0–1.4) | 1.1 (0.8–1.6) | 1.0 (0.7–1.5) |
P < 0.05 statistically significant variables shown in boldface.
ART, antiretroviral therapy; BMI, body mass index; BP, blood pressure; HR, hazard ratio; IDU, injecting drug use; MSM, men who have sex with men; MTCT, mother to child transmission; OR, odds ratio; SD, standard deviation; SSA, sub‐Saharan African.
Relative risks are adjusted for all variables statistically significant in univariate analysis and HIV reference centre (HRC) and year of HIV care (year of HCI for the analyses of return to care and gap in care).
For those presenting an HCI, return to HIV care was associated, after adjustment, with younger age and female gender. HIV diagnosis in more recent years, non‐Belgian nationality, being MSM, other mode of HIV acquisition and low CD4 count at HCI were associated with a lower likelihood of return to care. For those who returned to HIV care, factors associated with experiencing a gap during HCI in the multivariable analysis were female gender, younger age, a more recent HIV diagnosis, no ART uptake at HCI and a low CD4 count at HCI. Europeans had a lower risk of gap compared to other nationalities.
Immune status and evolution after a gap in HIV care
Among the patients who returned to care after a gap and with an available CD4 count at the time of return (n = 1246), 31.4% had a CD4 count < 200 cells/µL, 23.0% a CD4 count of between 200 and 349 cells/µL and 45.6% a CD4 count of ≥ 350 cells/µL. The mean decrease in CD4 count during the gap in care was 75 cells/µL/year (95% CI 68.9–81.2 cells/µL/year).
The incidence rate of death amongst all patients who remained in HIV care was 0.5/100 person‐years (95% CI 0.5–0.6/100 person‐years). In comparison, the incidence rate of death in the year following return to care after a gap was 1.0/100 person‐years (95% CI 0.6–1.7/100 person‐years; P = 0.02), and 2.7/100 person‐years (95% CI 1.4–5.0/100 person‐years; P < 0.0001) for those with a CD4 count < 200 cells/µL upon return to care.
Discussion
Each year, one in 20 HIV‐infected patients in care presents an HCI in Belgium. This study of data representing a 10‐year period allowed the assessment of longstanding care relationships for 85% of the patients in care in Belgium even if they changed the centre of HIV care, thanks to multicentric data collection.
Analysis of return to care and health status upon return is necessary to disentangle the various possible reasons for the HCI. The estimated incidence rate of a gap in HIV care was 2.3/100 HIV‐infected persons in care in Belgium per year. This seems in line with studies in other Western European countries [10, 11] although comparison should be made with caution given the varying definitions of HCI and approaches to handling out‐migration in these analyses.
Patients with a gap in HIV care who have detectable VLs may contribute to HIV transmission in the community. Moreover, those patients were more vulnerable to poor clinical evolution, with a higher mortality incidence rate in the year following their return to care, compared with mortality incidence rates of patients maintained in HIV care. Significantly higher mortality rates were found in those who had CD4 counts < 200 cells/µL upon return to care. Given that patients with low CD4 counts had twice the rate of HCI and also a higher risk of a gap during HCI, this finding suggests that especially prompt and intensive intervention for retention in care is required in the case of missed appointments among patients with low CD4 counts.
ART uptake was the strongest predictor of better retention in HIV care identified by our analysis. In Belgium, initiation of ART was contingent upon a CD4 count < 500 cells/µL or the presence of clinical symptoms up to 1 December 2016. From then on, initiation of ART for all HIV‐infected patients was implemented. Observed ART coverage in the HRCs increased from 75% in 2007 to 97% in 2017 [8]. Given the strong association of ART with retention in care, we might expect the high ART coverage to reinforce regular care in recent years and in the future.
Younger patients were more vulnerable to HCI and to a gap in HIV care, in line with the findings of other studies [3, 20, 21, 22, 23], but were less prone to permanent out‐migration. It may be particularly challenging for young people to cope at once with the stigmatizing dimension of the disease, its impact on their sexual and emotional wellbeing and the necessary commitment to life‐long medical care [20, 24]. Also, increased mobility of young people related to relationships, jobs and study might impact on their capacity to remain in HIV care. Other demographic predictors of HCI identified in this analysis were male gender and foreign nationality; those who were male or of foreign nationality were less likely to return to HIV care in Belgium as a consequence of higher permanent out‐migration during HCI. MSM were less likely to experience HCI compared to heterosexuals, as reported in the literature [10, 11, 25, 26, 27].
Injecting drug users had higher incidence rates of HCI. Assessment of drug use, including “chemsex”, which has been increasingly reported among people living with HIV [28], should be performed regularly for patients in HIV care to enable provision of targeted advice, support and possibly referral to drug treatment services for collaborative care. Use of other substances such as alcohol was identified as a predictor of HCI in other studies [3, 20, 23], although no data on these exposures were available in this study.
Difficulties in facing a recent diagnosis of HIV infection may contribute to the higher incidence rates of HCI for those recently diagnosed. For those in HCI, a recent diagnosis was associated with a higher hazard of no return to care as a consequence of out‐migration, and a higher risk of a gap for those returning to care in Belgium. The period following diagnosis is crucial, as poor engagement in HIV care during the first year following diagnosis is associated with higher mortality [29]. A greater frequency of medical contacts when initiating treatment increases opportunities for providing targeted support for engagement in HIV care to newly diagnosed patients facing social or administrative barriers. In contrast to our findings, in both a Spanish and an English study, recently diagnosed patients had fewer missed medical appointments [25, 30], but these studies did not examine retention in HIV care over a long period.
Irregular care did not predict subsequent HCI in our study. Many of the patients with irregular care according to our definition had in fact very stable HIV disease requiring less frequent medical visits. Those in regular care who experienced more HCI might include patients identified as more vulnerable to HCI for whom clinicians plan more frequent visits.
Patients with a higher risk of comorbidity were less prone to HCI, in line with a previous study showing a dose–response relationship between the number of comorbidities and optimal retention [21]. We found no association between HCI and indicators of unhealthy lifestyle, nor with urbanization or income levels of place of residence. A recent Swiss study also found no association between neighbourhood socio‐economic position and loss to follow‐up [31].
Our analysis of determinants of HCI or a gap in HIV care was restricted to factors available in the cohort data. Other individual factors such as mental illness and perceived stigma [32, 33] or aspects related to health care services and external environment [23, 32] may also play a key role in retention in HIV care in Belgium. For example, a confident relationship with the HIV care provider and a facilitating health care structure, with features such as ease of reach by phone, ease of appointment taking, extended hours of consultation, automatic text messages or pre‐consultation reminder phone calls and a positive waiting room experience, have frequently been reported as facilitators [12, 33, 34, 35, 36].
Guidelines for HIV care recommend a routine assessment at entry into HIV care of new patients [9]. Based on the factors identified in this study and in others, the information gathered might be used to identify patients at increased risk of HCI and provide them with targeted support. Peers could play a role here, as shown in UK and US programmes reporting enhanced patient empowerment, retention in care and adherence to treatment following peer interventions [27, 37].
Guidelines [9] advise an HIV care visit every 3–6 months. We used a definition of 1 year without an HIV care record to allow some flexibility for stable patients spacing their appointments while remaining properly followed up. Various metrics have been used to study regularity of HIV care, each with its own strengths and weaknesses [30, 38]. Our definition is relevant for an epidemiological approach to HCI and its predictors. In clinical practice, with the aim of early intervention for patients deviating from regular care to prevent long‐term attrition, monitoring of missed appointments is more suitable and easier to implement routinely.
In the case of an HCI or missed appointment, prompt contact with the patient for return to care is facilitated if all contact information for the patient is available, for instance through a systematic assessment at initiation of care of the patient’s agreement to be contacted and the preferred means of contact. This topic could be added to the initial assessment section of HIV care guidelines. Tracing of patients might be facilitated if they have a regular general practitioner (GP); it has also been shown that those with a regular GP have fewer missed appointments [27]. The potential use of the Belgian eHealth [39] system – electronic exchange of health‐related data between health care providers – for supporting retention and return to care should be further explored.
This study helped to disentangle the heterogeneity of situations underlying HCI by looking at the three main pathways defined for our analysis. Nevertheless, medical care during HCI was not fully captured. For instance, patients returning to care with a controlled VL after HCI were grouped as a single entity although their individual care use during HCI may have been diverse, including care abroad, incarceration and various patterns of access to ART. Also, the group of patients classified as having experienced a gap in care based on uncontrolled VL upon return might present heterogeneity in terms of a partial or complete gap in care throughout the HCI. Further research using alternative sources of medical data will help to refine our understanding of individual HIV care trajectories.
This study has limitations. First, our analysis did not include patients receiving care exclusively outside HRCs, who represented 15% of all patients in HIV care in Belgium during the study period. They differed from those followed in the HRCs, with slightly more people who inject drugs, fewer MSM, more women and fewer Belgians [6]. As these characteristics are associated with HCI incidence rate, our results may slightly underestimate the national levels of HCI. Secondly, the cohort included both patients who entered care after the study start date and patients already in care beforehand. In the case of HCI and return before the study start date, a subsequent episode of HCI during the study period would have been misclassified as first HCI for those patients. Whether incidence rates of repeated and first HCI differ was not captured by the design of our study. Finally, our HIV surveillance is linked to Belgium’s civil registry to ascertain death status in some but not all HRCs. Nevertheless, deaths of patients caused by chronic conditions would probably have been captured in the medical records of the HRC where the patients were in care. A few sudden deaths may have remained unrecorded, and possibly led to a slight underestimation of the number of deaths in our results. As only a few deaths would have been missed, complete absence of care or death records for the whole follow‐up period following HCI was interpreted as out‐migration.
In Belgium, the incidence rate of HCI is low, and less than half of patients experience a real gap in care during the interruption. A high level of access to HIV care in Belgium through fully reimbursed ART and multidisciplinary HIV care centres contributes to limit HCI and facilitate return to HIV care. Young patients, heterosexual men, foreigners, IDUs, those recently diagnosed, those with low CD4 counts and those with a lower risk of comorbidities were found to be at higher risk for HCI and should be targeted for prevention. Such targeting could be supported by the addition of a section in HIV care guidelines on the investigation of HCI risk and means of contact. Despite the decreasing rate of HIV infection in Belgium in recent years, the HIV‐infected population continues to grow and live longer [8]. To allow these individuals to experience the full benefit of therapy and a good health‐related quality of life, awareness and support for long‐term maintenance in HIV care will be increasingly necessary.
Author contributions
DVB and JM defined the research theme. DVB, HVO and JM designed the study. EF, SDW and CWT contributed to data collection. DVB and AS performed the data management. DVB performed the statistical analyses and drafted the manuscript. EF, SDW, AS, HVO and JM supervised the study. All authors contributed to interpretation, reviewed drafts of the manuscript, and approved the final manuscript.
Acknowledgements
We thank the following members of the Belgian Research on AIDS and HIV Consortium (BREACH) for providing the data and supporting the study: S. Allard (HRC UZ Brussel), N. Ausselet (HRC CHU Dinant Godinne), R. Demeester (HRC CHU Charleroi), P. De Munter (HRC UZ Leuven), J.‐C. Goffard (HRC Hôpital Erasme), D. Vaira (HRC/ARL CHU Liège), L. Vandekerckhove (HRC UZ Gent), B. Vandercam (HRC Cliniques Universitaires Saint‐Luc) and J. Van Praet (HRC AZ Sint‐Jan Brugge).
Conflicts of interest: The authors declare no conflicts of interest.
Financial disclosure: The Belgian HIV surveillance, including this study, is financed by the National Institute for Sickness and Invalidity Insurance (INAMI/RIZIV).
References
- 1. Sabin CA. Do people with HIV infection have a normal life expectancy in the era of combination antiretroviral therapy? BMC Med 2013; 27: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sabin CA, Howarth A, Jose S et al Association between engagement in‐care and mortality in HIV‐positive persons: a cohort study. AIDS 2017; 31: 653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Colasanti J, Stahl N, Farber EW, Del RC, Armstrong WS. An Exploratory Study to Assess Individual and Structural Level Barriers Associated With Poor Retention and Re‐engagement in Care Among Persons Living With HIV/AIDS. J Acquir Immune Defic Syndr 2017; 74(Suppl 2): S113–S120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kay E, Batey D, Mugavero M. The HIV treatment cascade and care continuum: updates, goals, and recommendations for the future. AIDS Res Ther 2016; 13: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test‐and‐treat strategies for prevention of HIV infection. Clin Infect Dis 2011; 52: 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Van Beckhoven D, Florence E, Ruelle J et al Good continuum of HIV care in Belgium despite weaknesses in retention and linkage to care among migrants. BMC Infect Dis 2015; 3: 496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. UNAIDS . 90‐90‐90. An ambitious treatment target to help end the AIDS epidemic. Available at: http://www.unaids.org/sites/default/files/media_asset/90‐90‐90_en_0.pdf. Geneva; 2014.
- 8. Sasse A, Deblonde J, Jaminé D, Van Beckhoven D. Epidémiologie du SIDA et de l'infection à VIH en Belgique: Situation au 31 décembre 2017. Brussels: Scientific Institute of Public Health; 2017. Report No.: 67. [Google Scholar]
- 9. European AIDS Clinical Society . EACS guidelines. Version 9.1. 2018.
- 10. Curtis H, Yin Z, Clay K, Brown AE, Delpech VC, Ong E. People with diagnosed HIV infection not attending for specialist clinical care: UK national review. BMC Infect Dis 2015; 15: 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Helleberg M, Engsig FN, Kronborg G et al Retention in a public healthcare system with free access to treatment: a Danish nationwide HIV cohort study. AIDS 2012; 26: 741–8. [DOI] [PubMed] [Google Scholar]
- 12. Ndiaye B, Ould‐Kaci K, Salleron J et al Characteristics of and outcomes in HIV‐infected patients who return to care after loss to follow‐up. AIDS 2009; 23: 1786–9. [DOI] [PubMed] [Google Scholar]
- 13. Mocroft A, Kirk O, Aldins P et al Loss to follow‐up in an international, multicentre observational study. HIV Med 2008; 9: 261–9. [DOI] [PubMed] [Google Scholar]
- 14. Schepens T, Morreel S, Florence E, Koole O, Colebunders R. Incidence and risk factors associated with lost to follow‐up in a Belgian cohort of HIV‐infected patients treated with highly active antiretroviral therapy. Int J STD AIDS 2010; 21: 765–9. [DOI] [PubMed] [Google Scholar]
- 15. Van Beckhoven D, Buve A, Ruelle J, Seyler L, Sasse A. A national cohort of HIV‐infected patients in Belgium: design and main characteristics. Acta Clin Belg 2012; 67: 333–7. [DOI] [PubMed] [Google Scholar]
- 16. Eurostat . Degree of urbanisation classification ‐ 2011 revision. 2019. Available at: https://ec.europa.eu/eurostat/statistics‐explained/index.php/Degree_of_urbanisation_classification_‐_2011_revision#Revision_of_the_degree_of_urbanisation
- 17. IWEPS . Degré de densité de la population des communes belges (méthode DG REGIO). 2019. Available at: https://www.iweps.be/indicateur‐statistique/degre‐de‐densite‐de‐population‐communes‐belges‐methode‐dg‐regio/
- 18. Statbel . Census 2011 ‐ Population by sex according to the km2 grid. 2019. Available at: https://statbel.fgov.be/en/open‐data/census‐2011‐population‐sex‐according‐km2‐grid.
- 19. Statbel . Taxable income. 2019. Available at: https://statbel.fgov.be/en/themes/households/taxable‐income
- 20. Bulsara SM, Wainberg ML, Newton‐John TR. Predictors of adult retention in HIV care: a systematic review. AIDS Behav 2016; 22: 752–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Crawford TN, Sanderson WT, Breheny P, Fleming ST, Thornton A. Impact of non‐HIV related comorbidities on retention in HIV medical care: does retention improve over time? AIDS Behav 2014; 18: 617–24. [DOI] [PubMed] [Google Scholar]
- 22. Rachlis B, Burchell AN, Gardner S et al Social determinants of health and retention in HIV care in a clinical cohort in Ontario, Canada. AIDS Care 2017; 29: 828–37. [DOI] [PubMed] [Google Scholar]
- 23. Ulett KB, Willig JH, Lin HY et al The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS 2009; 23: 41–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Armstrong A, Nagata JM, Vicari M et al A global research agenda for adolescents living with HIV. J Acquir Immune Defic Syndr 2018; 78(Suppl 1): S16–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Diaz A, Ten A, Marcos H et al Factors determining irregular attendance to follow‐up visits among human immunodeficiency virus patients: results of the hospital survey of patients infected with human immunodeficiency virus. Enferm Infecc Microbiol Clin 2015; 33: 324–30. [DOI] [PubMed] [Google Scholar]
- 26. Engelhard EAN, Smit C, Van Sighem A et al Impact of HIV care facility characteristics on the cascade of care in HIV‐infected patients in the Netherlands. AIDS 2016; 30: 301–10. [DOI] [PubMed] [Google Scholar]
- 27. Howarth A, Apea V, Michie S et al REACH: a mixed‐methods study to investigate the measurement, prediction and improvement of retention and engagement in outpatient HIV care. Southampton (UK), NIHR Journals Library, 2017. [PubMed] [Google Scholar]
- 28. Giorgetti R, Tagliabracci A, Schifano F, Zaami S, Marinelli E, Busardo FP. When "Chems" meet sex: a rising phenomenon called "ChemSex". Curr Neuropharmacol 2017; 15: 762–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mugavero MJ, Lin HY, Willig JH et al Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis 2009; 48: 248–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Howarth AR, Burns FM, Apea V et al Development and application of a new measure of engagement in out‐patient HIV care. HIV Med 2017; 18: 267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gueler A, Schoeni‐Affolter F, Moser A et al Neighbourhood socio‐economic position, late presentation and outcomes in people living with HIV in Switzerland. AIDS 2015; 29: 231–8. [DOI] [PubMed] [Google Scholar]
- 32. Holtzman CW, Shea JA, Glanz K et al Mapping patient‐identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen's Behavioral Model. AIDS Care 2015; 27 (7): 817–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yehia BR, Stewart L, Momplaisir F et al Barriers and facilitators to patient retention in HIV care. BMC Infect Dis 2015; 15: 246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dang BN, Westbrook RA, Hartman CM, Giordano TP. Retaining HIV patients in care: the role of initial patient care experiences. AIDS Behav 2016; 20: 2477–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gill VC, Krentz HB. Patient perspectives on leaving, disengaging, and returning to HIV care. AIDS Patient Care STDS 2015; 29: 400–7. [DOI] [PubMed] [Google Scholar]
- 36. Wessinger MH, Hennink MM, Kaiser BN et al Retention in HIV care depends on patients' perceptions of the clinic experience. AIDS Care 2017; 29: 1212–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Enriquez M, Cheng AL, McKinsey D et al Peers keep it real: re‐engaging adults in HIV care. J Int Assoc Provid AIDS Care 2019; 18: 2325958219838858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Horstmann E, Brown J, Islam F, Buck J, Agins BD. Retaining HIV‐infected patients in care: Where are we? Where do we go from here? Clin Infect Dis 2010; 50 (5): 752–61. [DOI] [PubMed] [Google Scholar]
- 39. Portail des services de l'eSanté . 2019. Available at: https://www.ehealth.fgov.be/fr/esante/professionnels‐de‐la‐sante/hubs‐metahub/en‐savoir‐plus.


