Abstract
Aim:
This study aimed to evaluate a protocol using post thyroidectomy parathyroid hormone (PTH) levels on the day after surgery to facilitate early discharge of patients.
Methods:
This prospective observational study was done in Christian Medical College, India over 1 year with 125 consecutive patients who had serum PTH and calcium values measured in the morning following thyroidectomy/first postoperative day (D1). Patients with no symptoms and signs of hypocalcemia and with serum calcium ≥8 mg/dL and PTH ≥6 pg/ml according to the protocol were discharged without supplements on D1. Patients were followed up and tested for a week after surgery in the outpatient clinic to assess hypocalcemia and readmission rates.
Results:
Seventy five patients (60%) could be discharged early on D1without calcium supplementation; only one patient had mild hypocalcemia symptoms managed with oral calcium supplements during outpatient follow-up within 1 week and none who followed the protocol required readmission. Temporary biochemical hypocalcemia was encountered in 36 patients (28.8%) including symptomatic hypocalcemia in 13 patients (10.4%). Among the 36 patients with hypocalcemia, 26 patients (72.2%) had a PTH level <6 pg/ml. Three patients required intravenous calcium infusion to correct hypocalcemia. Sensitivity, specificity and positive predictive value, and ROC of PTH 6 pg/ml in predicting hypocalcemia were 70.5%, 94.5% and 83.3%, 0.86, respectively. The low PTH could also guide early supplementation of calcium and all the severe hypocalcemia patients had PTH lower than the cut off of 6 pg/ml.
Conclusion:
A PTH and calcium-based protocol can be effectively used for early discharge of thyroidectomy patients the day after surgery without calcium supplementation. The compliance of the patient for early discharge was good.
Keywords: Hypocalcemia, parathyroid hormone, total thyroidectomy
INTRODUCTION
Total thyroidectomy is a commonly performed surgical procedure for various benign and malignant thyroid diseases and much progress has been achieved in ensuring a safe technique and early discharge from hospital.[1] Temporary hypocalcemia remains the commonest complication encountered, the median rate reported in a meta-analysis being 27%[2] and it is the main limiting factor for early discharge because a few patients may require intravenous calcium therapy for hypocalcemia thereby requiring prolonged inpatient care. Carefully selected patients can often be discharged on the day of surgery (day case protocol) or on the day after surgery (short-stay protocol). In low–middle-income countries like India where insurance and costs do not drive same day discharge and return to hospital mechanisms are inefficient, the day after surgery may be optimal for discharge allowing pain, nausea and vomiting to settle and most bleeding complications to be managed in the hospital. The reported sensitivity of a low PTH as a predictor of hypocalcemia in various studies with the cut-off levels of 6-24 pg/ml, ranged from 59%-100%; the time of measurement varied from intra-operative, same day to next day.[3,4,5,6,7,8,9,10,11] In a recent prospective study[12] done at our institution, post-operative Day 1(the day after surgery) PTH was found to have good sensitivity and specificity at the cut-off range of 6.1–8 pg/ml; hence, the cut-off of 6 pg/ml was derived for our study.[12] It is likely that factors other than hypoparathyroidism which may influence calcium in the immediate postoperative state are hypothermia, calcitonin release and the vasoactive peptide, such as Endothelin 1, but these factors have not been studied adequately because of low therapeutic potential. We, therefore, considered both PTH and calcium values in our protocol when discharging patients and prescribing calcium supplements.[3,4,5,6,7,8,9,10,11] Prophylactic supplementation of oral calcium and vitamin D can facilitate short-stay surgery[13,14,15,16,17,18,19,20] but the supplements would be unnecessary for patients not developing hypocalcemia; it exposes them to complications of hypercalcemia and the burden of additional costs of the supplements. The optimal duration of supplementation is also unknown. We hypothesized that calcium supplementation can be safely avoided in the patients with sufficient PTH and calcium and supplementation guided by a graded protocol.
METHODS
Study design
This prospective observational study was done at Christian Medical College hospital, Vellore, a tertiary referral centre, over 1 year (July 2014-July 2015). Sample size: A difference of 25% in hypocalcemia rate between low PTH and high PTH using a two-side Z test of the difference between proportions with 80% power and 5% significance level was used to calculate a sample size of 125 patients. The calculation is based on our previous study.[12] Aim and objectives: The aim of the study was to evaluate a protocol using post thyroidectomy parathyroid hormone (PTH) and calcium levels on the day after surgery to facilitate early discharge of patients. The objectives were to apply an early discharge protocol for post thyroidectomy patients based on PTH at the cut-off value of 6 pg/ml and calcium and to analyze patient compliance with the early discharge protocol. Participants: All the patients who underwent total thyroidectomy or completion thyroidectomy and willing for early discharge were included in the study. Exclusion criteria: Patients with goiter more than 6 cm, locally advanced thyroid malignancy, retrosternal extension and hyperthyroidism were excluded. The study was approved by the institutional review board. Patients underwent preoperative counselling and were consented for the study. Intraoperative findings of some parathyroids seen, saved or auto-transplanted were noted. Patients were monitored for complications after surgery such as hemorrhage, voice change and clinical features of hypocalcemia. Samples for total serum calcium, albumin and PTH were sent by 6 am on the day after surgery irrespective of the time of procedure. Serum iPTH was estimated by chemiluminescence using the Advia centaur centre (Siemens). Biochemical hypocalcemia was defined as corrected total serum calcium <8 mg/dl and was considered temporary if it occurred in the immediate postoperative period of 1 week and recovered with oral supplements of calcium and vitamin D.
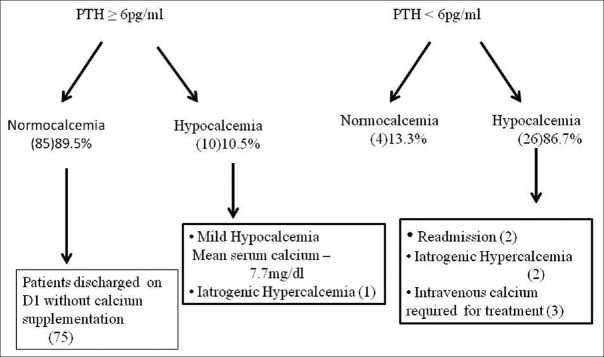
Serum magnesium was monitored if hypocalcemia was severe or resistant to calcium and vitamin D therapy and the patients were supplemented with intravenous magnesium sulphate if they had hypomagnesemia. The protocol that was followed is shown in Figure 1. At discharge, patients were explained about the symptoms and signs of hypocalcemia and hemorrhage which they might develop, contact telephone numbers and 24-hour emergency access were provided to gain the confidence of the patients; this is of paramount importance in implementing a short-stay protocol.
Figure 1.
Discharge protocol followed
The protocol used for calcium and vitamin D supplementation during the inpatient period.
Patients with PTH <6 pg/ml irrespective of serum calcium levels were routinely supplemented with oral calcium and vitamin D therapy in the form of tablet calcium carbonate given 1 gm thrice daily and calcitriol 0.5 mcg twice daily to avoid the development of hypocalcemia. These patients were monitored with serum calcium levels on day 2 and discharged if normocalcemic. For patients with PTH ≥6 pg/ml and hypocalcemia, the dose of supplementation was based on their severity as shown in Table 1.
Table 1.
Protocol used for management of patients with hypocalcemia
| S.calcium (mg/dl) | Sign (Chvostek) | Symptoms | Treatment |
|---|---|---|---|
| <8.0 | No/mild grade 1 | No | T. CaCO3 1 gm BD |
| <8.0 | Grade 2/3 | No/mild | T. CaCO3 1 gm TID and T. Calcitriol 0.25 mcg OD |
| < or ≥8 | Yes/No | Severe | T. CaCO3 1 gm TID and T. Calcitriol 0.5 mcg BD increased accordingly to maximum of T.CaCO3 4 gm and T. Calcitriol 1 mcg per day |
If symptoms were severe in addition to above, infusion of 50 ml of 10% calcium gluconate in 500 ml of 5% dextrose over 12 h continued till asymptomatic and normocalcemia achieved. For spontaneous visible spasm intravenous calcium gluconate bolus 10 ml diluted with 10 ml saline given over 10 min and repeated till spasm resolved. For persistent hypocalcemia, serum magnesium checked and hypomagnesaemia if present corrected. T. CaCO3 - Tablet calcium carbonate
Follow-up
Patients discharged early were followed up in the outpatient department on postoperative days 3 and 7, checked for clinical and biochemical hypocalcemia and managed accordingly. Patients discharged with supplements of calcium and vitamin D were monitored with serum calcium and if the hypocalcemia improved, the oral calcium and vitamin D tablets were tapered and stopped in 2 months. The study did not aim to detect permanent hypoparathyroidism at 6 months.
Statistical method used
The descriptive statistics were performed using mean with standard deviation or frequency with percentages. The relationship between PTH and hypocalcemia, various factors affecting discharge, treatment protocol and presence of hypocalcemia are all analyzed using two sample t-test, Chi-square test, and proportion. A significant association was defined with a P value of less than 0.05. The accuracy of PTH as a diagnostic test was evaluated using the ROC, sensitivity and specificity.
RESULTS
Patient demography and tumor characteristics
The mean age in the study group of 125 patients was 38.6 years ranging from 17 to 68 years. The most common (35.2%) age group was 31-40 years. The gender distribution was predominantly female with male-female ratio 1:10.4. The mean size of the goiter was 3.5 cm ranging from 1 to 6 cm. Total thyroidectomy was the commonest procedure done in 119 patients (95.2%), with only 6 patients (4.8%) undergoing completion thyroidectomy. Final histopathological report for more than half of the patients (55.2%) was papillary carcinoma, 32.8% had nodular hyperplasia and only 5.6% and 0.8% had thyroiditis and follicular adenoma, respectively.
Hypocalcemia
Postoperative temporary biochemical hypocalcemia was encountered in 36 patients (28.8%). Of them, 13 patients (36.1%) were symptomatic, forming 10.4% of the total group. None of the normocalcemic patients developed symptoms. Biochemical hypocalcemia was diagnosed on the first day after surgery among 75% of patients with hypocalcemia, on the second day in 19.4%, and 5.6% during follow up on day 3 and day 5 after discharge, one of them belongs to the early discharge group.
Autotransplantation of parathyroid was performed in 16 out of 119 (13.4%) total thyroidectomy patients. The hypocalcemia rate in autotransplanted patients was 7 out of 16 (43.8%) was not significantly greater (P = 0.18) than the not autotransplantated group 28 out of 103 (27.2%).
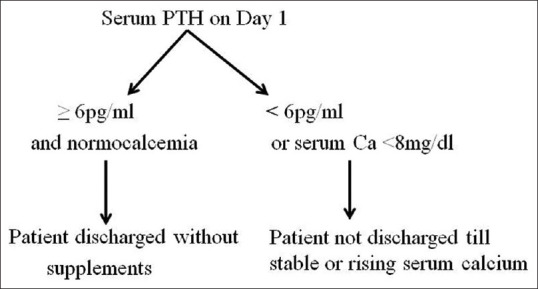
The mean PTH value in the study group was 27.9 pg/ml. A PTH level ≥6 pg/ml was noted in 95 patients (76%); the majority of these patients (89.5%) were normocalcemic. Although hypocalcemia was seen in ten patients (10.5%) in this group with PTH level ≥6 pg/ml, it was mild with the mean and median calcium values in this group at 7.7 and 7.8 mg/dl. Only three patients had symptoms that were mild and transient and none of the ten required readmission. Among 30 patients with low PTH (<6 pg/ml), 86.7% had hypocalcemia. The PTH level was found to be significant (P < 0.001) in differentiating normocalcemia and hypocalcemia. Sensitivity, specificity and positive predictive value of PTH 6 pg/ml in predicting hypocalcemia was 70.5%, 94.5% and 83.3% (CI 65.3%-94.4%) [Table 2]. The area under the receiver operator curve (ROC) was 0.86, indicating PTH is a reliable test for differentiating hypocalcemia and normocalcemia.
Table 2.
Sensitivity and specificity for various PTH cut off
| PTH Value pg/ml | Sensitivity | Specificity |
|---|---|---|
| <1.5 | 2.9% | 100% |
| <6 | 70.5% | 94.5% |
| <9.8 | 79.4% | 92.3% |
| <15 | 79.4% | 79.2% |
| <21 | 85.2% | 70.3% |
Treatment of hypocalcemia
Oral calcium and vitamin D supplements were sufficient to manage 33 (91.7%) out of 36 hypocalcemia patients. Three patients required intravenous calcium infusion to correct hypocalcemia. All these three patients had very low PTH <1.5 pg/ml and concomitant hypomagnesaemia, which was corrected intravenously over 2 days.
Early discharge of patients and their compliance
Eighty five patients were eligible for early discharge and we achieved early discharge on day 1 in 75 (88.2%). The reason for the delayed discharge of 10 eligible patients was due to the presence of a drain tube in five and postoperative hemorrhage in one patient; these six were kept longer for observation. Only four patients requested a longer stay due to inability to arrange for local transfer. Thus the compliance of the patients to the protocol was 95.3% (81 out of 85 eligible patients were willing), but practically feasible in 88.2%.
Follow up of discharged patients
There were no readmissions, telephonic contact or emergency room visits in the early discharged group of 75 patients. One reported mild symptoms of hypocalcemia starting on day 4 post surgery, with a calcium level of 7.1 mg/dl and was managed with oral supplements. The serum PTH and calcium at discharge were 23 pg/ml and 8.3 mg/dl.
Iatrogenic hypercalcemia
Forty patients received supplementation in the study group which included 36 patients with hypocalcemia and four patients with normocalcemia but PTH <6 pg/ml. Three patients developed hypercalcemia in the first week, with values of 10.5, 11.1, 11.6 mg/dl, but none was symptomatic.
Complications of surgery and readmissions in the study
Among the study group of 125 patients, two patients were readmitted with hypocalcemic symptoms; both had PTH <1.5 pg/ml. One was non-compliant in taking the prescribed calcium supplements and the other had requested discharge despite hypocalcemia in a breach of protocol. Other complications were unilateral recurrent laryngeal nerve palsy in two and postoperative hemorrhage also in two patients.
The PTH and calcium in the study patients with their management and follow-up are summarized in Figure 2.
Figure 2.
Management and follow-up of patients according to serum PTH
DISCUSSION
Hypocalcemia
The temporary hypocalcemia rate in the study was 28.8%, the patients symptomatic for hypocalcemia was 10.4% in our group. In a meta-analysis that studied the predictive factors of hypocalcemia, the transient hypocalcemia rate across various studies ranged from 19% to 38% with a median of 27%.[2] Onset of hypocalcemia commonly ranges from 9 to 75 hours as suggested by studies by SperlonganoP et al. and Lee YS et al.[21,22] The majority (75%) of patients with hypocalcemia were diagnosed on the first postoperative day in our study. However, we did not monitor serial calcium levels on all postoperative days; only selected patients in our study underwent calcium evaluation on the second day or on follow-up as outpatients as per protocol.
The risk of temporary hypocalcemia after autotransplantation of parathyroid is variable in literature with some showing increased risk[23,24] and others not,[25,26] however, the risk of permanent hypocalcemia is not increased.[20] In our study, a statistically significant association of temporary hypocalcemia with autotransplantation was not present.
PTH as a predictor of hypocalcemia
Serial measurements of calcium and the trend in their postoperative values were scrutinized to allow early discharge until 1988 when Nussbaum et al. popularized the rapid intact PTH assay.[27] Serum PTH with its short half-life of just 5-6 minutes can depict the changes following parathyroid injury early.
PTH was shown in various studies as a good predictor of hypocalcemia at different cut-off values (3-20 pg/ml) and timing of PTH measured (intraoperative to 24 hours post surgery.[7,28,29,30,31] Hence, the cut-off value and the timing of PTH measurement needs to be institutionalized. In our study PTH <6 pg/ml measured in the morning after surgery had sensitivity and specificity of 70.5% and 94.5% for predicting hypocalcemia which is comparable to a large (458 patients) multicenter study was done in Australia (sensitivity 70.7% and specificity 92.6%).[32] However, single value of PTH ≤8 pg/ml with the highest sensitivity of 100% and PTH ≤10 pg/ml with 94% sensitivity and 100% specificity are also reported.[5,33]
PTH as a guide for supplementation and early discharge
Published protocols have used PTH level as a guide for calcium supplementation[3] or a guide for early discharge[10] or both.[7,30,34] Sabour S et al.[3] reported hypocalcemia in 35% of patients in the control group in whom treatment of hypocalcemia was based on serum calcium value, 14% in the group in whom calcium supplementation was based on PTH and calcium value and 4.5% in routinely supplemented group. Grodski S et al.[10] from Australia routinely supplemented all patients but used PTH >10pg/ml as a guide for discharge on the first postoperative day. Three other studies listed in Table 3, used a similar PTH-based protocol, discharging the majority of patients without calcium supplementation.[7,30,34]
Table 3.
Studies with patients discharged based on PTH without calcium supplementation
| Study | PTH sample time and cut off | Discharged without supplementation if | Follow up of discharged patients |
|---|---|---|---|
| Chow et al.[34]China | Day 1, 6pg/ml | PTH >6pg/ml and normocalcemia | No readmission Hypocalcemia not mentioned |
| Cayo et al.[7] Wisconsin | Day 1, 10 pg/ml | PTH >10pg/ml and normocalcemia | No readmission No hypocalcemia |
| Cote V et al.[30]Canada | 1 hr, 15 pg/ml | PTH>15pg/ml and normocalcemia | Readmission and hypocalcemia not recorded |
Compliance with the protocol
We were satisfied to note a 95.3% willingness to comply with our protocol, though the practical discharge rate was 88.2% owing to other complications and logistics. There is no data for comparison in an Indian setting. An Italian study, assessing the safety of 1-day thyroid surgery in 1571 patients, had excellent compliance and patient satisfaction rates, with only three patients staying more than 1 day due to the lack of accompanying person for early discharge.[35]
Complications of surgery and readmissions
Other complications like hemorrhage (1.6%), recurrent laryngeal nerve injury (0.8%) and readmission (1.6%) rates of the study group were similar to that quoted in literature.[36,37,38,39,40]
Iatrogenic hypercalcemia
Hypercalcemia which is possible in the patients supplemented with oral calcium and vitamin D is infrequently reported in the literature. We had three patients in the group with hypercalcemia, a report of 5% have been reported by Sabour S et al.[3] Although the hypercalcemia rate is similar to the mentioned study,[3] our study points out the benefit that can be achieved by the select group of patients who will not require calcium supplementation thereby avoiding hypercalcemia in them.
CONCLUSIONS
A PTH and calcium-based protocol can be effectively used for safe early discharge of thyroidectomy patients the day after surgery without calcium supplementation. The compliance of patients for early discharge was good. Hence, we conclude that our protocol is an effective protocol with multiple benefits to patients and hospital services.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I thank the department of biochemistry for their support in running the PTH test and giving results as soon as possible. I thank Dr. Deepak Thomas Abraham Professor, Dr. Anish Jacob Cherian Associate Professor and my colleagues of Endocrine Surgery CMC Vellore for helping me write up the study.
REFERENCES
- 1.Zarnegar R, Brunaud L, Clark OH. Prevention, evaluation, and management of complications following thyroidectomy for thyroid carcinoma. Endocrinol Metab Clin North Am. 2003;32:483–502. doi: 10.1016/s0889-8529(03)00009-4. [DOI] [PubMed] [Google Scholar]
- 2.Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. 2014;101:307–20. doi: 10.1002/bjs.9384. [DOI] [PubMed] [Google Scholar]
- 3.Sabour S, Manders E, Steward DL. The role of rapid PACU parathyroid hormone in reducing post-thyroidectomy hypocalcemia. Otolaryngol Head Neck Surg. 2009;141:727–9. doi: 10.1016/j.otohns.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 4.Lindblom P, Westerdahl J, Bergenfelz A. Low parathyroid hormone levels after thyroid surgery: A feasible predictor of hypocalcemia. Surgery. 2002;131:515–20. doi: 10.1067/msy.2002.123005. [DOI] [PubMed] [Google Scholar]
- 5.Lombardi CP, Raffaelli M, Princi P, Santini S, Boscherini M, De Crea C, et al. Early prediction of post thyroidectomy hypocalcemia by one single iPTH measurement. Surgery. 2004;136:1236–41. doi: 10.1016/j.surg.2004.06.053. [DOI] [PubMed] [Google Scholar]
- 6.Youngwirth L, Benavidez J, Sippel R, Chen H. Postoperative parathyroid hormone testing decreases symptomatic hypocalcemia and associated emergency room visits after total thyroidectomy. Surgery. 2010;148:841. doi: 10.1016/j.surg.2010.07.038. [DOI] [PubMed] [Google Scholar]
- 7.Cayo AK, Yen TWF, Misustin SM, Wall K, Wilson SD, Evans DB, et al. Predicting the need for calcium and calcitriol supplementation after total thyroidectomy: Results of a prospective, randomized study. Surgery. 2012;152:1059–67. doi: 10.1016/j.surg.2012.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seo ST, Chang JW, Jin J, Lim YC, Rha K-S, Koo BS. Transient and permanent hypocalcemia after total thyroidectomy: Early predictive factors and long-term follow-up results. Surgery. 2015;158:1492–9. doi: 10.1016/j.surg.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 9.Toniato A, Boschin IM, Piotto A, Pelizzo M, Sartori P. Thyroidectomy and parathyroid hormone: Tracing hypocalcemia-prone patients. Am J Surg. 2008;196:285–8. doi: 10.1016/j.amjsurg.2007.06.036. [DOI] [PubMed] [Google Scholar]
- 10.Grodski S, Lundgren CI, Sidhu S, Sywak M, Delbridge L. Postoperative PTH measurement facilitates day 1 discharge after total thyroidectomy. Clin Endocrinol (Oxf) 2009;70:322–5. doi: 10.1111/j.1365-2265.2008.03317.x. [DOI] [PubMed] [Google Scholar]
- 11.Payne RJ, Tewfik MA, Hier MP, Tamilia M, Mac Namara E, Young J, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. OtolaryngolHead Neck Surg. 2005;133:386–90. doi: 10.1016/j.otohns.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Cherian AJ, Ramakant P, Paul TV, Abraham DT, Paul MJ. Next-day parathyroid hormone as a predictor of post-thyroidectomy hypocalcemia. World J Endoc Surg. 2016;8:203–7. [Google Scholar]
- 13.Alhefdhi A, Mazeh H, Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: A systematic review and meta-analysis. Oncologist. 2013;18:533–42. doi: 10.1634/theoncologist.2012-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antakia R, Edafe O, Uttley L, Balasubramanian SP. Effectiveness of preventative and other surgical measures on hypocalcemia following bilateral thyroid surgery: A systematic review and meta-analysis. Thyroid. 2015;25:95–106. doi: 10.1089/thy.2014.0101. [DOI] [PubMed] [Google Scholar]
- 15.Tolone S, Roberto R, del Genio G, Brusciano L, Parmeggiani D, Amoroso V, et al. The impact of age and oral calcium and vitamin D supplements on postoperative hypocalcemia after total thyroidectomy. A prospective study. BMC Surg. 2013;13(Suppl 2):S11. doi: 10.1186/1471-2482-13-S2-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abboud B, Sleilaty G, Zeineddine S, Braidy C, Aouad R, Tohme C, et al. Is therapy with calcium and vitamin D and parathyroid auto transplantation useful in total thyroidectomy for preventing hypocalcemia? Head Neck. 2008;30:1148. doi: 10.1002/hed.20836. [DOI] [PubMed] [Google Scholar]
- 17.Roh JL, Park CI. Routine oral calcium and vitamin D supplements for prevention of hypocalcemia after total thyroidectomy. Am J Surg. 2006;192:675–8. doi: 10.1016/j.amjsurg.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Docimo G, Tolone S, Pasquali D, Conzo G, D'Alessandro A, Casalino G, et al. Role of pre and post-operative oral calcium and vitamin D supplements in prevention of hypocalcemia after total thyroidectomy. Il G Chir. 2012;33:374–8. [PubMed] [Google Scholar]
- 19.Sanabria A, Dominguez LC, Vega V, Osorio C, Duarte D. Routine postoperative administration of vitamin D and calcium after total thyroidectomy: A meta-analysis. Int J Surg Lond Engl. 2011;9:46–51. doi: 10.1016/j.ijsu.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Snyder SK, Hamid KS, Roberson CR, Rai SS, Bossen AC, Luh JH, et al. Outpatient thyroidectomy is safe and reasonable: Experience with more than 1,000 planned outpatient procedures. J Am Coll Surg. 2010;210:575. doi: 10.1016/j.jamcollsurg.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 21.Sperlongano P, Sperlongano S, Foroni F, De Lucia FP, Pezzulo C, Manfredi C, et al. Postoperative hypocalcemia: Assessment timing. Int J Surg Lond Engl. 2014;12(Suppl 1):S95–7. doi: 10.1016/j.ijsu.2014.05.042. [DOI] [PubMed] [Google Scholar]
- 22.Lee YS, Chang H-S, Chung WY, Nam K-H, Park CS. Relationship between onset of hypocalcemic symptoms and the recovery time from transient hypocalcemia after total thyroidectomy. Head Neck. 2014;36:1732–6. doi: 10.1002/hed.23530. [DOI] [PubMed] [Google Scholar]
- 23.Promberger R, Ott J, Kober F, Mikola B, Karik M, Freissmuth M, et al. Intra- and postoperative parathyroid hormone-kinetics do not advocate for autotransplantation of discolored parathyroid glands during thyroidectomy. Thyroid. 2010;20:1371–5. doi: 10.1089/thy.2010.0157. [DOI] [PubMed] [Google Scholar]
- 24.Lang BH-H, Yih PC-L, Ng KK. A prospective evaluation of quick intraoperative parathyroid hormone assay at the time of skin closure in predicting clinically relevant hypocalcemia after thyroidectomy. World J Surg. 2012;36:1300–6. doi: 10.1007/s00268-012-1561-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sitges-Serra A, Ruiz S, Girvent M, Manjón H, Dueñas JP, Sancho JJ. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg. 2010;97:1687–95. doi: 10.1002/bjs.7219. [DOI] [PubMed] [Google Scholar]
- 26.Vescan A, Witterick I, Freeman J. Parathyroid hormone as a predictor of hypocalcemia after thyroidectomy. Laryngoscope. 2005;115:2105–8. doi: 10.1097/01.MLG.0000181504.69230.87. [DOI] [PubMed] [Google Scholar]
- 27.Nussbaum SR, Thompson AR, Hutcheson KA, Gaz RD, Wang CA. Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism. Surgery. 1988;104:1121–7. [PubMed] [Google Scholar]
- 28.Chindavijak S. Prediction of hypocalcemia in postoperative total thyroidectomy using single measurement of intra-operative parathyroid hormone level. J Med Assoc Thail Chotmaihet Thangphaet. 2007;90:1167–71. [PubMed] [Google Scholar]
- 29.Mazeh H, Khan Q, Schneider DF, Schaefer S, Sippel RS, Chen H. Same-day thyroidectomy program: Eligibility and safety evaluation. Surgery. 2012;152:1133–41. doi: 10.1016/j.surg.2012.08.033. [DOI] [PubMed] [Google Scholar]
- 30.Cote V, Sands N, Hier MP, Black MJ, Tamilia M, MacNamara E, et al. Cost savings associated with post-thyroidectomy parathyroid hormone levels. OtolaryngolHead Neck Surg. 2008;138:204–8. doi: 10.1016/j.otohns.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 31.Scurry WC, Beus KS, Hollenbeak CS, Stack BC. Peri operative parathyroid hormone assay for diagnosis and management of post thyroidectomy hypocalcemia. Laryngoscope. 2005;115:1362–6. doi: 10.1097/01.MLG.0000166699.23264.37. [DOI] [PubMed] [Google Scholar]
- 32.AES Guidelines 06/01 Group Australian Endocrine Surgeons Guidelines AES06/01. Postoperative parathyroid hormone measurement and early discharge after total thyroidectomy: Analysis of Australian data and management recommendations. ANZ J Surg. 2007;77:199–202. doi: 10.1111/j.1445-2197.2007.04018.x. [DOI] [PubMed] [Google Scholar]
- 33.Lam A, Kerr PD. Parathyroid hormone: An early predictor of post thyroidectomy hypocalcemia. Laryngo scope. 2003;113:2196–200. doi: 10.1097/00005537-200312000-00029. [DOI] [PubMed] [Google Scholar]
- 34.Chow T-L, Choi C-Y, Chiu AN-K. Postoperative PTH monitoring of hypocalcemia expedites discharge after thyroidectomy. Am J Otolaryngol. 2014;35:736–40. doi: 10.1016/j.amjoto.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Materazzi G, Dionigi G, Berti P, Rago R, Frustaci G, Docimo G, et al. One-day thyroid surgery: Retrospective analysis of safety and patient satisfaction on a consecutive series of 1,571 cases over a three-year period. Eur Surg Res Eur Chir Forsch Rech Chir Eur. 2007;39:182–8. doi: 10.1159/000100904. [DOI] [PubMed] [Google Scholar]
- 36.Harding J, Sebag F, Sierra M, Palazzo FF, Henry J-F. Thyroid surgery: Postoperative hematoma--prevention and treatment. Langenbecks Arch Surg. 2006;391:169–73. doi: 10.1007/s00423-006-0028-6. [DOI] [PubMed] [Google Scholar]
- 37.Lee HS, Lee BJ, Kim SW, Cha YW, Choi YS, Park YH, et al. Patterns of Post-thyroidectomy Hemorrhage. Clin Exp Otorhinolaryngol. 2009;2:72–7. doi: 10.3342/ceo.2009.2.2.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Campbell MJ, McCoy KL, Shen WT, Carty SE, Lubitz CC, Moalem J, et al. A multi-institutional international study of risk factors for hematoma after thyroidectomy. Surgery. 2013;154:1283. doi: 10.1016/j.surg.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 39.Narayanan S, Arumugam D, Mennona S, Wang M, Davidov T, Trooskin SZ. An evaluation of postoperative complications and cost after short-stay thyroid operations. Ann Surg Oncol. 2015;23:1440–5. doi: 10.1245/s10434-015-5004-3. [DOI] [PubMed] [Google Scholar]
- 40.Trottier DC, Barron P, Moonje V, Tadros S. Outpatient thyroid surgery: Should patients be discharged on the day of their procedures? Can J Surg J Can Chir. 2009;52:182–6. [PMC free article] [PubMed] [Google Scholar]