Abstract
Background In the hand, giant cell tumors (GCTs) of the bones account for 2 to 5% of all hand tumors; they are often seen in the metacarpals and phalanges, seldom in the carpal bones. In the carpal bones, GCT usually occurs as a single lesion, with multifocal involvement being extremely rare. On analysis of recent English literature, we could find out only two reports having simultaneous involvement of multiple carpal bones.
Case Description We report a case of a 29-year-old female with simultaneous involvement of two carpal bones: capitate and hamate. After confirming the diagnosis by histopathological examination, the affected carpals were resected, and the defect was filled with autologous bone graft. Follow-up at 18 months demonstrated no evidence of local recurrence or metastatic disease, and the patient is now having a reasonable hand function.
Literature Review We analyzed nine case reports on GCTs in carpal bones in the past 25 years. Seven out of nine cases that we could analyze showed single carpal bone involvement (three capitate, two scaphoid, one hamate, one triquetrum). In these, four patients had undergone resection, and five patients had undergone curettage, of whom one patient came back 5 months later with recurrence. Only two cases were there with simultaneous involvement of multiple carpal bones. Both the cases were managed with resection and reconstruction with autologous graft iliac graft.
Clinical Relevance GCTs of the carpal bones are relatively rare, and simultaneous involvement of two bones is rarer. Every attempt should be made to preserve useful wrist range of motion by excision and limited carpal fusion.
Keywords: giant cell tumor, capitate and hamate, carpal fusion, tricortical iliac graft
Giant cell tumors (GCTs) of the bone accounts for approximately 5% of primary bone tumors. 1 2 3 4 They are most frequently located in the metaepiphyses of the long bones, more commonly at the knee and distal radius, followed by the sacrum. In the hand, GCTs of the bone account for 2 to 5% of all hand tumors; they are most often seen in the metacarpals and phalanges and rarely in the carpal bones. 1 2
Most cases of GCTs in the carpal bones consist of a single lesion, with multifocal involvement being very rare. 5
Plain radiographs show radiolucent, expansile lesion with indistinct borders involving the epiphyseal bone, with or without cortical destruction and extension into the soft tissues. 1 2 3 4 Even though GCT is histologically benign, it tends to recur after treatment with intralesionalcurettage 1 due to its local aggressiveness. Therefore, most hand surgeons prefer to perform en bloc tumor excision with wrist arthrodesis or proximal row carpectomy in cases of cortical erosion or multifocal involvement. 4
Case Report
A 29-year-old right-handed woman presented with a 1-year history of pain and localized swelling at the dorsum of the right wrist. She denied any history of wrist and hand trauma. Physical examination showed swelling, tenderness, and decreased range of motion (ROM) of the wrist joint ( Fig. 1 ). Routine blood laboratory values including thyroid profile were within normal limits.
Fig. 1.

Photograph showing swelling over the dorsum of the right wrist.
Standard radiographs of the right wrist showed osteolysis of the capitate and hamate, with areas of cortical destruction ( Fig. 2 ).
Fig. 2.

(A, B) Plain radiograph of the wrist showing osteolysis of the capitate and hamate, with areas of cortical destruction.
A magnetic resonance imaging (MRI) was performed ( Fig. 3 ), which confirmed abnormal bone marrow signal throughout the capitate and hamate, with homogenously intermediate signals present on T1-weighted imaging and diffusely hyperintense signals on STIR (short tau inversion recovery) images.
Fig. 3.
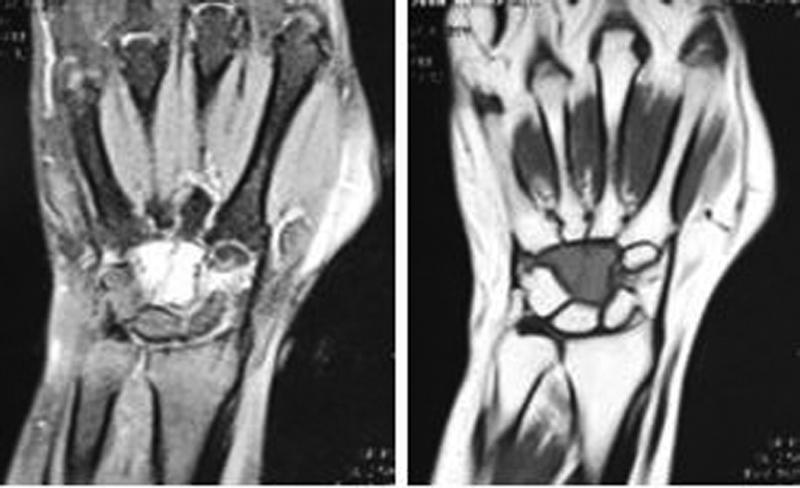
(A, B) Magnetic resonance imaging coronal sections showing homogenously intermediate signal mass in the capitate and hamate in T1-weighted imaging and diffusely hyperintense signal on STIR (short tau inversion recovery) image (1.5 T).
A core biopsy was performed to confirm the diagnosis. Histopathological examination ( Fig. 4 ) showed many multinucleate giant cells dispersed amidst sheets of mononuclear cells, and the individual cells were round to oval in shape having bland nuclear chromatin and pale cytoplasm, suggesting GCT. The possibility of brown tumors due to hyperparathyroidism has been ruled out through blood investigation.
Fig. 4.
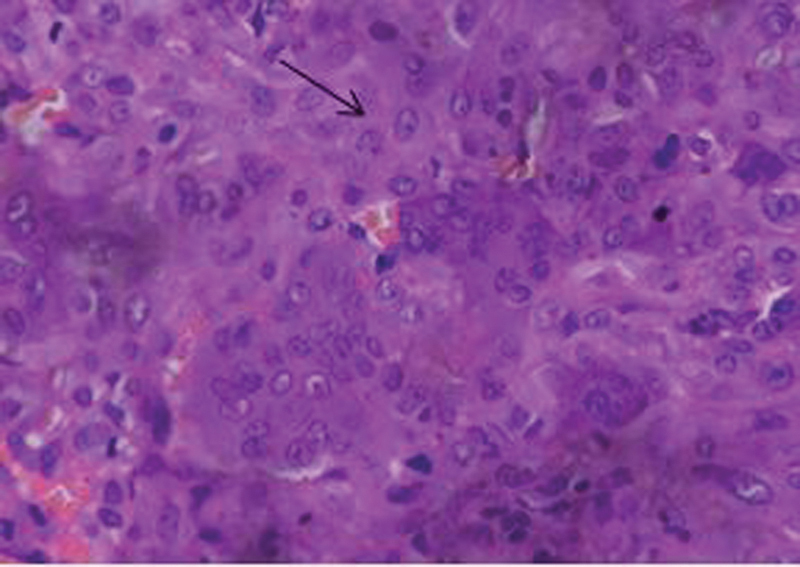
Histopathology: multinucleate giant cell dispersed amidst sheets of mononuclear cells (hematoxylin–eosin staining, 400 × ).
After confirming the diagnosis, the affected carpal bones along with any macroscopic soft tissue were resected through a dorsal approach to the wrist ( Fig. 5 ) and the defect was filled with a carefully shaped autologous tricortical iliac crest bone graft, and limited wrist arthrodesis was achieved between the lunate and triquetrum proximally and the third, fourth, and fifth metacarpals distally ( Fig. 6 ). Wrist ROM between the radius and proximal carpal row was well preserved. After skin closure, a volar slab in functional hand position was applied for 6 weeks. Grip strengthening exercises and wrist ROM exercises were started thereafter.
Fig. 5.
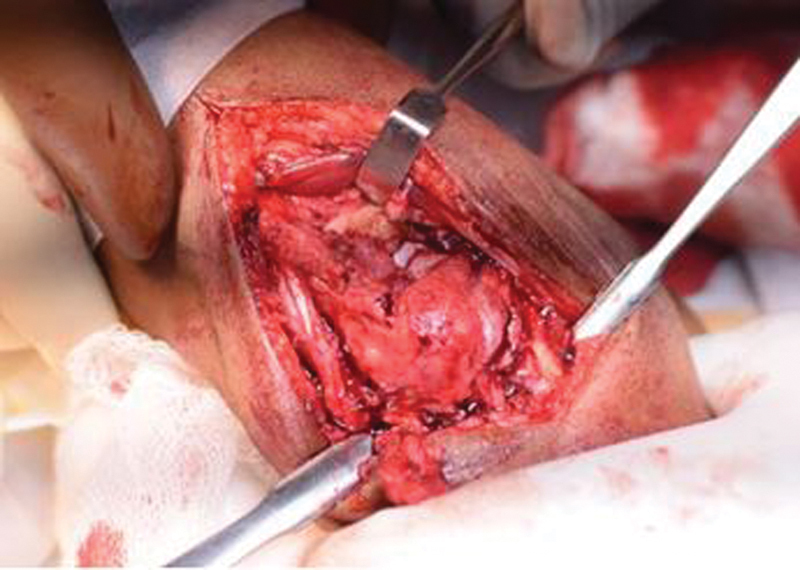
Tumor involving the capitate and hamate on dorsal approach to the wrist.
Fig. 6.
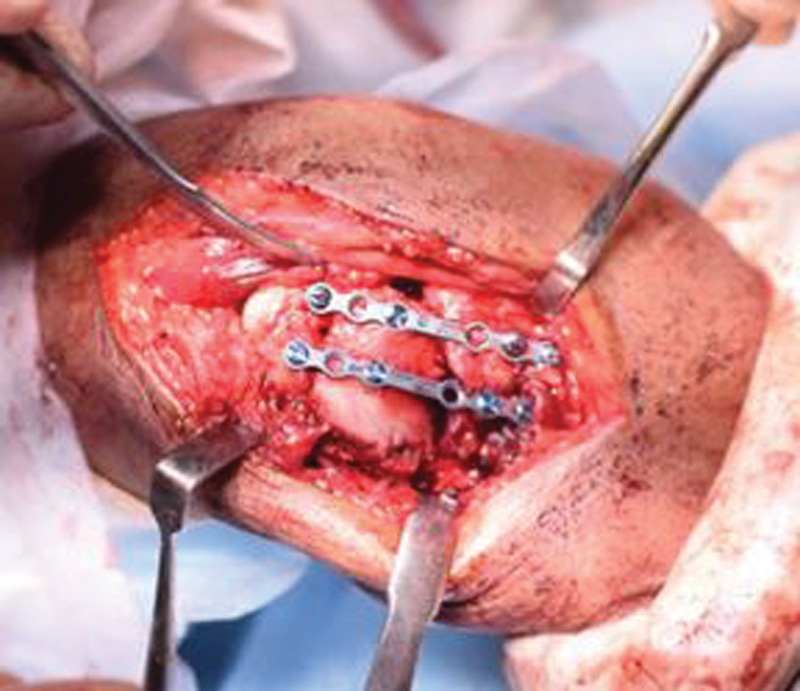
Arthrodesis between the lunate and triquetrum proximally and the third, fourth, and fifth metacarpals distally using a miniplate.
Time period : the patient has been followed up for 18 months postsurgery.
Discussion
GCTs are an uncommon tumor of the wrist bones. Averill et al reported 2 GCTs in the hamate and trapezoid bones among 28 GCTs of the hand and wrist bones. 2 In a review of 1,228 GCTs from 20 articles, there were 4 GCTs in the hamate, lunate, and scaphoid bones. 2 In a review of 28,600 primary neoplasms of the carpal bones between 1909 and 1990, there were two GCTs of the capitate among the five GCTs of the wrist bones. 6
Two general treatment strategies have been used for the treatment of bone GCTs in the hand: (1) Intralesional procedures including curettage with or without bone grafting and (2) excisional procedures including excision of the affected carpus, wide excision, and amputation. Although GCTs are almost always benign, these tumors are locally aggressive and tend to have a high recurrence rate (probably 60% or greater) after treatment by curettage and bone grafting. 7 8 9
We analyzed nine case reports on GCT in carpal bones in the past 25 years ( Table 1 ). Seven out of nine cases that we could analyze showed single carpal bone involvement (three capitate, two scaphoid, one hamate, one triquetrum). Of these patients, four had undergone resection and five had undergone curettage, of who one came back 5 months later with recurrence in the hamate and the base of the second, third, and fourth metacarpals, which was managed with resection of the capitate, part of the hamate, and the base of the third metacarpal, phenol application, and carpometacarpal arthrodesis with autologous iliac crest bone graft.
Table 1. Summary of review of the literature on GCTs of the carpal bones.
| No. | Authors | Year | Age | Sex | Bone(s) | Duration | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Abdu et al 10 | 1994 | 30 | M | Scaphoid | 6 mo | Resection and silicone implant | Mild reactive silicone synovitis Good wrist function and no evidence of recurrent disease |
| 2 | Gupta et al 5 | 1995 | 30 | M | Capitate, hamate, and triquetrum | Distal row carpectomy with reconstruction of the left wrist with a bicortical iliac autogenous bone graft and arthrodesis of the distal carpal segment to metacarpals | No recurrence with good hand function on 18-mo follow-up | |
| 3 | Kew et al 11 | 2000 | 18 | M | Scaphoid | 2 mo | Resection and a pronator quadratus pedicle bone grafting with radioscaphoid fusion | No recurrence was found on 7-y follow-up |
| 4 | Sakayama et al 12 | 2008 | 24 | F | Hamate | 3 mo | Curettage with acrylic cementation | No recurrence with 100% functional recovery on 3-y follow-up |
| 5 | Tarng et al 13 | 2009 | 29 | F | Scaphoid, capitate, trapezium, and trapezoid | En bloc resection through a dorsal and volar approach for soft tissue resection, with defect filled autologous with bicortical iliac crest bone graft | No evidence of clinical and radiological evidence of recurrence on 1-y follow-up | |
| 6 | Kotnis et al 14 | 2009 | 44 | M | Triquetrum | 8 mo | Surgical exploration and local curettage | The patient was symptom-free till for 4 m |
| 7 | Angelini et al 15 | 2011 | 21 | F | Capitate | 7 mo | Curettage + phenol ablation + morselized corticocancellous bone allograft | Recurrence noticed after 5 mo |
| 8 | Oufkir et al 16 | 2017 | 48 | F | Capitate | 1 y | Staged procedure Curettage and bone cement Corticocancellous bone graft from the iliac crest, with lunometacarpal arthrodesis |
Complex regional pain syndrome in the early postoperative period 2 y after surgery: pain-free with functional range of motion (30 degrees of extension, 25 degrees of flexion), the grip strength was 50% of that of the unaffected side |
| 9 | Afsharet al 17 | 2018 | 16 | F | Capitate | 6 mo | Intralesional curettage + alcohol ablation + allogenic bone graft | Satisfactory hand function without any recurrence at 2-y follow-up |
Abbreviations: F, female; GCT, giant cell tumor; M, male.
Only two reports in the English literature shows simultaneous involvement of multiple carpal bones. In the first case, which was reported by Gupta et al, there was simultaneous involvement of the capitate, hamate, and triquetrum, which was managed with distal row carpectomy with reconstruction of the left wrist with a bicortical iliac autogenous bone graft and arthrodesis of the distal carpal segment to metacarpals, and there was no recurrence, with good hand function on 18-month follow-up. The second case was reported by Tarng et al in 2008 in which the scaphoid, capitate, trapezium, and trapezoid were involved and was managed with en bloc resection through a dorsal and volar approach for soft tissue resection, the defect was filled with autologous bicortical iliac crest bone graft, and there was no clinical and radiological evidence of recurrence on 1 year of follow-up.
Ours is the only third case with simultaneous involvement of two carpal bones. In our patient, 18-month follow-up demonstrated no evidence of local recurrence or metastatic disease. The patient is now experiencing a reasonable functional ROM (wrist flexion of 35 degrees, wrist extension of 40 degrees, ulnar deviation of 10 degrees, radial deviation of 5degrees) ( Fig. 7 ) and a good hand grip. Check X-ray showed good fusion with preservation of radiolunate articulation ( Fig. 8 ).
Fig. 7.

Range of motion of the wrist after 18 months.
Fig. 8.

(A, B) Postoperative X-ray on 18-month follow-up after surgery.
Conclusion
GCTs of carpal bones are relatively rare, and simultaneous involvement of two bones is rarer. Every attempt should be made to preserve useful wrist ROM by excision and limited carpal fusion.
Acknowledgments
We thank our seniors and colleagues in our institute who helped us to publish this case by providing articles on GCTs that includes carpal bones.
Conflict of Interest None declared.
Note
This work was performed at All India Institute of Medical Sciences (AIIMS), Rishikesh, Uttarakhand, India.
References
- 1.Shigematsu K, Kobata Y, Yajima H, Kawamura K, Maegawa N, Takakura Y. Giant-cell tumors of the carpus. J Hand Surg Am. 2006;31(07):1214–1219. doi: 10.1016/j.jhsa.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 2.Averill R M, Smith R J, Campbell C J. Giant-cell tumors of the bones of the hand. J Hand Surg Am. 1980;5(01):39–50. doi: 10.1016/s0363-5023(80)80042-6. [DOI] [PubMed] [Google Scholar]
- 3.McDonald D J, Schajowicz F. Giant cell tumor of the capitate. A case report. Clin Orthop Relat Res. 1992;(279):264–268. [PubMed] [Google Scholar]
- 4.Howard F M, Lassen K. Giant cell tumor of the capitate. J Hand Surg Am. 1984;9(02):272–274. doi: 10.1016/s0363-5023(84)80159-8. [DOI] [PubMed] [Google Scholar]
- 5.Gupta G G, Lucas G L, Pirela-Cruz M. Multifocal giant cell tumor of the capitate, hamate, and triquetrum: a case report. J Hand Surg Am. 1995;20(06):1003–1006. doi: 10.1016/S0363-5023(05)80149-2. [DOI] [PubMed] [Google Scholar]
- 6.Murray P M, Berger R A, Inwards C Y. Primary neoplasms of the carpal bones. J Hand Surg Am. 1999;24(05):1008–1013. doi: 10.1053/jhsu.1999.1008. [DOI] [PubMed] [Google Scholar]
- 7.Goldenberg R R, Campbell C J, Bonfiglio M. Giant-cell tumor of bone. An analysis of two hundred and eighteen cases. J Bone Joint Surg Am. 1970;52(04):619–664. [PubMed] [Google Scholar]
- 8.Johnson E W, Jr, Dahlin D C. Treatment of giant-cell tumor of bone. J Bone Joint Surg Am. 1959;41-A(05):895–904. [PubMed] [Google Scholar]
- 9.Hutter R VP, Worcester J N, Jr, Francis K C, Foote W F, Jr, Stewart F W. Benign and malignant giant cell tumors of bone. A clinicopathological analysis of the natural history of the disease. Cancer. 1962;15:653–690. doi: 10.1002/1097-0142(196207/08)15:4<653::aid-cncr2820150402>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 10.Abdu W A, Murphy L M, Memoii V A. Giant cell tumor of the scaphoid: a case report and review of the literature. J Hand Surg Am. 1994;19(06):1003–1005. doi: 10.1016/0363-5023(94)90105-8. [DOI] [PubMed] [Google Scholar]
- 11.Kew J, Kumta S M, Leung P C. Case reports. Giant cell tumour in the scaphoid bone. ClinRadiol. 2000;55(09):717–718. doi: 10.1053/crad.2000.0112. [DOI] [PubMed] [Google Scholar]
- 12.Sakayama K, Sugawara Y, Kidani T. Giant cell tumour of the hamate treated successfully by acrylic cementation: a case report. J Hand Surg Eur Vol. 2008;33(06):803–805. doi: 10.1177/1753193408095880. [DOI] [PubMed] [Google Scholar]
- 13.Tarng Y W, Yang S W, Hsu C J. Surgical treatment of multifocal giant cell tumor of carpal bones with preservation of wrist function: case report. J Hand Surg Am. 2009;34(02):262–265. doi: 10.1016/j.jhsa.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Kotnis N A, Davies A M, Kindblom L G, James S LJ. Giant cell tumour of the triquetrum. Skeletal Radiol. 2009;38(06):593–595. doi: 10.1007/s00256-009-0684-z. [DOI] [PubMed] [Google Scholar]
- 15.Angelini A, Mavrogenis A F, Ruggieri P. Giant cell tumor of the capitate. MusculoskeletSurg. 2011;95(01):45–48. doi: 10.1007/s12306-011-0105-z. [DOI] [PubMed] [Google Scholar]
- 16.Oufkir A A, Lazerges C, Coulet B, Chammas M. Giant cell tumor of the capitate treated with excision and midcarpal fusion. J Wrist Surg. 2017;6(03):238–243. doi: 10.1055/s-0037-1598187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Afshar A, Tabrizi A, Aidenlou A, Abbasi A. Giant cell tumor of the capitate bone. J Hand Microsurg. 2018;10(03):158–161. doi: 10.1055/s-0038-1631876. [DOI] [PMC free article] [PubMed] [Google Scholar]


