Abstract
Background
Loneliness is common in dementia caregivers as cognitive impairment (CI) alters marital and social relationships. Unexplored is how an individual’s loneliness is affected at earlier, more ambiguous, periods of their spouse’s CI.
Methods
Using the Health and Retirement Study, our study participants included 2,206 coupled individuals with normal cognitive function at the 2006/8 baseline. Loneliness outcomes at baseline, 4-year and 8-year follow-up are assessed by the status of transition to cognitive impairment no dementia (TCIND) (2010/12 & 2014/16) using linear mixed models.
Results
Individual’s loneliness was stable when their spouse’s cognition remained normal, but increased with the spouse’s TCIND. The increase in loneliness did not vary by gender.
Conclusions
Loneliness, a key risk factor for reduced life quality and increased depression, increases even at early stages of a partner’s CIND. This work suggests the potential impact of early intervention and social support for partners of individuals with CIND.
The health and well-being of spouses are inextricably linked with one another. As individuals age, the likelihood that either they or their spouse experiences cognitive decline increases (Legdeur et al., 2018). Cognitive decline necessitates many changes in an individual’s and his/her spouse’s lives—they are limited in the activities they can do, how they connect with each other, and ultimately their relationships might change due to the many social ramifications of cognitive decline (Auyeung et al., 2008; Holdsworth & McCabe, 2018; Vitaliano, Murphy, Young, Echeverria, & Borson, 2011). However, relatively little research has examined the psychological experience of individuals who witness their spouse’s cognitive decline—do they become lonelier as a result of the onset of cognitive decline in their spouses? In the current study, we explored how individuals’ loneliness changes in response to spousal declines in cognitive functioning among 2,206 coupled individuals from the Health and Retirement Study.
Loneliness in Late-Adulthood
Loneliness, the subjective or perceived deficiencies in the quantity or quality of an individual’s social relationships, is one of the most painful human experiences (Peplau & Perlman, 1982). Weiss’s (1973) foundational theory assessed two components of loneliness: social- the absence of a social network, sense of belonging, or companionship and emotional- one’s attachment to a particular figure (such as romantic or familial) to turn to for emotional affection or security. Thus, while it is often related to social isolation, loneliness is distinct and can be experienced even in the context of large social networks (Tomaka, Thompson, & Palacios, 2006). Exposure to loneliness has detrimental effects on mental and physical health, such as increased risk of cognitive decline, depression, coronary heart disease, and mortality (Cacioppo, Hawkley, & Thisted, 2010; Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Chen & Feeley, 2013; Luo, Hawkley, Waite, & Cacioppo, 2012; Perissinotto, Stijacic Cenzer, & Covinsky, 2012; Rico-Uribe et al., 2018). Loneliness is especially pervasive among older adults. About 17–41% percent of Americans age 50 and older report feelings of loneliness. This is a wide estimate range likely due to 1) different data sources, 2) recruiting different populations, 3) applying varying survey designs, and 4) assessing loneliness with unique measures (Chen & Feeley, 2013; de Jong Gierveld, Van Tilburg, & Dykstra, 2006; Solway et al., 2019; Theeke, 2010; Wilson & Moulton, 2010).
Loneliness in the Context of a Spouse’s Cognitive Impairment
As social relationships in late-life often center around spousal relationships, shifting dynamics such as disability or cognitive impairment (CI) in one person may impact their spouses’ experience of loneliness (Mortiz, Kasl, & Ostfeld, 1992). Indeed, research on caregivers for individuals with dementia has shown this to be the case. Older adult caregivers for individuals with dementia are more likely to experience loneliness relative to their non-caregiving peers (Beeson, 2003; Lavela & Ather, 2010), though contrasting findings exist (e.g. Ekwall et al., 2005 found that caregivers were not lonelier than non-caregivers). Further, while loneliness is more common among older caregivers (Greenwood, Pound, Brearley, & Smith, 2019), even midlife partners dealing with younger-onset dementia report increasing loneliness (Holdsworth & McCabe, 2018). The life course perspective of linked lives posits that spouses and partners have mutual influence on one another, and we expect this to be the case as they manage and cope with cognitive decline (Elder, Johnson, & Crosnoe, 2003; Mejía & Gonzalez, 2017). However, the impact of early cognitive decline (non-dementia) on a spouse’s loneliness has not been explored and is the focus of the current study.
As an individual transitions to CI and symptoms progress, this may be a key time of adaptation for spouses as they change their interactions both within and beyond the dyad. For example, within the context of a dyad where one partner is cognitively impaired, spouses describe a loss of intimacy in marriage while watching their partner cope with the transition from independence to dependence (Evans & Lee, 2013). Spouses may need to adapt to changes in the interaction and quality of a relationship, such as declines in intellectually stimulating conversations and mutual support, thereby relating to the experience of social and emotional loneliness (Vitaliano, Murphy, Young, Echeverria, & Borson, 2011; Weiss, 1973).
Beyond the dyadic relational context, adaptation may occur in external social relations as well. For example, a caregiving partner may decide to avoid social outings due to uncertainty regarding the individual with CI’s behavior and to avoid potentially embarrassing social situations (Holdsworth & McCabe, 2018; Ory, Hoffman, Yee, Tennstedt, & Schulz, 1999). In contrast, however, some individuals may receive more help from family, friends, and other care providers when their partner is sick, which could engender more social support. Thus, while adapting to a partner’s dementia is known to impact a spouse’s loneliness, we explore whether this psychological change may occur at earlier stages of cognitive decline.
Considering Context: Gender Differences in Loneliness and Marriage
Prior research suggests that the experience of loneliness may differ by gender, and thus gender is a key contextual factor to assess across the transition to CI (Aartsen & Jylhӓ, 2011; Dahlberg & McKee, 2014; Pinquart & Sorensen, 2001). Among caregivers, wives tend to report more loneliness than husbands (Ekwall, Sivberg, & Hallberg, 2005; Lavela & Ather, 2010). However, the recent National Poll on Healthy Aging found only a small gender difference in loneliness reports of older adults, with women being only slightly more likely to report loneliness than men (36 vs 31%; Solway et al., 2019). Indeed, within a traditional marriage, women tend to take major responsibility for maintaining social connections to families and friends, while men’s social circles tend to revolve around their wives (Bernard, 1972; Umberson, Williams, & Thomeer, 2013). Wives are also more likely to provide emotional and social support to their husband and play the caregiving role when their husband is sick, while husbands are less likely to do so in a relationship (Bernard, 1972; Revenson et al., 2016; Umberson et al., 2013; Zimmerman, Litt, & Bose, 2006). Thus, bereavement or a spouse’s CI can be a particular challenge for men, necessitating greater adjustment (Forster et al., 2019; Liu, Zhang, Choi, & Langa, 2019; Williams & Umberson, 2004). For example, a spouse’s disability is associated with greater social loneliness for men, whereas only their own disability was associated with greater social loneliness for wives (Korporaal, Broese van Groenou, & van Tilburg, 2008). Therefore, we hypothesize that a husband’s loneliness would increase more with their wife’s developing CI while wives’ loneliness may be less (or not) affected by the CI of their husbands.
The Current Study
While a robust amount of research highlights the loneliness that caregivers face while caring for a spouse with dementia, little focus has been placed on how spouses are impacted earlier in the process—particularly at points of transition from normal cognitive functioning to early cognitive decline. This transition may be more ambiguous as early cognitive changes can be more easily covered up or unclear as to etiology. This is of key importance as loneliness may put spouses themselves at increased risk of CI (Cacioppo & Cacioppo, 2014; Cacioppo & Hawkley, 2009). Our research question is based on the theory of social and emotional loneliness and previous longitudinal studies suggesting that losing personal or social resources- particularly from a healthy spouse is associated with increases in loneliness (Aartsen & Jylhӓ, 2011; Dykstra, van Tilburg, & Gierveld, 2005). We consider individuals’ loneliness among those whose spouse or partner (spouse henceforth) is transitioning from normal cognitive function to cognitive impairment no dementia (hereafter TCIND), relative to those whose spouse maintains their normal cognition in a national sample of older adults. We hypothesize that loneliness will increase among individuals whose spouse experiences TCIND. We further hypothesize that the association between an individual’s loneliness and a spouse’s cognitive transition would differ by a key contextual factor, gender, such that the rate of increase in loneliness is greater for men than women in response to a spouse’s TCIND. We test these hypotheses about an individual’s TCIND related to spouse loneliness using a secondary data analysis of a 3-wave study (over an 8-year interval) by comparing individual-level changes in loneliness across the three times between (a) couples where both members remained at normal cognitive functioning four years later at the first follow-up (both normal group) to (b) couples where only one member experienced TCIND at the first follow-up (TCIND group). The sample was restricted so all individuals who had normal cognitive functioning at time 1.
Method
Data
The Health and Retirement Study (HRS) is a longitudinal study that surveys approximately 20,000 Americans over the age of 50 every two years. Begun in 1992, new cohorts of older adults were added in 1998 such that the HRS sample became nationally-representative of the US population age 51 and older. With sample refreshment every 6 years, the HRS continues to be representative of adults age 51 and older in years of refreshment. Since 2006, the Psychosocial and Lifestyle Questionnaire (which assesses loneliness) was surveyed in each biennial wave from a rotating 50% of the core panel participants who complete the enhanced face-to face interview. Accordingly, longitudinal data are available at four-year intervals (Smith, Ryan, Fisher, Sonnega, & Weir, 2016) for half of the core participants.
Analysis Sample
In our study, we examine three time points - baseline (time 1) referring to 2006 for the first rotating panel and 2008 for the second panel, first follow-up (time 2) referring to 2010 for the first rotating panel and 2012 for the second panel, and second follow-up (time 3) referring to 2014 for the first rotating panel and 2016 for the second panel. We first restrict the sample to those who were married or partnered at baseline, which consists of 9,525 coupled respondents. Because we were interested in the transition from normal functioning to CIND, we restricted the sample to 6,462 individuals who and whose spouse both had normal cognitive functioning at baseline. Of these 6,462 individuals, 5,244 had a follow-up interview in time 2, but 404 lost a spouse/partner (283 widowed; 121 separated, absent, or divorced) in time 2, resulting in 4,840 individuals. Of these, 4,650 had a follow-up interview for time 2 with non-missing data in the cognitive functioning variable and 4,633 remained as married or partnered with the same person in the follow-up periods. We further excluded individuals if they or their spouse transitioned to dementia because of the study’s focus on early cognitive decline (from normal to CIND), dropped the same sex couple because of the study’s focus on gender difference, and dropped multiple couples in the same household. These restrictions lead to 4,540 individuals and 11,021 individual-year (or, 2,430 couples and 5,889 couple-year observations) for our final analytic sample.
We consider the focal person in our analysis who may/may not TCIND. This decision was made as the HRS study design samples a focal person to create a nationally representative sample of adults aged 51 and older, with a spouse of the focal individual included as available. In addition to the study sampling design, HRS targets respondents required to be 51 years of age or older, whereas spouses could be younger. Further, in the two groups (i.e., TCIND and Both Normal), there is an asymmetry in that two members in the Both Normal group could be considered contrasts to spouses not experiencing TCIND (unlike in the TCIND group where couples contain only one member who did not TCIND). Thus, we count the target HRS respondent as the focal individual who could TCIND in predicting their spouse’s loneliness.
Measures
Our main independent variable is the CIND status of the spouse based on a measure developed by Langa and Weir (Crimmins et al., 2011). We include the items from the modified Telephone Interview for Cognitive Status (TICS) since our sample includes individuals younger than 65 years old (as some items are only provided to 65+ years old individuals; Ofstedal, Fisher, & Herzog, 2005). The total score of cognitive functioning ranges from 0 to 27 points and represents the sum of: immediate word recall (0–10 points); delayed word recall (0–10 points); serial 7s (0–5 points); and backwards counting from 20 (0–2 points). This composite score has been previously validated as a proxy measure for CIND given its high predictive rate of Alzheimer’s disease and related dementia (Choi, Schoeni, Martin & Langa, 2018; Crimmins, Kim, Langa, & Weir, 2011). A higher number reflects better cognitive functioning. In the Langa-Weir specification, a total score of 0–6 points is labeled as “dementia,” 7–11 as “cognitively impaired but not dementia (CIND),” and 12–27 as “normal.” Our analysis focuses on the CIND category.
Our outcome variable is the loneliness of individuals, which is measured based on the validated Revised UCLA Loneliness Scale (R-UCLA) (Hughes, Waite, Hawkley, & Cacioppo, 2014). The loneliness scale includes three items: “How often do you feel you lack companionship?”; “How often do you feel left out?”; and “How often do you feel isolated from others?” Responses to each item range from 1(hardly ever or never) to 3(often). Averaging the scores across three items creates an index of loneliness (α for full sample = .801). The R-UCLA scale is a unidimensional scale aimed at measuring global loneliness (Hughes et al., 2004). In fact, these three items were chosen specifically from one factor of a longer multi-factor measure of loneliness (Russell, 1996). The three-item version is in line with Weiss’s (1973) theoretical assessment of these types of measures assessing social loneliness more than emotional loneliness. However, while previous research has found the UCLA loneliness scale to be most strongly correlated with social loneliness (on scales designed to distinguish between the two), it is also significantly associated with emotional loneliness, suggesting that it aligns with both theoretical concepts but is most closely related to social loneliness (DiTommaso, Brannen, & Best, 2004).
In our multilevel regression models, we adjust for potential confounding factors. Prior research has identified key correlates of loneliness in older adults including demographic (e.g. being female, being widowed), socioeconomic (e.g. low socioeconomic status), and health (e.g. physical disabilities, low activity levels) factors (Aartsen & Jylhӓ, 2011; Dahlberg & McKee, 2014; Pinquart & Sorensen, 2001). These factors may limit an individual from social activities, aligning with Weiss’s (1973) theoretical conception of social loneliness. Thus we account for demographic, socioeconomic, and health measures for both individuals and spouses including: age (continuous), race (white, black, other), ethnicity (Hispanic or not Hispanic), the number of people in the household, marital status (married vs. partnered), education (1= less than high school, 2= GED, 3= high school graduate, 4=some college, 5=college and above), having at least one activity of daily living (ADL) limitation out of six items (dressing, getting in and out of bed, bathing, walking across rooms, eating, toileting) and as a separate term having at least one instrumental activity of daily living (IADL) out of five items (using a telephone, shopping, preparing meals, managing money, taking medicine), seven indicators of having a diagnosis of chronic diseases (high blood pressure, diabetes, cancer, lung disease, heart problems, stroke, and arthritis), and personality. Personality is measured using the Big Five personality traits of extraversion (5-items) and neuroticism (4-items) on a 4-point likert scale where participants indicate how much a characteristic describes them from 1) not at all to 4) a lot averaged, where a higher score indicates more of the trait. Extraversion and neuroticism were chosen based on meta-analysis results (Buecker, Maes, Denissen, & Luhmann, 2020). To avoid controlling for potential pathways, we include these confounding factors measured at baseline (i.e., characteristics as of 2006 for rotating panel 1 and 2008 for rotating panel 2).
Analytic Approach
We conducted linear mixed models with restricted maximum likelihood to account for the longitudinal and dyadic nature of the data (i.e., special case of a growth curve model). A random intercept was included for the couple. Both time (a factor with three levels) and gender were included in the model as fixed effects. We created an effect code based on whether both couple members remained at normal cognitive functioning at the first follow-up (time 2) or one couple member experienced TCIND. To keep model parsimony with only three time points we did not include a random slope nor did we want to impose linear change across the three time points.
In the analytic models, we first included our 1) effects of interest (i.e., a significant TCIND group x time interaction predicting loneliness) and then sequentially included 2) demographics of HRS target, 3) health variables of HRS target 4) socioeconomic characteristics of the spouse, and 5) health conditions and personality of the spouse (as sequential blocks) to control for potential confounding factors and to check if any baseline characteristics confounded the main effects. Statistical significance on the key interactions (two-way between TCIND group and time and three-way between TCIND group, time, and gender) did not differ across these three blocks so we report only the final model with all blocks of covariates controlled in the results section. Results from additional sensitivity analyses testing time varying physical health and IADL/ADLs across all three waves suggested that the statistical significance of the key two-way interaction remained the same and the key three-way interaction remained nonsignificant. Results from additional sensitivity analyses that involved relaxing sample exclusion criteria such as including households where either member exhibited dementia at wave 3 suggested that the two key interactions remained the same.
Degrees of freedom were computed using Satterthwaite’s method; omnibus significance tests were computed using Type III sum of squares (to be consistent with standard regression output) and contrasts were tested with Wald tests. All reported significance tests are based on two-tailed alpha at the level of .05. Full-information (restricted) maximum likelihood was used to estimate parameters in the linear mixed models accounting for missing data in the dependent variable loneliness, and cases with missing values on the covariates were dropped in regressions using covariates. Inferential tests using survey weights are presented. Standard errors were adjusted and population weights were employed using the complex survey design factors provided from the HRS.
Results
Descriptive statistics
Descriptive statistics (unweighted) of the sample appear in Table 1. We focus on the demographic, socioeconomic and health variables of individuals who have normal cognitive functioning at both time 1 and time 2 given that the primary outcome variable, loneliness, is based on this individual (not their spouse). These statistics are estimated for the overall sample and stratified by the main comparison groups - both normal and TCIND (as defined above). The p-values presented in Table 1 are based on contingency table tests comparing the two groups (‘both normal’ and TCIND) except for the age and the two personality variables, which are based on two-sample t-tests. In general, individuals in the TCIND group were four years older, included more females, had a lower share of white participants and reported lower levels of education. Individuals in the TCIND group had significantly more ADL and IADL impairments, and reported higher rates of hypertension and arthritis.
Table 1.
Unweighted Sample Characteristics, overall and by TCIND Status
| Overall (n=2206) |
Both Normal (n=2016) |
TCIND (n=190) |
P value | |
|---|---|---|---|---|
| Age | ||||
| Mean (SE) | 63 (0.2) | 62 (0.2) | 66 (0.71) | <0.001 |
| Gender | ||||
| Female | 1384 (63 %) | 1249 (62 %) | 135 (71 %) | 0.016 |
| Race | ||||
| White | 2021 (92 %) | 1854 (92 %) | 167 (88 %) | 0.012 |
| Black | 111 (5 %) | 93 (5 %) | 18 (9 %) | |
| Other | 74 (3 %) | 69 (3 %) | 5 (3 %) | |
| Ethnicity | ||||
| Hispanic | 112 (5 %) | 99 (5 %) | 13 (7 %) | 0.324 |
| Number of People in Household | ||||
| 2 | 1652 (75 %) | 1506 (75 %) | 146 (77 %) | 0.855 |
| 3 | 347 (16 %) | 319 (16 %) | 28 (15 %) | |
| 4 | 131 (6 %) | 122 (6 %) | 9 (5 %) | |
| 5+ | 76 (3 %) | 69 (3 %) | 7 (4 %) | |
| Married/Partnered | ||||
| Married | 2125 (96 %) | 1939 (96 %) | 186 (98 %) | 0.318 |
| Partnered | 81 (4 %) | 77 (4 %) | 4 (2 %) | |
| Education | ||||
| <12 years | 264 (12 %) | 227 (11 %) | 37 (19 %) | <0.001 |
| 12 years | 704 (32 %) | 630 (31 %) | 74 (39 %) | |
| >12 years | 1237 (56 %) | 1159 (57 %) | 78 (41 %) | |
| Any ADL | 161 (7 %) | 139 (7 %) | 22 (12 %) | 0.026 |
| Any IADL | 100 (5 %) | 84 (4 %) | 16 (8 %) | 0.012 |
| Hypertension | 1005 (46 %) | 903 (45 %) | 102 (54 %) | 0.023 |
| Diabetes | 287 (13 %) | 261 (13 %) | 26 (14 %) | 0.866 |
| Cancer | 273 (12 %) | 244 (12 %) | 29 (15 %) | 0.253 |
| Chronic lung disease | 128 (6 %) | 112 (6 %) | 16 (8 %) | 0.146 |
| Heart Problems | 334 (15 %) | 303 (15 %) | 31 (16 %) | 0.716 |
| Stroke | 71 (3 %) | 64 (3 %) | 7 (4 %) | 0.869 |
| Arthritis | 1140 (52 %) | 1022 (51 %) | 118 (62 %) | 0.003 |
| Extraversion Mean (SE) | 3.24 (.01) | 3.24 (.01) | 3.23 (.04) | .99 |
| Neuroticism Mean (SE) | 2.03 (.01) | 2.03 (.01) | 2.04 (.04) | .99 |
Hypothesis testing
We first present the results of a linear mixed model with time, gender and TCIND status as sole predictors. The omnibus two-way interaction between time and TCIND status was statistically significant, F(2, 3465.6)=6.34, p=.002, Cohen’s f = .06, suggesting that individuals in the Both Normal group and TCIND group differentially changed in loneliness over time (as predicted). The omnibus three-way interaction between time, TCIND status, and gender was not statistically significant, p=.085, Cohen’s f = .035. Coefficients are presented in Table 2.
Table 2.
The Effects of Spouse’s TCIND status, Time, and Gender on Loneliness
| No Covariates | With Covariates | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | Estimates | CI | std. Beta | p | Estimates | CI | std. Beta | p |
| Intercept | 1.393 | 1.347 – 1.438 | 0.080 | 0.125 | 1.766 | 1.460 – 2.071 | 0.267 | 0.101 |
| Gender | −0.002 | −0.047 – 0.043 | −0.017 | 0.744 | 0.012 | −0.040 – 0.065 | 0.026 | 0.674 |
| TCIND status | −0.046 | −0.091 – −0.000 | −0.090 | 0.084 | −0.030 | −0.081 – 0.021 | −0.068 | 0.253 |
| Time 2 v Time 1 | −0.025 | −0.048 – −0.001 | −0.043 | 0.124 | −0.022 | −0.048 – 0.004 | −0.051 | 0.105 |
| Time 3 v Time 1 | 0.060 | 0.029 – 0.091 | 0.106 | 0.004 | 0.064 | 0.030 – 0.099 | 0.145 | 0.000 |
| Int: TCIND * T2v1 | 0.014 | −0.009 – 0.038 | 0.016 | 0.564 | 0.009 | −0.017 – 0.036 | 0.021 | 0.505 |
| Int: TCIND * T3v1 | −0.053 | −0.084 – −0.022 | −0.088 | 0.018 | −0.055 | −0.090 – −0.021 | −0.127 | 0.002 |
| Int: Gender * T2v1 | −0.006 | −0.030 – 0.017 | −0.013 | 0.649 | −0.007 | −0.034 – 0.019 | 0.021 | 0.498 |
| Int: Gender * T3v1 | 0.016 | −0.015 – 0.047 | 0.014 | 0.709 | 0.021 | −0.013 – 0.055 | −0.008 | 0.849 |
| Int: TCIND * Gender | −0.007 | −0.052 – 0.038 | −0.001 | 0.979 | −0.009 | −0.059 – 0.041 | −0.013 | 0.828 |
| Int: T2v1TCINDGender | 0.009 | −0.015 – 0.032 | 0.021 | 0.449 | 0.008 | −0.018 – 0.034 | −0.017 | 0.593 |
| Int: T3v1TCINDGender | −0.033 | −0.064 – −0.002 | −0.060 | 0.105 | −0.038 | −0.072 – −0.003 | −0.023 | 0.571 |
| Random effects | ||||||||
| σ2 | 0.07 | 0.07 | ||||||
| τ00 | 0.23 | 0.22 | ||||||
| ICC | 0.77 | 0.76 | ||||||
Note. TCIND: Compares the effect of couples who both report normal functioning to couples in which one member transitions to Cognitive Impairment Not Dementia. Int: Interaction. CI: Confidence Interval. ICC: Intra-class correlation. Survey sampling weighted estimates from the linear mixed model.
A second linear mixed model added the demographic, socioeconomic, and health variables described in the Methods section (352 couples had missing data on at least one of these covariates). The omnibus two-way interaction between time and TCIND status remained statistically significant even with the control variables, F(2, 2902.1)=6.53, p=.001, Cohen’s f = .06. The omnibus three-way interaction between time, TCIND status and gender remained non-significant after the control variables were added, p=.06, Cohen’s f = .04. Coefficients of the key predictor variables are presented in Table 2 and are compared to those in the first linear mixed model without covariates.
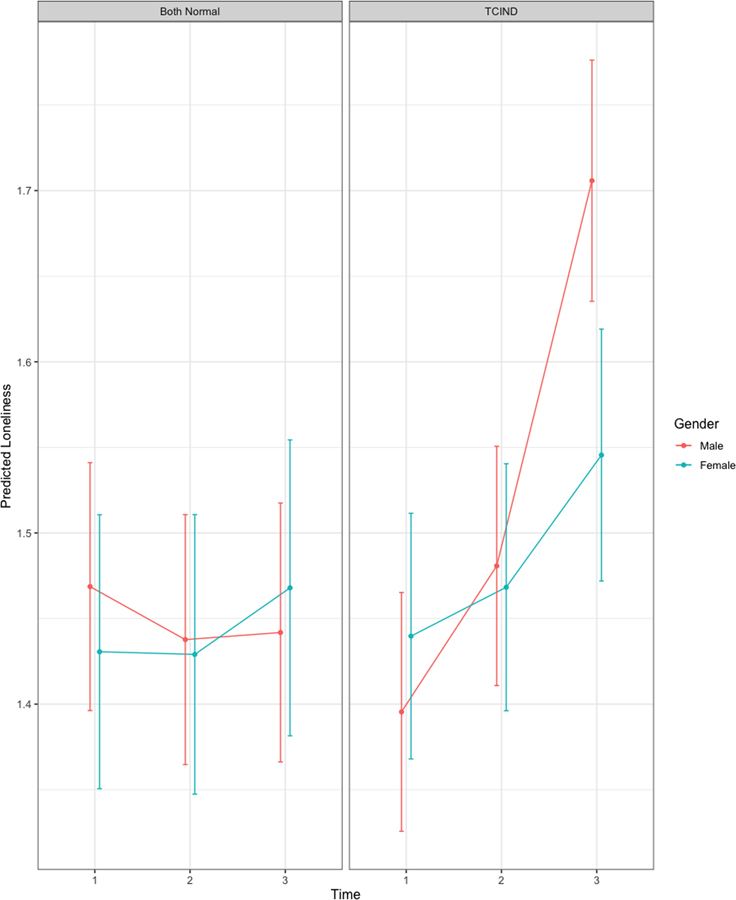
The estimated means from the second linear mixed model (survey sampling weighted and covariates controlled) are presented in Figure 1. We note that the estimated means for both TCIND groups at time 1 are comparable, suggesting the control variables were successful at statistically equating these two groups (the pairwise comparison of loneliness at time 1 between the two cognitive status groups was not statistically significant, p=.56). Following our hypotheses, we performed a set of contrasts on these estimated means using Wald tests. First, the TCIND group demonstrated a significant linear trend across the three times, z=3.79, p=.0002 (collapsing across gender) while loneliness remained stable across the three times for the Both Normal group, p= .70 for linear contrast. The interaction between the linear contrast for the two groups was statistically significant, z=3.59, p=.0003. Second, collapsing across gender, the TCIND group at time 3 exhibited higher loneliness than both time 1 and time 2 (i.e., a −1, −1, 2 contrast), z=3.53, p=.0004, but this contrast is not significant for the “both normal” group (p=.27) and the interaction between these contrasts was statistically significant, z=3.18, p=.001. Third, the omnibus two-way interaction between time and gender within the TCIND group was not statistically significant, p=.39, so we do not see reliable evidence for a gender difference in the individual’s loneliness when a spouse TCIND. We also conducted a post hoc contrast comparing the interaction of the linear and quadratic contrasts of time with gender and neither test was significant (p=.18 and p=.26, respectively) suggesting that the apparent pattern on the right panel in Figure 1 is not reliably different across gender.
Figure 1.
Linear Mixed Model Estimated Loneliness Means by Gender and TCIND Status (survey sampling weighted)
Discussion
The current study is one of the first to examine adjustment in individuals whose spouses experience cognitive decline longitudinally in older adulthood. Building upon prior work examining loneliness among caregivers for individuals living with dementia, we examined changes in loneliness among spouses whose partner is at an earlier stage of initial cognitive decline utilizing the nationally representative Health and Retirement Study. In support of the life course perspective of linked lives (Elder, Johnson, & Crosnoe, 2003; Mejía & Gonzalez, 2017), we find that accounting for the demographic, socioeconomic, and health covariates of both individuals and their spouses, an individual’s loneliness increases significantly if his or her spouse TCIND. On the other hand, individuals whose spouse retained cognitive functioning had relatively stable levels of loneliness over time. Our design considers individuals who all had normal cognitive functioning at baseline, and compares two groups, one where a spouse experienced TCIND and one where both partners remain cognitively normal. The design features allow for stronger inferences about the role of TCIND and suggest that findings aren’t attributable to a formal dementia status—changes in loneliness were apparent at more moderate levels of cognitive impairment.
Prior work has found that feelings of nervousness, uselessness, and a reduction in social activities are associated with the initial onset of loneliness, and these are all factors that may increase in individuals who have a spouse showing ambiguous or early signs of cognitive decline (Aartsen & Jylhӓ, 2011). Yet while prior work in the HRS has found loneliness to be relatively stable over time, we see changes in relation to a partner’s TCIND (Gum et al., 2017). These increases in loneliness appear to take place over time, with a sharper increase happening between four and eight years following the TCIND, as opposed to the first four years immediately following the transition. As we started with couples who were both cognitively normal, the initial transition may be more ambiguous with subtle changes in the couple’s relationship and social interactions being noticed more over time. It could be that interpersonal frustrations related to a spouse’s CIND accumulate over time and are not present until sometime after the transition begins. Future studies may consider the trajectory of loneliness before and after a TCIND to better understand the time period over which loneliness is mutable in relation to cognitive decline.
In contrast to our second hypothesis, even if rates of CIND or other risk factors differ for men and women, our findings suggest that the TCIND impacts husbands and wives similarly in terms of increases in experienced loneliness — both men and women feel lonelier when their spouse experiences CIND. While prior caregiving studies tend to show that wives report more loneliness than husbands (Ekwall, Sivberg, & Hallberg, 2005; Lavela & Ather, 2010), we did not find a difference in changes in loneliness between wives and husbands whose partner had CIND. There was a trend toward greater loneliness in men four years following a wife’s TCIND relative to men whose wife stayed cognitively normal, but it was not significant — likely related to low statistical power due to small sample size. Future research may further consider the timeline over which longitudinal changes in loneliness take place among husband’s whose wives’ TCIND.
Implications
Loneliness is a key outcome of public health interest as it may put spouses of individuals with CIND themselves at risk for CI in addition to other chronic medical conditions and mortality (Cacioppo & Cacioppo, 2014; Cacioppo & Hawkley, 2009; Chen & Feeley, 2013; Luo, Hawkley, Waite, & Cacioppo, 2012; Perissinotto, Stijacic Cenzer, & Covinsky, 2012; Rico-Uribe et al., 2018).Wilson and colleagues (2007) found that with each one-unit increase on a loneliness scale, the risk for Alzheimer’s disease increases by 51% (RR=1.51). Yet loneliness is modifiable and may be addressable in improving quality of life and mental and physical health outcomes for spouses (Cacioppo, Hawkley, & Thisted, 2010; Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Chen & Feeley, 2013; Luo, Hawkley, Waite, & Cacioppo, 2012; Perissinotto, Stijacic Cenzer, & Covinsky, 2012; Rico-Uribe et al., 2018). As a more engaged lifestyle and participating in cognitively stimulating activities has been found to reduce the risk of cognitive decline, psychosocial interventions aimed at incorporating social interactions and support may be of benefit for individuals with a spouse experiencing cognitive decline (Hultsch, Hertzog, Small, & Dixon, 1999; Wilson et al., 2002).
Moreover, our findings suggest the need for early interventions for individuals whose spouses are starting to show signs of cognitive decline to help them be resilient to loneliness increases associated with the spouse’s TCIND. A dementia diagnosis provides a more definitive time for intervention when both partners are likely to attend a diagnostic medical appointment. However, physicians may need to take preventative measures in discussing loneliness and support among older couples at earlier stages of CI. Individuals who are lonely have more primary care visits than individuals who are not lonely, suggesting ripe opportunities for intervention (Ellaway, Wood, & MacIntyre, 1999). Yet additional visits may increase burden on physicians, healthcare costs, and appointment waiting lists (Ellaway et al., 1999). Physician consideration of social problems may increase their workload and the amount of time needed with the patient, which is already limited due to overbooked schedules of physicians and clinics. Indeed, primary care physicians commonly circumvent questions regarding social issues to not extend the length of the appointment (Jovicic et al., 2019; McPherson, Byng, and Oxley, 2014). Physicians also may not ask about loneliness if they are unaware of resources for referral or feel incapable of improving their patient’s loneliness.
Yet not initiating these conversations may increase the shame individuals feel surrounding loneliness and prevent needed intervention (Jovicic et al., 2019). Thus, the collaborative care model, whereby primary care providers work in teams with psychiatrists and behavioral health care managers, may be a particularly effective approach to monitoring and preventing increases in loneliness among older couples experiencing cognitive decline. Loneliness can be screened with brief measures, such as those used in this study, and may be an important assessment along with brief cognitive screeners for use with older patients. This is particularly important to include in screening processes as loneliness might exacerbate the symptomatology arising from dementia (Hsiao, Chang, & Gean, 2018). Measurement of loneliness could be integrated in the collaborative care model where patient goals and outcomes are regularly measured and assessed.
Limitations
While our study has the benefit of a large nationally representative sample of older couples followed over time, there are several caveats that should be noted. First, our operationalization of CIND is based on the Langa-Weir classification of “cognitive impairment no dementia” (a score of 7 to 11 on a 27-point scale) (Langa, Weir, Kabeto, & Sonnega, 2018). While these classifications were based on diagnostic categories from a more comprehensive screening study, our classification (and the fidelity and separability of individuals on the border between categories) may not align with a diagnosis of mild CIND, and participant’s scores could fall anywhere within a range to be classified as having CIND. Next, for simplicity of analysis and interpretation, same sex partnerships were excluded from our model and thus results may not be generalizable to such partnerships. Despite the large, nationally representative sample, there was a relatively small number of couples in the TCIND group which may limit our ability to detect a gender difference. Further, transition to dementia could not be used as a contrast group in our analyses due to the very small number of participants making this transition. Another contrast group that would be fruitful to consider in future studies is progression to another serious illness to determine whether the transition is unique to cognitive decline or a more general phenomenon of physical illness.
Similarly, future studies may extend our findings with a broader measure of loneliness that may detect greater variation and over shorter follow-up intervals to explore the trajectories of change in loneliness. Given a clear increase in loneliness among partners of a spouse who TCIND after accounting for demographic and health controls, future work should explore potential mechanisms that explain this change, for example, whether receipt of social support, the social integration of the couple, and contact with family and friends change with spouse’s early stage cognitive decline that in turn leads to increases in loneliness.
Conclusion
In conclusion, in a nationally representative sample of older couples, we find that relative to couples who stay cognitively normal over time, in couples in which one person TCIND, this transition is impactful on their spouse’s experience of loneliness. This increase in loneliness over time was consistent for both husbands and wives, with a particularly sharp increase in loneliness four to eight years following the spouse TCIND. In comparing risk factors for poor health, Holt-Lunstad, Smith, & Layton (2010) found that having strong social relationships and quitting smoking were equivalent in their impact on health. Thus, intervening early to help older individuals stay resilient, particularly those whose partner is showing signs of CI, may improve well-being in the dyad and have great public health benefit.
Acknowledgments
Support for this work was provided by the Michigan Center for Contextual Factors in Alzheimer’s Disease (MCCFAD) (P30 AG059300–01). This research was partly supported by awards from the National Institute on Aging (K01AG056557 for Leggett, R03AG054705–01A1 for Chopik, K01AG057820 for Choi, and R01AG061118 for Liu).
Contributor Information
Amanda N. Leggett, Department of Psychiatry, University of Michigan.
HwaJung Choi, Department of Internal Medicine, University of Michigan, Survey Research Center, Institute for Social Research.
William J. Chopik, Department of Psychology, Michigan State University.
Hui Liu, Department of Sociology, Michigan State University.
Richard Gonzalez, Department of Psychology and Statistics, University of Michigan.
References
- Aartsen M & Jylhӓ M (2011). Onset of loneliness in older adults: Results of a 28 year prospective study. European Journal of Ageing, 8, 31–38. 10.1007/s10433-011-0175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auyeung TW, Kwok T, Lee J, Leung PC, Leung J, & Woo J (2008). Functional decline in cognitive impairment- The relationship between physical and cognitive function. Neuroepidemiology, 31, 167–173. 10.1159/000154929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeson RA (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17(3), 135–143. 10.1016/S0883-9417(03)00057-8 [DOI] [PubMed] [Google Scholar]
- Bernard J (1972). The Future of Marriage. New Haven, CT: Yale University Press. [Google Scholar]
- Buecker S, Maes M, Denissen JJA, & Luhmann M (2020). Loneliness and the big five personality traits: A meta-analysis. European Journal of Personality, 34, 8–28. 10.1002/per.2229 [DOI] [Google Scholar]
- Cacioppo JT, & Cacioppo S (2014). Older adults reporting social isolation or loneliness show poorer cognitive function 4 years later. Evid Based Nurs, 17(2), 59–60. 10.1136/eb-2013-101379 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, & Hawkley LC (2009). Perceived social isolation and cognition. Trends Cogn Sci, 13(10), 447–454. 10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging, 25(2), 453–463. 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA (2006). Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140–151. 10.1037/0882-7974.21.1.140 [DOI] [PubMed] [Google Scholar]
- Chen Y, & Feeley TH (2013). Social support, social strain, loneliness, and well-being among older adults: An analysis of the Health and Retirement Study*. Journal of Social and Personal Relationships, 31(2), 141–161. 10.1177/0265407513488728 [DOI] [Google Scholar]
- Choi H, Schoeni RF, Martin LG, & Langa KM (2018). Trends in the Prevalence and Disparity in Cognitive Limitations of Americans 55–69 Years Old. J Gerontol B Psychol Sci Soc Sci, 73(suppl_1), S29–s37. 10.1093/geronb/gbx155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Langa KM, & Weir DR (2011). Assessment of Cognition Using Surveys and Neuropsychological Assessment: The Health and Retirement Study and the Aging, Demographics, and Memory Study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66B(Supplement 1), i162–i171. 10.1093/geronb/gbr048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg L & McKee KJ (2014). Correlates of social and emotional loneliness in older people: evidence from an English community study. Aging & Mental Health, 18(4), 504–514, 10.1080/13607863.2013.856863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong Gierveld J, Van Tilburg T, & Dykstra PA (2006). Loneliness and social isolation In Perlman D & Vangelisti A (Eds.), The Cambridge handbook of personal relationships. Cambridge, UK: Cambridge University Press. [Google Scholar]
- DiTommaso E, Brannen C, & Best LA (2004). Measurement and Validity Characteristics of the Short Version of the Social and Emotional Loneliness Scale for Adults. Educational and Psychological Measurement, 64(1), 99–119. 10.1177/0013164403258450 [DOI] [Google Scholar]
- Dykstra PA, van Tilburg TG, & Gierveld J de J. (2005). Changes in Older Adult Loneliness: Results From a Seven-Year Longitudinal Study. Research on Aging, 27(6), 725–747. 10.1177/0164027505279712 [DOI] [Google Scholar]
- Ekwall AK, Sivberg B, & Hallberg IR (2005). Loneliness as a predictor of quality of life among older caregivers. Journal of Advanced Nursing, 49(1), 23–32. 10.1111/j.1365-2648.2004.03260.x [DOI] [PubMed] [Google Scholar]
- Elder GH, Johnson MK, & Crosnoe R (2003). The emergence and development of life course theory In Mortimer JT & Shanahan MJ (Eds.), Handbooks of Sociology and Social Research. Boston, MA: Springer. [Google Scholar]
- Ellaway A, Wood S, & MacIntyre S (1999). Someone to talk to? The role of loneliness as a factor in the frequency of GP consultations. British Journal of General Practice, 49, 363–367. [PMC free article] [PubMed] [Google Scholar]
- Evans D, & Lee E (2013). Impact of dementia on marriage: A qualitative systematic review. Dementia, 13(3), 330–349. 10.1177/1471301212473882 [DOI] [PubMed] [Google Scholar]
- Forster F, Pabst A, Stein J, Rohr S, Lobner M, Heser K, … Riedel-Heller SG (2019). Are older men more vulnerable to depression than women after losing their spouse? Evidence from three German old-age cohorts (AgeDifferent.de platform). J Affect Disord, 256, 650–657. 10.1016/j.jad.2019.06.047 [DOI] [PubMed] [Google Scholar]
- Greenwood N, Pound C, Brearley S, & Smith R (2019). A qualitative study of older informal carers’ experiences and perceptions of their caring role. Maturitas, 124, 1–7. 10.1016/j.maturitas.2019.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gum A, Shiovitz-Ezra S, & Ayalon L (2017). Longitudinal associations of hopelessness and loneliness in older adults: Results from the US health and retirement study. International Psychogeriatrics, 29(9), 1451–1459. 10.1017/S1041610217000904 [DOI] [PubMed] [Google Scholar]
- Holdsworth K, & McCabe M (2018). The impact of younger-onset dementia on relationships, intimacy, and sexuality in midlife couples: a systematic review. International Psychogeriatrics, 30(1), 15–29. 10.1017/S1041610217001806 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7(7), e1000316 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao YH, Chang CH, & Gean PW (2018). Impact of social relationships on Alzheimer’s memory impairment: mechanistic studies. Journal of biomedical science, 25(1), 3 10.1186/s12929-018-0404-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res Aging. 2004;26(6):655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hultsch DF, Hertzog C, Small BJ, & Dixon RA (1999). Use it or lose it: Engaged lifestyle as a buffer of cognitive decline in aging? Psychology and Aging, 14(2), 245–263. 10.1037/0882-7974.14.2.245. [DOI] [PubMed] [Google Scholar]
- Jovicic A & McPherson S (2019). To support and not to cure: General practitioner management of loneliness. Health and Social Care in the Community, 00, 1–9. 10.1111/hsc.12869. [DOI] [PubMed] [Google Scholar]
- Korporaal M, Broese van Groenou MI, & van Tilburg TG (2008). Effects of Own and Spousal Disability on Loneliness Among Older Adults. Journal of Aging and Health, 20(3), 306–325. 10.1177/0898264308315431 [DOI] [PubMed] [Google Scholar]
- Langa KM, Weir DM, Kabeto M, & Sonnega A (2018). Langa-Weir classification of cognitive function (1995 Onward). Survey Research Center, Institute for Social Research, University of Michigan; Retrieved from: http://hrsonline.isr.umich.edu/modules/meta/researcher-contributions/langa-weir-classifications/Data_Description_Langa_Weir_Classifications.pdf [Google Scholar]
- Lavela SL, & Ather N (2010). Psychological health in older adult spousal caregivers of older adults. Chronic Illness, 6(1), 67–80. 10.1177/1742395309356943 [DOI] [PubMed] [Google Scholar]
- Legdeur N, Heymans MW, Comijs HC, Huisman M, Maier AB, & Visser PJ (2018). Age dependency of risk factors for cognitive decline. BMC Geriatrics, 18, 187 10.1186/s12877-018-0876-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Zhang Z, Choi S. w., & Langa KM (2019). Marital Status and Dementia: Evidence from the Health and Retirement Study. The Journals of Gerontology: Series B. 10.1093/geronb/gbz087 [DOI] [PMC free article] [PubMed]
- Luo Y, Hawkley LC, Waite LJ, & Cacioppo JT (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine, 74(6), 907–914. 10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson S, Byng R, & Oxley D (2014). Treatment resistant depression in primary care: Co-constructing difficult encounters. Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine, 18(3), 261–278. 10.1177/1363459313497607 [DOI] [PubMed] [Google Scholar]
- Mejía ST, & Gonzalez R (2017). Couples’ Shared Beliefs About Aging and Implications for Future Functional Limitations. The Gerontologist, 57(suppl_2), S149–S159. 10.1093/geront/gnx071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz DJ, Kasl SV, & Ostfeld AM (1992). The Health Impact of Living with a Cognitively Impaired Elderly Spouse: Blood Pressure, Self-Rated Health, and Health Behaviors. Journal of Aging and Health, 4(2), 244–267. 10.1177/089826439200400205 [DOI] [Google Scholar]
- Ofstedal MB, Fisher GG, & Herzog AR (2005). Documentation of cognitive functioning measures in the Health and Retirement Study. Ann Arbor, MI: University of Michigan, 10. [Google Scholar]
- Ory MG, Hoffman RR III, Yee JL, Tennstedt S, & Schulz R (1999). Prevalence and Impact of Caregiving: A Detailed Comparison Between Dementia and Nondementia Caregivers. The Gerontologist, 39(2), 177–186. 10.1093/geront/39.2.177 [DOI] [PubMed] [Google Scholar]
- Peplau LA, & Perlman D (1982). Loneliness: A sourcebook of current theory, research and therapy. New York: John Wiley and Sons. [Google Scholar]
- Perissinotto CM, Stijacic Cenzer I, & Covinsky KE (2012). Loneliness in Older Persons: A Predictor of Functional Decline and Death. JAMA Internal Medicine, 172(14), 1078–1084. 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M & Sorensen S (2001)s Influences on Loneliness in Older Adults: A Meta-Analysis. Basic and Applied Social Psychology, 23(4), 245–266, 10.1207/S15324834BASP2304_2 [DOI] [Google Scholar]
- Revenson TA, Griva K, Luszczynska A, Morrison V, Panagopoulou E, Vilchinsky N, & Hagedoom M (2016). Gender and caregiving: The costs of caregiving for women In Caregiving in the Illness Context (pp. 48–63). London: Palgrave Pivot. [Google Scholar]
- Rico-Uribe LA, Caballero FF, Martin-Maria N, Cabello M, Ayuso-Mateos JL, & Miret M (2018). Association of loneliness with all-cause mortality: A meta-analysis. PLoS One, 13(1), e0190033 10.1371/journal.pone.0190033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure. Journal of Personality Assessment, 66(1), 20–40. [DOI] [PubMed] [Google Scholar]
- Smith J, Ryan L, Fisher GG, Sonnega A, & Weir D (2016). Psychosocial and Lifestyle Questionnaire 2006–2016. Retrieved from Ann Arbor, MI: https://hrs.isr.umich.edu/sites/default/files/biblio/HRS%202006-2016%20SAQ%20Documentation_07.06.17_0.pdf [Google Scholar]
- Solway E, Piette J, Kullgren J, Singer D, Kirch M, & Malani P (2019). Loneliness and health. Retrieved from http://hdl.handle.net/2027.42/148147
- Theeke Laurie. A. (2010). Sociodemographic and health-related risks for loneliness and outcome differences by loneliness status in a sample of U.S. older adults. Research in Gerontological Nursing, 3, 113–125. 10.3928/19404921-20091103-99 [DOI] [PubMed] [Google Scholar]
- Tomaka J, Thompson S, & Palacios R (2006). The Relation of Social Isolation, Loneliness, and Social Support to Disease Outcomes Among the Elderly. Journal of Aging and Health, 18(3), 359–384. 10.1177/0898264305280993 [DOI] [PubMed] [Google Scholar]
- Umberson D, Williams K, & Thomeer M (2013). Family status and mental health: Recent advances and future directions In Aneshensel C & Phelan JC (Eds.), Handbook of the Sociology of Mental Health (pp. 405–431): Springer. [Google Scholar]
- Vitaliano PP, Murphy M, Young HM, Echeverria D, & Borson S (2011). Does Caring for a Spouse with Dementia Promote Cognitive Decline? A Hypothesis and Proposed Mechanisms. Journal of the American Geriatrics Society, 59(5), 900–908. 10.1111/j.1532-5415.2011.03368.x [DOI] [PubMed] [Google Scholar]
- Williams K, & Umberson D (2004). Marital status, marital transitions, and health: a gendered life course perspective. J Health Soc Behav, 45(1), 81–98. 10.1177/002214650404500106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, et al. Loneliness and Risk of Alzheimer Disease. Archives of General Psychiatry. 2007;64(2):234–240. 10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes de Leon CF, Barnes LL, et al. (2002). Participation in Cognitively Stimulating Activities and Risk of Incident Alzheimer Disease. JAMA. 287(6),742–748. 10.1001/jama.287.6.742 [DOI] [PubMed] [Google Scholar]
- Wilson C, & Moulton B (2010). Loneliness among older adults: A national survey of adults 45+. Washington, DC: [Google Scholar]
- Zimmerman MK, Litt JS, & Bose CE (2006). Global dimensions of gender and carework. Stanford, CA: Stanford University Press. [Google Scholar]