Abstract
Abdominal aortic aneurysm (AAA) is a disease of the elderly which may result in aneurysm rupture if not treated in a timely manner. The incidence of AAA has increased in part due to patient and physician education, ultrasound screening, and liberal use of computed tomography imaging in conjunction with an aging population. Endovascular aneurysm repair has become the preferred treatment for surgeons and interventionalists. When endografts are placed outside of device-specific instructions for use, the risk of endoleak development is significantly increased. Open surgical repair of Type Ia endoleaks is recommended when endovascular options have been exhausted. Open surgical repair of Type Ia endoleaks provides acceptable perioperative morbidity and mortality rates, long-term durability, and low reintervention rates when performed in the elective setting.
Keywords: endovascular aneurysm repair, endoleaks, open surgical repair, aortic wrap, interventional radiology
Abdominal aortic aneurysm (AAA) is a disease of the elderly which may result in rupture if not treated prophylactically. During the last half century, the incidence of AAA has increased largely due to more liberal use of ultrasound and computed tomography (CT) imaging in conjunction with an aging population. A family history of AAA, hypertension, connective tissue disorders, and tobacco use have identified as independent risk factors for the development and rupture of aneurysms. 1
Aneurysm diameter, rate of growth, morphology, and patient comorbidities determine the timing and repair approach for each patient. Open surgical repair (OSR) of the aneurysmal aortic segment and endovascular aneurysm repair (EVAR) remain the mainstays of treatment. Since its development in the 1990s, EVAR has become the preferred treatment strategy for AAAs due to the significant advantage it confers on patient morbidity and mortality. 2 3 4
Contemporary literature has shown that widespread adoption of EVAR has taken place and OSR has congruently decreased during this same time period. 5 Unfortunately, despite the significant early advantages EVAR provides over OSR, patients remain at risk for late endograft complications and aneurysm sac enlargement especially when endografts are placed outside of the instructions for use (IFU) of each device. 6 Incomplete sealing of the aneurysm sac following EVAR is defined as an endoleak. Failure of the endograft to seal at the proximal aortic neck (Type Ia endoleak) may leave the aortic sac pressurized and at risk of rupture. A significant portion of endoleaks can generally be treated by endovascular means; however, open reinterventions are still required. In this article, we will summarize the indications and options for open repair of Type Ia endoleaks, the available literature, and technical considerations in patients requiring these therapies.
Indications
As the use of EVAR has become more readily available and more devices are approved by the Food and Drug Administration (FDA), a growing volume of surgeons and interventionalists are placing endografts. When placed outside of the device-specific IFU, the risk of endoleak development increases. Some approved endografts may be placed within their own IFU; however, hostile neck anatomy increases the risk of endograft complications (proximal neck length) <10 mm, focal bulge in the proximal aortic neck >3 mm, > 10% reverse taper within 15 mm of the renal arteries, neck thrombus >50% of the circumference, and extensive calcification or proximal neck angulation >60 degrees 7 ( Fig. 1 ). Open repair of Type Ia endoleaks is recommended when endovascular options have been exhausted and enlargement of the aortic sac occurs.
Fig. 1.
Type Ia endoleak with hostile neck anatomy: proximal neck length <10 mm, >10% reverse taper within 15 mm of the renal arteries, and proximal neck angulation >60 degrees. These additive features increase the risk of endograft complications.
Explantation/Open Conversion
Surgical endograft explantation and open conversion are the most invasive and successful OSR options for the correction of persistent Type Ia endoleaks ( Fig. 2 ). The EUROSTAR registry estimated a 2.1% risk of open conversion with the majority performed for treating Type I, II, and III endoleaks. Moulakakis et al determined the incidence of open conversion to be 0.8 to 5.9% among all AAA patients following EVAR. 8 Our institutional data show an increase in open conversions over time with Type Ia endoleaks being the primary indication (both in ruptured and unruptured patients). 1
Fig. 2.

Ex vivo image of surgical endograft explantation for correction of Type Ia endoleak.
Technique and Technical Considerations
Advanced endovascular interventions such as parallel stent grafting (i.e., snorkels, chimneys, and/or periscopes) and the use of active fixation endoanchors have reduced the need for open reinterventions ( Fig. 3 ). However, they have made open conversion far more challenging when advanced interventions fail. Meticulous preoperative planning and a solid fund of knowledge about device-specific nuances must be considered prior to performing open repair. Fixation of the endograft in a suprarenal location, in the setting of suprarenal fixation stents or parallel stent grafts, often necessitates supraceliac aortic cross clamping or balloon occlusion for inflow control. The decision to remove the entirety of the endograft is dependent on physician experience, quality of the aortic neck, endograft type, previous endovascular reinterventions, and/or the presence of infection. Proximal device components can safely be left in place and incorporated in the proximal anastomosis if explanting the endograft is not safe or possible. Inflammation and active fixation can make endograft explant difficult and often the aortic wall will be “thinned out” which supports the concept of incorporating the proximal portion of the endograft into the suture line. Similarly, the iliac limbs may be left in place and incorporated into the distal anastomosis if the iliac fixation makes removal problematic. Surgeons should not underestimate the degree of periaortic inflammation and retroperitoneal fibrosis which makes exposure challenging.
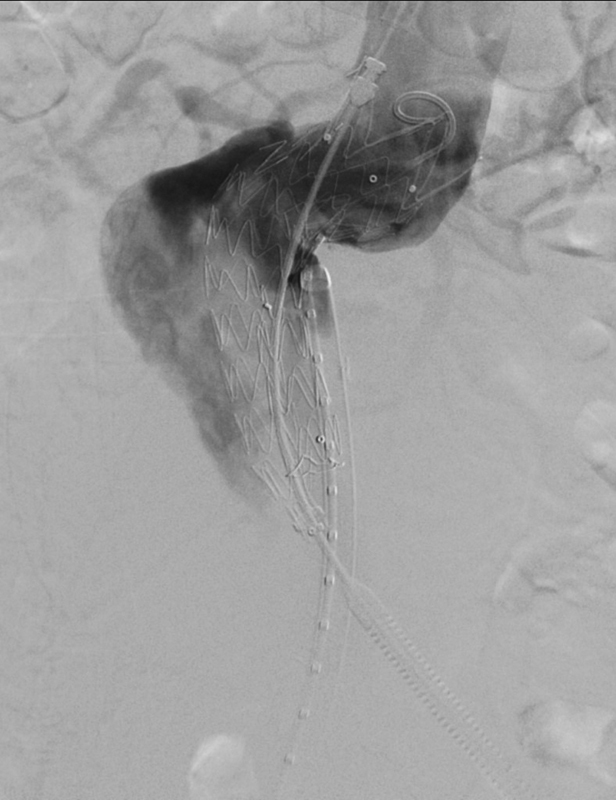
Fig. 3.

Endovascular interventions such as parallel stent grafting and active fixation endoanchors have made open conversion far more challenging when advanced interventions fail.
The majority of open endograft conversions are achieved through a midline celiotomy. Retroperitoneal exposure or thoracolaparotomy incisions may be required in selected situations or by surgeon preference. A review of 587 open conversions by Kouvelos et al found that infrarenal aortic cross clamping was possible in 43% of cases, with 26.2% requiring suprarenal clamping and 27.9% requiring supraceliac clamping. 9
Once inflow control has been achieved, the aneurysm sac is opened and distal control is obtained by clamping the iliac arteries or endograft limbs. Residual back bleeding may be seen from the lumbar arteries or inferior mesenteric artery should be ligated at this juncture. Endografts with infrarenal fixation (i.e., Gore Excluder, Medtronic Aneuryx) are explanted without much difficulty. Devices with suprarenal fixation (i.e., Cook Zenith, Medtronic Endurant) require one of several techniques to remove the graft and active fixation components: clamp device and gently pullout, cranially advancing the endograft and compressing the hooks prior to withdrawal, or transecting the endograft at the level of the fabric followed by releasing the barbs from the main body with wire cutters ( Fig. 4 ). Alternatively, collapsing the suprarenal fixation stents using a modified large 50-mL syringe may aid in the removal of the graft. The proximal anastomosis may then be performed using 2–0 or 3–0 polypropylene sutures with or without incorporating the remaining endograft material if removal was not safe or possible. An end-to-end anastomosis can be performed to the common iliac arteries ( Fig. 5 ) or the endograft limbs, if the limbs cannot be completely removed.
Fig. 4.

Devices with suprarenal fixation, as demonstrated here, often require supraceliac aortic control and special techniques to remove the graft and active fixation components.
Fig. 5.

An end-to-end anastomosis performed with a polyester graft sewn to the common iliac arteries.
Aortic Wraps
Preservation of the entire endograft may be possible in select patients. In a series by Kouvelos et al, 4.8% of endografts were able to be fully preserved. 9 This was achieved by external aortic neck banding for Type Ia endoleaks or ligation of lumbar or inferior mesenteric arteries after sacrotomy for Type II endoleaks. We will focus on aortic neck banding or wraps.
An aortic wrap or “neo-aortic neck” may be created by wrapping a 2- to 3-cm polyester graft around the proximal aortic wall ( Fig. 6 ). Circumferential dissection of the infrarenal aortic neck is required, with careful consideration to not injure the posterior lumbar arteries, renal arteries, or a retroaortic left renal vein. Once circumferential control is obtained, a Dacron graft is passed behind the aorta to create an external cerclage. Banding of the aortic neck is achieved by tightening down the graft material and then securing it to both the aortic wall and endograft. Polypropylene sutures are placed through the external wrap, native aortic wall, and indwelling endograft with felt pledgets for reinforcement ( Fig. 7 ). Loss of aortic sac pulsation, intraoperative duplex, sacrotomy, or diagnostic angiography may be considered to evaluate procedural success.
Fig. 6.

Aortic wrap or “neo-aortic neck” created by wrapping a 2- to 3-cm polyester graft around the proximal aorta.
Fig. 7.
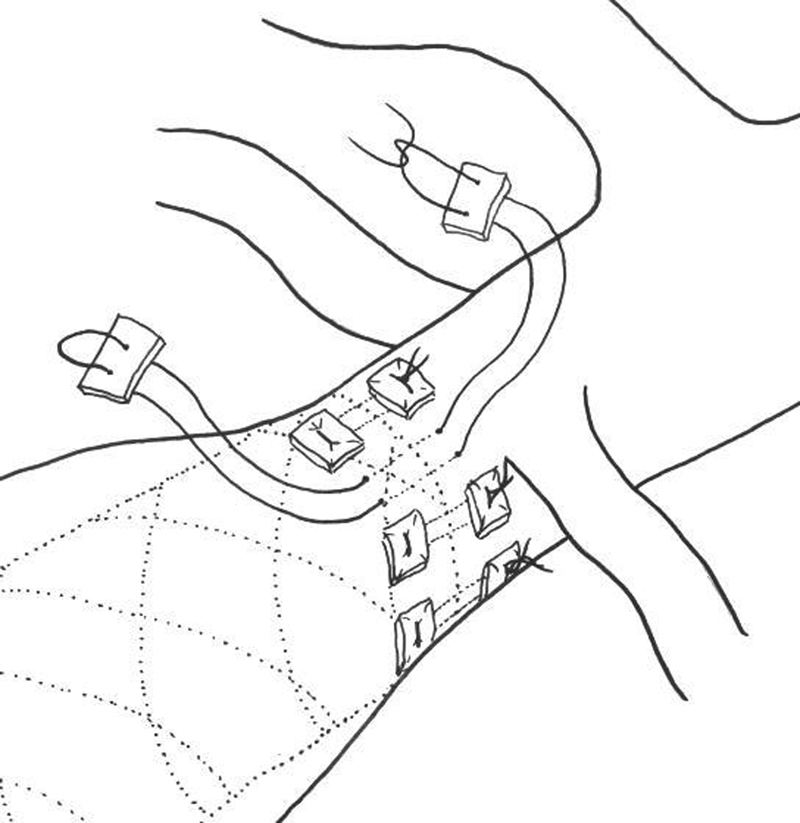
Polypropylene sutures placed through the external wrap, native aortic wall, and indwelling endograft with felt pledgets for reinforcement.
Similar considerations may be taken intraoperatively with regard to periaortic inflammation and retroperitoneal fibrosis. Aortic cross clamping can be avoided utilizing this technique, which limits the physiologic stress and blood loss imposed on the patients undergoing this procedure. Our institutional series found the perioperative morbidity and mortality rates in this cohort to be similar to complete open conversion, though this cohort appeared to be older and of higher risk. 10
Outcomes
As several interventionalists and surgeons become familiar with EVAR, a growing number of patients will require reinterventions and ultimately OSR will be required once endovascular therapy has been exhausted. Current literature suggests that endograft implantation outside of device-specific IFU increases the risk of secondary reinterventions. A review of 1,060 patients by Kansal et al found that 16 patients required open conversion, and all endografts were found to have been placed outside of device-specific IFU. 11 This liberalization of EVAR use may lead to increasing numbers of open reinterventions.
Open repairs of Type Ia endoleaks, especially those which require aortic cross clamping, expose patients to many of the same risks as traditional OSR. An 8-year single-center experience of 31 open conversions published by Abdallah et al reported an overall 30-day mortality rate of 6% and overall hospital mortality of 10%. 12 Overall, 42% of the patients in that cohort experienced moderate to severe complications, with pulmonary and renal being significantly higher in the setting of emergent open conversion (42 vs. 5%, p = 0.02 and 42 vs. 0%, p = 0.005, respectively). Kouvelos et al identified 26 articles encompassing 641 patients who underwent open conversion. Thirty-day mortality was reported to be 9.1% with a significantly higher rate for nonelective interventions (29.2 vs. 3.2%). 9 Multiple studies have also demonstrated higher rates of mortality with nonelective conversions (40–56%). 13 14 The Vascular Quality Initiative registry was queried by Scali et al and they noted a mortality rate of 51.5% for open conversion when performed for rupture. This was significantly higher than the 35.1% rate of mortality noted for primary open repair for rupture ( p = 0.009). 15 Our institutional data were reported and noted a 40% rate of perioperative mortality of open conversion for rupture. 1 The literature suggests that patients undergoing open conversion are generally older with more significant comorbidities compared with patients undergoing primary open AAA repair.
The majority of open conversions are not performed in emergent settings. Kouvelos et al noted in their review that 62.4% were performed electively to treat refractory endoleaks. Mortality rates for elective open conversions are significantly lower than those performed for rupture; however, the National Surgical Quality Improvement Program study revealed that open conversion was associated with higher perioperative mortality rates compared with primary OSRs (10 vs. 4.2%, p < 0.0001). 9 Morbidity and mortality rates may be decreased by utilizing less invasive interventions like aortic wraps, which eliminate the need for aortic cross clamping. Our institutional experience of 28 limited open conversions (i.e., aortic wraps) achieved a mortality rate of 3.6%. 1 This supports aortic wrapping as an additional treatment option in a select group of patients with acceptable mortality rates.
Conclusion
Open surgical repair of Type Ia endoleaks requires a unique skillset that must be maintained in current practice. Modern endograft technology allows for better active fixation and sealing while maintaining perfusion to branch vessels. Despite these advancements, device-related complications still require OSR. Open interventions for the treatment of Type Ia endoleaks provide acceptable perioperative morbidity and mortality rates, long-term durability, and reintervention rates especially when performed in the elective setting. Multiple open surgical options are available to treat this growing patient population. As the use of EVAR becomes more widespread and providers continue to push the envelope outside of the IFU, these OSR options remain effective in managing some of the inevitable EVAR complications that are not amenable to endovascular therapy.
Footnotes
Conflict of Interest None declared.
References
- 1.Mohapatra A, Robinson D, Malak O. Increasing use of open conversion for late complications after endovascular aortic aneurysm repair. J Vasc Surg. 2019;69(06):1766–1775. doi: 10.1016/j.jvs.2018.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.EVAR Trial participants Greenhalgh R, Brown L C, Kwong G PS, Powell J T, Thompson S G.Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial Lancet 2004364(9437):843–848. [DOI] [PubMed] [Google Scholar]
- 3.Dutch Randomized Endovascular Aneurysm Management (DREAM)Trial Group . Prinssen M, Verhoeven E LG, Buth J. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351(16):1607–1618. doi: 10.1056/NEJMoa042002. [DOI] [PubMed] [Google Scholar]
- 4.Open Versus Endovascular Repair (OVER) Veterans Affairs Cooperative Study Group . Lederle F A, Freischlag J A, Kyriakides T C. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302(14):1535–1542. doi: 10.1001/jama.2009.1426. [DOI] [PubMed] [Google Scholar]
- 5.Suckow B D, Goodney P P, Columbo J A. National trends in open surgical, endovascular, and branched-fenestrated endovascular aortic aneurysm repair in Medicare patients. J Vasc Surg. 2018;67(06):1690–16970. doi: 10.1016/j.jvs.2017.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schanzer A, Greenberg R K, Hevelone N. Predictors of abdominal aortic aneurysm sac enlargement after endovascular repair. Circulation. 2011;123(24):2848–2855. doi: 10.1161/CIRCULATIONAHA.110.014902. [DOI] [PubMed] [Google Scholar]
- 7.Dillavou E D, Muluk S C, Rhee R Y. Does hostile neck anatomy preclude successful endovascular aortic aneurysm repair? J Vasc Surg. 2003;38(04):657–663. doi: 10.1016/s0741-5214(03)00738-9. [DOI] [PubMed] [Google Scholar]
- 8.Moulakakis K G, Dalainas I, Mylonas S, Giannakopoulos T G, Avgerinos E D, Liapis C D. Conversion to open repair after endografting for abdominal aortic aneurysm: a review of causes, incidence, results, and surgical techniques of reconstruction. J Endovasc Ther. 2010;17(06):694–702. doi: 10.1583/1545-1550-17.6.694. [DOI] [PubMed] [Google Scholar]
- 9.Kouvelos G, Koutsoumpelis A, Lazaris A, Matsagkas M. Late open conversion after endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2015;61(05):1350–1356. doi: 10.1016/j.jvs.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 10.Makaroun M S, Mohaptra A, Singh M J. Ermes: 2018. Open conversion for failed EVAR: increasing need and different strategies; pp. 219–228. [Google Scholar]
- 11.Kansal V, Nagpal S, Jetty P. Editor's choice - late open surgical conversion after endovascular abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2018;55(02):163–169. doi: 10.1016/j.ejvs.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Ben Abdallah I, El Batti S, Abou-Rjeili M, Fabiani J N, Julia P, Alsac J M. Open conversion after endovascular abdominal aneurysm repair: an 8 year single centre experience. Eur J Vasc Endovasc Surg. 2017;53(06):831–836. doi: 10.1016/j.ejvs.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Turney E J, Steenberge S P, Lyden S P. Late graft explants in endovascular aneurysm repair. J Vasc Surg. 2014;59(04):886–893. doi: 10.1016/j.jvs.2013.10.079. [DOI] [PubMed] [Google Scholar]
- 14.Marone E M, Mascia D, Coppi G. Delayed open conversion after endovascular abdominal aortic aneurysm: device-specific surgical approach. Eur J Vasc Endovasc Surg. 2013;45(05):457–464. doi: 10.1016/j.ejvs.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 15.Scali S T, Beck A W, Chang C K. Defining risk and identifying predictors of mortality for open conversion after endovascular aortic aneurysm repair in the vascular quality initiative. J Vasc Surg. 2016;63(04):873–810. doi: 10.1016/j.jvs.2015.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]


