Abstract
Background:
Nursing home residents with dementia commonly experience low food intake, leading to negative functional and nutritional consequences. While the importance of staff-resident (dyadic) interactions during mealtime is acknowledged, little research has examined the role of dyadic verbal interactions on food intake.
Objectives:
This study aimed to examine the relationship between food intake and dyadic verbal interactions.
Methods:
This study was a secondary analysis of 110 videotaped observations of mealtime care interactions among 25 residents with dementia and 29 staff (42 unique dyads) in 9 nursing homes. Staff positive utterances and resident positive and negative utterances (independent variables) and food intake (dependent variable) were coded from the videotaped observations using the Cue Utilization and Engagement in Dementia video coding scheme. A linear mixed model was fit to the data. The two-way interaction effects of food type and video duration with each independent variable as well as two-way interaction effects among the independent variables were tested. Covariates included in the model were the number of years staff worked as a caregiver, and resident age, gender, and eating function.
Results:
The model included three significant interaction effects involving verbal variables: the interaction effect of staff positive utterances with resident positive utterances (p = .030), the interaction effect of staff positive utterances with food type (p = .027), and the interaction effect of resident negative utterances with video duration (p = 0.002). Increased number of intakes of liquid food per minute was associated with increased number of staff positive utterances per minute when residents did not make positive utterances. Decreased number of intakes of solid food per minute was associated with increased number of staff positive utterances per minute, especially when residents made between 0 and 3 positive utterances per minute. As the duration of the videos increased, the number of intakes per minute increased for residents who made one or more negative utterances and decreased for residents who made no negative utterances in the videos. The number of intakes per minute was associated with resident gender in that male residents had increased number of intakes per minute compared with female residents (p = .017), and was not associated with other participant characteristics.
Conclusion:
Intake was associated with dyadic verbal interactions, and such relationship was complex in that it was moderated by food type and video duration. Findings support the significant role of dyadic verbal interactions on intake, and inform the development of effective, tailored mealtime care interventions to promote intake.
Keywords: Behavioral Coding, Dementia, Food Intake, Intake Episodes, Nursing Home, Verbal Interactions, Video
1. Introduction
1.1. Intake of Solid and Liquid Food in Residents with Dementia
Adequate intake of solid and liquid food (intake) is crucial to maintain nutrition and hydration as fundamental health needs for the growing aging population with dementia. In residential care settings, around 68–70% persons with dementia (residents) commonly experience low intake (Thies and Bleiler, 2013, Zimmerman et al., 2014). Approximately 31%–62% of residents have low solid intake (i.e., consumed 75% or less of a meal), and 46–63% have low fluid intake (i.e., consumed 8 ounces of liquid or less per meal) (Lin et al., 2010, Reed et al., 2005). Low intake leads to increased risks of malnutrition and dehydration, which further result in increased confusion, functional decline, infection, weight loss, morbidity, mortality, and decreased quality of life (Hanson et al., 2013, Chang and Roberts, 2011). While cognitive impairment, functional decline, and swallowing difficulty are major risk factors for malnutrition and dehydration, residents with dementia are at a particularly high risk of malnutrition and dehydration compared with cognitively intact residents (Chang and Roberts, 2011, Bell et al., 2015, Guigoz, 2006). Mealtime is a critical component of activities of daily living (ADLs) for residents with dementia to ensure adequate daily intake, as well as an opportunity for staff to engage residents in eating activities and meaningful social conversations both functionally and cognitively. Positively engaging residents in mealtime is associated with improved function and increased chance of intake (Liu et al., 2019, Keller et al., 2017, Liu et al., 2019a, Liu et al., 2017).
1.2. Resident, Staff, and Environment Characteristics that Influence Intake
At the resident level, individuals experience progressive declines in cognition, behaviors, biological and motor function, taste and smell function, and the ability to tolerate the texture of regular food (Droogsma et al., 2015). These declines further lead to poor appetite, changes in dietary habits, mealtime difficulties, lack of alertness, impaired swallowing, decline in oral health and hygiene, and inability to plan and perform complex eating activities, subsequently resulting in functional dependence and inadequate intake (Droogsma et al., 2015, Liu et al., 2016, Cipriani et al., 2016, Chang et al., 2017, Liu et al., 2019). Particularly, meal-time difficulties, defined as the functional, cognitive, and behavioral symptoms that interfere with the process of getting food into the mouth and swallowing it (Cipriani et al., 2016, Aselage and Amella, 2010), occur among 32–87% of residents with dementia (Liu et al., 2016, Chang, 2012) and often result in low intake (Lin et al., 2010, Keller et al., 2017). Additionally, low pace of intake (i.e., number of bites and drinks the resident gets into the mouth within a designated time period (Liu et al., 2019)) is common among residents with dementia, and is associated with insufficient intake (Keller et al., 2017, Namasivayam-MacDonald et al., 2018).
At the staff level, the quality of mealtime assistance is associated with resident functional independence and intake (Abdelhamid et al., 2016, Anderson et al., 2016, Paquet et al., 2008, Liu et al., 2018). Direct care staff provide most mealtime care daily and have most of the opportunities to engage residents in eating. High quality mealtime care with continuous facilitation and engagement from staff, including one-on-one assistance tailored to individual residents using appropriate verbal and nonverbal guidance, is associated with decreased mealtime difficulties and improved intake (Liu et al., 2019, Liu et al., 2019a, Liu et al., 2017). This association is especially obvious for cognitively impaired residents who require physical assistance, have chewing or swallowing difficulties, and eat slowly (takes ≥ 25 minutes for a meal) (Simmons and Schnelle, 2004). However, staff frequently miss the opportunity to positively engage residents, including those who have the potential functional ability to eat by themselves, and tend to provide full assistance for most of the mealtime regardless of residents’ ability and motivation to eat (Liu et al., 2019a, Liu et al., 2018). Such care practice disengages residents from eating, increases dependence on staff, and reinforces residents’ functional decline, which subsequently results in decreased intake (Lin et al., 2010, Keller et al., 2017, Liu et al., 2019a).
At the environmental level, prior work showed inconsistent evidence for improving mealtime difficulties and intake through modifications of the social and physical dining environment (Liu et al., 2014, Bunn et al., 2016, Poscia et al., 2017, Buckinx et al., 2017). Recent research suggests that better quality environmental stimulation, characterized as highly specific stimuli with active dyadic interactions that targets a resident’s needs and preferences, is associated with reduced mealtime difficulties and improved intake (Liu et al., 2019, Liu et al., 2017). Specifically, food is considered the strongest and most specific environmental stimuli for residents during meatlime. The type of food (solid vs. liquid) is associated with intake, in that drinking liquid is more likely to result in intake than eating solid food, especially when continuous engagement is provided to residents by staff (Liu et al., 2019a).
1.3. Assessments of Staff-Resident (Dyadic) Mealtime Interactions
While the importance of dyadic verbal and nonverbal interactions during mealtime care is acknowledged through emerging evidence, little research has examined the role of the positive vs. negative dyadic verbal interactions on intake. Recent research has examined the association of staff verbal, visual, and physical assistance with pace of food intake, and found that pace of food intake was associated with staff visual and physical assistance, but not associated with staff verbal assistance (Liu et al., 2019). This study is limited by the use of dichotomous measures to assess the three types of staff assistance (i.e., whether each type of assistance is provided < 1 time/minute vs. ≥ 1 time/minute) in a small sample of videotaped mealtime observations, and failed to capture the complexity of staff verbal and nonverbal behaviors (Liu et al., 2019). In addition, the study did not examine the role of resident verbal or nonverbal behaviors on food intake (Liu et al., 2019). In the context of dementia mealtime care, it is critical to address the characteristics of the dynamic intake process as well as the complex dyadic interactions in greater detail. The use of computer-assisted behavioral coding scheme to analyze videotaped observations has become an emerging and innovative methodology to assess the complex dynamic mealtime care scenarios, because it allows for repeated viewing and coding of multiple factors, more precise measurement, and deeper levels of analysis that are not achievable with direct on-site observations (Riley and Manias, 2004, Gilmore-Bykovskyi et al., 2015). However, currently available measurements that assess staff and resident mealtime behaviors and dyadic interactions fail to capture the dynamic and interactive nature of the dyadic communication, warrant further psychometric testing, and are mostly developed for direct observations (Reed et al., 2005, Keller et al., 2013, Edahiro et al., 2012, Kline and Sexton, 1996). There are only a few tools developed for videotaped observations, including Feeding Traceline Technique (FLTL) which lacks feasibility (i.e., time and labor intensive) (Phillips and Van Ort, 1993), and a video coding scheme on person-centeredness of care which was used to assess only staff behaviors that are not specific to mealtime care (Gilmore-Bykovskyi et al., 2015).
1.4. The Cue Utilization and Engagement in Dementia (CUED) Mealtime Coding Scheme
To address the gap, the Cue Utilization and Engagement in Dementia (CUED) mealtime coding scheme was refined and validated to assess 1) staff and resident verbal and nonverbal mealtime behaviors, and 2) characteristics of resident intake episodes (Liu et al., 2019b and 2019b). An intake episode is defined as the process of getting one bite of solid food or one drink of liquid food from the plate/tray/cup, putting it into the mouth, and chewing and swallowing it (Liu et al., 2019a). The CUED addresses an inclusive list of verbal and nonverbal behaviors from staff and residents in the context of dementia mealtime care based on multiple established observational tools (Edahiro et al., 2012, Edvardsson et al., 2008, Lann-Wolcott et al., 2011, Aselage, 2010). Our recent work accumulated evidence on the feasibility, ease of use, and inter-rater reliability of CUED using videotaped observations among staff and residents with dementia (Liu et al., 2019a and 2019b). The CUED was initially tested using 18 videotaped mealtime care observations, and shows good inter-rater reliability (r = .80) and feasibility in that 6 hours (mean) are needed to code a one-hour video (video length: coding time needed = 1:6, vs. 1:20 using FTLT). We further refined the CUED by adding more nonverbal behaviors from staff and residents (Liu et al., 2019b) based on three resources: 1) a literature review of resident mealtime difficulties and targeted staff behavioral strategies (Liu, 2019), 2) a review of measures that assess caregiver mealtime care related knowledge, skills, and behaviors as well as measures that assess dyadic mealtime interactions (Liu et al., 2020), and 3) findings from a qualitative study that examined staff’s perspectives of barriers to and facilitators of engaging residents in eating (Liu et al., 2018). We tested the refined CUED using 110 videotaped mealtime observations, and established its feasibility and inter-rater reliability (Liu et al., 2019a and 2019b).
1.5. Objectives
The purpose of this study was to examine the relationship between intake of solid and liquid food (dependent variable) and utterances by staff and residents with dementia (independent variables). It was hypothesized that intake would be significantly associated with positive and negative utterances by staff and residents, after controlling for resident characteristics (i.e., age, gender, and eating function), staff characteristic (i.e., number of years staff worked as a caregiver), and characteristics of videos ((i.e., video duration) and intake episodes (i.e., food type).
2. Methods
2.1. Study Design
In this study, we performed a secondary behavioral coding and analysis of cross-sectional videotaped observations of mealtime care interactions among nursing home (NH) staff and residents with dementia. The parent study, from which the videotaped observations were obtained, was a randomized clinical trial that aimed to examine the effect of a dementia communication staff training program to decrease resistiveness to care among NH residents with dementia (Williams et al., 2016). Ethical approvals were obtained from Institutional Review Boards of the universities where the parent study and this study were conducted.
2.2. Sample and Setting
In the parent study, residents were eligible if they had a diagnosis of dementia, long stay status, staff-reported resistiveness to care, capacity to hear staff communication, and a surrogate decision maker available to provide informed consent. Staff were eligible if they were at least 18 years old, English speaking, a permanent nursing home employee, and provided direct care for a resident participant at least twice a week over the previous month. Morning care interactions that did not require a curtain or door to be closed were recorded to ensure privacy (Williams et al., 2016, Sloane et al., 2007). In total, 127 staff and 83 residents in 13 NHs were enrolled in Kansas.
In this study, videotaped observations were selected from the parent study archived inventory if they were: 1) collected prior to staff training (i.e., under usual care), 2) captured mealtime activities (i.e., eating, drinking), 3) lasted ≥1 minute (to ensure adequate information to capture at least one intake episode), 4) showed interactions between one primary staff and one resident (to minimize the complexity of dyadic interactions and focus on the one-on-one interactions), and 5) had good quality to capture verbal and/or nonverbal behaviors. Videos were excluded if the resident was taking medication rather than eating a meal, was being transferred to or from the dining area, or was present in the dining area but not eating the meal. A total of 1125 baseline videos were screened, among which 974 did not capture mealtime activities and were excluded, leaving 151 videos. Of the 151 videos, 31 lasted < 1 minute and were excluded, leaving 121 videos. Of the 121 videos, 10 videos that involved more than one staff and/or more than one resident and one video that was too dark to have non-verbal behaviors coded were excluded, leaving 110 videos for this study. The 110 videos involved 25 residents and 29 staff (42 unique staff-resident dyads) in 9 NHs.
2.3. The CUED Coding Scheme
The CUED assesses characteristics of intake episodes (Part I11, focus of this study), as well as verbal (Part II, focus of this study) and non-verbal (Part III) behaviors from staff and residents. All the behavioral codes, the operational definitions, and examples of each code were described in detail elsewhere (Liu et al., 2019a and 2019b). In Part I, each intake episode was coded as a state event (an event with starting and ending time points) for four characteristics: 1) the person that initiates and completes the intake episode (i.e., resident, staff), 2) type of food being consumed (i.e., solid, liquid), 3) duration of the intake episode, and 4) outcome of the intake episode (i.e., intake, no intake). Each video may have one or more intake episodes depending on the length of dyadic interactions. In Part II, all verbal behaviors by staff and residents were coded as point events (behaviors were coded as they occurred, and instead of a starting point and an ending point there was only one time point for each behavior). Codes for staff and resident verbal behaviors include two categories: 1) eight positive behaviors (i.e., asking for help/cooperation, assessing for comfort/condition, giving choices, orientation/giving instructions, showing approval/agreement, showing interest, gain attention verbally, unsure-positive), and 2) four negative behaviors (i.e., interrupting/changing topic, verbal refusal/disagreement, controlling voice, unsure-negative).
2.4. Behavioral Coding of Videos
For all the videos, we first coded characteristics of intake episodes (Part I), and then transcribed and coded staff and resident verbal behaviors (Part II). All videotaped observations were coded second-by-second by four trained coders using Noldus Observer® 14.0 (Noldus Information Technology Inc., Leesburg, VA, USA), a software for coding behaviors in a quantitative way and unraveling the sequence of behaviors on a timeline. The coders were trained by the authors (WL and MB) through coding gold standard videos following a standard CUED training and coding manual (Liu et al., 2019a and 2019b). After training, coders coded a couple of randomly selected videos from the sample on their own, and then met as a group with the authors to discuss coding issues and came up with appropriate solutions. Multiple rounds of separate coding and group meetings were done until inter-rater reliability (percent agreement ≥ 85%, and Cohen’s Kappa ≥ 0.80) (McHugh, 2012) was established before trained coders started to code videos independently.
In this study, the CUED demonstrated good feasibility: 2.52 hours (mean) were used to code a one-hour video for characteristics of intake episodes (Part I); and 5.12 hours (mean) and 4.16 hours (mean) were used to transcribe and code staff and resident verbal behaviors in a one-hour video, respectively (Part II). The CUED demonstrates good inter-rater reliability through ratings of randomly selected 22 videos (20% of the 110 videos) across four trained raters (Cohen’s Kappa = .93 − .99, 95% CI = .92−.99, p<.001) (Liu et al., 2019a and 2019b).
3. Measures and Variables
3.1. Participant Characteristics
Data on staff and resident characteristics were collected in the parent study. Staff characteristics included age, gender, race, ethnicity, education, job title, number of years worked as a nursing caregiver, and number of years worked in the study site. Resident characteristics included age, gender, race, ethnicity, dementia stage, comorbidities, and functional ability. Dementia stage was determined by extracting data from the Minimum Data Set (MDS) 3.0 using Functional Assessment Staging in Alzheimer’s Disease (FAST) (Sclan and Reisberg, 1992). The FAST score ranges from 1 (normal cognition and functioning) to 8 (very severe dementia). Resident physical comorbidities were evaluated by extracting data from MDS 3.0 and clinical records using the Modified Cumulative Illness Rating Scale (total score range: 0–70; higher score indicates higher level of physical comorbidities) (Knoefel and Patrick, 2003). Functional ability was extracted from the MDS 3.0 Section G (ADL self-performance and support provided) (Centers for Medicare, and Medicaid Services C 2013). The total score ranges from 0 to 160, with higher score indicating more dependence in self-performance and more support needed.
3.2. Video Duration
Video duration is the length of each videotaped observation (in minutes). In this study, video duration is conceptualized as the period of time during which the dyadic mealtime interactions occurred, because all the video clips that we selected captured the eating and/or drinking activities by the resident who was assisted by one primary care staff. Most videos in the study captured part of the mealtime rather than the whole mealtime.
3.3. Intake of Solid and Liquid Food by Residents
The outcome variable in this study was the number of intake episodes that result in successful intake of solid or liquid food per minute (number of intakes per minute). An indicator variable, food type, was added to the data to identify whether the number of intakes per minute was calculated for solid food or liquid food. The per minute adjustment was used in this study to account for the varied durations of the videos. Thus, the outcome variable was calculated with two values for each video as follows:
The number of intakes of solid food per minute: the total number of intake episodes that result in intake of solid food during the video divided by the video duration.
The number of intakes of liquid food per minute: the total number of intake episodes that result in intake of liquid food during the video divided by the video duration.
3.4. Verbal Behaviors by Staff and Residents
For this study, three variables were created to represent the positive and negative utterances by residents and staff.
The number of positive utterances by staff towards residents per minute was calculated for each video as follows: the total number of positive utterances by staff to the resident during the video was divided by the video duration.
The number of positive utterances by the resident towards staff per minute was calculated for each video as follows: the total number of positive utterances by the resident to the staff during the video was divided by video duration. In this study, there was no recorded positive utterances by the resident in 31.8% of the videos, and in the other 68.2% of the videos, the number of positive resident utterances per minute was skewed to the right. Based on the distribution, a three-category variable was created for each video to represent resident positive utterances: 0 utterance/minute, between 0 and 3 utterances/minute, and 3 or more utterances/minute.
The number of negative utterances by resident towards staff per minute was not calculated because no resident negative utterances were coded in the majority of the 110 videos (68.2%). Based on the distribution, a two-category indicator variable was created for each video to represent resident negative utterances: 0 utterances, and 1 or more utterance (up to 13).
The number of negative utterances by staff towards residents per minute was not used in the analysis, because negative utterances by staff towards residents were very rare in the videos, accounting for 0.01% (n = 16) of all staff utterances (N = 2142). Ninety-seven videos (88.2%) had no negative staff utterance recorded. Among the other 13 videos that had negative staff utterances coded, 10 (9.1%) videos had one negative staff utterance coded, and only three videos (2.7%) had two negative staff utterances coded.
3.5. Resident Eating Function
Resident eating function was conceptualized as the level of resident functional ability to initiate and complete the intake episodes. Resident eating function was operationalily defined as the mean proportion of intake episodes initiated and completed by an individual resident, and was calcuated by dividing the total number of intake episodes initiated and completed by an individual resident by the total number of intake episodes in all the videos that involved the same resident. Based on the distribution of the mean proportion of all intake episodes that were initiated and completed by an individual resident, resident eating function was further categorized into three categories: dependent (0% to 25%), partially (in)dependent (between 25% and 75%), and independent (75% to 100%).
3.6. Data Analysis
All statistical analyses were performed in SAS 9.4 (SAS Institute Inc., 2017). The level of significance alpha = .05 was used. Descriptive statistics were used to summarize characteristics of staff and resident participants, as well as characteristics of the video sample. The linear mixed modeling (LMM) approach was used to examine the association between intake and verbal interactions utilizing the residual maximum likelihood estimation method. This approach accounts for repeated measures (intake was measured twice for each video as intake of solid food and intake of liquid food, indicated by the variable “food type”) and clustering effects within dyads (Cohen et al., 2014). A compound symmetry covariance structure was used to account for the within-video correlation due to repeated measures (food type). Dyads were fit as a random effect to account for correlation due to repeating dyads. The covariance parameter estimate for the random effect of dyads was not statistically significant (p = .302). Residuals were examined graphically to identify violations to normality and homogeneity of variance assumptions, as well as outliers and influential observations (Cohen et al., 2014). In the study sample, no apparent outliers or violations of assumptions were found.
In the LMM model, the independent variable was the number of intakes per minute. Based on the examination of residuals, the number of intakes of liquid and solid food per minute was transformed as follows: 1) a constant 1 was added to each value to eliminate zero intake and 2) the natural log function was applied to the values. The three independent variables were the number of staff positive utterances per minute (a continuous variable), the number of resident positive utterances per minute (categorized as 0, between 0 and 3, and 3 or more), and the indicator for resident negative utterances (0 vs. 1 or more). The two-way interaction effects of food type and video duration with each of the three independent variables were examined, because food type and duration of mealtime dyadic interactions were associated with chance of intake based on our prior work (Liu et al., 2019a), and may impact the relationship between the number of intake and verbal behaviors from staff and residents. The two-way interaction effects among the three independent variables were also tested because the relationship between intake and independent variables may be affected by relationships among staff and resident verbal behaviors. Due to a small sample size, a sequential approach was used to test interaction effects, and only statistically significant interaction effects (p < .05) were included in the model.
Covariates included in the model as fixed effects were the number of years staff worked as a caregiver, and resident age, gender, and eating function. The rationale to adjust for these variables was that these characteristics were associated with intake based on prior work (Liu et al., 2019, Droogsma et al., 2015, Liu et al., 2018) and/or bivariate associations in this study sample. For ease of interpretation, continuous covariates (video duration, years staff worked as a caregiver, and resident age) were centered at the sample means. Video duration was natural log-transformed prior to centering.
4. Results
4.1. Characteristics of Resident and Staff Participants
Table 1 shows the characteristics of resident participants. Residents had a mean age of 84.6 years old (range: 64–96), with the majority being female (60.0%) and non-Hispanic (92.0%). All residents were white. Two-thirds of the residents had moderately severe dementia (FAST score range: 6.0 to less than 7.0) and one-third had severe dementia (FAST score 7.0 or greater). With regard to eating function, 36.0% of residents were independent, 40.0% were partially (in)dependent, and 24.0% were dependent. Residents had moderate levels of comorbidities (range: 19–36) and functional ability in ADL (range: 12–39).
Table 1.
Resident Characteristics (N = 25).
| Variable | M ± SD | Range |
|---|---|---|
| Age, n = 24 | 84.6 ± 8.0 | 64.0 – 96.0 |
| ADL score (0 – 60), n = 23 | 24.2 ± 5.8 | 12.0 – 39.0 |
| Comorbidity score (0 – 70), n = 22 | 26.9 ± 5.5 | 19.0 – 36.0 |
| Variable | N (%) | |
| Gender, n = 25 | ||
| Male | 10 (40.0) | |
| Female | 15 (60.0) | |
| Ethnicity, n = 25 | ||
| Non-Hispanic | 23 (92.0) | |
| Hispanic | 2 (8.0) | |
| FAST, n = 18 | ||
| Moderately severe dementia (6 to less than 7) | 12 (66.7) | |
| Severe dementia (7 or higher) | 6 (33.3) | |
| Eating function (proportion of intake episodes initiated by resident), n = 25 | ||
| Dependent (0 to 25 %) | 6 (24.0) | |
| Partially (in) dependent (between 25% and 75%) | 10 (40.0) | |
| Independent (75% to 100%) | 9 (36.0) |
Table 2 shows the characteristics of staff participants. Staff had a mean age of 34.9 years old (range: 19–79), worked as a caregiver for 8.9 years (mean, range: 0.3–30), and worked in the current NH for 3.7 years (mean, range: 0.1–13). The majority of staff were female (82.8%), white (72.4%), non-Hispanic (79.3%), and had a college degree or were attending college (72.4%) at the time of recruitment. Two staff were RNs (6.9%), the remaining staff (93.1%) were Certified Nursing Assistants (CNAs). Some of the CNAs (34.5%) played additional roles in the current NH (e.g., activity assistant, medication or rehabilitation aide).
Table 2.
Staff Characteristics (N = 29).
| Variable | M ± SD | Range |
|---|---|---|
| Staff age | 34.9 ± 12.3 | 19.0 – 79.0 |
| Years worked as caregiver | 8.9 ± 7.8 | 0.3 – 30.0 |
| Years worked in current facility | 3.7 ± 3.7 | 0.1 – 13.0 |
| Variable | N (%) | |
| Staff gender, n= 29 | ||
| Male | 5 (17.2) | |
| Female | 24 (82.8) | |
| Staff race, n = 29 | ||
| White | 21 (72.4) | |
| African American | 8 (27.6) | |
| Staff ethnicity, n=29 | ||
| Non-Hispanic | 23 (79.3) | |
| Hispanic | 6 (20.7) | |
| Staff education, n=29 | ||
| High school | 8 (27.6) | |
| College | 21 (72.4) | |
| Role | ||
| RN | 2 (6.9%) | |
| Certified Nursing Assistants (CNAs) only | 17 (58.6%) | |
| CNAs plus additional roles (e.g., activity assistant, medication or rehabilitation aide, or LPN) | 10 (34.5%) |
4.2. Characteristics of Videos
Table 3 shows the characteristics of videos. The mean duration of the videos was 4.5 minutes (range: 1–23.8). The mean number of intakes of solid food per minute was 1.3 (range: 0–7.2), and the mean number of intakes of liquid food was 0.9 (range: 0–5.4). Overall, the mean number of intakes of both solid and liquid food was 2.2 per minute (range: 0–7.2). The mean number of positive utterances by staff was 4.7 per minute (range: 0–13.4). There were no positive utterances by residents in almost one third of the videos (31.8%). Residents spoke less than 3 positive utterances per minute in more than half of the videos (52.7%) and 3 or more positive utterances in 15.5% of the videos. There were no negative utterances by residents in two-thirds of the videos (68.2%) and one or more (up to 13) negative utterances in the remaining 31.8% of the videos.
Table 3.
Characteristics of Videos (N = 110).
| Variable | M ± SD | Range |
|---|---|---|
| Successful intakes of solid food/minute | 1.3 ± 1.1 | 0.0 – 7.2 |
| Successful intakes of liquid food/minute | 0.9 ± 0.9 | 0.0 – 5.4 |
| Successful intakes of solid and liquid food/minute | 2.2 ± 1.3 | 0.0 – 7.2 |
| Staff positive utterances/minute | 4.7 ± 3.2 | 0.0 – 13.4 |
| Video duration (minutes) | 4.5 ± 4.0 | 1.0 – 23.8 |
| Variable | N | % |
| Resident positive utterances/minute | ||
| 0 | 35 | 31.8 |
| Between 0 and 3 | 58 | 52.7 |
| 3 or more | 17 | 15.5 |
| Resident negative utterances | ||
| 0 | 75 | 68.2 |
| 1 or more | 35 | 31.8 |
4.3. Intake and Verbal Behaviors by Staff and Residents
The linear mixed model for intake is shown in Table 4. A smaller sample of videos (n = 104) was used to fit the model because five of the original 110 videos had missing data on age for one resident and one video had no staff positive utterance. The remaining 104 videos included 24 residents and 28 staff. Of the 41 dyads in the included videos, 22 dyads (53.7%) were present in one video, 8 dyads (19.5%) were present in two videos, and the remaining 11 dyads (26.8%) were present in 3 to 17 videos.
Table 4.
Linear Mixed Model for Intake per Minute (Natural Log Transformed).
| Variable | b | 95% CI | t | P > |t| | F | P > F |
|---|---|---|---|---|---|---|
| Intercept | 0.766 | [0.494, 1.038] | 5.58 | < .001 | ||
| Staff positive utterances/minute | −0.006 | [−0.054, 0.041] | −0.26 | .793 | 0.57 | .452 |
| Resident positive utterances/minute | 2.13 | .125 | ||||
| Between 0 and 3 vs. 0 | 0.193 | [0.000, 0.386] | 1.99 | .049 | ||
| 3 or more vs. 0 | −0.012 | [−0.522, 0.498] | −0.05 | .963 | ||
| Resident negative utterances (no vs. 1 or more) | −0.029 | [−0.159, 0.101] | −0.45 | .655 | 0.20 | .655 |
| Food type (liquid vs. solid food) | −0.450 | [−0.682, −0.219] | −3.86 | < .001 | 14.91 | < .001 |
| Video duration [ln(minutes)] | 0.111 | [−0.022, 0.244] | 1.65 | .102 | 0.10 | .758 |
| Staff positive utterances/minute * food type (liquid vs. solid food) | 0.046 | [0.005, 0.087] | 2.25 | .027 | 5.05 | .027 |
| Staff positive utterances/minute * resident positive utterances/minute | 3.64 | .030 | ||||
| Between 0 and 3 vs. 0 | −0.060 | [−0.107, 0.014] | −2.56 | .012 | ||
| 3 or more vs. 0 | −0.019 | [−0.085, 0.047] | −0.58 | .564 | ||
| Resident negative utterances (no vs. 1 or more) * video duration [ln(minutes)] | −0.247 | [−0.403, −0.091] | −3.15 | .002 | 9.89 | .002 |
| Years staff worked as a caregiver | −0.001 | [−0.011, 0.009] | −0.17 | .869 | 0.03 | .869 |
| Resident age (years) | −0.007 | [−0.016, 0.001] | −1.85 | .072 | 3.42 | .072 |
| Resident gender (male vs. female) | 0.162 | [0.032, 0.291] | 2.59 | .017 | 6.73 | .017 |
| Resident eating function (proportion of intake episodes initiated by resident) | 1.59 | .227 | ||||
| 0 – 25% vs. 75% – 100% | −0.050 | [−0.212, 0.112] | −0.64 | .530 | ||
| Between 25% and 75% vs. 75% – 100% | 0.079 | [−0.076, 0.233] | 1.04 | .308 |
Note: b = unstandardized regression coefficient estimate; 95% CI = 95% confidence interval; p > |t| = p-values for a t-test of significance of an effect or a level of an effect; p > F = p-values for an F-test of significance of each effect overall. N = 104 videos.
The model included three statistically significant interaction effects involving verbal behaviors: staff positive utterances with resident positive utterances (p = .030), staff positive utterances with food type (p = .027), and resident negative utterances with video duration (p = 0.002). Fig. 1a illustrates the interaction effect between staff positive utterances and resident positive utterances for liquid food (left panel) and solid food (right panel). As seen in the figure, when the number of staff positive utterances per minute was small (i.e., 6 or lower), the differences in intake of both solid and liquid food between residents who made 0, between 0 and 3, and 3 or more positive utterances per minute were small, but the differences amplified as the number of staff positive utterances per minute increased (i.e., 7 or more). Increased number of intakes of liquid food per minute was associated with increased number of staff positive utterances per minute when residents did not make positive utterances. Decreased number of intakes of solid food per minute was associated with increased number of staff positive utterances per minute, especially when residents made between 0 and 3 positive utterances per minute. Thus, the direction and strength of the association between intake and staff positive utterances were dependent on resident positive utterances as well as the type of food.
Fig. 1.
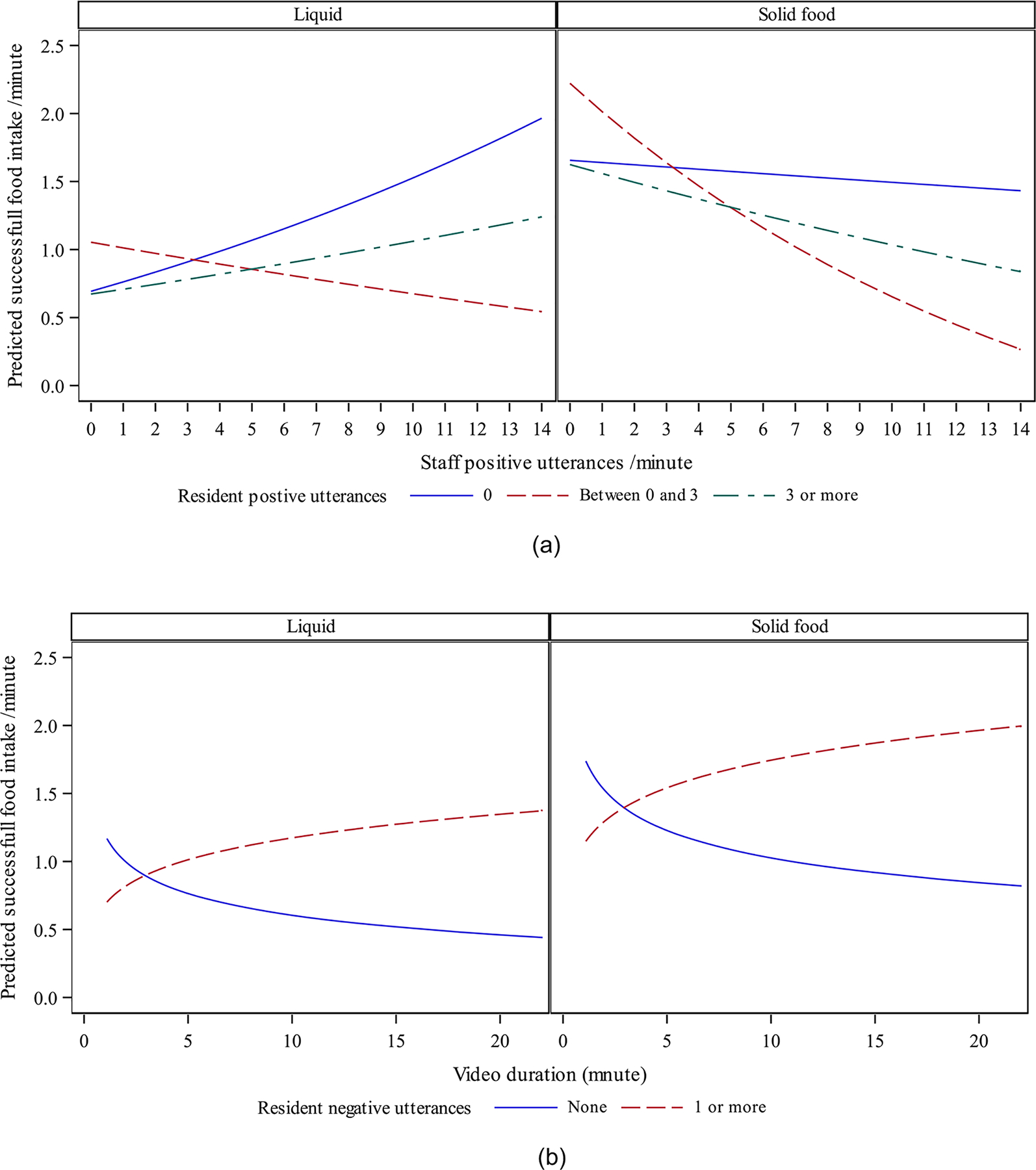
(a) Interaction effects between staff positive utterances and resident positive utterances for liquid food (left panel) and solid food (right panel)
Note. The dependent variable (the number of intakes per minute) was back-transformed to the number of intakes per minute. Resident positive utterances = between 0 and 3, male resident, resident eating function = partially dependent, mean resident age, mean number of years staff worked as a caregiver, mean staff positive utterances.
(b) Interaction effect between resident negative utterances and video duration.
Note. Both the dependent variable (the number of intakes per minute) and video duration were back-transformed to the original scales. Resident negative utterances = 0, male resident, resident eating function = partially dependent, mean resident age, mean number of years staff worked as a caregiver, mean video duration
Fig. 1b illustrates the interaction effect between resident negative utterances and video duration. The differences in the number of intakes of both solid and liquid food between residents who made no negative utterance and those who made one or more negative utterances in the videos were small for shorter videos (i.e., less than 5 minutes), but the differences amplified as video duration increased. For both liquid and solid food, as the duration of the videos increased, the number of intakes per minute increased for residents who made one or more negative utterances and decreased for residents who made no negative utterances in the videos.
The other two-way interaction effects were not statistically significant and were not included in the model: 1) staff positive utterances with resident negative utterances, 2) resident positive utterances with resident negative utterances, 3) staff positive utterances with video duration, 4) resident positive utterances with food type, 5) resident positive utterances with video duration, and 6) resident negative utterances with food type.
With respect to covariates included in the model, only resident gender was statistically significantly associated with the number of intakes per minute in that male residents had more intakes per minute than female residents (p = .017). The number of intakes per minute was not significantly associated with the number of years staff worked as a caregiver (p = .869), resident age (p = .072), or eating function (p = .227).
5. Discussion
This study is the first that examined the role of dyadic verbal interactions on intake of solid and liquid food in NH residents with dementia using the CUED coding scheme. The findings supported the hypothesis that intake was associated with staff and resident verbal behaviors. The relationships between intake and verbal behaviors were moderated by food type and video duration. Further-more, intake was impacted by an interaction effect between staff positive utterances and resident positive utterances. Intake was associated with resident gender and was not associated with staff caregiving length and resident age and eating function. The study adds to prior work in that verbal behaviors from both staff and residents were assessed in greater depth using an innovative and reliable behavioral coding scheme in a larger sample of videotaped mealtime observations.
5.1. Staff and Resident Positive Utterances
In this study, the association between staff positive utterances and intake was impacted by the type of food (i.e., solid vs. liquid) and resident positive utterances. As the number of staff positive utterances per minute increased, there was an increasing trend for the number of intakes of liquid food only for residents who made no positive utterances; there was also a decreasing trend of the number of intakes of solid food, especially when residents made 0–3 positive utterances. This finding was interesting in that staff positive utterances affected intake differently depending on the type of food consumed and the number of resident positive utterances, and these differences amplified as the number of staff positive utterances increased. Compared with solid food, consumption of liquid food generally involves less chewing and swallowing effort from residents, is less likely to be interrupted when residents speak, and takes less time for residents to be ready for the next drink. When staff continuously and positively interacted with residents during mealtime, it was possible that staff positive utterances played a role of ongoing “engagement” when residents made no positive utterances while consuming liquids. On the other hand, staff positive utterances could have played a role of “interruption” when residents consumed solid food, and such influence on intake was more apparent when residents had less than three positive utterances compared with having no positive utterances. This finding may suggest that a large amount of staff positive utterance may not be beneficial when the resident is consuming solid food, especially when the resident is also making positive utterances which interferes the process of chewing and swallowing the food and initiating the next bite.
Prior research has primarily acknowledged the importance of staff engagement on resident intake (Liu et al., 2019, Liu et al., 2019a, Liu et al., 2017, Simmons and Schnelle, 2004, Ullrich and McCutcheon, 2008), but rarely examined how the type of food or frequency of resident positive utterances impacted the relationship between staff positive verbal engagement and intake. Findings of this study in terms of the role of food type were consistent with our recent work that identified the significant role of food type on chance of intake (Liu et al., 2019a). Findings of this study are of interest in that resident positive verbal response towards staff also played an important role on intake. Prior research mostly focuses on the role of staff verbal and/or nonverbal assistance, and seldom examines the role of resident verbal behaviors or dyadic interactions on intake (Liu et al., 2019, Liu et al., 2019a, Liu et al., 2017, Simmons and Schnelle, 2004). This study provides preliminary evidence of the role of resident positive utterances as well as positive dyadic verbal interactions on intake. This study adds to the literature through identifying the role of these characteristics in the relationship of staff positive verbal engagement and intake. Findings of this study confirm the importance of the continuity of staff positive engagement on resident intake and provide directions for the development of effective staff mealtime assistance programs to improve resident intake.
5.2. Resident Negative Utterances
This study found that when the video duration was short (i.e., five minutes or less), the number of intakes per minute was slightly higher for residents who made no negative utterances compared with residents who made one or more negative utterances. For longer videos (i.e., five minutes or longer), the relationship reversed: the intake was higher for residents who made negative utterances. In this study, resident negative utterances were coded when the resident was verbally refusing food or staff assistance, disagreeing with staff, interrupting staff, or changing the topic. It is possible that the resident was delivering a message that he or she had unmet needs or was not satisfied with the assistance or food being provided. This message could inform the staff to modify care assistance approaches, such as reassessing food preferences and providing a different food choice, to meet the resident’s needs, which could possibly increase intake for the resident making negative utterances. Such impact of preference reassessment and care modification on improved intake may not show up when staff has short interactions with residents, and may be more apparent when the staff provides longer and continuous assistance to residents, like that in longer videos. On the other hand, if the resident did not make any negative utterances and was not verbally refusing food or care being provided, the staff may have thought the resident was satisfied with the food or care being provided. Thus, the staff were less likely to identify unmet needs and preferences or to modify care approaches, which resulted in decreased intake over time.
This finding was interesting as it showed a positive impact of resident negative utterances on intake for long staff-resident mealtime interactions. In this context, resident negative utterances should be conceptualized as not just a demonstration of resistiveness to care or aversive feeding behaviors, but a way of communicating unmet needs or preferences by residents which staff should address by modifying the way mealtime care is delivered or the type of food being provided. In interpreting the finding, it is important to notice that resident negative utterance was measured as a dichotomous variable, and the variation of this variable in the study sample was limited. Residents did not make any negative utterance in 68.2% of the videos, and made only one or two negative utterances in 20.9% of the videos and three to 13 negative utterances in the remaining 10.9% of the videos. Future research using valid measures that can assess resident negative verbal behaviors as a continuous variable may be needed to confirm the findings.
5.3. Resident Eating Function
The study showed no association between intake and resident eating function. This finding is inconsistent with prior research that reported better eating performance (i.e., resident functional ability to get food to the mouth and swallow it) was associated with improved intake (Lin et al., 2010, Liu et al., 2019, Keller et al., 2017, Liu et al., 2019a, Namasivayam-MacDonald et al., 2018), when the role of dyadic verbal interactions were not considered. It is possible that the lack of association between resident eating function and intake is due to the inclusion of variables representing dyadic verbal interactions in this study. Another reason may be the way resident eating function was conceptualized and operationalized in this study. Resident eating function was conceptualized as the level of a specific resident’s functional ability to initiate and complete the intake episodes. This variable was operationalized as the mean proportion of intake episodes initiated and completed by each resident across all videotaped mealtime observations that involved that resident, and was further categorized into 3 categories of eating function: dependent, partially (in)dependent, and independent. The purpose was to have a resident-level characteristic (rather than a video-level or a meal-level characteristic) to control for in the model. This was the first time that resident eating function was conceptualized and operationalized in this way in examining the relationship with intake. While the variable may be representative of resident-level eating function, it may not be the best reflection of the resident’s actual eating function in a specific meal and may result in limited variability. Prior research found that there is high variability of eating performance within the resident across meals and days due to physical, cognitive, and behavioral changes (Liu et al., 2018). Future research may need to explore other ways of operationalization in examining the role of resident eating function, such as using multiple-item validated measures to obtain continuous variables with better variability.
5.4. Resident Age and Gender, and Staff Caregiving Length
This study found resident age was not associated with intake, which is consistent with our prior work (Liu et al., 2019, Liu et al., 2019a). This study also found that resident gender was associated with intake and was consistent with prior work, which reported that female gender was associated with lower intake amount (Lin et al., 2010), less chance of intake (Liu et al., 2019a), and lower pace of intake (Liu et al., 2019). Further, staff caregiving length was not associated with intake, which was consistent with prior work (Liu et al., 2019a). Future research may be needed to confirm the findings using a larger and more diverse sample of videotaped mealtime observations in different care settings.
5.5. Implications for practice and research
Despite the increased risks and consequences of mealtime difficulties and inadequate intake, residents are not provided with optimal mealtime care (Liu et al., 2014, Bunn et al., 2016, Poscia et al., 2017). Currently, task-centered care that focuses on completion of eating activities regardless of resident needs and preferences is commonly provided in care practice. Recent systematic reviews show that 1) current mealtime assistance interventions primarily focus on the use of direct feeding skills, rather than positive engagement and interactions, and have low to insufficient evidence to decrease mealtime difficulties and increase intake (Liu et al., 2014, Liu et al., 2015). In comparison, person-centered mealtime care (PCMC) features optimal care through adherence of four key principles: 1) providing choices and acknowledging preferences, 2) supporting independence, 3) showing respect, and 4) promoting social interactions (Liu et al., 2019a, Liu et al., 2017, Liu et al., 2018, Reimer and Keller, 2009). Findings of this study directly support the four principles by demonstrating the significant role of staff positive and continuous verbal interactions with residents on meal intake, as well as addressing residents’ unmet needs and preferences by appropriately interpreting resident verbal refusal or interruptive behaviors. In mealtime care practice, staff are encouraged to engage residents in eating continuously using multiple positive verbal strategies, such as giving instructions, giving choices, getting attention, asking for cooperation, and showing approval. While PCMC is highly recommended for mealtime care, little research has been done to develop and empirically test PCMC-related strategies (Aselage et al., 2015, Keller et al., 2014). Future intervention research is needed in creating effective, person-centered interventions to optimize mealtime care quality and resident intake.
This study is the first that uses an innovative, feasible, and reliable computer-assisted behavioral coding scheme to evaluate the dyadic verbal interactions using videotaped mealtime observations among NH staff and residents with advanced dementia. It is noticeable that the use of CUED and videotaped mealtime observations could be time and labor intensive compared with traditional observational measures. However, the benefits of this approach outweigh the efforts in that it yields more precise and rich data to capture the complexity and dynamics of mealtime care interactions as well as the intake process, and thereby enables more advanced analyses to address certain research objectives. In the next steps of our research plan, the CUED will be used to address three research objectives: 1) characterize the patterns of dyadic nonverbal interactions and examine its association with intake, 2) examine the association between verbal interactions and nonverbal interactions among the dyads, and 3) examine temporal relationships between staff behaviors and resident behaviors, as well as temporal relationships between staff and resident behaviors and resident intake using sequential analysis techniques. Such information will not only provide a better understanding of the characteristics of mealtime dyadic interactions, but also guide the development of effective interventions to improve intake in residents with dementia. In addition, the three parts of CUED can be used altogether or separately as assessment tools to evaluate the effects of dementia mealtime care interventions on staff verbal/nonverbal behaviors, resident verbal/nonverbal behaviors, and resident intake depending on the pre-defined research purposes.
5.6. Limitations
First, the video sample captured part of the mealtime with varied durations and one-on-one interactions, and was collected from a convenience sample of NH staff and residents with dementia who consented to participate in the parent study. Second, the role of staff negative utterances was not examined due to limited amount of data coded from the study sample. Third, while the videos were collected following standard procedures (Williams et al., 2016), including the use of practice recording sessions to minimize Hawthorne effect (Caris-Verhallen et al., 1998), it is possible that staff were aware of the video recording, and were not inter-acting with residents in the same way as they were without the video recording or tended to perform more positively than they usually did. Fourth, data on indication of dysphagia or diet prescriptions, which may impact the relationship between intake and dyadic verbal interactions, were not collected in the parent study. Lastly, intake (the dependent variable) was operationalized as the number of intakes of solid and liquid food per minute due to varied video duration, and essentially measured the pace or speed of intake, rather than amount or likelihood of intake.
5.7. Future Research Directions
Based on the study limitations, it is important to acknowledge five directions for future research in addressing the role of dyadic verbal interactions on intake. First, due to the characteristics of the study sample, findings of this study may not be generalized to observations of the whole meal, more complex dyadic mealtime interactions than one-on-one interactions, NH residents without dementia, or other care settings (assisted living, community home-based settings). Future research may need to use videos that capture the whole meal and/or more complex dyadic interactions (e.g., one-on-two and two-on-one) collected from a larger and more diverse sample of staff and residents in different care settings.
Second, the number of staff negative verbal behaviors was very few in this study. This finding was consistent with a recent report that described cases of staff negative verbal prompts in three NHs during mealtime care of residents with dementia (Palese et al., 2018). While use of negative prompts is less much frequent compared with use of positive prompts by staff, the influence on residents may be significant. Future work needs to examine the role of staff negative behaviors on resident outcomes using data with enough variation.
Third, the limited frequency on staff negative utterances may be due to the limited number of codes on negative verbal behaviors in the CUED, and/or the limited variability of the videotaped observations used in this study. Future work is needed to refine the CUED tool by adding more negative verbal codes appropriate for the context of dementia mealtime care, as well as to collect videotaped mealtime observations that capture more diverse, natural, and real-life dyadic interactions.
Fourth, it is possible that residents with indication of dysphagia and/or special diet prescriptions need to focus on eating when provided with solid food, and staff verbal utterances may be viewed as interruption in this scenario. Future research needs to collect this information and examine the impact on the relationship between dyadic interactions and intake.
Lastly, while appropriate pace of intake is crucial for residents in consideration of the limited designated mealtime period in residential care settings, currently there is no recommended standard for optimal pace or speed of intake. Comparatively, there is more research with regard to the amount of food intake, and low intake has been clearly defined as consumption of less than 75% of the solid and liquid in a meal (Lin et al., 2010, Reed et al., 2005). Future research may need to collect data on the amount of food intake and further examine the role of dyadic verbal interactions.
6. Conclusions
This is the first study that characterized dyadic mealtime verbal interaction using a behavioral coding approach and established its relationship with intake. The relationship is complex in that the direction and strength were dependent on video duration and food type. The findings support the significant role of dyadic verbal interactions on intake, and inform the development of effective, tailored mealtime care interventions to promote intake.
What is already known about the topic?
Nursing home residents with dementia commonly experience mealtime difficulties and insufficient intake, leading to negative nutritional and functional outcomes.
While quality of staff-resident (dyadic) interactions during mealtime is considered an important modifiable factor to manage mealtime difficulties and promote intake, little research has examined the role of the positive vs. negative dyadic verbal interactions on intake.
Several tools exist in assessing dyadic mealtime interactions but have limited feasibility and/or reliability and fail to capture the complexity of dyadic interactions. Therefore, the Cue Utilization and Engagement in Dementia (CUED) mealtime video-coding scheme was refined and validated to assess characteristics of intake process (Part I), and dyadic verbal (Part II) and nonverbal (Part III) mealtime interactions.
What this paper adds
There were significant interaction effects between staff positive utterances and resident positive utterances (p = .030), and between staff positive utterances and food type (p = .027) on intake. Increased number of intakes of liquid food per minute was associated with increased number of staff positive utterances per minute when residents did not make positive utterances. Decreased number of intakes of solid food per minute was associated with increased number of staff positive utterances per minute, especially when residents made between 0 and 3 positive utterances per minute.
There was significant interaction effect between resident negative utterances and video duration (p = 0.002) on intake. As the duration of the videos increased, the number of intakes per minute increased for residents who made one or more negative utterances and decreased for residents who made no negative utterances in the video.
The number of intakes per minute was associated with resident gender in that male residents had increased number of intakes per minute compared with female residents (p = .017), and was not associated with other participant characteristics.
Acknowledgement
The parent study was supported by NIH/NINR grant NR011455-04, Changing Talk to Reduce Resistiveness in Dementia Care (CHAT), K. Williams, PI. ClinicalTrials.gov Identifier: NCT01324219. The sponsor was not involved in study design, data collection and analysis, interpretation of findings, and manuscript preparation. Development of the coding scheme by Melissa Batchelor-Murphy was supported by the National Hartford Centers for Gerontological Nursing Excellence Claire M. Fagin Fellow and Robert Wood Johnson Foundation Nurses Faculty Scholar programs [NCT01780402] and NIH/ NINR [NCT02269956]. The authors acknowledge the assistance from research assistants for coding the videos, and keeping coding logs and time logs in this study.
Funding support
This study was supported by NIH/NIA grant 1R03AG063170-01, and American Nurses Foundation Nursing Research Grant (PI: Wen Liu, Co-Is: Melissa Batchelor and Kristine Williams). The sponsors were not involved in study design, data collection and analysis, interpretation of findings, and manuscript preparation.
Footnotes
Author statement
The work described has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
Conflict of interest
None.
References
- Abdelhamid A, Bunn D, Copley M, et al. , 2016. Effectiveness of interventions to directly support food and drink intake in people with dementia: systematic review and meta-analysis. BMC geriatrics 16 (1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K, Bird M, MacPherson S, et al. , 2016. How do staff influence the quality of long-term dementia care and the lives of residents? A systematic review of the evidence. International Psychogeriatrics 28 (8), 1263–1281. [DOI] [PubMed] [Google Scholar]
- Aselage MB., 2010. Measuring mealtime difficulties: eating, feeding and meal behaviours in older adults with dementia. Journal of Clinical Nursing 19 (5–6), 621–631. [DOI] [PubMed] [Google Scholar]
- Aselage MB, Amella EJ, 2010. An evolutionary analysis of mealtime difficulties in older adults with dementia. Journal of Clinical Nursing 19 (1–2), 33–41. [DOI] [PubMed] [Google Scholar]
- Aselage MB, Amella EJ, Rose SB, et al. , 2015. Dementia-Related Mealtime Difficulties: Assessment and Management in the Long-Term Care Setting Handbook of Clinical Nutrition and Aging. Springer, New York, pp. 287–301. [Google Scholar]
- Bell CL, Lee AS, Tamura BK, 2015. Malnutrition in the nursing home. Current Opinion in Clinical Nutrition & Metabolic Care 18 (1), 17–23. [DOI] [PubMed] [Google Scholar]
- Buckinx F, Morelle A, Bruyère O, 2017. Influence of environmental factors on food intake among nursing home residents: a survey combined with a video approach. Clinical Interventions in Aging 12, 1055–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunn DK, Abdelhamid A, Copley M, et al. , 2016. Effectiveness of interventions to indirectly support food and drink intake in people with dementia: Eating and Drinking Well IN dementiA (EDWINA) systematic review. BMC geriatrics 16 (1), 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caris-Verhallen WM, Kerkstra A, van der Heijden PG, et al. , 1998. Nurse-elderly patient communication in home care and institutional care: an explorative study. International journal of nursing studies 35 (1), 95–108. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services C. MDS 3.0 QM User’s Manual V8.0 (v8.0 04-15-2013). http://www.cmsgov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-30-QM-User%E2%80%99s-Manual-V80pdf 2013.
- Chang CC, Roberts BL, 2011. Malnutrition and feeding difficulty in Taiwanese older with dementia. Journal of Clinical Nursing 20 (15–16), 2153–2161. [DOI] [PubMed] [Google Scholar]
- Chang C-C, Lin Y-F, Chiu C-H, et al. , 2017. Prevalence and factors associated with food intake difficulties among residents with dementia. PloS one 12 (2), e0171770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C-C, 2012. Prevalence and factors associated with feeding difficulty in institutionalized elderly with dementia in Taiwan. The journal of nutrition, health & aging 16 (3), 258–261. [DOI] [PubMed] [Google Scholar]
- Cipriani G, Carlesi C, Lucetti C, et al. , 2016. Eating Behaviors and Dietary Changes in Patients With Dementia. American Journal of Alzheimer’s Disease & Other Dementias® 31 (8), 706–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P, West SG, Aiken LS, 2014. Applied multiple regression/correlation analysis for the behavioral sciences. Psychology Press. [Google Scholar]
- Droogsma E, van Asselt D, De Deyn PP, 2015. Weight loss and undernutrition in community-dwelling patients with Alzheimer’s dementia: From population based studies to clinical management. Zeitschrift fur Gerontologie und Geriatrie 48 (4), 318–324. [DOI] [PubMed] [Google Scholar]
- Edahiro A, Hirano H, Yamada R, et al. , 2012. Factors affecting independence in eating among elderly with Alzheimer’s disease. Geriatrics & Gerontology International 12 (3), 481–490. [DOI] [PubMed] [Google Scholar]
- Edvardsson D, Winblad B, Sandman P-O, 2008. Person-centred care of people with severe Alzheimer’s disease: current status and ways forward. The Lancet Neurology 7 (4), 362–367. [DOI] [PubMed] [Google Scholar]
- Gilmore-Bykovskyi AL, Roberts TJ, Bowers BJ, et al. , 2015. Caregiver Person-Centeredness and Behavioral Symptoms in Nursing Home Residents with Dementia: A Timed-Event Sequential Analysis. Gerontologist 55 (Supplement), s61–s66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guigoz Y, 2006. The Mini Nutritional Assessment (MNA) review of the literature–What does it tell us? The Journal of nutrition, health aging 10 (6), 466–485. [PubMed] [Google Scholar]
- Hanson LC, Ersek M, Lin FC, et al. , 2013. Outcomes of feeding problems in advanced dementia in a nursing home population. Journal of the American Geriatrics Society 61 (10), 1692–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller HH, Laurie CB, McLeod J, et al. , 2013. Development and reliability of the mealtime social interaction measure for long-term care (MSILTC). Journal of Applied Gerontology 32 (6), 687–707. [DOI] [PubMed] [Google Scholar]
- Keller HH, Carrier N, Duizer L, et al. , 2014. Making the most of mealtimes (m3): grounding mealtime interventions with a conceptual model. Journal of the American Medical Directors Association 15 (3), 158–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller HH, Carrier N, Slaughter SE, et al. , 2017. Prevalence and Determinants of Poor Food Intake of Residents Living in Long-Term Care. Journal of the American Medical Directors Association 18 (11), 941–947. [DOI] [PubMed] [Google Scholar]
- Kline N, Sexton DL, 1996. Eating behaviors of nursing home residents who display agitation. Nursing management 27 (9), 32JJ. [DOI] [PubMed] [Google Scholar]
- Knoefel FD, Patrick L, 2003. Improving outcomes in geriatric rehabilitation: The impact of reducing cumulative illness. Geriatrics Today 6, 153–157. [Google Scholar]
- Lann-Wolcott H, Medvene LJ, Williams K, 2011. Measuring the person-centered-ness of caregivers working with nursing home residents with dementia. Behavior therapy 42 (1), 89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LC, Watson R, Wu S, 2010. What is associated with low food intake in older people with dementia? Journal of Clinical Nursing 19 (1–2), 53–59. [DOI] [PubMed] [Google Scholar]
- Liu W, Cheon J, Thomas SA, 2014. Interventions on mealtime difficulties in older adults with dementia: A systematic review. International journal of nursing studies 51 (1), 14–27. [DOI] [PubMed] [Google Scholar]
- Liu W, Galik E, Boltz M, et al. , 2015. Optimizing Eating Performance for Older Adults with Dementia Living in Long-term Care: A Systematic Review. World-views on Evidence-Based Nursing 12 (4), 228–235. [DOI] [PubMed] [Google Scholar]
- Liu W, Galik E, Boltz M, et al. , 2016. Factors associated with eating performance for long-term care residents with moderate-to-severe cognitive impairment. Journal of Advanced Nursing 72 (2), 348–360. [DOI] [PubMed] [Google Scholar]
- Liu W, Jao YL, Williams KN, 2017. The association of eating performance and environmental stimulation among older adults with dementia in nursing homes: A secondary analysis. International Journal of Nursing Studies 71, 70–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Jao YL, Williams KN, 2019. Factors Influencing the Pace of Food Intake for Nursing Home Residents with Dementia: Resident Characteristics, Staff Mealtime Assistance and Environmental Stimulation. Nursing open 0 (0), 1–11. doi: 10.1002/nop1002.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Tripp-Reimer T, Williams KN, Shaw C, 2018. Facilitators and barriers to optimizing eating performance among cognitively impaired older adults: A qualitative study of nursing assistants’ perspectives. Dementia. [DOI] [PubMed] [Google Scholar]
- Liu W, Williams KN, Batchelor-Murphy M, et al. , 2019a. Eating Performance in Relation to Food and Fluid Intake in Nursing Home Residents with Dementia: a Secondary Behavioral Analysis of Mealtime Videos. International journal of nursing studies 96, 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Shaw C, Chen X, 2019. Dental-related Function and Oral Health in Relation to Eating Performance in Assisted Living Residents With and Without Cognitive Impairment. Special Care in Dentistry 39 (5), 497–504. doi: 10.1111/scd.12405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Batchelor-Murphy M, Williams KN, 2019b. Feasibility, Ease of Use, and Inter-rater Reliability of the Cue Utilization and Engagement in Dementia Mealtime Video-coding Scheme. Presented as a paper at Midwest Nursing Research Society (MNRS) 43rd Annual Research Conference Kansas City, KS, USA. [Google Scholar]
- Liu W, Kim S, Alessio H, 2020. Measuring Caregivers’ Knowledge, Attitude, and Behaviors During Mealtime Care of Persons With Dementia: A Systematic Review of instruments. Presented as a poster at Midwest Nursing Research Society (MNRS) 44th Annual Research Conference (Virtual) Schaumburg, IL, USA. [Google Scholar]
- McHugh ML, 2012. Interrater reliability: the kappa statistic. Biochemia medica: Biochemia medica 22 (3), 276–282. [PMC free article] [PubMed] [Google Scholar]
- Namasivayam-MacDonald AM, Slaughter SE, Morrison J, et al. , 2018. Inadequate fluid intake in long term care residents: prevalence and determinants. Geriatric Nursing 39 (3), 330–335. [DOI] [PubMed] [Google Scholar]
- Palese A, Gonella S, Kasa T, et al. Negative prompts aimed at maintaining eating independence in nursing home residents: purposes and implications-A critical analysis. 2018. [DOI] [PubMed]
- Paquet C, St-Arnaud-McKenzie D, Ma Z, et al. , 2008. More than just not being alone: the number, nature, and complementarity of meal-time social interactions influence food intake in hospitalized elderly patients. The Gerontologist 48 (5), 603–611. [DOI] [PubMed] [Google Scholar]
- Phillips LR, Van Ort S, 1993. Measurement of mealtime interactions among persons with dementing disorders. J Nurs Meas 1 (1), 41–55 15p. [PubMed] [Google Scholar]
- Poscia A, Milovanovic S, La Milia DI, et al. , 2017. Effectiveness of nutritional interventions addressed to elderly persons: umbrella systematic review with meta-analysis. European journal of public health 28 (2), 275–283. [DOI] [PubMed] [Google Scholar]
- Rediehs M, Liu W, 2019. Mealtime Difficulties and Targeted Non-Pharmacological Interventions for Individuals with Dementia: A Systematic Review. Presented as a student competitive poster at MNRS 43rd Annual Research Conference Kansas City, KS, USA. [Google Scholar]
- Reed PS, Zimmerman S, Sloane PD, et al. , 2005. Characteristics associated with low food and fluid intake in long-term care residents with dementia. The Gerontologist 45 (suppl 1), 74–81. [DOI] [PubMed] [Google Scholar]
- Reimer HD, Keller HH, 2009. Mealtimes in nursing homes: striving for person–centered care. Journal of Nutrition for the Elderly 28 (4), 327–347. [DOI] [PubMed] [Google Scholar]
- Riley RG, Manias E, 2004. The uses of photography in clinical nursing practice and research: a literature review. Journal of advanced nursing 48 (4), 397–405. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc., 2017. SAS 9.4 Language Reference: Concepts, Sixth Edition SAS Institute Inc., Cary, NC. [Google Scholar]
- Sclan SG, Reisberg B, 1992. Functional assessment staging (FAST) in Alzheimer’s disease: Reliability, validity, and ordinality. International Psychogeriatrics 4 (Supplement 1), 55–69. [DOI] [PubMed] [Google Scholar]
- Simmons SF, Schnelle JF, 2004. Individualized feeding assistance care for nursing home residents: Staffing requirements to implement two interventions. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 59 (9), M966–M973. [DOI] [PubMed] [Google Scholar]
- Sloane PD, Miller LL, Mitchell CM, et al. , 2007. Provision of morning care to nursing home residents with dementia: opportunity for improvement? American journal of Alzheimer’s disease and other dementias 22 (5), 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thies W, Bleiler L, 2013. Alzheimer’s Disease Facts and Figures. Alzheimer’s & Dementia: the Journal of the Alzheimer’s Association 9 (2), 208–245. [DOI] [PubMed] [Google Scholar]
- Ullrich S, McCutcheon H, 2008. Nursing Practice and Oral Fluid Intake of Older People with Dementia. Journal of Clinical Nursing 17 (21), 2910–2919. [DOI] [PubMed] [Google Scholar]
- Williams KN, Perkhounkova Y, Herman R, et al. , 2016. A Communication Intervention to Reduce Resistiveness in Dementia Care: A Cluster Randomized Controlled Trial. The Gerontologist 57 (4), 707–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman S, Sloane PD, Reed D, 2014. Dementia Prevalence and Care in Assisted Living. Health Affairs 33 (4), 658–666. [DOI] [PubMed] [Google Scholar]


