Abstract
Background:
Trauma quality improvement (QI) has resulted in decreased trauma mortality and morbidity in high-income countries and has the potential to do the same in low-and middle-income countries. Effective implementation of QI programs relies on a foundational culture of patient safety; however, studies on trauma-related patient safety culture in Sub-Saharan Africa remain scarce. This study assesses baseline patient safety culture in Cameroon to best identify opportunities for improvement.
Materials and Methods:
Over a 3-week period, the Hospital Survey on Patient Safety Culture (HSOPSC) was administered in 3 hospitals in the Littoral region of Cameroon. Percentages of positive responses (PPRs) were calculated across 42 items in 12 survey dimensions. A mixed-effects logistic regression model was used to summarize dimension-level percentages and confidence intervals.
Results:
A total of 179 trauma-related hospital personnel were surveyed with an overall response rate of 76.8%. High PPRs indicate favorable patient safety culture. Of the 12 dimensions evaluated by the HSOPSC, 9 had a PPR below 50%. Dimensions particularly pertinent in the context of quality improvement include Non-Punitive response to Errors with a PPR of 25.8% and Organization Learning—Continuous Improvement with a PPR of 64.7%.
Conclusion:
The present study elucidates an opportunity for the development of trauma patient safety culture in Cameroon. Low PPR for Non-punitive Response to Errors indicates a need to shift cultural paradigms from ascribing individual blame to addressing systemic shortcomings of patient care. Moving forward, data from this study will inform interventions to cultivate patient safety culture in partnering Cameroonian hospitals.
Keywords: Trauma, Quality improvement, Patient safety culture, Survey, Low-and middle-income countries, Cameroon
Introduction:
Trauma remains one of the leading causes of death worldwide. Of the nearly six million injury-related deaths that occur each year globally, over 90% occur in low- and middle-income countries (LMICs).1,2 Trauma-related mortality and morbidity continues to grow with the increasing use of motor vehicles, inadequate road infrastructures, and limited traffic and occupational safety legislation.3–5 Although deaths due to trauma exceed that of HIV, malaria, and tuberculosis combined, the issue has not received adequate prioritization as a global health epidemic.6
It is estimated that improvements in trauma care in LMICs could save two million lives each year.7 Sub-Saharan Africa (SSA), in particular Cameroon, is heavily impacted by trauma-related mortality and represents an important target for quality improvement (QI).6,8,9 Effective implementation of QI programs is best facilitated by developing a central culture of quality and patient safety, which encompasses the collective attitudes, values, and expectations of hospital personnel to reduce medical errors and adverse events.10,11 As described by the Institute of Medicine, progress in patient safety requires a movement away from assigning blame to individuals and encouraging the scrutinization of underlying, systemic causes of medical error.12,13 The development of a robust patient safety culture is a crucial step to improving healthcare systems, and measuring the existing patient safety culture amongst hospital personnel is the first step to identifying areas for improvement.14
Studies on trauma-related patient safety culture in SSA are scarce, and there is currently no baseline data on patient safety culture in Cameroonian hospitals.15–19 The majority of existing studies assessing patient safety culture amongst hospital personnel in SSA countries have been qualitative.16,18 Although these studies may provide more detailed knowledge on the intricacies of patient safety culture, quantitative approaches allow for serial evaluations to track improvements following interventions to strengthen patient safety culture.
As part of an effort to introduce hospital-based trauma QI initiatives in Cameroon, we sought to evaluate patient safety culture in three partnering Cameroonian hospitals using the Hospital Survey on Patient Safety Culture (HSOPSC) developed by the Agency for Healthcare Research and Quality (AHRQ). This tool has been applied and validated in various countries and settings, and has demonstrated to be useful in identifying shortcomings and strengths in hospital staff patient safety culture.13 The aim of this study was to obtain a baseline assessment of existing patient safety culture strengths and weaknesses, which will be used to build trauma quality improvement initiatives.
Materials and Methods
Study Design and Setting
A cross-sectional approach was used to assess patient safety culture amongst healthcare professionals involved in trauma patient care at three francophone hospitals in the Littoral region of Cameroon. Cameroon is a low-income country, with a GDP per capita of 1533.7 USD (2018).20 The Littoral region has an estimated population of 3.3 million, with 124 inhabitants per square kilometer.21,22 The selected hospitals included a small-capacity mission hospital, a medium-sized regional referral hospital, and a large-capacity tertiary hospital. These are three of four hospitals currently participating in a long-term trauma quality improvement initiative with the Cameroonian Ministry of Public Health, University of Buea, and University of California, Los Angeles to improve trauma patient outcomes in Cameroon. The remaining location could not be evaluated due to safety concerns during the time of the study. A validated French version of the HSOPSC was administered throughout the month of June 2019.
Study Instrument
The HSOPSC assesses patient safety culture using 42 items across 12 dimensions.These dimensions include Overall Perceptions of Patient Safety, Communication Openness, Feedback & Communication About Error, Teamwork Within Units, Teamwork Across Units, Handoffs & Transitions, Supervisor/Manager Expectations & Actions Promoting Patient Safety, Management Support for Patient Safety, Non-punitive Response to Errors, Staffing, Organizational Learning—Continuous Improvement, and Frequency of Events Reported. Each of these dimensions consists of several positively or negatively worded individual questionnaire items that respondents assess on a 5-point Likert scale. Indicators of strong patient safety culture include attitudes of shared responsibility, transparent and non-punitive error reporting, support of leadership, and effective communication within and across functional hospital units.23 The French translation of HSOPSC has been validated and applied in France.24 It has also been applied in Tunisia, another francophone LMIC.25
Study Sample
The target population of this study included all hospital personnel who were directly involved in trauma patient care. The criteria captured various roles, including physicians, nurses, nurse aides, and “other” personnel, such as care technicians and support staff. Departments involved in trauma patient care included Surgery (General, Orthopedic, Urology, and Otolaryngology), Emergency Medicine, Intensive Care Unit (ICU), Anesthesiology, and Unspecified (no department-specific job assignment). Personnel who were on extended administrative leave, post-graduate resident interns, or rotating medical students were excluded from participating in the survey study.
Survey Procedure
A list of personnel in each trauma-related department at the medium and large-capacity hospital was generated by the respective department’s Charge Nurse according to the inclusion criteria. Due to the small capacity and rural context of the mission hospital, personnel are assigned to various departments on a rotating basis, and trauma patients often require an “all hands-on-deck” approach. The roster to be surveyed therefore included all hospital personnel involved in patient care and was generated by the hospital’s Chief Medical Officer. The total survey population size was determined by totaling the numbers from each department roster. Written informed consent was obtained from all participants in the study. Self-administered questionnaires were completed anonymously by study participants and turned in to the respective departments’ Charge Nurse or directly to study administrators upon completion.
Data Analysis
Responses were interpreted per AHRQ standards by calculating percentage of positive responses (PPR) for each of the 42 items. A positive response on the Likert scale was defined as a 4 or 5 for positively worded items such as “We are actively doing things to improve patient safety” and 1 or 2 for negatively worded questions such as “We have patient safety problems in this unit.26 Higher PPRs are representative of stronger patient safety culture. Composite PPRs for each of the 12 dimensions were generated by summing the total number of positive responses in the dimension and dividing it by the total number of responses in the dimension. In order to compute confidence intervals for the dimensions, which were comprised of multiple items, a mixed-effects logistic regression model was used.
Differences in the PPRs between demographic groups for each dimension were assessed using mixed-effects logistic regression. Reported p-values are based on an omnibus test for differences in the proportions across groups, with significant findings (p < 0.05) indicating that one or more groups demonstrate a reliably different proportion of positive responses.
Every two years, the AHRQ publishes HSOPSC data, most recently in 2018, with data from 630 US Hospitals and 382,834 respondents. Given the extensive history of HSOPSC data collection since the conception of the AHRQ in 2005, the dataset is used as a benchmark for US and other high-income country hospitals to evaluate their own patient safety culture. In this study, we present Cameroonian data alongside US data for context. However, this data is not meant to encourage direct comparison, which would not be appropriate between hospitals of different resources and culture.27
Ethical Approval
Ethical clearance was provided by the University of California, Los Angeles Institutional Review Board and the University of Buea Institutional Review Board. A signature and hospital approval seal was provided by the hospital directors at each site for administrative clearance to conduct the surveys.
Results
Study Participant Characteristics
Across the three sites, out of 233 trauma-related hospital personnel, a total of 179 (76.8%) were surveyed (Table 1). There were 21 (11.7%) participants from the mission hospital, 40 (22.3%) from the regional referral hospital, and 118 (65.9%) from the large-capacity tertiary hospital. The largest proportion of respondents came from the Emergency department (44.6%), followed by Surgery (27.4%). By role, the largest group of respondents were nurses (53.7%), followed by physicians (19.2%).
Table 1:
Demographic characteristics of study participants (N=179)
| Department/Unit | N | % |
|---|---|---|
| Surgery | 48 | 27.4% |
| Emergency | 78 | 44.6% |
| Anesthesiology | 14 | 8.0% |
| Intensive Care Unit | 14 | 8.0% |
| Unspecified * | 21 | 12.0% |
| Role in Unit | ||
| Physician | 34 | 19.2% |
| Nurse | 95 | 53.7% |
| Caretaker | 30 | 16.9% |
| Patient transport | 14 | 7.9% |
| Other ** | 4 | 2.3% |
| Experience in role | ||
| <1 yr | 19 | 10.8% |
| 1 – 2 yrs | 30 | 17.0% |
| 3 – 4 yrs | 37 | 21.0% |
| 6 – 10 yrs | 54 | 30.7% |
| 11 + yrs | 36 | 20.5% |
| Experience in hospital | ||
| 1 month - 1 yr | 35 | 19.9% |
| 1 – 2 yrs | 37 | 21.0% |
| 3 – 4 yrs | 33 | 18.8% |
| 6+ yrs | 71 | 40.3% |
| Experience in unit | ||
| 1 month - 1 yr | 51 | 29.0% |
| 1 – 2 yrs | 65 | 36.9% |
| 3 – 4 yrs | 26 | 14.8% |
| 6+ yrs | 34 | 19.3% |
| Hospital | ||
| Mission Hospital | 21 | 11.7% |
| Regional Referral Hospital | 40 | 22.3% |
| Tertiary Hospital | 118 | 65.9% |
Personnel without specified departmental affiliation
Additional trauma care personnel including care technicians and support staff
HSOPSC Response Overview
Overall dimension-level scores showed that Staffing, which includes items evaluating the appropriateness of staff workload, had the lowest PPR at 24.1% (Table 2). The second-lowest PPR occurred in Non-Punitive Response to Error with a PPR of 25.8%. Meanwhile, Teamwork within Units had the highest score at 65.1%, followed by Organizational Learning for Continuous Improvement at 64.7%. Of the 12 dimensions evaluated, three had a majority of participants providing positive responses. With regards to Patient Safety Grade, 60.5% of respondents rated their hospital patient safety as “Acceptable.” Meanwhile, 15.3% gave ratings of “Very Good” or “Excellent,” and 24.2% gave ratings of “Poor” or “Failing.” In terms of error reporting, 70.4% of respondents had not officially reported an adverse event in the past year, while 15.1% reported one to two adverse events.
Table 2:
Percentage of positive responses (PPR) by dimension. 95% CI calculated using mixed-effect logistical regression.
| Survey Item by Dimension | PPR | 95% CI (%) | |
|---|---|---|---|
| 1. Overall Perceptions of Patient Safety | 41.7% | 38.0 | − 45.4 |
| 2. Communication Openness | 42.5% | 37.8 | − 47.2 |
| 3. Feedback & Communication About Error | 48.5% | 43.5 | − 53.5 |
| 4. Teamwork Within Units | 65.1% | 60.6 | − 69.7 |
| 5. Teamwork Across Units | 51.9% | 47.3 | − 56.6 |
| 6. Handoffs & Transitions | 37.9% | 33.4 | − 42.5 |
| 7. Supervisor/Manager Expectations & Actions Promoting Patient Safety | 57.5% | 52.9 | − 62.2 |
| 8. Management Support for Patient Safety | 42.8% | 37.6 | − 48.1 |
| 9. Non-punitive Response to Errors | 25.8% | 21.6 | − 30.0 |
| 10. Staffing | 24.1% | 20.9 | − 27.3 |
| 11. Organizational Learning—Continuous Improvement | 64.7% | 60.5 | − 69.0 |
| 12. Frequency of Events Reported | 46.2% | 40.2 | − 52.2 |
Mixed Effects Logistical Regression
A significant difference existed in PPRs between roles (physician, nurse, caretaker, etc.) for the Communication Openness dimension, with caretakers having the highest PPR at 56.7%, and physicians having the lowest at 35.3% (Figure 1). Significant differences also existed in PPRs between departments (Surgery, ED, Anesthesiology, etc.) for several dimensions, including Feedback & Communication About Error, Teamwork within Units, Handoffs & Transitions, and Frequency of Events Reported. The ICU reported the highest PPR for Feedback and Communication About Error and Teamwork Within Units at 66.7% and 82.1%, respectively. Meanwhile, Anesthesiology reported the lowest PPRs for the same dimensions at 31.0% and 50.0%, respectively. For Handoffs and Transitions, departmentally unspecified personnel from the mission hospital reported the highest PPR at 57.1%, while Anesthesiology had the lowest PPR at 21.4%. Overall, Anesthesiology frequently reported the lowest PPR in dimensions with statistically significant inter-departmental differences.
Figure 1:
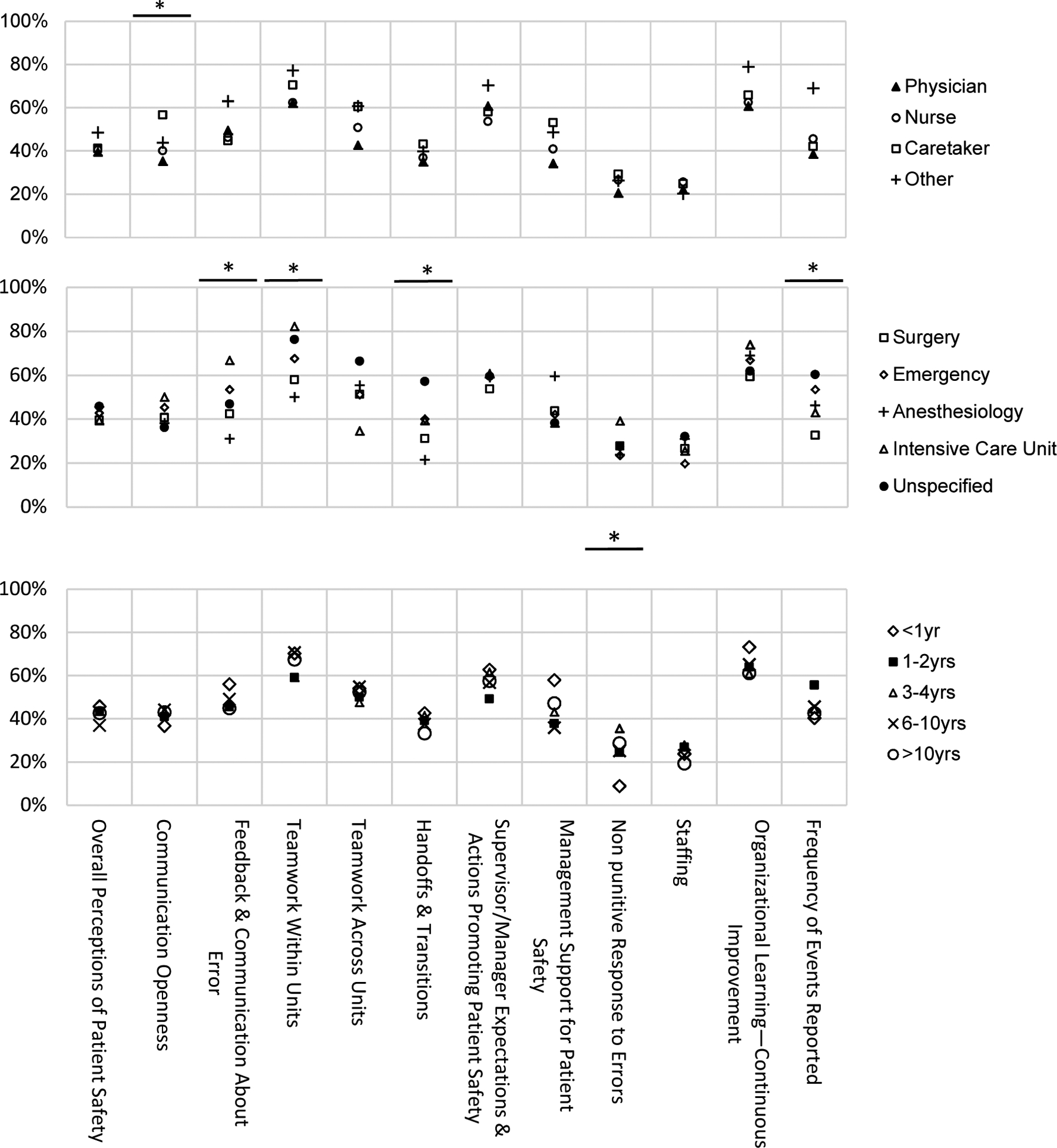
Comparison of percentage of positive responses across 12 dimensions by work role, department, and experience in role.
* P < 0.05, one or more groups demonstrate a reliably different percentage of positive responses.
Amongst groups of staff members divided based on years of experience in their respective roles, significant differences in PPR only existed within the Non-punitive response to error dimension. Interestingly, those with <1yr of experience had the lowest PPR at 8.9%, compared to 3–4 years of experience having the highest PPR of 35.5%.
Discussion
Although many studies have looked into structure, process, and outcome measures of patient safety, few studies quantitatively assess patient safety culture in Sub-Saharan Africa.28 To our knowledge, this is the first study to assess patient safety culture in Cameroon. Our baseline assessment of three Cameroonian hospitals suggests there is a significant opportunity to further develop trauma-related patient safety culture. Of the 12 cultural dimensions assessed, nine had PPRs below 50%. In particular, we found that Staffing had the lowest PPR, meaning that less than a quarter of respondents felt there was adequate staffing to handle the workload required to maintain optimal patient safety. Within this dimension, PPR for the survey statement “We have enough staff to handle the workload” was particularly low at 17.0%. This is consistent with qualitative data on patient safety culture in two East African countries, in which interviewees described being spread too thin and overworked as having major negative impacts on patient safety.18 Although staffing constraints are commonplace in healthcare settings, issues of human resource limitations seem to fall disproportionately on LMICs. Our data reflects staff members’ perception of these limitations, with the largest proportional difference in PPRs between Cameroon and US hospitals (Figure 2).
Figure 2:
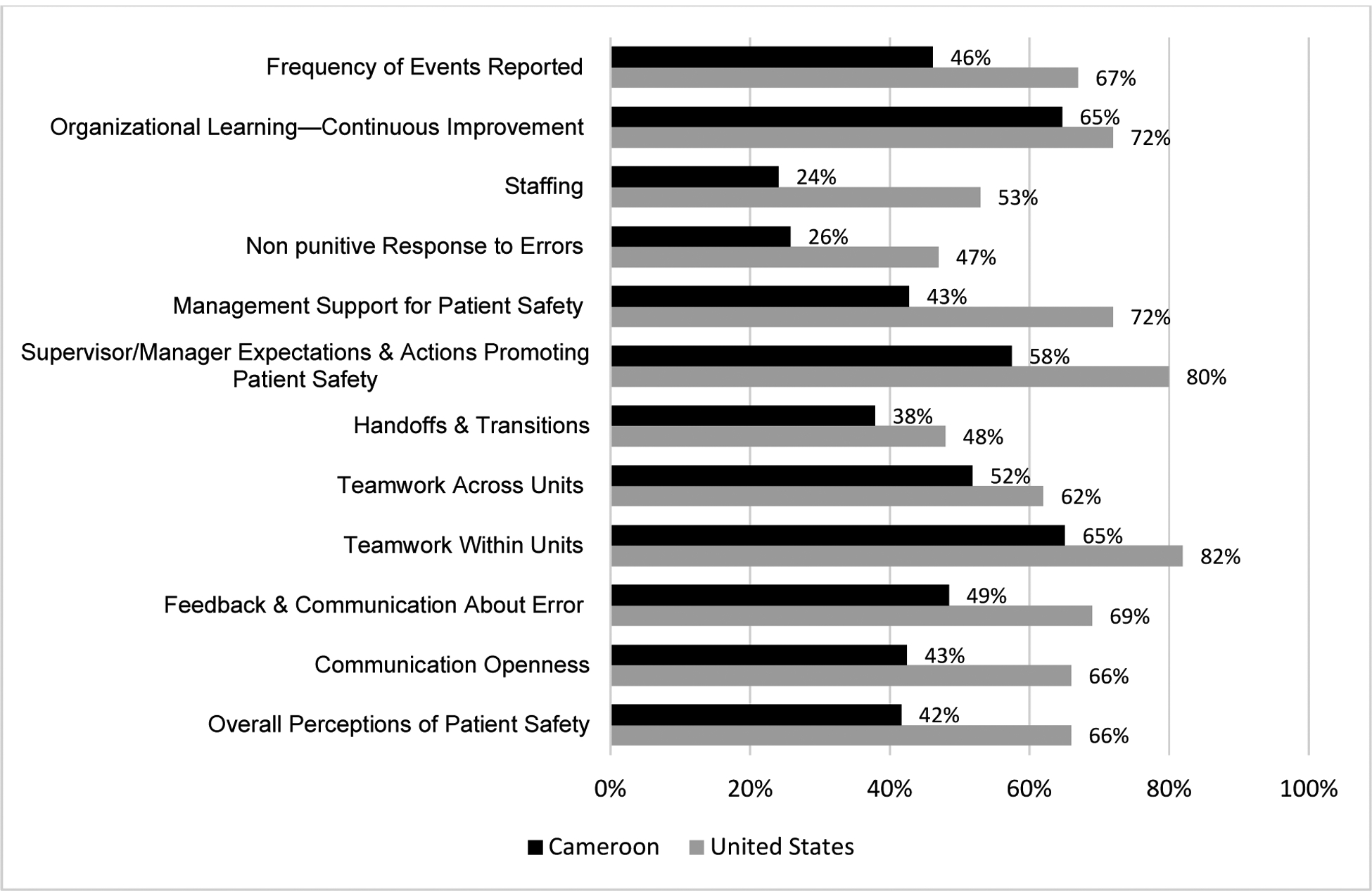
Dimensional Percent Positive Responses from Cameroonian HSOPSC data vs. 2018 United States HSOPSC data
The second-lowest PPR was Non-Punitive Response to Errors, indicating that punitive error culture is still pervasive in trauma care at our partnering Cameroonian hospitals. Interestingly, an HSOPSC study done in Peru showed similar areas of weakness, with the lowest PPR rates reported for Staffing followed by Non-Punitive Response to Error.29 Relative weakness in Non-Punitive Response to Errors is not unique to LMICs, as 2018 US data also showed this dimension to have the lowest PPR. These findings highlight a particular aspect of culture that must be targeted in order for quality improvement initiatives to be successful. Cultures of hierarchy and blame can act as barriers to transparent error reporting and scrutinization of systems-level causes of adverse patient outcomes.16,18 There must be a shift away from assigning blame to healthcare providers and towards a higher level of scrutiny on systemic shortcomings that allowed these errors to occur in the first place. Such a shift in ideology in the healthcare setting was first described by James Reason in his “Swiss cheese model,” which illustrates how many systemic safeguards and defenses must be breached in order for an error to consequently impact patient safety. Errors are ultimately not a consequence of personal failures, but failures on multiple systemic levels, or “slices.”30
However, a culture of punitive error reporting cannot be viewed in isolation from other cultural norms of the healthcare setting. In a recent report, the Care Quality Commission of England recognized that hierarchical culture discourages staff members from speaking out about errors and incidents impacting patient safety.31,32 In our data, we found that “Experience within Role” had significant within-group differences in PPR for Non-Punitive Response to Error, where staff members across all roles with <1 year of experience had the lowest PPR at 8.9%. Although this phenomenon may be due to a self-perceived level of scrutiny amongst new staff members working in a novel environment, it can also be an indication of hierarchical culture in which years of experience denotes seniority amongst staff. Qualitative studies of healthcare staff in the Democratic Republic of Congo and East Africa indicate hierarchical culture is a major factor that negatively impacts patient safety by discouraging transparent error reporting.16,18 Thus, initiatives targeted at improving non-punitive error reporting must be multifaceted and work towards reducing entrenched workplace hierarchies.
On the other hand, survey data revealed some areas of strength in patient safety culture. The higher PPR for Teamwork within Units suggests that a majority of staff members feel cohesive, respected, and supported by others within their department. This dimension of patient safety culture also received the highest PPRs in US hospitals, suggesting that within-group dynamics and cohesiveness may be inherently more conducive to clear communication and teamwork. One variable that had significant within-group variability for Teamwork within Units was at the department level, with ICU having the highest PPR at 82.1%. Although it is difficult to qualitatively extrapolate reasons for the ICU’s particularly high teamwork ratings, some factors cited in studies include: the team-centric and high-pressure nature of ICU patient care, rejection of within-team hierarchies, and reliance on protocols as factors that encourage favorable within-unit teamwork in ICUs.33,34 Such qualities, particularly non-hierarchical, team-based care and a reliance on protocols, can be leveraged and generalized to improve the quality of trauma care.
Lastly, the high PPR for Organizational Learning suggests that interventions to improve patient safety have the potential to gain traction and affect change in Cameroonian hospitals. Traditionally, organizational learning encompasses continued training, performance monitoring, and information gathering in addition to attitudes of self-learning and improvement.35
Additionally, this dimension had the smallest proportional difference when compared to US hospital data. This pre-existing culture of learning amongst trauma care staff at our partnering hospitals can be leveraged to improve other critical aspects of patient safety culture, including Non-Punitive Response to Error, providing a promising foundation on which QI initiatives can be built.
Limitations
Although the French translation of the HSOPSC that we administered has been validated in France and previously applied in Tunisian hospitals it has not been validated in the Cameroonian context.24,25 Additionally, the French survey recommended an assessment of 10 dimensions with 40 items based on results from exploratory analyses.24 We decided to include all 12 dimensions of the French translation per recommendation by AHRQ guidelines.36 Because of the small cohort of our study, internal validity and context-appropriate validation methods could not be properly executed. Larger-scale future studies would be necessary to modify the HSOPSC survey for the Cameroonian context. Another potential limitation was the lack of observation from study administrators for every participant, as some surveys were completed during night shifts and off-hours. Although participants were instructed to complete surveys independently, it is possible that staff members completing the survey in groups could have shared and influenced one another’s’ responses. Survey forms were numbered and completely unidentified to preserve anonymity of respondents. However, a portion of respondents turned in their completed surveys directly to the department’s Charge Nurse, creating a connection between respondent and completed form that may potentially have influenced the way participants responded to various survey items. The higher number of nurses responding to the survey was proportional to the higher number of nurses staffing the respective departments.
Future directions
Our goal is to cultivate QI and patient safety culture amongst a core group of trauma quality improvement committee members and trauma QI fellows in Cameroon through annual intensive training courses and ongoing peer-mentorship. The expectation is that these core individuals will act as epicenters for the implementation of patient safety culture amongst care providers in their respective hospitals and departments. After assessing baseline patient safety culture at our partnering hospitals, the next step is to incorporate patient safety culture training into the existing continued education of QI committee members. The HSOPSC can then be used as a quantitative tool to serially evaluate the effect of these training programs. Finally, supplementation of HSOPSC quantitative survey data with interview-based qualitative studies will allow deeper insights into specific areas of concern, allowing us to address them in a more nuanced fashion.
Conclusion
The present study elucidates a need for the development of trauma patient safety culture in Cameroon. Notably, the particularly low PPR for Non-Punitive Response to Errors indicates a need to shift cultural paradigms from ascribing individual blame to identifying and rectifying systemic shortcomings of patient care. High PPR for Organizational Learning suggests a pre-existing attitude of self-improvement and progress monitoring, characteristics that are essential to the success of QI initiatives. Moving forward, data from this study will inform targeted interventions for cultivating quality and patient safety culture in partnering Cameroonian hospitals.
Highlights:
Effective implementation of QI programs relies on a foundational culture of patient safety
There is opportunity for the development of trauma patient safety culture in Cameroon
Existing cultures of self-improvement and progress monitoring in Cameroon are a promising foundation upon which to facilitate quality improvement initiatives
Acknowledgements:
Authors would like to thank the Cameroonian Ministry of Public Health and individual hospital staff and personnel for both participating in and helping facilitate the execution of this study. Statistics consulting and analysis was provided by the UCLA Clinical and Translational Institute Connections (CTSI).
Funding: This work was supported by the National Institutes of Health [7R21TW010453-02].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Declarations of interest: none
References
- 1.Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22(1):3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Injuries and Violence: The Facts. Geneva: World Health Orgnization;2010. [Google Scholar]
- 3.Global Status Report on Road Safety 2018. Geneva: World Health Organization;2018. [Google Scholar]
- 4.Global status report on road safety: supporting a decade of action. Geneva: World Health Organization;2013. [Google Scholar]
- 5.Ameratunga S, Hijar M, Norton R. Road-traffic injuries: confronting disparities to address a global-health problem. Lancet. 2006;367(9521):1533–1540. [DOI] [PubMed] [Google Scholar]
- 6.World Health Report 2004 Statistical Annex. Geneva: World Health Organization;2004. [Google Scholar]
- 7.Mock C, Joshipura M, Arreola-Risa C, Quansah R. An estimate of the number of lives that could be saved through improvements in trauma care globally. World J Surg. 2012;36(5):959–963. [DOI] [PubMed] [Google Scholar]
- 8.Chichom Mefire A, Etoundi Mballa GA, Azabji Kenfack M, Juillard C, Stevens K. Hospital-based injury data from level III institution in Cameroon: retrospective analysis of the present registration system. Injury. 2013;44(1):139–143. [DOI] [PubMed] [Google Scholar]
- 9.Hashmi ZG, Haider AH, Zafar SN, et al. Hospital-based trauma quality improvement initiatives: first step toward improving trauma outcomes in the developing world. J Trauma Acute Care Surg. 2013;75(1):60–68; discussion 68. [DOI] [PubMed] [Google Scholar]
- 10.Ali H, Ibrahem SZ, Al Mudaf B, Al Fadalah T, Jamal D, El-Jardali F. Baseline assessment of patient safety culture in public hospitals in Kuwait. BMC Health Serv Res. 2018;18(1):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tereanu C, Sampietro G, Sarnataro F, et al. Survey on patient safety culture in the Republic of Moldova: a baseline study in three healthcare settings. Clujul Med. 2018;91(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adams-Pizarro I, Walker ZA, Robinson J, Kelly S, Toth M. Using the AHRQ Hospital Survey on Patient Safety Culture as an Intervention Tool for Regional Clinical Improvement Collaboratives In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 2: Culture and Redesign ). Rockville (MD)2008. [PubMed] [Google Scholar]
- 13.In: Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human: Building a Safer Health System. Washington (DC)2000. [PubMed] [Google Scholar]
- 14.Stephen Powell DB, Njide Ndili, Christopher Ente. Patient Safety in Africa: A Culture Shift? Patient Safety & Quality Healthcare. Analyses: Patient Safety Web site. https://www.psqh.com/analysis/patient-safety-in-africa-a-culture-shift/. Published 2011. Accessed July 1, 2010, 2019. [Google Scholar]
- 15.Syed SB, Dadwal V, Storr J, et al. Strengthening the evidence-policy interface for patient safety: enhancing global health through hospital partnerships. Globalization and Health. 2013;9(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Labat F, Sharma A. Qualitative study exploring surgical team members’ perception of patient safety in conflict-ridden Eastern Democratic Republic of Congo. BMJ Open. 2016;6(4):e009379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mortell M Is there a Theory – Practice – Ethics gap? A Patient Safety Case Study. International Journal of Africa Nursing Sciences. 2019;10:38–42. [Google Scholar]
- 18.Aveling EL, Kayonga Y, Nega A, Dixon-Woods M. Why is patient safety so hard in low-income countries? A qualitative study of healthcare workers’ views in two African hospitals. Global Health. 2015;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wami SD, Demssie AF, Wassie MM, Ahmed AN. Patient safety culture and associated factors: A quantitative and qualitative study of healthcare workers’ view in Jimma zone Hospitals, Southwest Ethiopia. BMC Health Serv Res. 2016;16:495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.GDP per capita (current US$) - Cameroon. World Bank Group. World Bank national accounts data, and OECD National Accounts data files Web site. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=CM. Published 2019. Accessed February 26, 2020.
- 21.Cameroon, Republic of Cameroon. Thomas Brinkhoff. City Population Web site. http://www.citypopulation.de/Cameroon-Cities.html. Updated 2016-11-13. Accessed 2019-2-26, 2020. [Google Scholar]
- 22.Analyse Thématique: Résumé - Etat et Structures de la popualtion. Burea central de recensemement et des etudes population (BUCREP). http://www.bucrep.cm/index.php/fr/recensements/3eme-rgph/resultats?id=125. Accessed 26 February, 2020.
- 23.El-Jardali F, Dimassi H, Jamal D, Jaafar M, Hemadeh N. Predictors and outcomes of patient safety culture in hospitals. BMC Health Serv Res. 2011;11:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Occelli P, Quenon JL, Kret M, et al. Validation of the French version of the Hospital Survey on Patient Safety Culture questionnaire. Int J Qual Health Care. 2013;25(4):459–468. [DOI] [PubMed] [Google Scholar]
- 25.Mallouli M, Tlili MA, Aouicha W, et al. Assessing patient safety culture in Tunisian operating rooms: A multicenter study. Int J Qual Health Care. 2017;29(2):176–182. [DOI] [PubMed] [Google Scholar]
- 26.Jones KJ, Skinner A, Xu L, Sun J, Mueller K. The AHRQ Hospital Survey on Patient Safety Culture: A Tool to Plan and Evaluate Patient Safety Programs In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 2: Culture and Redesign). Rockville (MD)2008. [PubMed] [Google Scholar]
- 27.Hospital Survey on Patient Safety Culture: 2018 User Database Report. Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; March 2018. [Google Scholar]
- 28.Carpenter KB, Duevel MA, Lee PW, et al. Measures of patient safety in developing and emerging countries: a review of the literature. Qual Saf Health Care. 2010;19(1):48–54. [DOI] [PubMed] [Google Scholar]
- 29.Arrieta A, Suarez G, Hakim G. Assessment of patient safety culture in private and public hospitals in Peru. Int J Qual Health Care. 2018;30(3):186–191. [DOI] [PubMed] [Google Scholar]
- 30.Reason J Human error: models and management. BMJ. 2000;320(7237):768–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brennan PA, Davidson M. Improving patient safety: we need to reduce hierarchy and empower junior doctors to speak up. BMJ. 2019;366:l4461. [DOI] [PubMed] [Google Scholar]
- 32.Opening the door to change. Care Quality Commission; December 2018. 2018. [Google Scholar]
- 33.Reader TW, Cuthbertson BH. Teamwork and team training in the ICU: where do the similarities with aviation end? Crit Care. 2011;15(6):313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ervin JN, Kahn JM, Cohen TR, Weingart LR. Teamwork in the intensive care unit. Am Psychol. 2018;73(4):468–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singer SJ, Benzer JK, Hamdan SU. Improving health care quality and safety: the role of collective learning. J Healthc Leadersh. 2015;7:91–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.AHRQ Hospital Survey on Patient Safety Culture: User’s Guide. Agency for Healthcare Research and Quality; U.S. Department of Health and Human Services; Jul, 2018. 2018. [Google Scholar]


