Abstract
Background Volar wrist ganglion is the second most common wrist mass and accounts for 20% of all cases. Surgery is the gold standard for persistent and symptomatic ganglia. Arthroscopic resection has gained popularity in the past two decades. Application of this technique to ganglia in less accessible locations, such as the scaphotrapeziotrapezoidal (STT) joint, however, remains controversial.
Case Description To date, no literature has described using the STT -ulnar (STT-u) and STT -radial (STT-r) joint portals for ganglionic resection.
Literature Review In this report, two cases of arthroscopic ganglionic resection utilizing the STT-u and STT-r joint portals at our institution were described.
Clinical Relevance Arthroscopic resection of STT joint ganglion under portal site local anesthesia is a technically feasible, safe, and effective approach. There was no recurrence observed for both cases at 50 months of follow-up.
Keywords: wrist, ganglion, scaphotrapeziotrapezoidal Joint, arthroscopy, portals
Ganglion is the most common benign soft tissue tumor encountered in hand and wrist. Among which dorsal wrist ganglion is the most common and most cases arise from the scapholunate interval as shown in previous studies. 1 Volar wrist ganglion accounts for 20% of all cases and occurs mainly in the radiocarpal joint, the mid carpal joint, and the scaphotrapeziotrapezoidal (STT) joint. Most of them are asymptomatic and may disappear spontaneously. For those that are persistent and painful, surgical excision is the treatment of choice. 1 2 Traditionally, this involves open surgery. In the past two decades, resection by arthroscopic means has been established as an alternative treatment option. It is recognized for less scarring, quicker functional recovery, and faster return to work. The recurrence rate has been similar if not superior to those of open surgery. 1
However, arthroscopic resection of volar ganglia in the midcarpal joint has been precluded by some authors. Fernandes et al 3 found it technically difficult and was associated with higher recurrence and complications rates. They concluded in their systemic review that there was no clear advantage over open surgery. A similar conclusion was drawn by Rocchi et al 4 in their prospective randomized study, citing neuropraxia, injury to a branch of the radial artery and recurrence as the main drawback of arthroscopic approach. Open surgery was again preferred. Complications in patients subjected to open resection approach include neurovascular injury, postoperative stiffness, pain, grip weakness, and decreased range of motion. Open surgery also results in a larger scar, often hypertrophic, and may be less well tolerated by patients with cosmetic concern. They would not prefer exchanging an unsightly lump for an unsightly permanent scar. 5
The STT-ulnar (STT-u) portal was first described by Whipple. 6 In 2003, Carro et al 7 presented the STT-radial (STT-r) portal which was situated immediately radial to the abductor pollicis longus tendon at the STT joint level. 7 Baré et al 8 also described a palmar (STT-p) portal in a cadaveric study. Together with the classical dorsal radial midcarpal portal, procedures, such as arthroscopic resection of the distal scaphoid and arthrodesis of the STT joint, can be performed. 9
Our center first reported the arthroscopic technique of volar wrist ganglion resection under portal site local anesthesia in 2003. 5 The technique applied to volar ganglia arising from the palmar ligaments of the radiocarpal joint. It has been our standard of practice since. To date, no literature has described using the STT-u and STT-r portals for STT joint ganglionic resection. In this paper, we describe two cases of volar midcarpal wrist ganglia arising from the STT joint that were treated successfully by a novel arthroscopic technique, incorporating the STT-r and STT-u portals.
Case Reports
Case 1
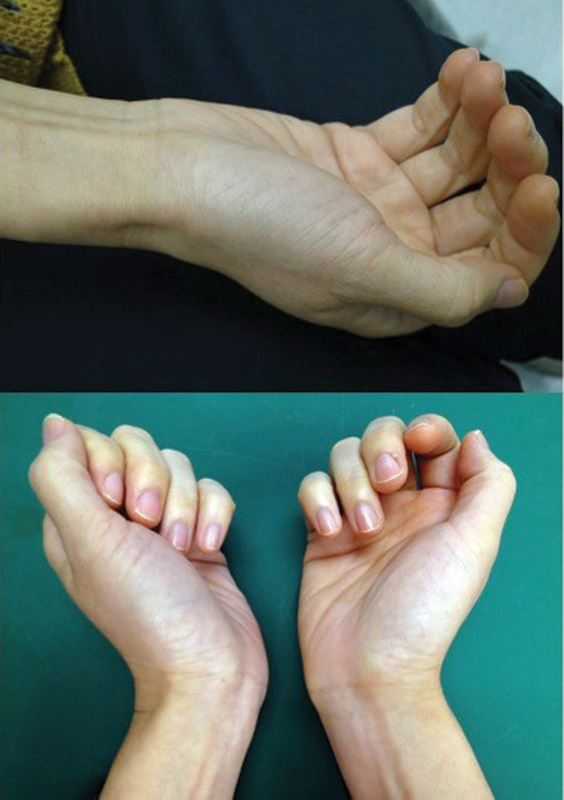
A 45-year-old woman presented with a painful 2 cm × 1.5 cm cystic sessile mass over the right distal radiovolar wrist crease area for more than 3 years ( Fig. 1 ). She has no associated wrist pain. There was no radiological abnormality. Aspiration was performed but the mass soon recurred. Magnetic resonance imaging (MRI) showed a ganglion arising from the STT joint ( Fig. 2 ). She underwent surgery for pain relief and cosmesis. The patient lied supine with the affected wrist placed on a traction tower with 5-kg traction. Three plastic Chinese finger traps were applied to the thumb, index, and middle fingers. Portal site local anesthesia without sedation and tourniquet was administered. To each portal site from the skin down to capsule 1 mL of 2% lignocaine with adrenaline (1:200,000) was injected, followed by injection of saline solution to distend the midcarpal joint and STT joint. Small transverse incisions were made on the skin only, followed by blunt dissection of subcutaneous tissue and joint capsule using a fine curved hemostat. A 30-degree inclined 1.9-mm arthroscope was then introduced into the STT-u portal. Saline irrigation was maintained during the surgery by using a 3-L bag of saline solution hanged 1.5 m above the patient's level. It showed significant synovitis at the STT joint and gross fibrillation of cartilage at the distal scaphoid surface. The base of the trapezium was not very well visualized due to the much thickened synovitis. Under direct vision, the STT-r portal was located and developed with the aid of an 18-G needle. The arthroscope was then switched to the STT-r portal for viewing, while arthroscopic instrument was inserted from the STT-u portal ( Fig. 3 ). By advancing the arthroscopy anteriorly negotiating the joint space between scaphoid, trapezoid, and trapezium, the volar scaphotrapezial ligament could be reached. Application of finger trap to the thumb helped to increase the working space. Synovitis was noted at the palmar capsule and the ligament fiber intervals. External mobilization of the ganglion provoked simultaneous movement of the palmar ligament and the capsule and this maneuver helped to imply the ganglion origin. Shaving of the capsular tissue at the ligament interval while preserving the ligament fiber using a 2-mm motorized arthroscopic shaver was performed. Digital pressure was applied over the ganglion externally to facilitate the shaving process until there was complete drainage of gelatinous fluid into the STT joint and a thorough decompression of the ganglion cyst was noted. Further shaving of the stalk until a capsular defect of 5 to 10 mm was made, with an aim to abolish the pathological valve phenomenon. The wounds were closed with steristrips and covered with compressive bandage. The operation took 52 minutes. There was no neurovascular complication. She was discharged on the same day. Free motion of the wrist was allowed after 3 days. At 1-month follow-up, she had regained full function of her wrist ( Fig. 4 ). An MRI wrist done at 2 years of postoperation did not show recurrence ( Fig. 5 ). She was last followed-up 52 months of postoperation. The scar was inconspicuous and the patient was almost pain free. Her wrist function was evaluated with a therapist-rated assessment tool developed by our hospital. 10 Specific wrist function assessment showed a wrist score of 37 out of 40, a pain score of 3 out of 20, a disabilities of the arm, shoulder, and hand (DASH) score of 25.9%, patient-rated wrist evaluation (PRWE) score 21.5, and a power grip of 26 kg as compare with 22 kg of the opposite hand.
Fig. 1.

Volar wrist mass in case 1.
Fig. 2.
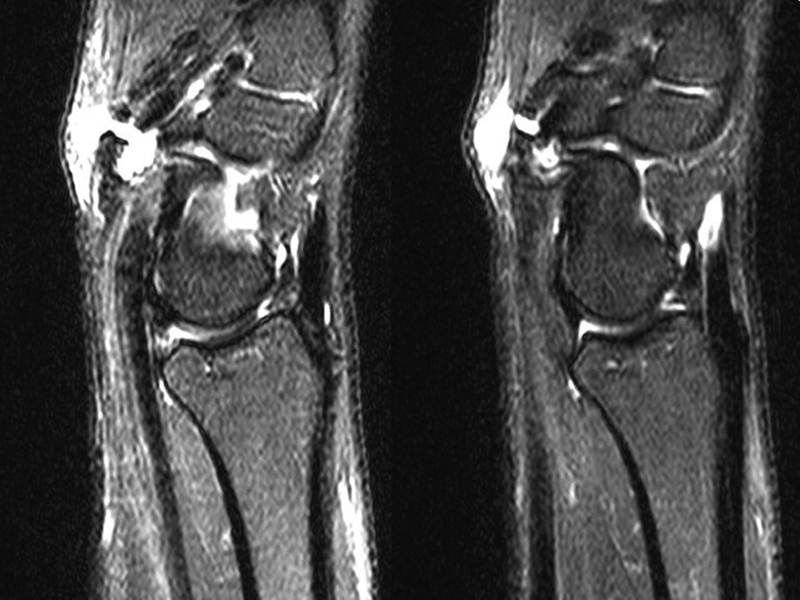
Preoperative wrist magnetic resonance images showing the ganglion stalk arising from the STT joint. STT, scaphotrapeziotrapezoidal.
Fig. 3.

Intraoperative image showing the arthroscope and the shaver in the STT-r and STT-u respectively. STT-r, scaphotrapeziotrapezoidal-radial; STT-u, scaphotrapeziotrapezoidal.
Fig. 4.
Postoperative photograph showing satisfactory cosmesis and extension range of motion at 37 months after surgery.
Fig. 5.

Preoperative wrist magnetic resonance images showing no evidences of ganglion recurrence.
Case 2
A 66-year-old woman presented to our clinic with a nontender 2.5 cm × 2 cm left volar wrist mass which had been there for 11 months, accompanied with radial sided wrist pain. Clinically the lobulated cystic mass extended from the distal to the proximal wrist crease and was separated from the flexor carpi radialis tendon ( Fig. 6 ). There was marked pain on radiocarpal grinding test. A preoperative mini-C arm fluoroscopy revealed marked STT joint arthritis and an ultrasonography confirmed a STT joint ganglion ( Fig. 7 ). The preoperative wrist assessment showed a full range of wrist motion and grip strength of 12 kg. Surgery was performed for pain and cosmesis. Portal site local anesthesia was administered without sedation and tourniquet and the arthroscopic ganglion resection was performed under the same setting as in case 1. Arthroscopy was performed using the midcarpal radial (MCR) portal for viewing and the STT-u portal for instrumentation. It showed a complete STT cartilage eburnation over the three articular surfaces with extensive synovitis ( Fig. 8 ). After removal of the extensive synovitis, the joint space widened due to the vast loss of cartilage and capsular attenuation. Complete evacuation of the ganglion was feasible without employing the STT-r portal, along with a 5 to 10 mm cuff of capsule in the same manner as in case 1 ( Fig. 9 ). The operation lasted for an hour. The patient was followed-up for 48 months ( Fig. 10 ). Postoperative MRI did not show recurrence of ganglion. The wrist range of motion was fully preserved, the scar was almost invisible, and the patient had minimal pain. Specific wrist function test showed a wrist score of 38, a pain score of 2, a DASH score of 39.3%, PRWE score 13.5%, and grip strength of 11 kg as compared with 10 kg of the opposite hand.
Fig. 6.

Photograph of the wrist mass before operation of case 2.
Fig. 7.
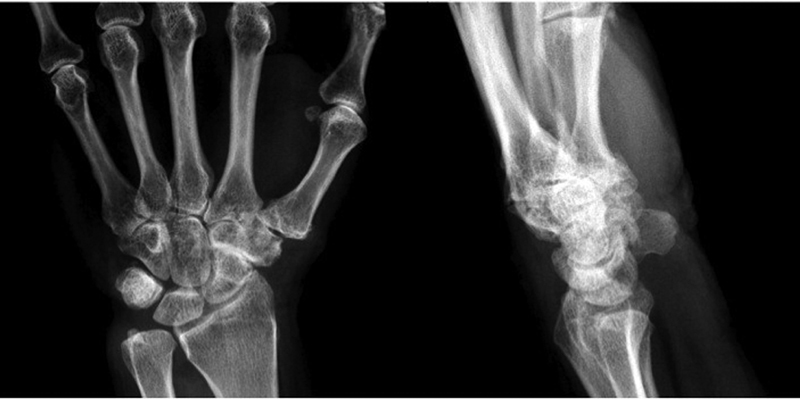
Anteroposterior and lateral radiographs of the wrist showing signs of STT arthritis. STT, scaphotrapeziotrapezoidal.
Fig. 8.
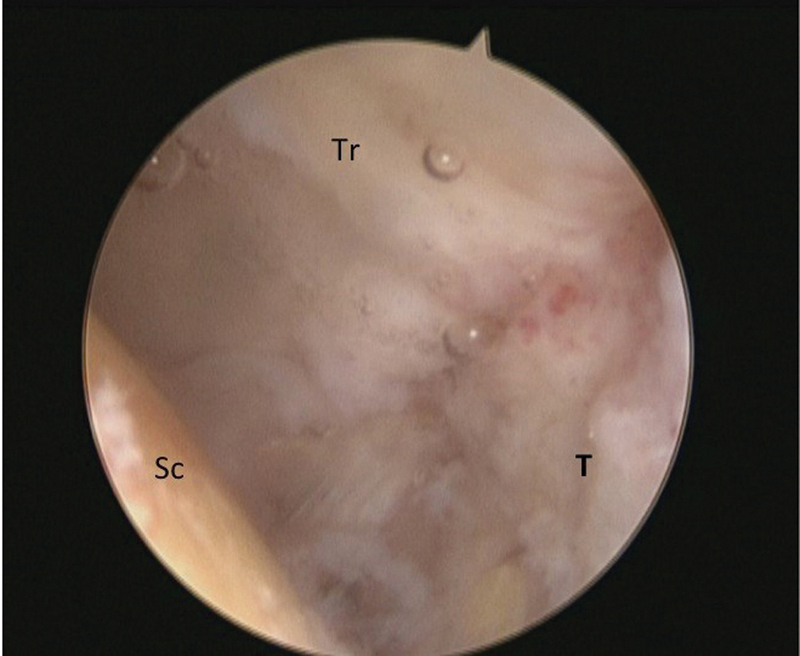
Arthroscopic picture showing the arthritic changes in the STT joint. STT, scaphotrapeziotrapezoidal; Sc, scaphoid, T, trapezium; Tr, trapezoid.
Fig. 9.

Arthroscopic picture showing the capsular defect created (arrow).
Fig. 10.

Postoperative photograph showing satisfactory cosmesis at 48 months after surgery.
Discussion
STT joint ganglion is thought to arise from the scaphotrapezial joint capsule. 1 The origin of the ganglion can be confirmed with the preoperative ganglion location, ultrasonography, and/or MRI. In contrast with the radiocarpal joint ganglion, the stalk of the ganglion lies over the distal wrist crease around the STT joint. During the operation, the stalk can be evaluated with contrast arthrogram performed at the midcarpal joint, or by direct visualization through the STT joint.
Utilizing the STT-r and STT-u portals allows us to navigate to the ganglion even when the joint space is tight, as illustrated in our first case. It is also possible to reach the volar scaphoid-trapezial ligament area by navigating the arthroscope along the outer distal surface of the scaphoid tubercle rather than driving through the space at the STT joint. Nevertheless, in our second case, the classical midcarpal radial and the STT-u portals were sufficient. The main reason was that after debriding the arthritic joint, the joint space widened due to the lack of the cartilage layer and underlying capsular laxity. Additional traction to the thumb also helped to increase the joint space for arthroscopic manipulation. Simultaneous management of the accompanied STT joint arthritis with synovectomy and joint debridement was another advantage of this arthroscopic approach. The operating times for both cases were within an hour.
Portal site local anesthesia was safe, effective, and well tolerated with this approach. Using 2% lignocaine with adrenaline allows almost instantaneous operative procedure without waiting and, hence, saves overall theater time. As the patients were widely awake throughout the procedure and no anesthesia was required on the palmar side of the wrist, neuropraxia of the palmar cutaneous branch of the median nerve could be checked immediately. Use of no tourniquet during the procedure also enabled the surgeon to monitor the status of the superficial radial artery, which was often just superficial to the ganglion. By resecting merely the stalk of the ganglion deep at the volar ligamentocapsular region without intruding the ganglion cyst wall, the risk of vascular injury was minimized.
In both cases, the wounds were opposed with adhesive sterile strips. No suturing was required though a bulky dressing was applied for a few days to avoid immediate pseudoganglion recurrence because the ganglia wall was not resected. Immobilization was not required, and active and gentle passive mobilization of the wrist was encouraged. The free communication between the cyst remnant and the wrist joint would allow accumulation of joint fluid in the cyst remnant, mimicking the recurrence of the ganglion cyst. Both patients were educated about this “pseudorecurrence” phenomenon and advised to perform regular self-massage of the ganglion site frequently to reduce pseudorecurrence of the ganglion for the first 3 weeks after surgery until the stalk completely healed with normal fibrosis. To date, no recurrence was noted in both cases even after more than 4 years. The transverse scars resulting from arthroscopic ganglion resection are minimal and inconspicuous, in contrast to the frequent appearance of hypertrophic scars as in open resection. The technique is therefore appealing to those patients with higher aesthetic expectation. As the STT-r portal is not commonly used by wrist arthroscopists, the technique requires some learning curve for the surgeon to reduce the possible complication, such as neurovascular injury or cartilage damage, especially in patients without coexisting STT arthritis. Using additional traction on the thumb and a small-sized arthroscope of 1.9 mm aid to improve the maneuverability of the joint.
Conflict of Interest None declared.
Note
All the work was performed at the Department of Orthopaedics and Traumatology, Prince of Wales Hospital, Hong Kong, People's Republic of China.
References
- 1.Mathoulin C, Gras M. Arthroscopic management of dorsal and volar wrist ganglion. Hand Clin. 2017;33(04):769–777. doi: 10.1016/j.hcl.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Lidder S, Ranawat V, Ahrens P. Surgical excision of wrist ganglia; literature review and nine-year retrospective study of recurrence and patient satisfaction. Orthop Rev (Pavia) 2009;1(01):e5. doi: 10.4081/or.2009.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernandes C H, Miranda C D, Dos Santos J B, Faloppa F. A systematic review of complications and recurrence rate of arthroscopic resection of volar wrist ganglion. Hand Surg. 2014;19(03):475–480. doi: 10.1142/S0218810414300046. [DOI] [PubMed] [Google Scholar]
- 4.Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scand J Plast Reconstr Surg Hand Surg. 2008;42(05):253–259. doi: 10.1080/02844310802210897. [DOI] [PubMed] [Google Scholar]
- 5.Ho P C, Lo W N, Hung L K. Arthroscopic resection of volar ganglion of the wrist: A new technique. Arthroscopy. 2003;19(02):218–221. doi: 10.1053/jars.2003.50035. [DOI] [PubMed] [Google Scholar]
- 6.Whipple T L. Philadelphia: JB Lippincott; 1992. Arthroscopic surgery. Volume 1: the wrist; pp. 171–175. [Google Scholar]
- 7.Carro L P, Golano P, Fariñas O, Cerezal L, Hidalgo C. The radial portal for scaphotrapeziotrapezoid arthroscopy. Arthroscopy. 2003;19(05):547–553. doi: 10.1053/jars.2003.50155. [DOI] [PubMed] [Google Scholar]
- 8.Baré J, Graham A J, Tham S K. Scaphotrapezial joint arthroscopy: a palmar portal. J Hand Surg Am. 2003;28(04):605–609. doi: 10.1016/s0363-5023(03)00253-3. [DOI] [PubMed] [Google Scholar]
- 9.Mathoulin C, Darin F. Arthroscopic treatment of scaphotrapeziotrapezoid osteoarthritis. Hand Clin. 2011;27(03):319–322. doi: 10.1016/j.hcl.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Ho P C, Tse W I, Wong C W, Chow E C. Arthroscopic osteochondral grafting for radiocarpal joint defects. J Wrist Surg. 2013;2(03):212–219. doi: 10.1055/s-0033-1351788. [DOI] [PMC free article] [PubMed] [Google Scholar]


