Abstract
Patients often experience a functional decline due to physical inactivity during illness. Nurses can influence the physical activity of patients while assisting them with activities of daily living. The purpose of this study was to identify effective interventions that are embedded in daily nursing care (irrespective of care setting) that aim to optimize the functional status of patients by increasing their physical activity. A systematic review was performed and reported following the preferred reporting items for systematic reviews and meta‐analyses. PubMed, CINAHL, and Cochrane were searched for studies from January 2002 to March 2019. The critical appraisal tools from the Joanna Briggs Institute were used to assess the risk of bias in individual studies. Study characteristics, intervention key components, and reported effects of included studies were extracted, summarized narratively, and compared. Twenty studies, evaluating nine different interventions were included. In these interventions, eight key components were identified. Four components were included in all six interventions with a positive effect on mobility, physical activity, or functional status. These components were: assessment of patient's functionality; goal setting with the patient; establishment of an individualized plan; and engagement of patients in physical and daily activity. The effects were limited due to the risk of bias in the studies, small sample sizes, limited clinical meaning of the effects, and variability of the adherence to the interventions. Multicomponent interventions were the most promising to enhance the functional status of patients. Future research should evaluate these interventions using research methods aiming at producing more rigorous evidence.
Keywords: activities of daily living, functional status, nursing interventions, physical activity, systematic review
1. INTRODUCTION
Patients often experience a functional decline due to normal aging and diseases (Hoogendijk et al., 2016; Li et al., 2020). Functional decline is defined as a loss of independence in performing activities of daily living (ADLs) such as bathing, toileting, and mobility, and leads to decreased quality of life, increased risk for further functional decline, and a growing need of care (Mlinac & Feng, 2016). Consequently, health care utilization and costs increase (He, Goodkind, & Kowal, 2016; Tappenden, Campbell, Rawdin, Wong, & Kalita, 2012).
To be able to perform ADLs independently for as long as possible is one of the most important health outcomes for all individuals with chronic illness or disability (Ayton et al., 2018; Karppinen, Laakkonen, Strandberg, Huohvanainen, & Pitkala, 2016). Performing ADL independently enables patients to live as independently as possible and to participate in society. Apart from normal aging and chronic diseases, patients also show a functional decline after hospitalization (Basic, Ní Chróinín, Conforti, & Shanley, 2017; Parry & Puthucheary, 2015). This decline is often due to physical inactivity, as during a hospital stay, patients are mostly inactive and bed‐bound (Fazio et al., 2019; Fini, Holland, Keating, Simek, & Bernhardt, 2017; Floegel et al., 2018). Likewise, in elderly and chronically ill people living in the community and in long‐term care, inactivity is an important risk factor for the functional decline (den Ouden et al., 2015; Legge, Blanchard, & Hanly, 2017; van der Vorst et al., 2016).
Physical activity during illness and early activity as soon as possible after hospital admission have a positive effect on maintaining and restoring patients' functional status (Brown et al., 2016; Grazioli et al., 2019; van der Vorst et al., 2016). The purpose of nursing care is to put or keep patients in the best condition and thus to enhance their recovery and maintenance of physical activity (Englebright, Aldrich, & Taylor, 2014; Kirkevold, 1997; Kitson, Marshall, Bassett, & Zeitz, 2013). In their daily nursing care, nurses are often involved in assisting patients with their ADLs, which is one of the essential nursing care activities (Kitson, Conroy, Wengstrom, Profetto‐McGrath, & Robertson‐Malt, 2010; Zwakhalen et al., 2018). However, despite its broad application, essential nursing care is informed poorly by evidence (Zwakhalen et al., 2018). For a better understanding, in this review, we used the term “daily nursing care” to refer to the nursing care that is focused on assisting patients with their ADLs.
In the past, several studies of daily nursing care interventions were evaluated on their effectiveness on physical activity and functional status (Brown et al., 2016; Krist, Dimeo, & Keil, 2013). However, these interventions often lacked a clear vision of the role of the nursing staff or did not seem to fit with daily nursing care. Additionally, in prior systematic reviews on a similar topic the focus was only on geriatric (Bakker, Robben, & Olde Rikkert, 2011) or stroke patients (Fletcher‐Smith, Walker, Cobley, Steultjens, & Sackley, 2013), just one setting (Crocker et al., 2013), or interventions were included that were not related to daily nursing care (Pollock et al., 2014). Therefore, the objective of this review was to determine the effects of interventions that can be embedded in daily nursing care, irrespective of the care setting, that aim to optimize the functional status of patients by increasing physical activity.
2. METHODS
This systematic review was conducted following the method described by the Preferred Reporting Items for Systematic review and Meta‐Analysis (PRISMA) protocols 2015 guideline (Moher et al., 2015; Shamseer et al., 2015). We used the critical appraisal tools from the Joanna Briggs Institute (JBI) Manual to assess the risk of bias in individual studies (Joanna Briggs Institute [JBI], 2014). The PRISMA statement was used for reporting the review (Liberati et al., 2009; Moher, Liberati, Tetzlaff, & Altman, 2009).
2.1. Search strategy
The electronic databases PubMed (Medline), CINAHL, and the Cochrane Library (CDSR and CENTRAL) were searched to identify relevant studies published between January 2002 and March 2019. Healthcare has been changed in the last decades and as a result, nursing care also showed a continuous development; for instance, it became more complex (Zwakhalen et al., 2018). Therefore, we chose to set a period for the search that was wide enough to include the intervention studies relevant for the current nursing care, and at the same time, narrow enough to prevent the inclusion of the irrelevant ones. Further limits were applied for language (English and Dutch), and the availability of the full text of articles. The search strategy was defined by the first author and finalized after discussion with two other authors. The electronic search and all keywords are described in Table 1. Here we present some examples of the keywords: (a) Population, using keywords like “patients” OR “clients” OR “residents”; (b) Intervention, using keywords such as “nursing care” AND “therapy” OR “rehabilitation” NOT “medical”; (c) Outcome, using keywords like “functional activity” OR “functional status” OR “functional impairment” OR “self‐care” OR “mobility.” The keyword “self‐care” was added as a synonym of ADL (Mlinac & Feng, 2016). The keyword “mobility” was added to prevent missing relevant studies that do not include mobility as part of ADL (Choi, Song, & Chun, 2017).
Table 1.
Keywords and search strategy
| Keywordsa | |
|---|---|
| Population | Patientsb or patients or clients or residents or care receivers or usersc |
| Intervention | [nursingb or nursing careb or nursing processb or nursing approach or nursing program or nurse or caregiverb or nursing programmec] and [treatment or therapy or intervention or management or reablement or restorative or rehabilitationb or care approach] not [pharmaceutical, medical] |
| Outcome | functional activity or functional activitiesc or functional status or functional capacity or functional recovery or functional performance or functional autonomy or functional movement or functional decline or functional disability or functional impairment or functional incapacity or functional capacityc or functional inability or functional abilityc or activities of daily livingb or ADL activities or ADL status or ADL functioning or ADL performance or daily activities or daily functioning or ADL or self‐careb or mobility or ambulation or walkingc or mobilizationc |
Abbreviation: MeSH, Medical Subject Headings.
Keywords were searched in title and/or abstracts (PubMed); in abstract (CINAHL); and in title, abstract, or keywords (Cochrane) by combining Population AND Intervention AND Outcome. Truncation was not used to prevent exploding of results; in Cochrane word variations have been searched.
Keywords which were MeSH terms in PubMed.
Additional keywords for CINAHL.
2.2. Eligibility criteria
Participants: adult patients (>18 years) within any care setting. We excluded studies that focused on patients in the end stage of their disease or life, where the main emphasis was on the quality of life instead of optimizing patients' functional status.
Interventions: the intervention had to focus on ADLs and had to be (potentially) embedded in the nursing care of the individual patient who was in need of assistance with these daily tasks. Therefore, group exercises or video‐based interventions were excluded, as they do not fit daily nursing care.
Outcome measures: measures focusing on maintaining or restoring functional status of patients, defined as the level of independency in ADLs, such as bathing, toileting, and mobility (Mlinac & Feng, 2016). Physical activity as an outcome was included as well due to its positive effect on functional status. We excluded studies aiming at outcomes such as muscle strength, balance, or bone density, as these outcomes are at the level of body function itself instead of at the level of functioning of the person in day‐to‐day life (World Health Organization, 2001).
Studies: randomized experimental studies, quasi‐ and nonrandomized studies. We included different types of experimental studies because daily nursing care interventions are not often studied with a robust design. Systematic reviews were not included in the review, but used for snowball sampling, that is, individual studies from the systematic reviews were screened to select the studies that met our inclusion criteria. Meta‐analyses were only included as such if the inclusion criteria that were applied in the meta‐analysis were identical to those we applied for the study included in our review. Otherwise, the procedure used for systematic reviews was followed.
2.3. Selection process and assessing the risk of bias
After removing duplicates, one reviewer undertook the initial screening of titles. To enhance objectivity, a second author checked a random sample of these titles. Then, the abstracts of the remaining papers were independently reviewed for relevance by two authors. Disagreements were resolved by discussion, and if no consensus was reached, a third author was consulted. The same strategy was followed in assessing the full‐text papers and the risk of bias in the individual studies.
The critical appraisal tools from the Joanna Briggs Reviewers Manual 2014 for (pseudo) randomized studies, for comparable cohort/case–control studies and descriptive/case series studies were used (JBI, 2014). The tools consist of different quality criteria, and a total methodological quality score was assigned to each study by calculating the proportion of the criteria that the study achieved (Table S1). The cut‐off for the inclusion of a study was made in advance as advised in the JBI Manual (JBI, 2014). Knowing that the evidence for basic nursing care is sparse (Zwakhalen et al., 2018), we tried to find a reasonable balance between finding sufficient intervention studies with a less optimal score and finding almost no intervention studies with low risk of bias. Therefore, we determined that studies scoring less than 40% had a too high risk of bias, and these were excluded from this review.
2.4. Data extraction and synthesis
To present an overview of the papers that were included, the following characteristics of the studies were extracted: first author, country where the study was performed, year of publication, intervention type, study design, participants (age, condition, number of participants in both the intervention group and the control group), care setting and measurement time points, outcome measures, and results (difference in means). Data extraction was performed independently by two authors and differences were resolved by discussion.
The included studies varied on most characteristics (see Table S2). Given this variation, the findings are described narratively. Furthermore, the interventions were studied in detail to reveal the key components as described by the authors. The key components, that is, the working mechanisms, are important to define to understand the effect of a complex intervention on a certain outcome (Craig et al., 2008). This was done independently by two authors. Then, two authors discussed and compared all components from the studies to identify the shared key components.
3. RESULTS
Figure 1 outlines the selection process and provides reasons for exclusion. The search in the electronic databases generated 4,657 papers and after removing duplicates (n = 783), screening on title and abstract, 69 individual studies, nine systematic reviews, and four meta‐analyses remained. The inclusion criteria that were applied in the meta‐analyses were different than the criteria we had used for the inclusion of studies in our review. Therefore, the meta‐analyses were not included as such, but we used them for snowball sampling, similar to the systematic reviews. Thus, the individual studies from the meta‐analyses and systematic reviews were assessed for inclusion. After removing duplicates and those published before 2002, the systematic reviews identified 153, and the meta‐analyses 39 individual studies. Out of a total of 261 studies, 237 did not meet our inclusion criteria, resulting in a selection of 24 studies.
Figure 1.
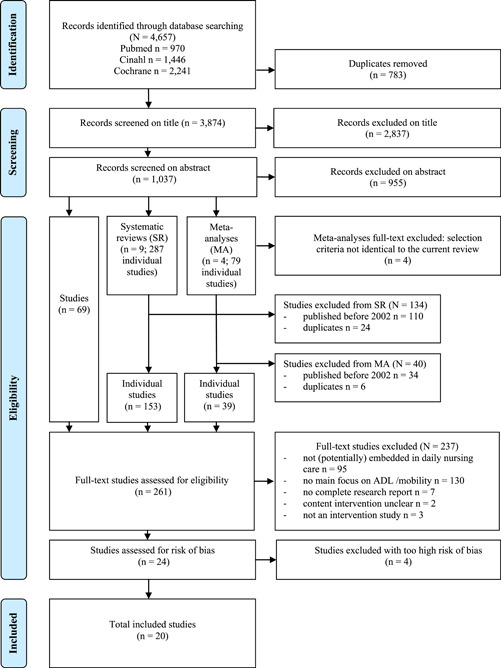
PRISMA flow diagram. ADL, activities of daily living; PRISMA, Preferred Reporting Items for Systematic review and Meta‐Analysis [Color figure can be viewed at wileyonlinelibrary.com]
The risk of methodological bias in the 24 included studies varied. See Table S1. Thirteen studies had a total quality score between 60% and 86% (Galik et al., 2008; Guidetti & Ytterberg, 2011; Hafsteinsdóttir, Algra, Kappelle, & Grypdonck, 2005; Hedman, Eriksson, von Koch, & Guidetti, 2019; Henskens, Nauta, Drost, & Scherder, 2018; Henskens, Nauta, Scherder, Oosterveld, & Vrijkotte, 2017; Henskens, Nauta, van Eekeren, & Scherder, 2018; Kerse et al., 2008; Parsons, Sheridan, Rouse, Robinson, & Connolly, 2013; Peri et al., 2008; Resnick et al., 2006; Resnick, Galik, Gruber‐Baldini, & Zimmerman, 2009; Tuntland, Aaslund, Espehaug, Førland, & Kjeken, 2015), and seven studies had a quality score between 40% and 59% (Bertilsson et al., 2014; Galik, Resnick, Hammersla, & Brightwater, 2013; Galik, Resnick, Lerner, Hammersla, & Gruber‐Baldini, 2015; Resnick, Gruber‐Baldini, et al., 2009; Resnick, Galik, Gruber‐Baldini, & Zimmerman, 2011; Sidani, Streiner, & LeClerc, 2012; Tinetti et al., 2002). Four studies fulfilled less than 40% of the quality criteria and were excluded from the review (Engelman, Mathews, & Altus, 2002; Johnson et al., 2004; Lim, 2003; Padula, Hughes, & Baumhover, 2009).
3.1. Study characteristics
All study characteristics are provided in Table S2. Different study designs were used. In most studies (60%), a (pseudo) randomized design was used. Of these 12 experimental studies, 10 were multicenter cluster trials, including 3 (Guidetti & Ytterberg, 2011) to 41 clusters in the study of Kerse et al. (2008). This was followed by observational (n = 4) and descriptive studies (n = 4).
A total of 4,551 participants participated in the 20 included studies. Sample sizes varied from 14 (Resnick, Galik, et al., 2009) to 1,382 participants in the study of Tinetti et al. (2002). The majority of studies (65%) were performed in long‐term care settings such as nursing homes and assisted living facilities. This was followed by rehabilitation centers (15%) and home care settings (15%). Only one study was performed in a hospital (Hafsteinsdóttiret al., 2005). The study participants suffered from a stroke or were included based on (higher) age. Participants in all studies were, on average, 66 years, and older. In 13 studies performed in long‐term settings, the participants were on average older than 80 years. In four studies the investigators only included patients with normal cognition, whereas in seven studies, the investigators specifically focused on patients with dementia.
The outcomes: functional status, mobility, and physical activity were evaluated in the studies. Functional status was measured in the majority of studies (90%), mostly (10 out of the 18 studies) with the Barthel Index (BI) on a score scale ranging from 0 to 100. Mobility outcome was measured in nine studies with five different measurements. Physical activity of the participants was measured in an objective way using an accelerometer (the ActiGraph) and in a subjective way using the physical activity survey for long‐term care. See Table S2 for all measurements used.
3.2. Intervention characteristics
Nine different interventions were identified through this review (Table S2). Four interventions were evaluated in more than one study. For instance, a function‐focused care (FFC) intervention was explored in seven studies. A summarized description of the interventions and the staff involved can be found in Table S3.
A comparison of the interventions identified eight key components as presented in Table 2. All nine interventions consist of more than one key component. This varied from two in the neurodevelopment treatment intervention to seven components in the FFC, reablement, and restorative care interventions. Interventions with five or more key components showed a positive effect on at least one of the three outcomes of interest: mobility, physical activity, or functional status (Galik et al., 2013; Henskens, Nauta, van Eekeren, et al., 2018; Parsons et al., 2013; Peri et al., 2008; Resnick, Galik, et al., 2009; Resnick, Gruber‐Baldini, et al., 2009; Tinetti et al., 2002; Tuntland et al., 2015). The FFC intervention revealed an effect on all three outcomes (Galik et al., 2013; Resnick, Galik, et al., 2009; Resnick, Gruber‐Baldini, et al., 2009). The effective interventions had the following key components in common: assessment of patient's functionality, goal setting with the patient, establishment of an individualized plan, and engagement of patients in physical activity/ADLs (Table 2).
Table 2.
Key components and effects of the interventions
| Key component | Positive effect is found in (one of them) included studies on the outcome | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Assessment of patient's functionality | Goal‐setting together with the patient | Establishment of an individualized plan for the patient | Engagement of patients in physical/ADLs | Assessment/adapta tion of environment | Training of all staff | Ongoing motivation and support of staff | Multidisciplinary approach | |||
| Mo | PA | FS | |||||||||
| Abilities‐focused care (Sidani et al., 2012) | ✓ | ✓ | ✓ | n/a | n/a | – | |||||
| ADL goal‐setting tool (Parsons et al., 2013) | ✓ | ✓ | ✓ | ✓ | ✓ | + | n/a | n/a | |||
| ADL training (Henskens et al. 2017; Henskens, Nauta, Drost, et al, 2018; Henskens, Nauta, van Eekeren, et al., 2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | + | n/a | – | ||
| Client‐centered ADL (Bertilsson et al., 2014; Guidetti and Ytterberg, 2011; Hedman et al., 2019) | ✓ | ✓ | ✓ | ✓ | ✓ | n/a | n/a | – | |||
| Functional activity program (Kerse et al., 2008; Peri et al., 2008) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | n/a | + | ||
| Function‐focused care (Galik et al., 2008, 2013, 2015; Resnick et al., 2006; Resnick, Galik, et al., 2009; Resnick, Gruber‐Baldini, et al., 2009; Resnick et al., 2011) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | + | + | + | |
| Neurodevelopmental treatment (Hafsteinsdóttir et al., 2005) | ✓ | ✓ | n/a | n/a | – | ||||||
| Reablement (Tuntland et al., 2015) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | n/a | + | |
| Restorative care (Tinetti et al., 2002) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | + | n/a | – | |
Note: “+”, positive significant effect was found; “–”, no significant effect was found.
Abbreviations: ADL, activity of daily living; FS, functional status outcome; Mo, mobility outcome; n/a, not applicable; PA, physical activity outcome.
3.3. Effectiveness of interventions
In the following section, we describe the effectiveness of the interventions according to the outcome measures of our interest. Earlier, we defined functional status as the ADLs, including mobility. However, mobility was also evaluated separately in several studies and therefore, we also describe mobility as a separate outcome. The measurements used and the effects of the interventions (difference in means over time per group) are presented in Table S2.
3.4. Outcome—Functional status
In 5 of the 18 studies, a statistically significant improvement in functional status was found in the intervention group when compared to the control group. In these studies, the FFC intervention (Galik et al., 2013; Resnick, Galik, et al., 2009; Resnick, Gruber‐Baldini, et al., 2009), the functional activity program (Peri et al., 2008), and reablement (Tuntland et al., 2015) were evaluated. The effects of FFC and the functional activity program did not last throughout the 6‐month follow‐up period in the studies of Galik et al. (2013) or Peri et al. (2008). Resnick, Gruber‐Baldini, et al. (2009) only found improvements in the FFC intervention group on some subscales of the BI measurement. In another FFC study, no improvement was found in the functional status of the patients; however, a decline in the intervention group was less than in the control group (Resnick et al., 2011). Additionally, in the functional activity program study of Kerse et al. (2008), residents with normal cognition in the intervention group showed less deterioration in functional status compared to those in the control group (Kerse et al., 2008).
3.5. Outcome—Mobility
Statistically significant findings in favor of the intervention group were found in four studies evaluating: restorative care (Tinetti et al., 2002), ADL training (Henskens, Nauta, van Eekeren, et al., 2018), ADL goal‐setting tool (Parsons et al., 2013), and FFC (Resnick, Gruber‐Baldini, et al., 2009). Resnick, Gruber‐Baldini, et al. (2009) found better overall mobility in the FFC group only at 4 months and a lower decline in gait in the FFC group at 12 months. Also, the mobility improvement in the ADL training intervention group was only found at 3 months (Henskens, Nauta, van Eekeren, et al., 2018).
3.6. Outcome—Physical activity
FFC increased the physical activity of participants, both objectively and subjectively in the study of Galik et al. (2013). In a study of Resnick, Galik, et al. (2009), by using the subjective measurement, an increase in time spent in physical activity was found based on the resident report as well as the nurse assistant report. A significant decrease in physical activity from preintervention time points to 4 months postintervention measured by the Actigraph, was found in the FFC study by Galik et al. (2008). In another study of Galik et al. (2015), a significant increase in time spent on physical activity was found in the control group, whereas the FFC group decreased in physical activity. In the study, only the subscale “repetitive behavior” of the physical activity survey for long‐term care showed a significant difference (Galik et al., 2015).
4. DISCUSSION
We included 20 studies evaluating nine interventions that are focused on optimizing the functional status of patients in different care settings and that are applicable during daily nursing care. Eight intervention key components were identified. Multicomponent interventions (five or more) showed a positive effect on mobility, physical activity, and/or functional status. Of these, only the FFC intervention showed a positive effect on all of these three outcomes. An assessment of the patient's functionality, goal setting with the patient, establishment of an individualized plan for the patient, and engagement of patients in physical activity/ADLs were the shared key components in the interventions with positive effect.
All of the identified interventions focus on engaging patients in physical and daily activities (key component 4). This finding is congruent with an earlier review regarding post stroke rehabilitation in which the authors concluded that encouraging the patients' self‐care will lead to improvements in functional outcomes (Rensink, Schuurmans, Lindeman, & Hafsteinsdóttir, 2009). Goal setting with the patient as a key component is included in seven interventions aiming to improve the patient's self‐efficacy and motivation to optimally engage them in functional tasks and physical activities (Bertilsson et al., 2014; Galik et al., 2008, 2013, 2015; Guidetti & Ytterberg, 2011; Henskens, et al., 2017; Henskens, Nauta, Drost, et al., 2018; Henskens, Nauta, van Eekeren, et al., 2018; Kerse et al., 2008; Parsons et al., 2013; Peri et al., 2008; Resnick et al., 2006; Resnick, Galik, et al., 2009; Resnick, Gruber‐Baldini, et al., 2009; Resnick et al., 2011; Tinetti et al., 2002; Tuntland et al., 2015). This is in line with the findings of a review assessing the effects of goal setting (Levack et al., 2016). The authors concluded that goal setting in adults can result in higher levels of motivation and self‐efficacy; however, this evidence was not conclusive due to methodological issues, and they proposed further research (Levack et al., 2016). We are also unable to draw conclusions about the effects of a single component like goal setting on patient outcomes. However, the components: assessment of patient's functionality, goal setting with the patient, establishment of an individualized plan for the patient, and engagement of patients in physical activity/ADLs, are included in all six effective interventions. This suggests that these components can be considered as working mechanisms of these interventions. In all interventions that include establishment of an individualized plan (key component 3), the plan is based on an assessment of patient's functionality (key component 1) in close collaboration with the patient or family. The same goes for setting goals with the patient. Only abilities‐focused care intervention does not include patient‐participation explicitly.
The interventions: ADL training, FFC, functional activity program, ADL goal‐setting tool, reablement, and restorative care all have a clear role for nursing staff and showed statistically significant effects in one or more patient outcomes of interest. However, there are some considerations relevant to the interpretation of these findings. As mentioned before, the quality scores in the studies varied between 40% and 86%. This variation was also present in the studies that reported a significant positive effect on patient outcomes (Galik et al., 2013; Henskens, Nauta, van Eekeren, et al., 2018; Parsons et al., 2013; Peri et al., 2008; Resnick, Galik, et al., 2009; Resnick, Gruber‐Baldini, et al., 2009; Tinetti et al., 2002; Tuntland et al., 2015). Because a risk of bias might influence the results (JBI, 2014; Liberati et al., 2009), this should be taken into account when interpreting the results. The paucity of robust results is in line with another systematic review focusing on the effectiveness of nursing interventions regarding fundamental nursing care activities (Richards, Hilli, Pentecost, Goodwin, & Frost, 2018).
In addition, a statistically significant effect, as expressed by the p value, does not equal a clinically relevant effect (Liberati et al., 2009; Sullivan & Feinn, 2012). For instance, in the FFC study of Galik et al. (2013), the BI showed an increase of 9.6 points in the intervention group compared to 8.7 points in the control group (p = .01). On a BI scale, which ranges from 0 (dependence) to 100 (independence), one can question whether a difference of 0.9 points is clinically relevant. On the other hand, as this study included mainly persons with an average age of over 66 years, from the perspective of an older person with a high risk of functional decline, small gains in functional status may be beneficial for the quality of life.
Twelve studies did not show positive effects on patient outcomes (Bertilsson et al., 2014; Galik et al., 2008, 2015; Guidetti & Ytterberg, 2011; Hafsteinsdóttir et al., 2005; Hedman et al., 2019; Henskens et al., 2017; Henskens, Nauta, Drost, et al., 2018; Kerse et al., 2008; Resnick et al., 2006, 2011; Sidani et al., 2012). In six of these studies, a cluster randomized controlled trial was used (Bertilsson et al., 2014; Galik et al., 2015; Guidetti & Ytterberg, 2011; Henskens, Nauta, Drost, et al., 2018; Kerse et al., 2008; Resnick et al., 2011). Although clustering is often used for practical reasons, an important disadvantage is the need for a larger sample size to achieve the same power due to the similarities among subjects in the clusters (Killip, Mahfoud, & Pearce, 2004; Sullivan & Feinn, 2012). However, in only one study, the researchers stated that they had adjusted for a cluster effect and how the sample size was calculated (Kerse et al., 2008). Therefore, an insufficient sample size could be a reason for not detecting an effect in some studies. Adherence of professionals to the interventions might be another reason why effects on patient outcomes were not detected. In four studies, the investigators described some variability in adherence with the intervention or questioned the extent to which nursing staff delivered the intervention (Guidetti & Ytterberg, 2011; Kerse et al., 2008; Resnick et al., 2006; Sidani et al., 2012).
4.1. Strengths and limitations
The strength of this review is its focus on interventions regarding the ADLs of individual patients applicable to daily nursing care practice. Therefore, the findings of this review will most likely provide nurses with some beneficial interventions for patients who are in need of assistance with these daily tasks. Another strength of this review is the rigorous evaluation of the studies by two independent investigators using the critical appraisal forms of the JBI, which is a well‐established international research and development center. These critical appraisal forms are especially developed for different study designs. Consequently, they take into account the features, advantages, and limitations of each study design (JBI, 2014).
This review has limitations that need to be considered as well. Although we included physical activity as an outcome, the term “physical” was removed from the keywords in the search strategy. This term mainly led to studies focusing on outcomes at the level of body function, such as balance and strength of arm muscles, whereas we were searching explicitly for interventions that focused on outcomes at the level of functioning of persons in day‐to‐day life. Additionally, truncation was not used to prevent the exploding of results. Nevertheless, the search strategy resulted in a high number of studies. Most of the studies described interventions that seem not (easy) to embed in daily nursing care, such as planned training sessions that are provided by physiotherapists or occupational therapists. These interventions, as described in a study where hospitalized patients were assisted with ambulation up to twice daily (Brown et al., 2016), are often shown to be effective, but these time‐consuming activities might also be difficult to integrate into the daily nursing care practice. Another limitation is that the title selection was carried out by one person, although in the event that the title met the minimum requirement for the stated criteria, the study was included in the review. The use of at least two investigators for the title selection may reduce the possibility of rejecting relevant reports (Liberati et al., 2009). As a consequence, we may have missed some relevant interventions. The subsequent steps of the selection process for relevant papers were performed independently by at least two researchers. A final limitation we want to address is linked to the generalizability of our review. All of the significant effects were found in the long‐term or home care setting. This may affect the generalizability to acute care settings.
5. CONCLUSIONS
Through this review, we found nine different interventions that are embedded in daily nursing care with the aim to optimize the functional status of patients within any care setting. Accounting for the risk of bias, the inconsistency of some findings, the limited clinical relevance of the significant effects, and the variability of the adherence to the interventions, some promising results were found. Six multicomponent interventions showed a positive effect on functional status, mobility, or physical activity. These were a functional activity program, an ADL training intervention, an ADL goal‐setting tool intervention, restorative care, reablement, and FFC. The key components included in these interventions were assessment of patient's functionality, goal setting with the patient, establishment of an individualized plan for the patient, and engagement of patients in physical activity/ADLs.
Future research should evaluate multicomponent interventions using research methods that are aimed at producing more rigorous evidence for nursing interventions. Additional future research could be a meta‐analysis or even network meta‐analysis to compare and explain the variation of intervention effects utilizing the study and intervention characteristics. In daily practice, nurses should support their patients in maintaining the highest possible level of physical activity in daily life. This will enable them to optimize patients' functional status and achieve one of the core purposes of nursing.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Study concept and design: C. C. J. M. M. V., S. F. M., M. J. S., and J. M. M.‐G. Acquisition of data: C. C. J. M. M. V., S. F. M., and J. M. M.‐G. Analysis and interpretation of data: C. C. J. M. M. V., S. F. M., L. S., M. J. S., and J. M. M.‐G. Drafting of the manuscript: C. C. J. M. M. V., S. F. M., L. S., M. J. S., and J. M. M.‐G. Critical revision of the manuscript for important intellectual content: C. C. J. M. M. V., S. F. M., L. S., M. J. S., and J. M. M.‐G. Final approval of the version to be published: C. C. J. M. M. V., S. F. M., L. S., M. J. S., and J. M. M.‐G. Agreement to be accountable for all aspects of the work: C. C. J. M. M. V., S. F. M., L. S., M. J. S., and J. M. M.‐G.
Supporting information
Supporting information
Supporting information
Supporting information
ACKNOWLEDGMENT
This study was funded by The Netherlands Organization for Health Research and Development (ZonMw) (Grant # 80‐80705‐98‐025).
Verstraten CCJMM, Metzelthin SF, Schoonhoven L, Schuurmans MJ, de Man‐van Ginkel JM. Optimizing patients' functional status during daily nursing care interventions: A systematic review. Res Nurs Health. 2020;43:478–488. 10.1002/nur.22063
REFERENCES
- Ayton, D. R. , Barker, A. L. , Peeters, G. M. E. E. , Berkovic, D. E. , Lefkovits, J. , Brennan, A. , … McNeil, J. , et al. (2018). Exploring patient‐reported outcomes following percutaneous coronary intervention: A qualitative study. Health Expectations, 21(2), 457–465. 10.1111/hex.12636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker, F. C. , Robben, S. H. M. , & Olde Rikkert, M. G. M. (2011). Effects of hospital‐wide interventions to improve care for frail older inpatients: A systematic review. BMJ Quality & Safety, 20(8), 680–691. 10.1136/bmjqs.2010.047183 [DOI] [PubMed] [Google Scholar]
- Basic, D. , Ní Chróinín, D. , Conforti, D. , & Shanley, C. (2017). Predictors on admission of functional decline among older patients hospitalised for acute care: A prospective observational study. Australasian Journal on Ageing, 36(4), E57–E63. 10.1111/ajag.12458 [DOI] [PubMed] [Google Scholar]
- Bertilsson, A. S. , Ranner, M. , Koch, L. , Eriksson, G. , Johansson, U. , Ytterberg, C. , … Tham, K. (2014). A client‐centred ADL intervention: Three‐month follow‐up of a randomized controlled trial. Scandinavian Journal of Occupational Therapy, 21(5), 377–391. 10.3109/11038128.2014.880126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, C. J. , Foley, K. T. , Lowman, J. D. , MacLennan, P. A. , Razjouyan, J. , Najafi, B. , … Allman, R. M. (2016). Comparison of posthospitalization function and community mobility in hospital mobility program and usual care patients: A randomized clinical trial. JAMA Internal Medicine, 176(7), 921–927. 10.1001/jamainternmed.2016.1870 [DOI] [PubMed] [Google Scholar]
- Choi, Y. , Song, C. , & Chun, B. (2017). Activities of daily living and manual hand dexterity in persons with idiopathic Parkinson disease. Journal of Physical Therapy Science, 29(3), 457–460. 10.1589/jpts.29.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig, P. , Dieppe, P. , Macintyre, S. , Michie, S. , Nazareth, I. , & Petticrew, M. (2008). Developing and evaluating complex interventions: The new medical research council guidance. BMJ (Clinical Research Ed.), 337, a1655 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crocker, T. , Forster, A. , Young, J. , Brown, L. , Ozer, S. , Smith, J. , … Greenwood Darren, C. (2013). Physical rehabilitation for older people in long‐term care (Review). Cochrane Database of Systematic Reviews, Issue 2, CD004294 10.1002/14651858.CD004294.pub3 [DOI] [PubMed] [Google Scholar]
- den Ouden, M. , Bleijlevens, M. H. C. , Meijers, J. M. M. , Zwakhalen, S. M. G. , Braun, S. M. , Tan, F. E. S. , & Hamers, J. P. H. (2015). Daily (in)activities of nursing home residents in their wards: An observation study. Journal of the American Medical Directors Association, 16(11), 963–968. [DOI] [PubMed] [Google Scholar]
- Engelman, K. K. , Mathews, R. M. , & Altus, D. E. (2002). Restoring dressing independence in persons with alzheimer's disease: A pilot study. American Journal of Alzheimer's Disease and Other Dementias, 17(1), 37–43. 10.1177/153331750201700102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englebright, J. , Aldrich, K. , & Taylor, C. R. (2014). Defining and incorporating basic nursing care actions into the electronic health record. Journal of Nursing Scholarship, 46(1), 50–57. 10.1111/jnu.12057 [DOI] [PubMed] [Google Scholar]
- Fazio, S. , Stocking, J. , Kuhn, B. , Doroy, A. , Blackmon, E. , Young, H. , & Adams, J. (2019). How much do hospitalized adults move? A systematic review and meta‐analysis. Applied Nursing Research, 51, 151189 10.1016/j.apnr.2019.151189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fini, N. , Holland, A. , Keating, J. , Simek, J. , & Bernhardt, J. (2017). How physically active are people following stroke? Systematic review and quantitative synthesis. Physical Therapy, 97(7), 707–717. 10.1093/ptj/pzx038 [DOI] [PubMed] [Google Scholar]
- Fletcher‐Smith, J. C. , Walker, M. F. , Cobley, C. S. , Steultjens, E. M. J. , & Sackley, C. M. (2013). Occupational therapy for care home residents with stroke (Review). Cochrane Database of Systematic Reviews, Issue 6, CD010116 10.1002/14651858.CD010116.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floegel, T. , Dickinson, J. , DerAnanian, C. , McCarthy, M. , Hooker, S. , & Buman, M. (2018). Association of posture and ambulation with function 30 days after hospital discharge in older adults with heart failure. Journal of Cardiac Failure, 24(2), 126–130. 10.1016/j.cardfail.2018.01.001 [DOI] [PubMed] [Google Scholar]
- Galik, E. , Resnick, B. , Gruber Baldini, A. , Nahm, E. , Pearson, K. , & Pretzer Aboff, I. (2008). Pilot testing of the restorative care intervention for the cognitively impaired. Journal of the American Medical Directors Association, 9(7), 516–522. 10.1016/j.jamda.2008.04.013 [DOI] [PubMed] [Google Scholar]
- Galik, E. , Resnick, B. , Hammersla, M. , & Brightwater, J. (2013). Optimizing function and physical activity among nursing home residents with dementia: Testing the impact of function‐focused care. The Gerontologist, 54(6), 930–943. 10.1093/geront/gnt108 [DOI] [PubMed] [Google Scholar]
- Galik, E. , Resnick, B. , Lerner, N. , Hammersla, M. , & Gruber‐Baldini, A. L. (2015). Function focused care for assisted living residents with dementia. The Gerontologist, 55(Suppl. 1), S13–S26. 10.1093/geront/gnu173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grazioli, E. , Tranchita, E. , Borriello, G. , Cerulli, C. , Minganti, C. , & Parisi, A. (2019). The effects of concurrent resistance and aerobic exercise training on functional status in patients with multiple sclerosis. Current Sports Medicine Reports, 18(12), 452–457. 10.1249/JSR.0000000000000661 [DOI] [PubMed] [Google Scholar]
- Guidetti, S. , & Ytterberg, C. (2011). A randomised controlled trial of a client‐centred self‐care intervention after stroke: A longitudinal pilot study. Disability and Rehabilitation, 33(6), 494–503. 10.3109/09638288.2010.498553 [DOI] [PubMed] [Google Scholar]
- Hafsteinsdóttir, T. B. , Algra, A. , Kappelle, L. J. , & Grypdonck, M. H. F. (2005). Neurodevelopmental treatment after stroke: A comparative study. Journal of Neurology, Neurosurgery and Psychiatry, 76(6), 788–792. 10.1136/jnnp.2004.042267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, W. , Goodkind, D. , & Kowal, P. (2016). An aging world: 2015, U.S. Census Bureau (U.S. Census Bureau, International Population Reports, P95/16‐1). Washington, DC: U.S. Government Publishing Office; Retrieved from https://www.census.gov/content/dam/Census/library/publications/2016/demo/p95-16-1.pdf [Google Scholar]
- Hedman, A. , Eriksson, G. , von Koch, L. , & Guidetti, S. (2019). Five‐year follow‐up of a cluster‐randomized controlled trial of a client‐centred activities of daily living intervention for people with stroke. Clinical Rehabilitation, 33(2), 262–276. 10.1177/0269215518809791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henskens, M. , Nauta, I. M. , Drost, K. T. , & Scherder, E. J. (2018). The effects of movement stimulation on activities of daily living performance and quality of life in nursing home residents with dementia: A randomized controlled trial. Clinical Interventions in Aging, 13, 805–817. 10.2147/CIA.S160031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henskens, M. , Nauta, I. M. , Scherder, E. J. A. , Oosterveld, F. G. J. , & Vrijkotte, S. (2017). Implementation and effects of movement‐oriented restorative care in a nursing home—A quasi‐experimental study. BMC Geriatrics, 17(1), 243 10.1186/s12877-017-0642-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henskens, M. , Nauta, I. , van Eekeren, M. A. , & Scherder, E. A. (2018). Effects of physical activity in nursing home residents with dementia: A randomized controlled trial. Dementia & Geriatric Cognitive Disorders, 46(1), 60–80. 10.1159/000491818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoogendijk, E. O. , Deeg, D. J. H. , Poppelaars, J. , van der Horst, M. , Broese van Groenou, M. I. , Comijs, H. C. , … Huisman, M. (2016). The longitudinal aging study Amsterdam: Cohort update 2016 and major findings. European Journal of Epidemiology, 31(9), 927–945. 10.1007/s10654-016-0192-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joanna Briggs Institute (JBI). (2014). Johanna Briggs Institute reviewers’ manual 2014 edition Retrieved from https://joannabriggs.org/assets/docs/jbc/operations/reviewersHandbook/JBI-ReviewersManual-2014.pdf
- Johnson, C. , Myers, A. , Jones, G. , Fitzgerald, C. , Lazowski, D. , Stolee, P. , … Ecclestone, N. (2004). Evaluation of the restorative care education and training program for nursing homes. Canadian Journal on Aging, 24(2), 115–126. 10.1353/cja.2005.0065 [DOI] [PubMed] [Google Scholar]
- Karppinen, H. , Laakkonen, M. , Strandberg, T. E. , Huohvanainen, E. A. , & Pitkala, K. H. (2016). Do you want to live to be 100? Answers from older people. Age and Ageing, 45(4), 543–549. 10.1093/ageing/afw059 [DOI] [PubMed] [Google Scholar]
- Kerse, N. , Peri, K. , Robinson, E. , Wilkinson, T. , Randow, M. , Kiata, L. , … Arroll, B. (2008). Does a functional activity programme improve function, quality of life, and falls for residents in long term care? Cluster randomised controlled trial. BMJ (Clinical Research Ed.), 337, a1445 10.1136/bmj.a1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killip, S. , Mahfoud, Z. , & Pearce, K. (2004). What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. Annals of Family Medicine, 2(3), 204–208. 10.1370/afm.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkevold, M. (1997). The role of nursing in the rehabilitation of acute stroke patients: Toward a unified theoretical perspective. Advances in Nursing Science, 19(4), 55–64. 10.1097/00012272-199706000-00005 [DOI] [PubMed] [Google Scholar]
- Kitson, A. , Conroy, T. , Wengstrom, Y. , Profetto‐McGrath, J. , & Robertson‐Malt, S. (2010). Defining the fundamentals of care. International Journal of Nursing Practice, 16(4), 423–434. 10.1111/j.1440-172X.2010.01861.x [DOI] [PubMed] [Google Scholar]
- Kitson, A. , Marshall, A. , Bassett, K. , & Zeitz, K. (2013). What are the core elements of patient‐centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. Journal of Advanced Nursing, 69(1), 4–15. 10.1111/j.1365-2648.2012.06064.x [DOI] [PubMed] [Google Scholar]
- Krist, L. , Dimeo, F. , & Keil, T. (2013). Can progressive resistance training twice a week improve mobility, muscle strength, and quality of life in very elderly nursing‐home residents with impaired mobility? A pilot study. Clinical Interventions in Aging, 8, 443–448. 10.2147/CIA.S42136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legge, A. , Blanchard, C. , & Hanly, J. (2017). Physical activity and sedentary behavior in patients with systemic lupus erythematosus and rheumatoid arthritis. Open Access Rheumatology, 9, 191–200. 10.2147/OARRR.S148376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levack, W. M. , Weatherall, M. , Hay‐Smith, J. C. , Dean, S. G. , McPherson, K. , & Siegert, R. J. (2016). Goal setting and strategies to enhance goal pursuit in adult rehabilitation: Summary of a cochrane systematic review and meta‐analysis. European Journal of Physical and Rehabilitation Medicine, 52(3), 400–416. [PubMed] [Google Scholar]
- Li, J. , Wang, J. , Wu, B. , Xu, H. , Wu, X. , Zhou, L. , & Deng, B. (2020). Association between early cognitive impairment and midterm functional outcomes among Chinese acute ischemic stroke patients: A longitudinal study. Frontiers in Neurology, 11, 20 10.3389/fneur.2020.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati, A. , Altman, D. G. , Tetzlaff, J. , Mulrow, C. , Gøtzsche, P. C. , Ioannidis, J. P. A. , … Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ (Clinical Research Ed.), 339, b2700 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim, Y. M. (2003). Nursing intervention for grooming of elders with mild cognitive impairments in Korea. Geriatric Nursing, 24(1), 11–15. 10.1067/mgn.2003.9 [DOI] [PubMed] [Google Scholar]
- Mlinac, M. , & Feng, M. (2016). Assessment of activities of daily living, self‐care, and independence. Archives of Clinical Neuropsychology, 31(6), 506–516. 10.1093/arclin/acw049 [DOI] [PubMed] [Google Scholar]
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , … Stewart, L. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Systematic Reviews, 4(1), 1 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. , The PRISMA Group . (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA Statement. PLOS Medicine, 6(7), e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padula, C. , Hughes, C. , & Baumhover, L. (2009). Impact of a nurse‐driven mobility protocol on functional decline in hospitalized older adults. Journal of Nursing Care Quality, 24(4), 325–331. 10.1097/NCQ.0b013e3181a4f79b [DOI] [PubMed] [Google Scholar]
- Parry, S. , & Puthucheary, Z. (2015). The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extreme Physiology & Medicine, 4, 16 10.1186/s13728-015-0036-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons, J. G. M. , Sheridan, N. , Rouse, P. , Robinson, E. , & Connolly, M. (2013). A randomized controlled trial to determine the effect of a model of restorative home care on physical function and social support among older people. Archives of Physical Medicine and Rehabilitation, 94(6), 1015–1022. 10.1016/j.apmr.2013.02.003 [DOI] [PubMed] [Google Scholar]
- Peri, K. , Kerse, N. , Robinson, E. , Parsons, M. , Parsons, J. , & Latham, N. (2008). Does functionally based activity make a difference to health status and mobility? A randomised controlled trial in residential care facilities (the promoting independent living study; PILS). Age and Ageing, 37(1), 57–63. 10.1093/ageing/afm135 [DOI] [PubMed] [Google Scholar]
- Pollock, A. , Baer, G. , Campbell, P. , Choo Pei, L. , Forster, A. , Morris, J. , … Langhorne, P. (2014). Physical rehabilitation approaches for the recovery of function and mobility following stroke. The Cochrane Database of Systematic Reviews, 2014(4), CD001920 10.1002/14651858.CD001920.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rensink, M. , Schuurmans, M. , Lindeman, E. , & Hafsteinsdóttir, T. (2009). Task‐oriented training in rehabilitation after stroke: Systematic review. Journal of Advanced Nursing, 65(4), 737–754. 10.1111/j.1365-2648.2008.04925.x [DOI] [PubMed] [Google Scholar]
- Resnick, B. , Galik, E. , Gruber‐Baldini, A. L. , & Zimmerman, S. (2009). Implementing a restorative care philosophy of care in assisted living: Pilot testing of Res‐Care‐AL. Journal of the American Academy of Nurse Practitioners, 21(2), 123–133. 10.1111/j.1745-7599.2008.00394.x [DOI] [PubMed] [Google Scholar]
- Resnick, B. , Simpson, M. , Bercovitz, A. , Galik, E. , Gruber Baldini, A. , Zimmerman, S. , & Magaziner, J. (2006). Pilot testing of the restorative care intervention: Impact on residents. Journal of Gerontological Nursing, 32(3), 39–47. 10.3928/00989134-20060301-07 [DOI] [PubMed] [Google Scholar]
- Resnick, B. , Galik, E. , Gruber‐Baldini, A. , & Zimmerman, S. (2011). Testing the effect of function‐focused care in assisted living. Journal of the American Geriatrics Society, 59(12), 2233–2240. 10.1111/j.1532-5415.2011.03699.x [DOI] [PubMed] [Google Scholar]
- Resnick, B. , Gruber‐Baldini, A. L. , Zimmerman, S. , Galik, E. , Pretzer‐Aboff, I. , Russ, K. , & Hebel, J. R. (2009). Nursing home resident outcomes from the Res‐Care intervention. Journal of the American Geriatrics Society, 57(7), 1156–1165. 10.1111/j.1532-5415.2009.02327.x [DOI] [PubMed] [Google Scholar]
- Richards, D. A. , Hilli, A. , Pentecost, C. , Goodwin, V. A. , & Frost, J. (2018). Fundamental nursing care: A systematic review of the evidence on the effect of nursing care interventions for nutrition, elimination, mobility and hygiene. Journal of Clinical Nursing, 27(11–12), 2179–2188. 10.1111/jocn.14150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamseer, L. , Moher, D. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , … Stewart, L. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015: Elaboration and explanation. BMJ (Clinical Research Ed.), 350, g7647 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- Sidani, S. , Streiner, D. , & LeClerc, C. (2012). Evaluating the effectiveness of the abilities‐focused approach to morning care of people with dementia. International Journal of Older People Nursing, 7(1), 37–45. 10.1111/j.1748-3743.2011.00273.x [DOI] [PubMed] [Google Scholar]
- Sullivan, G. , & Feinn, R. (2012). Using effect size—Or why the P value is not enough. The Journal of Graduate Medical Education, 4(3), 279–282. 10.4300/JGME-D-12-00156.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tappenden, P. , Campbell, F. , Rawdin, A. , Wong, R. , & Kalita, N. (2012). The clinical effectiveness and cost‐effectiveness of home‐based, nurse‐led health promotion for older people: A systematic review. Health Technology Assessment (Winchester, England), 16(20), 1–72. 10.3310/hta16200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti, M. E. , Baker, D. , Gallo, W. T. , Nanda, A. , Charpentier, P. , & O'Leary, J. (2002). Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. JAMA: Journal of the American Medical Association, 287(16), 2098–2154. 10.1001/jama.287.16.2098 [DOI] [PubMed] [Google Scholar]
- Tuntland, H. , Aaslund, M. , Espehaug, B. , Førland, O. , & Kjeken, I. (2015). Reablement in community‐dwelling older adults: A randomised controlled trial. BMC Geriatrics, 15, 145 10.1186/s12877-015-0142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Vorst, A. , Zijlstra, G. A. R. , Witte, N. D. , Duppen, D. , Stuck, A. E. , Kempen, G. I. J. M. , & Schols, J. M. G. A. (2016). Limitations in activities of daily living in community‐dwelling people aged 75 and over: A systematic literature review of risk and protective factors. PLOS One, 11(10), e0165127 10.1371/journal.pone.0165127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2001). International classification of functioning, disability and health: ICF Geneva, Switzerland. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf
- Zwakhalen, S. M. G. , Hamers, J. P. H. , Metzelthin, S. F. , Ettema, R. , Heinen, M. , De Man‐Van Ginkel, J. M. , … Schuurmans, M. J. (2018). Basic nursing care: The most provided, the least evidence based. A discussion paper. Journal of Clinical Nursing, 27(11–12), 2496–2505. 10.1111/jocn.14296 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Supporting information
Supporting information


