Abstract
PURPOSE
The purpose of this study was to evaluate acupuncture use among breast cancer survivors, including perceived symptom improvements, and referral patterns.
METHODS
Breast cancer survivors who had used acupuncture for cancer- or treatment-related symptoms were identified using an ongoing prospective Mayo Clinic Breast Disease Registry (MCBDR). Additionally, Mayo Clinic electronic health records (MCEHR) were queried to identify eligible participants. All received a mailed consent form and survey including acupuncture-related questions about acupuncture referrals, delivery, and costs. Respondents were also asked to recall symptom improvements, symptom severity before and after acupuncture treatment, and time to benefit on Likert scales.
RESULTS
Acupuncture use was reported among 415 participants (12.3%) of the MCBDR. Among MCBDR and MCEHR eligible participants, 241 women returned surveys. 193 (82.1%) participants reported a symptomatic benefit from acupuncture and 57 (24.1% of participants reported a “substantial benefit” or “totally resolved my symptoms” (corresponding to 4 and 5 on the 5-point Likert scale). Mean symptom severity decreased by at least 1 point of the 5-point scale for each symptom; the percentage of patients who reported an improvement in symptoms ranged from 56% (lymphedema) to 79% (headache). The majority of patients reported time to benefit as “immediate” (34%) or “after a few treatments” (40.4%). Over half of participants self-referred for treatment, 24.1% were referred by their oncologist. Acupuncture delivery was more frequent in private offices (61.0%) than in hospital or medical settings (42.3%). Twelve participants (5.1%) reported negative side effects, such as discomfort.
CONCLUSIONS
Acupuncture is commonly utilized by patients for a variety of breast cancer-related symptoms. However, patients frequently self-refer for acupuncture treatments and most acupuncture care is completed at private offices, rather than medical clinic or hospital settings.
Background
Breast cancer survivors experience a number of symptoms from cancer and cancer-directed therapy, including hot flashes, arthralgias, fatigue, and neuropathy. Medications, from serotonin antagonists to opioids, are frequently prescribed to help manage these symptoms, but may carry significant side effects. Acupuncture, which has been used to treat various ailments as a component of traditional Chinese medicine since 6000 BCE, is an appealing treatment because it carries few such side effects. Acupuncture research suggests that it is a promising therapy for a variety of cancer-related symptoms.
Acupuncture has been shown to be helpful in treating a number of breast cancer-related symptoms, most notably, for aromatase inhibitor (AI)-induced arthralgias. A large, multi-institution trial found that pain scores significantly decreased by 2 or more points (on a 0–10 scale) in 58% of participants receiving true acupuncture, higher than the 33% of patients in the sham and 31% of patients in the waitlist control arms [1].
Acupuncture has also been reported to improve hot flashes in breast cancer survivors. Two large, multicenter trials have reported that hot flash severity is significantly lower among patients receiving acupuncture, when compared with those receiving usual care [2,3]. Arecent meta-analysis, including 10 randomized controlled trials – five of which included solely breast cancer patients – reported a significant improvement in fatigue among patients receiving acupuncture, when compared to control arms of sham acupuncture or typical care [4]. Non-randomized studies have suggested a benefit for acupuncture for chemotherapy-induced neuropathy [5–7].
Larger sample sizes and multi-center design would help to definitively determine the benefits of acupuncture in treating many symptoms faced by cancer survivors, but acupuncture is gaining national recognition as a viable strategy for cancer symptom management. Acupuncture was the subject of a National Cancer Institute symptom control symposium, and acupuncture use is recommended by National Comprehensive Cancer Network guidelines for a number of symptoms [8]. Furthermore, approximately 10% of patients with cancer have used acupuncture to help mitigate cancer-related symptoms [9].
Despite increasing visibility and data to support the use of acupuncture in the literature, it is unclear whether oncology providers and their patients with breast cancer are using acupuncture to help mitigate their symptoms and how this practice is being adopted. The purpose of the current study was to evaluate whether real-world acupuncture use among patients with breast cancer is aligned with scientific evidence, patient-perceived benefits of acupuncture for a variety of symptoms, and barriers to adoption of acupuncture use among breast cancer survivors.
Despite increasing visibility and data to support the use of acupuncture, it is unclear how this practice is being adopted. The purpose of the current study was to evaluate the perceived benefit of acupuncture for cancer-related symptoms among breast cancer survivors, as well as to describe patterns of acupuncture use, referral, and delivery. This information will allow for an improved understanding as to whether real-world acupuncture use among patients with breast cancer is aligned with scientific evidence.
Materials and Methods
Eligible Participants
This study was approved by the Mayo Clinic Institutional Review Board (IRB). Breast cancer survivors who had used acupuncture were identified using an ongoing prospective Mayo Clinic Breast Disease Registry (MCBDR). MCBDR is a clinic-based registry that enrolls and follows patients with newly diagnosed breast cancer, including both participants on active treatment and those who have completed treatment for their breast cancer. Participants in the MCBDR were contacted and asked to complete questionnaires, provide permission to allow review of their medical records, and to allow access to tumor tissue when available. Questionnaires, given to participants at baseline and in follow-up, ask patients to report breast cancer information and various breast cancer-related symptoms and treatments, including the use of acupuncture. The first follow-up surveys were mailed to MCBDR participants in 2016; subsequent follow-up surveys were mailed to all participants annually. Patients who reported using acupuncture were eligible subjects for this study.
Additional patients were identified using Mayo Clinic electronic health records (MCEHR). Patients who had been treated with acupuncture for the indications of a primary, secondary, or tertiary diagnosis of breast cancer were distinguished by ICD-9 and ICD-10 codes. Also, Mayo Clinic’s Advanced Cohort Explorer, a database that allows for text-based queries of clinical notes, was used to identify unique patients with clinical documentation of a personal history of breast cancer within acupuncture procedure notes.
Living breast cancer survivors with a history of acupuncture utilization, gleaned by the above described sources, were eligible for inclusion in this study and received a mailed consent form and a survey which asked acupuncture-related questions.
Data Collection
Between the data collection period of August 2018 to January 2019, participants were asked to fill out a 19-question survey related to their experience with acupuncture post-cancer diagnosis including, but not limited to: symptoms for which they received the acupuncture, number of treatments, adverse reactions, and out-of-pocket costs (per session and total). Participants that indicated that they never used acupuncture, only used acupuncture prior to their cancer diagnosis, or used acupuncture for symptoms unrelated to their breast cancer were excluded from subsequent analyses. Participants were asked whether acupuncture helped their symptoms, overall, on an investigator created 5-point Likert scale, with responses ranging from “it did not provide any benefit” (corresponding to 1 on the scale) to “it totally resolved my symptoms” (corresponding to 5 on the scale). Respondents were also asked to recall the severity of each of their symptoms: arthralgias, myalgias, post-surgical pain, hot flashes, nausea/vomiting, fatigue, depression, anxiety, insomnia, lymphedema, headache, and neuropathy on an investigator-created Likert scale from 1 to 5 (1=mild, 5=severe) before and after acupuncture treatment. Only participants that provided both pre-and post-severity scores were included in statistical analyses of these questions.
Demographics, breast cancer clinical information, and breast cancer treatment information were self-reported among patients in the MCBDR cohort, as patients in this database receive a majority of their treatment at other facilities, and abstracted from the medical record for patients in the MCEHR cohort.
Statistics
The analyses were retrospective and thus descriptive statistics, such as means/medians and percentages, were primarily utilized to generate hypotheses. Although these analyses were exploratory, inferential statistics were evaluated to facilitate the identification of statistically noteworthy findings that could be highlighted for the assessment of clinical importance and whether such might be worthy of further study. Associations between baseline characteristics and overall perceived benefit were assessed using the chi-squared test. The significance of symptom severity differences was determined by the Wilcoxon signed rank test. P values are two-sided and a bonferroni correction was applied to adjust for multiple comparisons, with a p-value cut-off of 0.003 (i.e., 0.05/13). Data obtained from participants who did not provide pre- and post-severity scores remained missing.
Results
Participant Demographics and Clinical Features
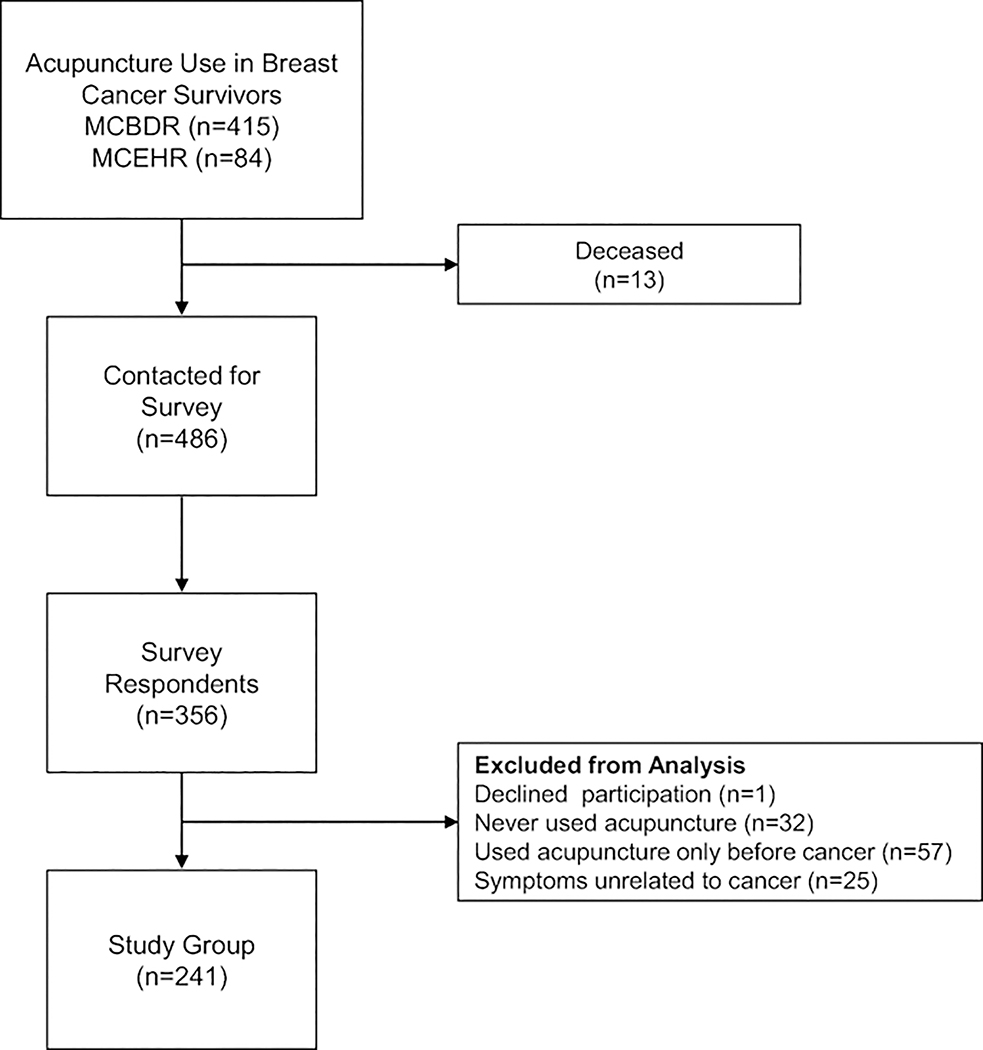
Current or past acupuncture use was reported among 415 participants of the total 3,379 MCBDR enrollees (12.3%). The numbers of eligible participants from each cohort and number of completed surveys are illustrated in Figure 1. The mean age of diagnosis was 50.4 (SD 9.7) with the mean age at survey completion being 58.9 (SD 10.1). Participants in the MCEHR cohort had mean of 2.3±1.6 years between date of last acupuncture therapy at Mayo Clinic and date of survey; three participants in this cohort had a recent acupuncture visit, within 6 months of the survey. Patient characteristics are noted in Table 1. The majority of participants (59.6%) reported they had enough money for special things; 34.9% reported they didn’t have enough money for bills or had little money to spare after bills; 5.5% did not respond to this query.
Figure 1:
Schematic of Participant Selection
There were 486 living breast cancer survivors with previous acupuncture usage that were contacted for this study. 356 responses were received and 241 met inclusion criteria of having used acupuncture for breast cancer or cancer treatment-related symptoms.
Table 1.
Participant Demographics and Breast Cancer Treatments.
| Demographics | n (%) |
|---|---|
| Sex | |
| Female | 241 (100) |
| Male | 0 (0) |
| Race | |
| White | 226 (93.8) |
| Asian Chinese | 3 (1.2) |
| Asian Indian | 1 (0.4) |
| African American | 1 (0.4) |
| American Indian/Alaskan Native | 1 (0.4) |
| Other | 4 (1.7) |
| Ethnicity | |
| Not Hispanic | 223 (92.5) |
| Choose Not to Disclose/Unknown | 18 (7.5) |
| Education | |
| High School Graduate or GED | 22 (9.1) |
| Vocational School | 9 (3.7) |
| Some College of 2-year Degree | 54 (22.4) |
| 4-year College Degree | 70 (29.0) |
| Post Graduate | 81 (33.6) |
| Unknown | 5 (2.1) |
| Religion | |
| Christian | 175 (72.6) |
| Protestant | 85 (35.3) |
| Catholic | 66 (27.4) |
| Other | 24 (10.0) |
| Jewish | 4 (1.7) |
| Hindu | 1 (0.4) |
| No Religious Affiliation | 28 (11.6) |
| Unknown/Prefer Not to Disclose | 33 (13.7) |
| Breast Cancer Clinical Information | |
| Stage | |
| 0 | 30 (12.4) |
| 1 | 82 (34.0) |
| 2 | 88 (36.5) |
| 3 | 28 (11.4) |
| 4 | 10 (4.1) |
| unknown | 3 (1.2) |
| Estrogen Receptor Positive | |
| Yes | 208 (86.3) |
| No | 32 (13.3) |
| Unknown | 1 (0.4) |
| Progesterone Receptor Positive | |
| Yes | 178 (73.9) |
| No | 61 (25.3) |
| Unknown | 2 (0.8) |
| HER2 Amplified | |
| Yes | 38 (15.8) |
| No | 174 (72.2) |
| Unknown | 28 (11.6) |
| Breast Cancer Treatments | n (%) |
| Endocrine Therapy | |
| Yes | 178 (74.2) |
| No | 62 (25.7) |
| Unknown | 1 (0.4) |
| Chemotherapy | |
| Yes | 136 (56.4) |
| No | 105 (43.6) |
| Radiation | |
| Any | 146 (60.6) |
| Breast | 142 (58.9) |
| Other | 8 (3.3) |
| Surgery | |
| Any | 237 (98.3) |
| Breast | 230 (95.4) |
| Lymph Node | 214 (88.8) |
| Reconstruction | 116 (48.1) |
Acupuncture Utilization in Breast Cancer Survivors
The most common symptoms that prompted acupuncture were joint pain, muscle pain, hot flashes, fatigue, and neuropathy (Table 2). Referrals to acupuncture clinics were most frequently made by participants themselves (50.2%), rather than healthcare providers, and the majority of acupuncture was performed at private offices (61.0%; Table 2). Sixty-six participants (27.4%) used acupuncture before and after their cancer diagnosis, and approximately half of participants self-referred for treatment. Treatment frequency was variable; 32.8% were treated 2–3 times per month, 23.2% were treated once per week, and 17.8% were treated once per month. The number of acupuncture treatments was also variable (median: 10, mean: 19.5 (SD 32.6), and range: 1–300). The median cost for participants with an out-of-pocket expense was $60 per treatment, $500 for a total treatment course.
Table 2.
Acupuncture Utilization.
| n (%) | |
|---|---|
| Timing of Acupuncture | |
| Only after diagnosis | 175 (72.6) |
| Before and after diagnosis | 66 (27.4) |
| Learned of Acupuncture from | |
| Friend or relative | 107 (44.4) |
| Medical professional | 111 (46.1) |
| Internet | 17 (7.1) |
| Other | 30 (12.4) |
| Treatment Location(s) a | |
| Private office | 147 (61.0) |
| Hospital or medical setting | 102 (42.3) |
| Spa | 7 (2.9) |
| Other | 15 (6.2) |
| Referral to Acupuncture | |
| Oncologist | 58 (24.1) |
| Primary care or family physician | 13 (5.4) |
| Other healthcare providers | 44 (18.3) |
| Self-referred | 121 (50.2) |
| Frequency | |
| Once | 26 (10.8) |
| Once per month | 43 (17.8) |
| 2–3 times per month | 79 (32.8) |
| Once per week | 56 (23.2) |
| 2–3 times per week | 16 (6.6) |
| Other | 46 (19.1) |
| Symptoms prompting Acupuncture b | |
| Joint pain | 87 (36.1) |
| Muscle pain | 83 (34.4) |
| Post-surgical pain | 45 (18.7) |
| Hot flashes | 80 (33.2) |
| Nausea/vomiting | 42 (17.4) |
| Fatigue | 76 (31.5) |
| Low mood/depression | 39 (16.2) |
| Anxiety | 49 (20.3) |
| Insomnia | 41 (17.0) |
| Lymphedema | 20 (8.3) |
| Headache | 35 (14.5) |
| Neuropathy | 61 (25.3) |
| Other | 30 (12.4) |
| Number of Symptoms Prompting Acupuncture | |
| 1 | 73 (30.3) |
| 2 | 50 (20.7) |
| 3 | 43 (17.8) |
| 4 | 24 (10.0) |
| 5 | 18 (7.5) |
| >5 | 25 (10.4) |
| Did not answer | 8 (3.3) |
Participants asked to mark all that apply
Includes participants that did not indicate the symptom severity
Perceived Benefits of Acupuncture for Breast Cancer-related Symptoms
One hundred and ninety-three (82.1%) participants retrospectively reported a symptomatic benefit from acupuncture overall. Specifically, 57 (24.1%) participants reported substantial improvement or complete resolution of symptoms, corresponding to scores of 4 or 5 out of 5 on the 5-point Likert scale), 81 (33.6%) reported moderate improvement (score of 3) and 54 (22.4%) reported a “little bit” of improvement (score of 2); 42 (17.5%) reported no benefit (score of 1). Neither level of education, stage of disease, chemotherapy usage, endocrine therapy usage, nor radiation treatment was associated with perceived benefit. There was a non-significant trend for participants that had undergone a breast cancer related surgery (with or without lymph node dissection) to perceive an increased benefit with acupuncture in comparison to those that did not have surgery (p=0.05). Participants who had tried acupuncture prior to cancer were more likely to perceive an increased benefit from acupuncture after cancer (p≤ 0.01).
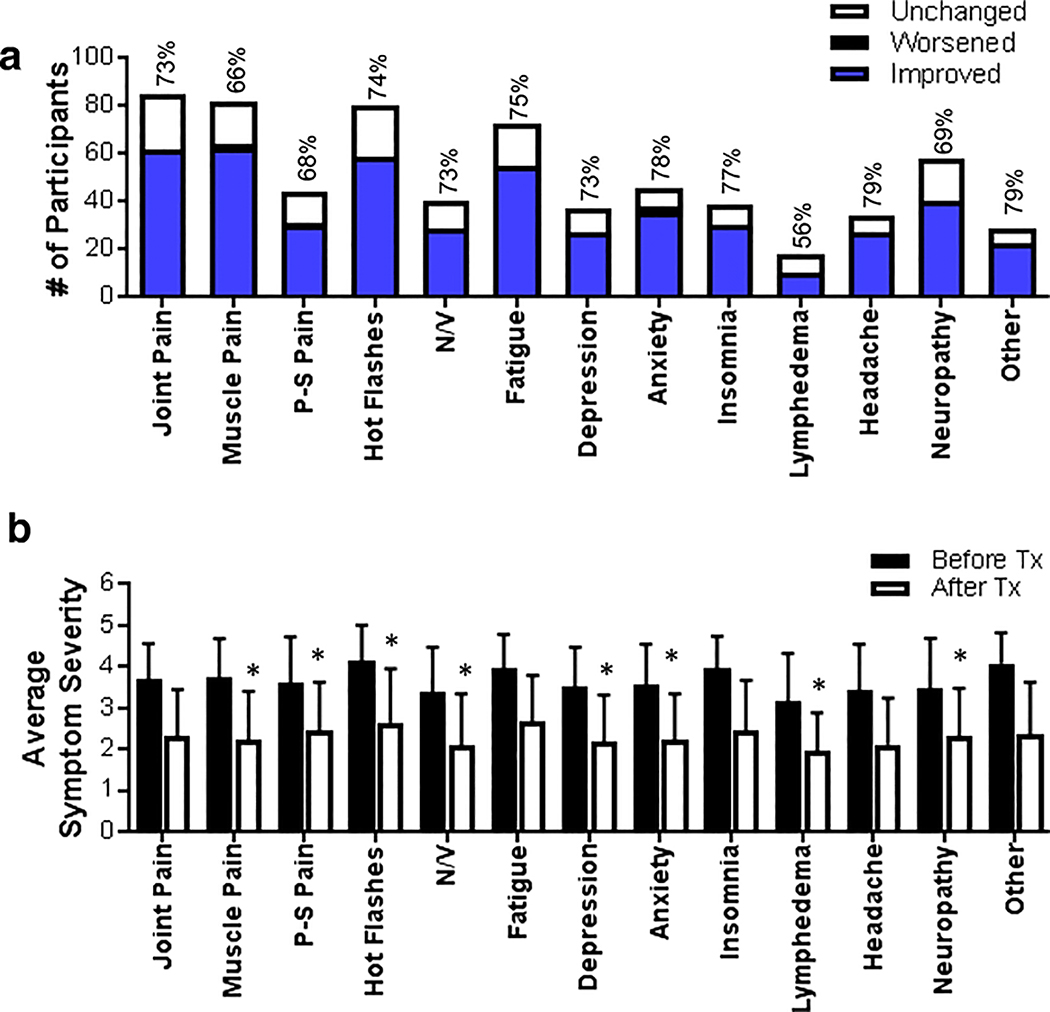
Patients retrospectively reported both pre- and post-acupuncture symptom severity scores, shown in Figure 2A. All symptoms had at least 50% of participants reported a change in severity score of at least 1. Lymphedema had the smallest proportion of patients reporting improvement at 56% whereas headache and “other symptoms” (such as constipation and focal areas of pain, i.e. back pain, leg pain) had the largest proportion of patients reporting improvement at 79%. In addition, mean symptom severity scores decreased from before to after acupuncture by at least 1 point for all queried symptoms (Figure 2B). There was a perceived improvement in muscle pain, post-surgical pain, hot flashes, nausea/vomiting, low mood/depression, anxiety, lymphedema, and neuropathy (p≤0.01).
Figure 2:
Perceived Benefit of Acupuncture in Breast Cancer Survivors. A) Symptoms prompting acupuncture. Change in severity score is represented in blue as an improvement in severity, in black as worsening severity, and in white as no change. Above each bar indicates the percentage of patients that reported symptom improvement (change in severity score of at least 1). B) Mean change in symptom severity score before and after acupuncture (mean ± SD) P-S pain= post-surgical pain; N/V= nausea/vomiting; TX= treatment. * p-value <0.01
Most participants reported time-to-benefit as immediate (34.4%) or after a few treatments (40.2%), few reported benefit after the final treatment (2.1%) or never (19.9%). Twelve participants (5.1%) reported negative side effects, including discomfort.
Discussion
Acupuncture use pervasive among cancer survivors to help mitigate cancer-related symptoms; the frequency and characteristics of real world acupuncture use among patients in this study was even higher than 1 in 10, which was previously reported in the literature [9]. The strength of data supporting the use of acupuncture to manage symptoms related to cancer and cancer-directed therapies is variable, ranging from large, randomized, placebo-controlled clinical trials (AI-induced arthralgias), to small, conflicting studies (neuropathy) [1].
Prior to this study, characteristics of real world acupuncture use among patients with cancer have not previously been well described [9,10]. Despite patient enthusiasm for pursuing acupuncture treatments, and acupuncture gaining national prominence as an efficacious treatment for cancer-related symptoms, fewer than a quarter of patients reported that their healthcare providers referred them for acupuncture; the majority of patients self-referred to acupuncture and received acupuncture in a private office. Perhaps this is because the randomized controlled trial data on acupuncture are relatively new: the largest trial of acupuncture for AI-induced arthralgias was reported in 2017. In addition, pre-existing physician attitudes towards acupuncture may not be enthusiastic. One study surveyed over 1500 practitioners as to how likely they would be to recommend a complementary medicine treatment after reading a vignette reporting its efficacy [11]. Conventional medicine physicians who read a vignette describing the efficacy of glucosamine were significantly more likely to say they would recommend it, compared to those who read the same vignette describing the efficacy of acupuncture. The authors posited that physician attitudes were shaped by physician education and experience with glucosamine, as compared to acupuncture.
Further studies investigating the efficacy of acupuncture may help to improve physician familiarity and knowledge, allowing for data from acupuncture clinical trials to permeate further into conventional medicine practices. The study’s retrospective design and potential for recall bias limit conclusions about the degree of symptom improvement provided by acupuncture. For instance, as the average time between breast cancer diagnosis and survey was eight years (mean time between last acupuncture treatment and survey was two years), interpretations of patient-reported details of symptom improvement should be made with caution. Studies of acupuncture use among cancer survivors at other academic institutions and community sites would help to better clarify the ways in which acupuncture is being utilized in a variety of settings, and use of larger validated instruments would help to supplement the current study’s survey data. However, it is encouraging that nearly all participants reported benefits of acupuncture with minimal side effects. Patient characteristics, such as gender, ethnicity, or BMI, may be associated with positive responses from acupuncture and deserve future study. The data from the present study support that placebo-controlled clinical trials evaluating acupuncture efficacy for symptoms such as fatigue and post-surgical pain are needed.
Acknowledgments
We would like to thank the study participants for their time as well as Melinda Cooper, Tricia Harstad, and Sebastian Armasu for their assistance with data collection.
Funding
This study was supported by Tracy Starr Breast Cancer Research Fund Award (PI: Ruddy). JZ was supported by Mayo Clinic Medical Scientist Training Program (National Institutes of Health, T32 GM065841).
Footnotes
Compliance with Ethical Standards
Disclosure of Potential Conflict of Interest
CLL has a consulting/advisory role with Pled Pharma, Disarm Therapeutics, Metys, and Asahi Kasei. KRJ inherited and then sold Merck and Pfizer stock in February 2018.
Research involving Human Participants and/or Animals
This study was approved by Mayo Clinic Institutional Review Board (IRB) (IRB #s 1815–04 and 18–006395) in accordance with ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Hershman DL, Unger JM, Greenlee H, Capodice J, Lew DL, Darke A, Kengla A, Melnik MK, Jorgensen CW, Kreisle WH, Minasian LM, Fisch MJ, Henry NL, Crew KD (December 2017) Randomized Blinded Sham- and Waitlist-Controlled Trial of Acupuncture for Joint Symptoms Related to Aromatase Inhibitors in Women with Early Stage Breast Cancer (SWOG 1200). Oral Presentation at: San Antonio Breast Cancer Symposium [Google Scholar]
- 2.Kim KH, Kang KW, Kim DI, Kim HJ, Yoon HM, Lee JM, Jeong JC, Lee MS, Jung HJ, Choi SM (2010) Effects of acupuncture on hot flashes in perimenopausal and postmenopausal women--a multicenter randomized clinical trial. Menopause (New York, NY) 17 (2):269–280. doi: 10.1097/gme.0b013e3181bfac3b [DOI] [PubMed] [Google Scholar]
- 3.Lesi G, Razzini G, Musti MA, Stivanello E, Petrucci C, Benedetti B, Rondini E, Ligabue MB, Scaltriti L, Botti A, Artioli F, Mancuso P, Cardini F, Pandolfi P (2016) Acupuncture As an Integrative Approach for the Treatment of Hot Flashes in Women With Breast Cancer: A Prospective Multicenter Randomized Controlled Trial (AcCliMaT). J Clin Oncol 34 (15):1795–1802. doi: 10.1200/jco.2015.63.2893 [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Lin L, Li H, Hu Y, Tian L (2018) Effects of acupuncture on cancer-related fatigue: a meta-analysis. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer 26 (2):415–425. doi: 10.1007/s00520-017-3955-6 [DOI] [PubMed] [Google Scholar]
- 5.Schroeder S, Meyer-Hamme G, Epplee S (2012) Acupuncture for chemotherapy-induced peripheral neuropathy (CIPN): a pilot study using neurography. Acupuncture in medicine : journal of the British Medical Acupuncture Society 30 (1):4–7. doi: 10.1136/acupmed-2011-010034 [DOI] [PubMed] [Google Scholar]
- 6.Bao T, Goloubeva O, Pelser C, Porter N, Primrose J, Hester L, Sadowska M, Lapidus R, Medeiros M, Lao L, Dorsey SG, Badros AZ (2014) A pilot study of acupuncture in treating bortezomib-induced peripheral neuropathy in patients with multiple myeloma. Integrative cancer therapies 13 (5):396–404. doi: 10.1177/1534735414534729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia MK, Cohen L, Guo Y, Zhou Y, You B, Chiang J, Orlowski RZ, Weber D, Shah J, Alexanian R, Thomas S, Romaguera J, Zhang L, Badillo M, Chen Y, Wei Q, Lee R, Delasalle K, Green V, Wang M (2014) Electroacupuncture for thalidomide/bortezomib-induced peripheral neuropathy in multiple myeloma: a feasibility study. Journal of hematology & oncology 7:41. doi: 10.1186/1756-8722-7-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zia FZ, Olaku O, Bao T, Berger A, Deng G, Fan AY, Garcia MK, Herman PM, Kaptchuk TJ, Ladas EJ, Langevin HM, Lao L, Lu W, Napadow V, Niemtzow RC, Vickers AJ, Shelley Wang X, Witt CM, Mao JJ (2017) The National Cancer Institute’s Conference on Acupuncture for Symptom Management in Oncology: State of the Science, Evidence, and Research Gaps. Journal of the National Cancer Institute Monographs 2017 (52). doi: 10.1093/jncimonographs/lgx005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mao JJ, Palmer CS, Healy KE, Desai K, Amsterdam J (2011) Complementary and alternative medicine use among cancer survivors: a population-based study. Journal of cancer survivorship : research and practice 5 (1):8–17. doi: 10.1007/s11764-010-0153-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Enblom A (2017) Patients— and Physiotherapists— Belief in and Use of Acupuncture for Cancer-Related Symptoms. Acupuncture in Medicine 35 (4):251–258. doi: 10.1136/acupmed-2015-011007 [DOI] [PubMed] [Google Scholar]
- 11.Tilburt JC, Miller FG, Jenkins S, Kaptchuk TJ, Clarridge B, Bolcic-Jankovic D, Emanuel EJ, Curlin FA (2010) Factors that influence practitioners’ interpretations of evidence from alternative medicine trials: a factorial vignette experiment embedded in a national survey. Medical care 48 (4):341–348 [DOI] [PMC free article] [PubMed] [Google Scholar]