Abstract
Bile acids are central signals in enterohepatic communication and they also integrate microbiota-derived signals into enterohepatic signaling. The tissue distribution and signaling pathways activated by bile acids through natural receptors, farnesoid X receptor and G protein-coupled bile acid receptor 1 (GPBAR1, also known as TGR5), have led to greater understanding of mechanisms and potential therapeutic agents. Bile acid diarrhea is most commonly encountered in ileal resection or disease, in idiopathic disorders (with presentation similar to functional diarrhea or irritable bowel syndrome with diarrhea), and in association with malabsorption such as chronic pancreatitis or celiac disease. Diagnosis of bile acid diarrhea is based on 75SeHCAT retention, or 48 hour fecal bile acid excretion, or serum 7αC4; the latter being a marker of hepatic bile acid synthesis. Bile acid diarrhea tends to be associated with higher BMI, increased stool weight and stool fat, and acceleration of colonic transit. Biochemical markers of increased bile acid synthesis or excretion are available through reference laboratories. Current treatment of bile acid diarrhea is based on bile acid sequestrants, and, in the future, it is anticipated that FXR receptor agonists may also be effective. The optimal conditions for an empiric trial with bile acid sequestrants as a diagnostic test are still unclear. However, such therapeutic trials are widely used in clinical practice. Some national guidelines recommend definitive diagnosis of bile acid diarrhea over empirical trial.
Keywords: malabsorption, SeHCAT, fecal, serum 7αC4, FGF19, fecal, treatment, diagnosis, FXR, TGR5, sequestrant
INTRODUCTION
Synthesis, Secretion and Circulation of Bile Acids
Bile acids (BAs) are synthesized from cholesterol in the liver; the rate limiting enzyme in the classical pathway of synthesis is 7α-hydroxylase (cytochrome P450 7A1, CYP7A1). The primary bile acids produced in the liver are cholic acid (CA) and chenodeoxycholic acid (CDCA), which are conjugated with taurine and glycine thereby increasing the solubility of the bile acid in bile, excreted in the bile, stored in the gallbladder, and delivered into the duodenum with ingestion of meals to emulsify fats and fat soluble vitamins and to aid in their absorption (1). BAs have detergent properties and they retain their cholesterol “backbone”; their conjugated state with taurine and glycine is preserved in the small intestine.
In the ileum, BAs that are not involved in micelles are efficiently (~95%) absorbed via an energy-requiring process involving the apical sodium bile acid transporter (ASBT). Within the ileal enterocytes (Figure 1), BAs stimulate the nuclear farsenoid X receptor (FXR) to produce fibroblast growth factor 19 (FGF-19), an enteroendocrine hormone that is transported to the liver and enters the hepatocyte through FGF-receptor 4 (FGF-R4) with interaction with a surface protein (klotho β), leading to the induction of a small heterodimer protein (SHP) to decrease hepatic BA synthesis by inhibiting the rate limiting enzyme, 7α-hydroxy-4-cholesten-3-one (C4) (Figure 2) (1).
Figure 1. A graphical representation of the enterohepatic circulation.
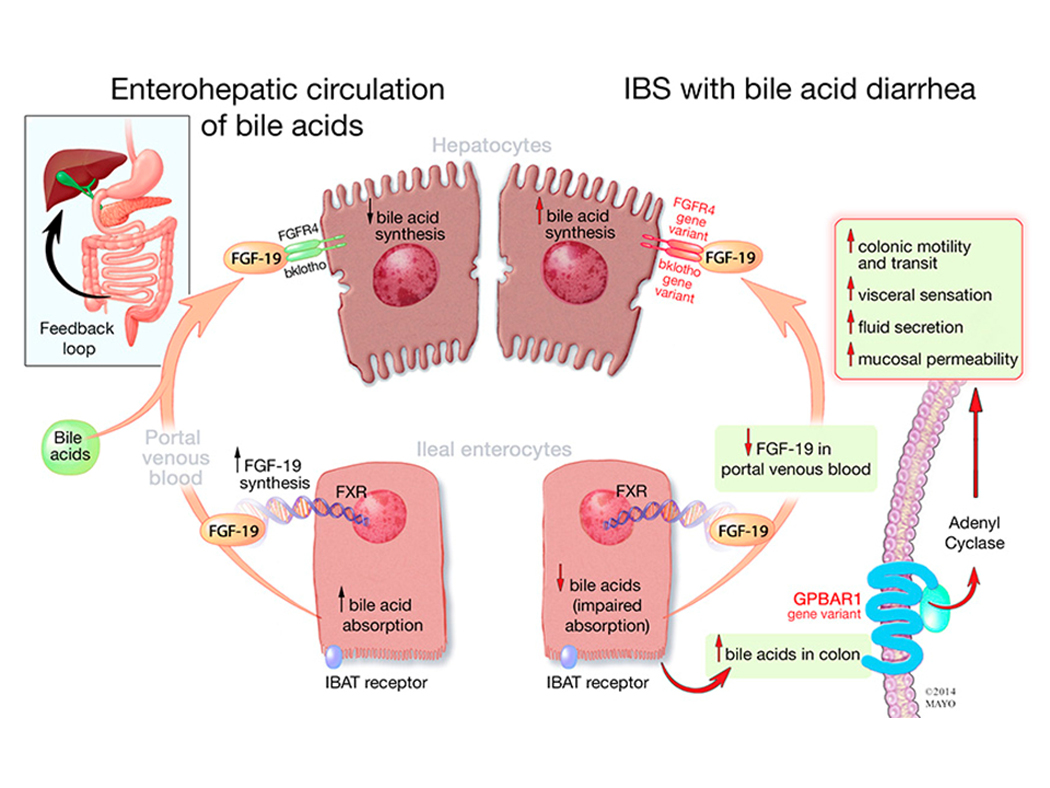
Left panel indicates bile acid circulation in healthy individuals. Bile acids are reabsorbed in the ileum, activate FXR and increase FGF-19 synthesis. FGF-19 then binds to the FGFR-4 and klotho β receptors to decrease C4 and subsequent hepatic bile acid synthesis. Right panel: In bile acid malabsorption, bile acids are reabsorbed, but FGF-19 remains low, or there are mutations within the FGFR-4 or klotho β receptors that do not inhibit hepatic bile acid synthesis. Bile acids that enter the colon bind to the GPBAR1 receptor and cause increased colonic transit and secretion. IBS=irritable bowel syndrome.
Reproduced with permission from ref. 34, Camilleri M. Physiological underpinnings of irritable bowel syndrome: neurohormonal mechanisms. J Physiol 2014;592:2967–80.
Figure 2. Synthesis, secretion and enterohepatic circulation of bile acids in humans.
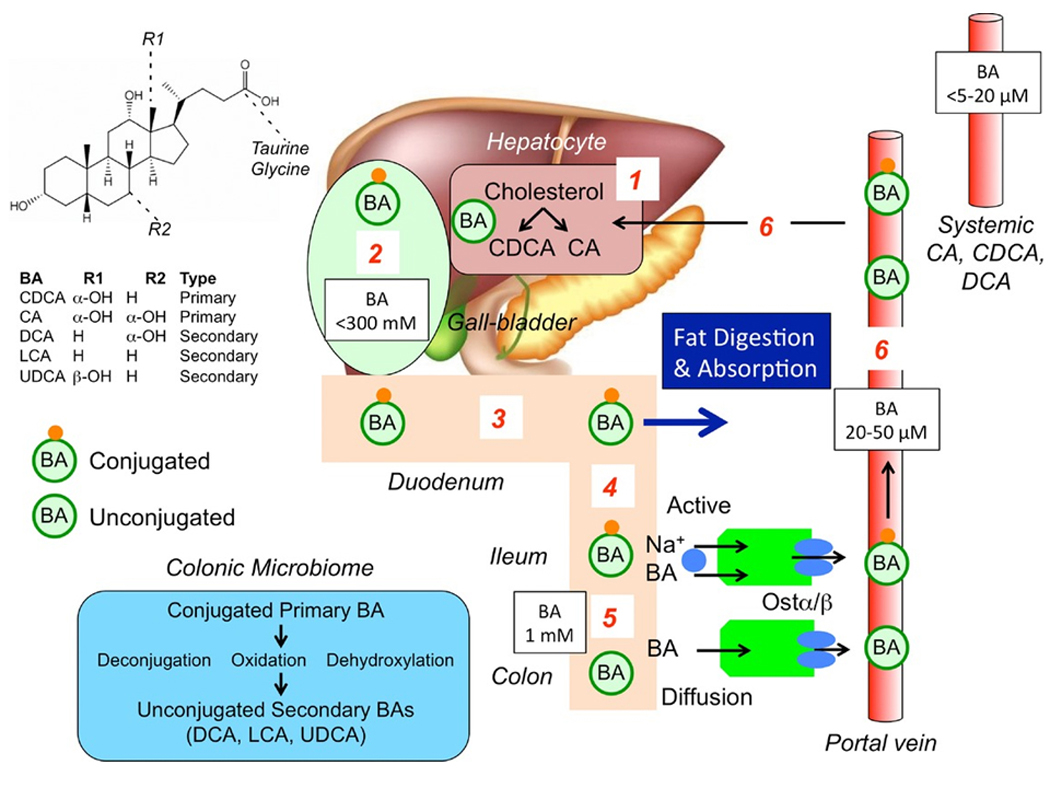
(1) Primary bile acids (BAs) are synthesized in hepatocytes from cholesterol. (2) BAs are conjugated to glycine and taurine and are stored in the gallbladder at high concentrations. (3) After feeding, conjugated BAs are secreted in the intestine where they emulsify dietary fats and form mixed micelles that facilitate digestion and absorption of the products of triglyceride digestion. (4) Conjugated BAs are actively absorbed by the apical sodium BA co-transporter [ASBT (IBAT)] at the apical membrane of enterocytes of the terminal ileum. (5) In the colon, bacteria deconjugate and dehydroxylate primary BAs to form secondary BAs, which are passively absorbed. (6) Conjugated and unconjugated BAs enter the portal vein and recirculate to the liver for re-use.
BA=bile acid; CA=cholic acid; CDCA=chenodeoxycholic acid; DCA=deoxycholic acid; LCA=lithocholic acid; UDCA=ursodeoxycholic acid; Na=sodium Reproduced with permission from ref. 1, Bunnett NW. Neuro-humoral signalling by bile acids and the TGR5 receptor in the gastrointestinal tract. J Physiol 2014;592:2943–50.
About 5% of the BAs (CA and CDCA) that are unabsorbed in the ileum are deconjugated on reaching the colon by bacterial bile salt hydrolases and by 7α-dehydroxylated by bacteria to form secondary bile acids (Figure 2), predominantly deoxycholic acid (DCA), lithocholic acid (LCA), and ursodeoxycholic acid (UDCA). Thus, colonic microbiota are integral to the effects of bile acids. In the colon, CDCA and DCA stimulate fluid secretion (2), increase mucosal permeability, and induce high amplitude propagated contractions (3,4). The colon reabsorbs, by diffusion, at least 50% of the mass of bile acids reaching the human colon (5).
The farnesoid X receptor (FXR) is highly expressed in the intestine and liver and is a natural receptor for bile acids. CDCA is the most potent FXR agonist, followed by CA (81%), DCA (40%), and LCA (4%) relative to CDCA’s potency (6).
The second natural BA receptor is G-protein coupled bile acid target receptor (GPBAR1), also called Takeda G-coupled receptor 5 (TGR5); it is located on cholangiocytes, intestinal cells, the basolateral surface of smooth muscle, neural cells, brown adipose tissue, immune cells including dendritic cells and macrophages, and enteroendocrine cells that produce glucagon-like peptide 1 (GLP-1) (7). TGR5 is most potently activated by LCA, among the natural bile acids, and it mediates effects of bile acids on motility, directly by action on neurons and indirectly by stimulating serotonin release (1).
Symptoms and Signs of Bile Acid Malabsorption
Diarrhea is the hallmark of bile acid malabsorption (BAM). In an online survey of 100 patients with BAM out of 1300 members of a BAM support group, 85% reported urgency, 54% abdominal pain, 88% occasional incontinence, and 52% felt the need to be close to the bathroom. Among those with abdominal discomfort, 40% reported fatigue and at least 60% ‘brain fog’ which prevented work efficiency. After treatment with bile acid sequestrants, gastrointestinal and systemic symptoms improved or resolved by at least 50%, and there was a significant improvement in work absences and altered work hours (8). Patients with unexplained diarrhea or irritable bowel syndrome-diarrhea (IBS-D) who have increased fecal bile acid excretion typically have higher BMI, increased stool weight and fat, and accelerated colonic transit compared to patients without increased fecal bile acid excretion (9).
Disease States Resulting in Bile Acid Malabsorption
BAM is characterized by diarrhea, abdominal discomfort and bloating (10,11). Four types of BAM (12) are recognized: type 1 BAM includes ileal disease, such as Crohn’s disease, resection, and radiation ileitis; type 2 BAM is “idiopathic”, and manifests clinically as functional diarrhea or IBS-D; type 3 BAM is malabsorption of BAs secondary to diseases, such as chronic pancreatitis, cholecystectomy and celiac disease; type 4 BAM results from increased BA synthesis induced by treatment with metformin, which inhibits ileal reabsorption of bile acids, thereby increasing fecal excretion of bile acids (13).
Prevalence of Bile Acid Malabsorption in Diverse Conditions
BAM is estimated to affect ~1% of the population in Western countries (14). The prevalence of BAM in different conditions is generally replicated in numerous studies. For example, type 1 BAM was present in 77/87 patients with Crohn’s disease who underwent 75SeHCAT (75Se-homocholic acid taurine) retention (15), in more than 90% of patients with Crohn’s disease with ileal resection >100cm, and in 11–52% of those without ileal resection (16). This test measures the retention of radiolabeled bile acids 7 days after oral ingestion. The lower the retention of radiolabeled BAs, measured by whole body scanning with a gamma camera, indicates that BAs are lost in the feces, and the lowest levels of retention reflect more severe BAM.
The prevalence of type 2 “idiopathic” BAM was assessed in two systematic reviews. One involved 15 prospective studies, mostly based on 75SeHCAT retention in patients with functional diarrhea or IBS-D. In this analysis, severe BAM (<5% retention) was present in 10%, moderate BAM (<10% retention) in 32%, and mild BAM (<15% retention) in 26% of patients (17). A second systematic review included other diagnostic methods (discussed below) and concluded that the prevalence was 30% in patients with functional diarrhea or IBS-D (18). The prevalence of types 3 and 4 BAM is unclear because screening for BAM in these patients is limited.
However, the prevalence of BAM in patients post-cholecystectomy is lower than generally considered. In a systematic review of 25 studies that included 3388 patients, only 9.1% of patients developed diarrhea after cholecystectomy, with two-thirds having been diagnosed with BAM (19). Similarly, in 125 consecutive patients who underwent laparoscopic cholecystectomy, 25.2% developed diarrhea at one week after surgery, and 5.7% had diarrhea at 3 months (20).
In microscopic colitis, there is considerable evidence of BAM in a subset of patients. In one study, 43% of patients with microscopic colitis had BAM [lymphocytic (60%); collagenous (27%) colitis], and 86% of patients with BAM responded to cholestyramine (21). Findings in other studies of BAM in microscopic colitis have been conflicting (22–24), and it has also been noted that diarrhea patients without BAM may respond to a bile acid sequestrant (25). The latter observation suggests that a therapeutic response to bile acid sequestrant does not prove BAM in such patients. The cause of BAM in microscopic colitis may be related to the villous atrophy, inflammation, and collagen deposition in the ileum that have been reported in patients with microscopic colitis (26,27).
Bile acids also may play a role in non-alcoholic fatty liver disease, with evidence of higher bile acid synthesis being associated with higher fibrosis scores (28).
Potential Mechanisms Underpinning Idiopathic Bile Acid Malabsorption
At present, the strongest data suggest that primary BAM results from reduced production of FGF-19 by ileal enterocytes, leading to low fasting serum FGF-19 and reciprocally increased serum 7α-C4, denoting increased hepatic synthesis of BAs (29). The low FGF-19 may result from reduced FGF-19 and ASBT mRNA expression in ileal biopsies from patients with BAM (30). The expression data were supported by functional effects. Thus, the in vivo retention of 75SeHCAT was significantly correlated with the basal ileal transcript expression of FGF-19 and ASBT. In addition, in vitro studies showed that CDCA stimulated transcripts of FGF-19 and ileal BA binding protein. Less than 1% of patients with type 2 BAD had impairment of BA reabsorption due to a mutation in the gene for the ileal BA transporter (31).
Other data support an association of BAM with proteins involved in the enterohepatic circulation, based on associations of genetic variants in GPBAR1 rs11554825, klotho β rs17618244, and FGFR4 (fibroblast growth factor receptor 4) rs351855, with acceleration of colonic transit (as a surrogate of BAM) in patients with IBS-D or functional diarrhea (Figure 1) (32–34). In mice, mutations within the Diet1 gene, exclusively expressed in the epithelial cells lining the small intestinal villi and kidney proximal tubules, have resulted in decreased FGF-15, the mice counterpart for the human FGF-19 (35). The relevance to humans with idiopathic BAM is unclear.
Mechanisms Leading to Gastrointestinal Symptoms in Bile Acid Malabsorption
BAs cause diarrhea by increasing colonic motility and secretion, and they affect inflammation and the microbiome. Water and electrolyte secretion in response to bile acids is based on several mechanisms (Table 1).
Table 1.
Mechanisms of colonic water and electrolyte movement in bile acid malabsorption
| Mechanism (ref. #) | Mediators/co-factors | Effects |
|---|---|---|
| Stimulation of intracellular mediators (32–34) | ↑cAMP, epidermal growth factor receptor, and mediators including exchange protein directly activated by cAMP and calcium++ ions | CFTR - induce chloride secretion |
| ↑ intestinal permeability (36–41) | detergent or structure activity properties of the bile acids, TGR5 activation, ↓occludins | ↑ secretion, ↑ motility, ↓ transepithelial barrier |
| Aquaporin channels (42,44,45) | ↑ aquaporin channels 3 and 8 in rats | ↑ water secretion |
| Enteroendocrine mechanisms (46,47) | ↑ serotonin | ↑ fluid and mucus secretion |
| Neurocrine mediation (47–49) | activate basal TGR5 and submucosal cholinergic neurons | ↑ colonic motility and secretion |
| Decreased sodium and water absorption (50) | ↓ sodium potassium ATPase β1 unit in colon and α1 unit in proximal colon | ↓ sodium and water reabsorption |
cAMP=calcium and cyclic adenosine monophosphate; CFTR=cystic fibrosis transmembrane conductance regulator
Stimulation of motility results from a series of processes. First, BAs are passively absorbed by diffusion to activate TGR5 receptors on enteric neurons to release serotonin, thereby inducing colonic contractions (1), chloride secretion (36), and stimulation of defecation in mice (37). The greatest potency for stimulation of TGR5 is with LCA, followed by DCA, CDCA, and CA (38). Stimulatory effects of BAs on colonic motility are induction of high amplitude propagating contractions (HAPCs) in the colon [e.g., with rectal infusion of 1 mM CDCA (4)] and acceleration of colonic transit with Na CDC (39). When CDC undergoes colonic dehydroxylation to LCA, the latter stimulates colonic motility through TGR5 receptors.
An additional effect on BA-induced colonic dysfunction may result from changes in the microbiome. Patients with BAM have a higher proportion of fecal primary BAs, particularly CDCA, a secretory BA (10,40), suggesting either insufficient time for dehydroxylation due to rapid colonic transit, or due to changes in the microbiome resulting in alteration of BA-transforming bacteria in feces. Indeed, whereas patients with IBS-D have a higher proportion of Escherichia coli and decreased Clostridium leptum and Bifidobacterium (40), a recent report showed that 24.5% of patients with IBS-D exhibited excessive excretion of total BAs and increase in Clostridia bacteria (e.g., C. scindens), which was positively associated with the levels of fecal BAs and serum 7α-hydroxy-4-cholesten-3-one (C4) (41). The latter finding suggested that Clostridia bacteria have potential as a biomarker for BAD and as a target for therapy (42), although this still requires formal testing in humans.
Diagnosis of Bile Acid Malabsorption
Current BAM diagnostic methods are based on documentation of impaired ileal BA absorption, decreased hepatic feedback inhibition, and increased hepatic BA synthesis. Table 2 summarizes the characteristics of the different diagnostic tests (43).
Table 2. Current and future bile acid diarrhea diagnostic tests.
(BA=bile acids; primary BAs are cholic acid and chenodeoxycholic acid; HPLC=high performance liquid chromatography) Modified with permission from ref. 43, Vijayvargiya P, Camilleri M. Commentary: Current practice in the diagnosis of bile acid diarrhea. Gastroenterology 2019;156:1233–8.
| Diagnostic Test | 75SeHCAT | Fasting serum C4 | Fasting serum FGF-19 | Total fecal BAs | Primary BAs >4% + total fecal BAs | Fecal primary BAs >10% | Single or combined tests of fecal primary BAs + fasting serum C4 |
|---|---|---|---|---|---|---|---|
| What does it measure? | Ileal capacity to reabsorb radiolabeled bile acid retention (%) on day 7 | Hepatic bile acid synthesis | Amount of feedback inhibition to hepatic bile acid synthesis | Total fecal bile acid excreted from the colon | Amount of bile acids with secretory potential with total fecal BA excretion | Amount of bile acids that are directly synthesized from the liver with secretory potential | Combining serum and stool biomarkers to simplify diagnosis of bile acid diarrhea |
| Diagnostic cutoffs | <5% (severe) <10% (moderate) <15% (mild) |
≥52.5 ng/mL | ≤61.7 pg/mL | ≥2,337 μmol/48h | Primary BAs >4% + total fecal BAs >1,000 μmol/48h | >10% primary BAs | To be determined |
| Sensitivity relative to fecal wt >400g/48h | 15% | 28% | 59% | 46% | 49% | ||
| Specificity relative to fecal wt >400g/48h | 86% | 75% | 92% | 97% | 91% | ||
| Diet, radiation and equipment required for measurement | Gamma camera with radiation exposure; 7-day test | HPLC Measure before 9am | ELISA Measure before 9am | HPLCRequires 100-gram high fat diet x 4 days and 2-day stool collection | HPLC + HPLCsingle, random stool sample + C4 measured before 9am | ||
| Comment or pitfalls of testing | Possibly best for type 1 bile acid diarrhea, as it primarily tests ileal bile acid absorption | Diagnostic accuracy high as shown by high specificity, but sensitivity is low | ? diagnostic accuracy | Direct way to analyze fecal BAs within colon | Identify additional patients | Identify additional patients | In development |
75Selenium HomotauroCholic Acid Test
75SeHCAT measures the retention of radiolabeled BAs 7 days after ingestion. This is the gold standard diagnostic method. Low retention of radiolabeled BAs indicates loss of BAs in feces; current cut-offs for mild, moderate, and severe BAM are <15%, <10%, and <5% retention, respectively, at 7 days. 75SeHCAT is simple and noninvasive, but it requires a gamma camera, exposes patients to radiation, and is not available in many countries including the USA. A potential confounder in the measured retention of bile acids in the whole body is the number of times the bile acid pool undergoes enterohepatic recycling, which can vary from 4–16 per day (44). For example, a small deficit in ileal bile acid absorption may result in high loss of isotope if the individual has 16 cycles per day, whereas, a more substantial deficit in ileal bile acid absorption may result in greater overall retention if there are fewer cycles of the bile acid pool per day. This confounder should be resolved by estimating retention over a longer period of time, such as the recommended 7 days for the test.
48 Hour Fecal Bile Acid Test
In places without access to 75SeHCAT, a 48 hour fecal BA test is the best current option. Patients consume a high fat diet (100 g/day) for 4 days and collect stool for the last 48 hours. Total and primary fecal BA levels have demonstrated a significant positive association with 75SeHCAT retention (45,46). Total and primary fecal bile acids and fecal fat were significant predictors of increased stool weight, frequency, and consistency, with AUC >0.71 (sensitivity >55%, specificity >74%) (47). In addition, primary fecal bile acid excretion was associated with fecal weight (>400 g/48h) and colonic transit average location of isotope at 24h >3.34, corresponding to sigmoid colon (48).
Although the stool collection is cumbersome, a 48 hour fecal BA test allows direct measurements of total and individual BAs without radiation exposure, with three criteria diagnostic of BAM: total fecal BAs ≥2,337 μmol/48h (5), primary BAs (CDCA and CA) >10%, or total fecal BAs ≥1,000 μmol/48h plus primary BAs >4% compared to healthy controls (<5%) [Figure 3] (48,49).
Figure 3. Primary bile acids alone or in combination with total fecal bile acids are equivalent to fecal bile acids in the ability to detect elevated fecal weight, a validated correlate of bile acid diarrhea. Receiver operating characteristic (ROC) curves of total fecal bile acids (larger central image), primary bile acids (bottom left ROC curve), and primary bile acids with total fecal bile acids (lower right ROC curve) predict fecal weight >400 grams.
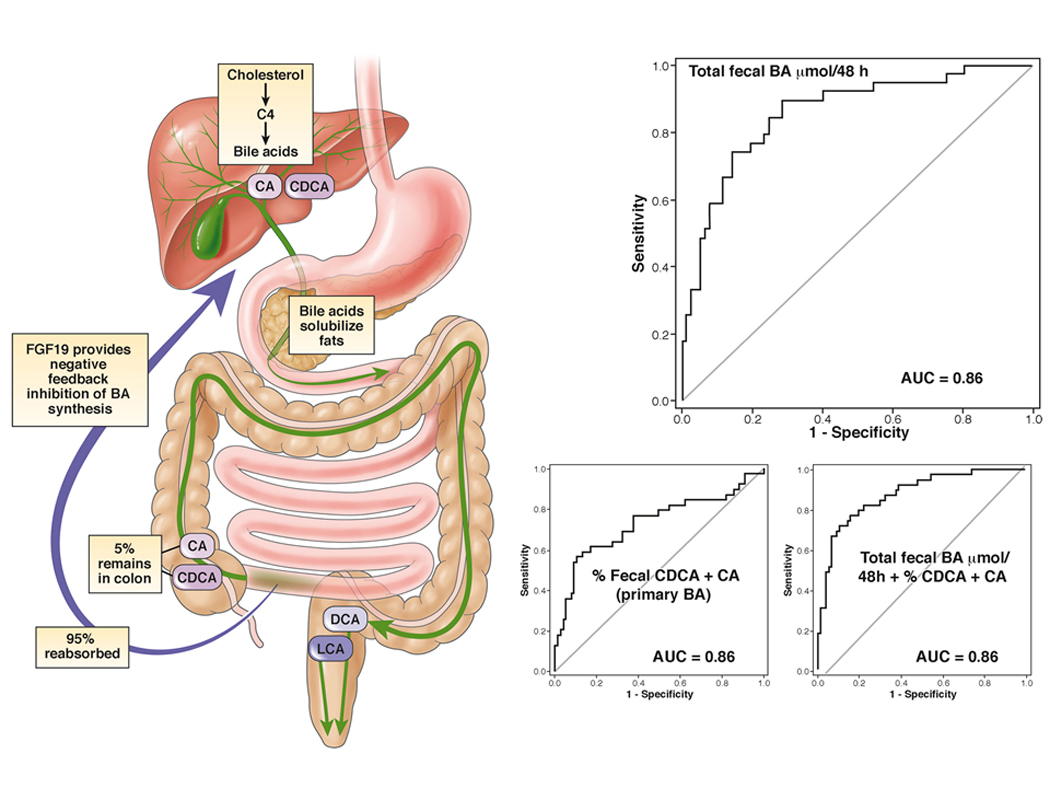
AUC=area under the curve; BA=bile acids; 7α-hydroxy-4-cholesten-3-one=7αC4; CA=cholic acid; CDCA=chenodeoxycholic acid; DCA=deoxycholic acid; LCA=lithocholic acid Reproduced from ref. 43, Vijayvargiya P, Camilleri M. Commentary: Current practice in the diagnosis of bile acid diarrhea. Gastroenterology 2019;156:1233–8.
Fasting Serum 7α-hydroxy-4-cholesten-3-one (C4)
Fasting serum C4 (before 9:00 a.m. because of diurnal variation) is measured by C18 liquid chromatography, tandem mass spectrometry (50). Serum C4 is a direct measure of BA synthesis; higher values indicate BAM. C4 has been validated in comparison with 75SeHCAT [C4 cut-off value >48.4 ng/mL: sensitivity of 90% and specificity of 79% (51)] and in comparison with fecal 48 hour BA test [C4 cut-off >52.5 ng/mL: sensitivity of 29% and specificity of 83% (52)].
Fasting serum C4 is an efficient and convenient method to rule out BAM (52), and it is available via commercial testing in the United States (Mayo Medical Laboratories and PROMETHEUS® IBcause™).
In patients with Crohn’s disease, high C4 was associated with ileal disease or resection and non-bloody diarrhea. In contrast, C4 levels in ulcerative colitis were similar to healthy controls (53). Thus, fasting serum C4 >48.3 ng/mL identifies Crohn’s patients with diarrhea likely attributable to BAM (90.9% sensitivity, 84.4% specificity) (54).
Serum Fasting Fibroblast Growth Factor 19 (FGF-19)
Serum FGF-19 is inversely correlated with serum C4 (55), and the 5th percentile in healthy volunteers is ≤61.7 pg/mL. However, fasting FGF-19 is not sensitive (29%) or specific enough (78%) relative to fecal BA excretion (52) to screen for BAD. Therefore, fasting serum FGF-19 would appear to be most helpful to rule out BAM, if and when it becomes available for use in clinical practice. Further research is required to assess a modification on the test, which is CDCA-stimulated FGF-19 (acting as a “stress test”) in the diagnosis of BAD (56). Recent guideline did not recommend the test as a first line diagnostic test for BAD (57).
Diagnostic Test versus Empiric Trial of BA Sequestrants
When diagnostic tests are not available, empiric treatment with bile acid sequestrants is advocated for patients with suspected BAM. However, compliance with a therapeutic trial may be suboptimal (58), compromising interpretation of a negative response. Since severity of BAM can predict response to treatment, there is strong rationale to measure BAM rather than just empiric treatment (17,59). British and Canadian gastroenterology organization guidelines also support diagnosis over empiric trial for suspected BAM in patients presenting with chronic diarrhea (57,60). In addition, a positive test for BAM was associated with reduced healthcare utilization in a referral center in the UK (61), and a retrospective study of almost 1,000 patients evaluated for chronic unexplained diarrhea in a US tertiary center showed high healthcare utilization in referred patients that could have been avoided by earlier implementation of a diagnostic test for BAM (62).
Treatment of BAM
Dietary Modifications
A low fat diet with <20% of total daily caloric intake complements efficacy of bile acid sequestrant treatment in the relief of abdominal discomfort, distension, urgency, and stool consistency and frequency (63).
Bile Acid Sequestrants
Three bile acid sequestrants are available in either powder or tablet formulations: cholestyramine, colestipol, and colesevelam. Patients should take these medications with meals in order to bind free BAs and prevent the colonic effects of increased colonic motility and secretion.
The only randomized trial of cholestyramine efficacy in BAD showed response rates of 40% and 53.8% in patients with 75SeHCAT (selenium homocholic acid taurine) retention <10% or 20%, respectively. Less than 15% retention is usually the cut-off for abnormal bile acid loss (10–15% retention mild, 5–10% moderate, and <5% severe bile acid loss).
In an open-label trial in patients with BAD with 75SeHCAT retention <20%, colestipol reduced stool frequency and IBS severity score (64).
In another open-label study in patients with high 48 hour stool bile acid excretion, colesevelam, 1875 mg twice daily for 10 days, decreased stool consistency and increased stool excretion of sequestered bile acids (65). Because of the loss of BAs in the stool with bile acid sequestrant treatment, hepatic BA synthesis and, thus, serum C4 were increased (65). Colesevelam also slowed emptying of the ascending colon compared with placebo in IBS-D; the treatment effect was associated with baseline serum C4, which reflects the hepatic bile acid synthesis rate (66).
Further controlled trials are necessary to assess the effects of bile acid sequestrants for diarrhea, and patients will likely need long-term therapy with bile acid sequestrants for symptom relief. In a long-term, follow-up study of patients with a median time from diagnosis of BAD of 6.8 years, 38% were still on bile acid sequestrants, with adequate relief of their symptoms, while 24% discontinued therapy, most commonly due to poor tolerability (67).
Two double-blinded, placebo-controlled, randomized trials with the bile acid sequestrant, colesevelam, in patients with BAM, based on elevated serum C4 in Crohn’s disease, showed a higher number of patients with >30% reduction of liquid stool and reduction of median number of liquid stools from 5 to 2 per week, compared to placebo (68). In a comparison of cholestyramine and hydroxypropyl cellulose in patients with chronic water diarrhea (some with 75SeHCAT <15%), there was higher decrease in watery stools in the cholestyramine group, although there was no difference in the primary endpoint of proportion with mean ≤3 liquid bowel movements per week (69). However, the equipoise between these treatments may be confounded by the fact that hydroxypropyl cellulose actually binds BAs without affecting hepatic bile acid synthesis, and it was shown in a separate study to improve stool frequency, consistency, urgency, and incontinence after 6 weeks’ treatment in patients with idiopathic BAM and Crohn’s disease with ileal resection (70).
Although bile acid sequestrants are effective in improving abdominal symptoms and stool characteristics, this treatment option does not target the underlying pathophysiology. This is addressed more directly by FXR agonists.
FXR Agonists
FXR agonists were initially developed for cholestatic liver diseases. However, efficacy of FXR agonists in BAM has been shown in in vitro and in two in vivo studies. FXR agonists attenuated calcium and cyclic adenosine monophosphate (cAMP) dependent chloride secretion on colonic epithelium (71). In two clinical trials in patients with BAM, a 2-week trial of obeticholic acid (6-ethyl CDCA) daily in patients with primary and secondary BAM and chronic diarrhea showed improvement in stool frequency, form, and total diarrhea index, with corresponding increase in FGF-19 and decrease in C4 and fecal BAs. However, obeticholic acid (which is chemically 6-ethyl CDCA) is associated with pruritus (72). A preliminary report showed the non-bile acid molecule, tropifexor, retarded ascending colon emptying in patients with BAD, although the clinical endpoints were not significantly altered in that small clinical trial (73).
CONCLUSIONS
The bile acid field has expanded in relevance, particularly in clinical diagnosis of unexplained diarrhea in patients with IBS-D, microscopic colitis, and inflammatory bowel disease without ileal inflammation or resection. This has been facilitated by the validation of screening serum tests and fecal bile acid excretion. Novel therapeutic approaches targeting FXR receptors might open new avenues for treatment of intestinal diseases.
Acknowledgments
Financial support: Michael Camilleri is supported by grant RO1-DK115950 from National Institutes of Health.
Footnotes
Competing interests: Michael Camilleri has conducted sponsored research on elobixibat and tropifexor. Priya Vijayvargiya has no conflicts of interest.
Guarantor of the article: Michael Camilleri accepts full responsibility for the conduct of the study. He had access to the data and control of the decision to publish.
Contributor Information
Michael Camilleri, Clinical Enteric Neuroscience Translational and Epidemiological Research (C.E.N.T.E.R.), Division of Gastroenterology and Hepatology, Department of Medicine, Mayo Clinic, Rochester, MN
Priya Vijayvargiya, Clinical Enteric Neuroscience Translational and Epidemiological Research (C.E.N.T.E.R.), Division of Gastroenterology and Hepatology, Department of Medicine, Mayo Clinic, Rochester, MN
REFERENCES
- 1.Bunnett NW. Neuro-humoral signalling by bile acids and the TGR5 receptor in the gastrointestinal tract. J Physiol 2014;592:2943–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wingate DL, Krag E, Mekhjian HS, et al. Relationships between ion and water movement in the human jejunum, ileum and colon during perfusion with bile acids. Clin Sci Mol Med 1973;45:593–606. [DOI] [PubMed] [Google Scholar]
- 3.Kirwan WO, Smith AN, Mitchell WD, et al. Bile acids and colonic motility in the rabbit and the human. Gut 1975;16:894–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bampton PA, Dinning PG, Kennedy ML, et al. The proximal colonic motor response to rectal mechanical and chemical stimulation. Am J Physiol Gastrointest Liver Physiol 2002;282:G443–9. [DOI] [PubMed] [Google Scholar]
- 5.Mekhjian HS, Phillips SF, Hofmann AF. Colonic absorption of unconjugated bile acids: perfusion studies in man. Dig Dis Sci 1979;24:545–50. [DOI] [PubMed] [Google Scholar]
- 6.Zhang JH, Nolan JD, Kennie SL, et al. Potent stimulation of fibroblast growth factor 19 expression in the human ileum by bile acids. Am J Physiol 2013;304:G940–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brighton CA, Rievaj J, Kuhre RE, et al. Bile acids trigger GLP-1 release predominantly by accessing basolaterally located G protein–coupled bile acid receptors. Endocrinology 2015;156:3961–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bannaga A, Kelman L, O’Connor M, et al. How bad is bile acid diarrhoea: an online survey of patient-reported symptoms and outcomes. BMJ Open Gastroenterol 2017;4(1):e000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camilleri M, Busciglio I, Acosta A, et al. Effect of increased bile acid synthesis or fecal excretion in irritable bowel syndrome-diarrhea. Am J Gastroenterol 2014;109:1621–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin A, Camilleri M, Vijayvargiya P, et al. Bowel functions, fecal unconjugated primary and secondary bile acids, and colonic transit in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2013;11:1270–5, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong BS, Camilleri M, Carlson P, et al. Increased bile acid biosynthesis is associated with irritable bowel syndrome with diarrhea. Clin Gastroenterol Hepatol 2012;10:1009–15, e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fromm H, Malavolti M. Bile acid-induced diarrhoea. Clinics in Gastroenterology 1986;15:567–82. [PubMed] [Google Scholar]
- 13.Scarpello JH, Hodgson E, Howlett HC. Effect of metformin on bile salt circulation and intestinal motility in type 2 diabetes mellitus. Diabetic Med 1998;15:651–6. [DOI] [PubMed] [Google Scholar]
- 14.Walters JR, Pattni SS. Managing bile acid diarrhoea. Ther Adv Gastroenterol 2010;3:349–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borghede MK, Schlütter JM, Agnholt JS, et al. Bile acid malabsorption investigated by selenium-75-homocholic acid taurine (75SeHCAT) scans: Causes and treatment responses to cholestyramine in 298 patients with chronic watery diarrhoea. Eur J Intern Med 2011;22:e137–40. [DOI] [PubMed] [Google Scholar]
- 16.Barkun AN, Love J, Gould M, et al. Bile acid malabsorption in chronic diarrhea: pathophysiology and treatment. Can J Gastroenterol 2013;27:653–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wedlake L, A’Hern R, Russell D, et al. Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2009;30:707–17. [DOI] [PubMed] [Google Scholar]
- 18.Valentin N, Camilleri M, Altayar O, et al. Biomarkers for bile acid diarrhoea in functional bowel disorder with diarrhoea: a systematic review and meta-analysis. Gut 2016;65:1951–9. [DOI] [PubMed] [Google Scholar]
- 19.Farahmandfar MR, Chabok M, Alade M, et al. Post-cholecystectomy diarrhoea: a systematic review. Surg Sci 2012;3:7. [Google Scholar]
- 20.Yueh T-P, Chen F-Y, Lin T-E, et al. Diarrhea after laparoscopic cholecystectomy: Associated factors and predictors. Asian J Surg 2014;37:171–7. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez-Banares F, Esteve M, Salas A, et al. Bile acid malabsorption in microscopic colitis and in previously unexplained functional chronic diarrhea. Dig Dis Sci 2001;46:2231–8. [DOI] [PubMed] [Google Scholar]
- 22.Giardiello FM, Bayless TM, Jessurun J, et al. Collagenous colitis: Physiologic and histopathologic studies in seven patients. Ann Intern Med 1987;106:46–9. [DOI] [PubMed] [Google Scholar]
- 23.Kingham JG, Levison DA, Ball JA, et al. Microscopic colitis-a cause of chronic watery diarrhoea. BMJ 1982;285:1601–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eusufzai S, Löfberg R, Veress B, et al. Studies on bile acid metabolism in colagenous colitis: no evidence of bile acid malabsorption as determined by the SeHCAT test. Eur J Gastroenterol Hepatol 1992;4:317–21. [Google Scholar]
- 25.Ung K, Gillberg R, Kilander A, et al. Role of bile acids and bile acid binding agents in patients with collagenous colitis. Gut 2000;46:170–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Einarsson K, Eusufzai S, Johansson U, et al. Villous atrophy of distal ileum and lymphocytic colitis in a woman with bile acid malabsorption. Eur J Gastroenterol Hepatol 1992;4:585–90. [Google Scholar]
- 27.Marteau P, Lavergne-Slove A, Lemann M, et al. Primary ileal villous atrophy is often associated with microscopic colitis. Gut 1997;41:561–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Appleby RN, Moghul I, Khan S, et al. Non-alcoholic fatty liver disease is associated with dysregulated bile acid synthesis and diarrhea: A prospective observational study. PLoS One 2019;14: e0211348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walters JR, Tasleem AM, Omer OS, et al. A new mechanism for bile acid diarrhea: defective feedback inhibition of bile acid biosynthesis. Clin Gastroenterol Hepatol 2009;7:1189–94. [DOI] [PubMed] [Google Scholar]
- 30.Johnston IM, Nolan JD, Pattni SS, et al. Characterizing factors associated with differences in FGF19 blood levels and synthesis in patients with primary bile acid diarrhea. Am J Gastroenterol 2016;111:423–32. [DOI] [PubMed] [Google Scholar]
- 31.Montagnani M, Love MW, Rossel P, et al. Absence of dysfunctional ileal sodium-bile acid cotransporter gene mutations in patients with adult-onset idiopathic bile acid malabsorption. Scand J Gastroenterol 2001;36:1077–80. [DOI] [PubMed] [Google Scholar]
- 32.Camilleri M, Shin A, Busciglio I, et al. Genetic variation in GPBAR1 predisposes to quantitative changes in colonic transit and bile acid excretion. Am J Physiol 2014;307:G508–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Camilleri M, Klee EW, Shin A, et al. Irritable bowel syndrome-diarrhea: characterization of genotype by exome sequencing, and phenotypes of bile acid synthesis and colonic transit. Am J Physiol 2014;306:G13–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Camilleri M Physiological underpinnings of irritable bowel syndrome: neurohormonal mechanisms. J Physiol 2014;592:2967–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee JM, Ong JR, Vergnes L, et al. Diet, bile acid diarrhea, and FGF15/19: mouse model and human genetic variants. J Lipid Res 2018;59:429–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zimmerman TW, Binder HJ. Serotonin-induced alteration of colonic electrolyte transport in the rat. Gastroenterology 1984;86:310–7. [PubMed] [Google Scholar]
- 37.Alemi F, Poole DP, Chiu J, et al. The receptor TGR5 mediates the prokinetic actions of intestinal bile acids and is required for normal defecation in mice. Gastroenterology 2013;144:145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kawamata Y, Fujii R, Hosoya M, et al. A G protein-coupled receptor responsive to bile acids. J Biolog Chem 2003;278:9435–40. [DOI] [PubMed] [Google Scholar]
- 39.Rao AS, Wong BS, Camilleri M, et al. Chenodeoxycholate in females with irritable bowel syndrome-constipation: a pharmacodynamic and pharmacogenetic analysis. Gastroenterology 2010;139:1549–58, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dior M, Delagrèverie H, Duboc H, et al. Interplay between bile acid metabolism and microbiota in irritable bowel syndrome. Neurogastroenterol Motil 2016;28:1330–40. [DOI] [PubMed] [Google Scholar]
- 41.Zhao L, Yang W, Chen Y, et al. A Clostridia-rich microbiota enhances bile acid excretion in diarrhea-predominant irritable bowel syndrome. J Clin Invest 2020;130:438–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Walters JR, Marchesi JR. Chronic diarrhea, bile acids, and Clostridia. J Clin Invest 2020;130:77–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vijayvargiya P, Camilleri M. Commentary: Current practice in the diagnosis of bile acid diarrhea. Gastroenterology 2019;156:1233–8. [DOI] [PubMed] [Google Scholar]
- 44.Brunner H, Northfield T, Hofmann A, et al. Gastric emptying and secretion of bile acids, cholesterol, and pancreatic enzymes during digestion: duodenal perfusion studies in healthy subjects. Mayo Clin Proc 1974;49:851–60. [PubMed] [Google Scholar]
- 45.Scheurlen C, Kruis W, Bull U, et al. Comparison of 75SeHCAT retention half-life and fecal content of individual bile acids in patients with chronic diarrheal disorders. Digestion 1986;35:102–8. [DOI] [PubMed] [Google Scholar]
- 46.Sciarretta G, Fagioli G, Furno A, et al. 75Se HCAT test in the detection of bile acid malabsorption in functional diarrhoea and its correlation with small bowel transit. Gut 1987;28:970–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vijayvargiya P, Camilleri M, Burton D, et al. Bile and fat excretion are biomarkers of clinically significant diarrhoea and constipation in irritable bowel syndrome. Aliment Pharmacol Ther 2019;49:744–58. [DOI] [PubMed] [Google Scholar]
- 48.Vijayvargiya P, Camilleri M, Chedid V, et al. Analysis of fecal primary bile acids detects increased stool weight and colonic transit in patients with chronic functional diarrhea. Clin Gastroenterol Hepatol 2019;17:922–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peleman C, Camilleri M, Busciglio I, et al. Colonic transit and bile acid synthesis or excretion in patients with irritable bowel syndrome–diarrhea without bile acid malabsorption. Clin Gastroenterol Hepatol 2017;15:720–7, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Donato LJ, Lueke A, Kenyon SM, et al. Description of analytical method and clinical utility of measuring serum 7-alpha-hydroxy-4-cholesten-3-one (7aC4) by mass spectrometry. Clin Biochem 2018;52:106–11. [DOI] [PubMed] [Google Scholar]
- 51.Sauter GH, Munzing W, Ritter CV, et al. Bile acid malabsorption as a cause of chronic diarrhea diagnostic value of 7α-hydroxy-4-cholesten-3-one in serum. Dig Dis Sci 1999;44:14–9. [DOI] [PubMed] [Google Scholar]
- 52.Vijayvargiya P, Camilleri M, Carlson P, et al. Performance characteristics of serum C4 and FGF19 measurements to exclude the diagnosis of bile acid diarrhoea in IBS‐diarrhoea and functional diarrhoea. Aliment Pharmacol Ther 2017;46:581–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gothe F, Beigel F, Rust C, et al. Bile acid malabsorption assessed by 7 alpha-hydroxy-4-cholesten-3-one in pediatric inflammatory bowel disease: correlation to clinical and laboratory findings. J Crohn’s & Colitis 2014;8:1072–8. [DOI] [PubMed] [Google Scholar]
- 54.Battat R, Duijvestein M, Vande Casteele N, et al. Serum concentrations of 7α-hydroxy-4-cholesten-3-one are associated with bile acid diarrhea in patients with Crohn’s disease. Clin Gastroenterol Hepatol 2019;17:2722–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Duboc H, Tolstanova G, Yuan PQ, et al. Reduction of epithelial secretion in male rat distal colonic mucosa by bile acid receptor TGR5 agonist, INT-777: role of submucosal neurons. Neurogastroenterol Motil 2016;28:1663–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Borup C, Syversen C, Bouchelouche P, et al. Diagnosis of bile acid diarrhoea by fasting and postprandial measurements of fibroblast growth factor 19. Eur J Gastroenterol Hepatol 2015;27:1399–402. [DOI] [PubMed] [Google Scholar]
- 57.Sadowski DC, Camilleri M, Chey WD, et al. Canadian Association of Gastroenterology clinical practice guideline on the management of bile acid diarrhea. Clin Gastroenterol Hepatol 2020;18:24–41. [DOI] [PubMed] [Google Scholar]
- 58.Wilcox C, Turner J, Green J. Systematic review: the management of chronic diarrhoea due to bile acid malabsorption. Aliment Pharmacol Ther 2014;39:923–39. [DOI] [PubMed] [Google Scholar]
- 59.Orekoya O, McLaughlin J, Leitao E, et al. Quantifying bile acid malabsorption helps predict response and tailor sequestrant therapy. Clin Med 2015;15:252–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arasaradnam RP, Brown S, Forbes A, et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition. Gut 2018;67:1380–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Turner JM, Pattni SS, Appleby RN, et al. A positive SeHCAT test results in fewer subsequent investigations in patients with chronic diarrhoea. Frontline Gastroenterol 2017;8:279–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vijayvargiya P, Gonzalez Izundegui D, Calderon G, et al. Fecal bile acid testing in assessing patients with chronic unexplained diarrhea: implications for healthcare utilization. Am J Gastroenterol (submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jackson A, Lalji A, Kabir M, et al. PTU-128: the efficacy of using low-fat dietary interventions to manage bile acid malabsorption. Gut 2017;66(Suppl.2):A114. [Google Scholar]
- 64.Bajor A, Törnblom H, Rudling M, et al. Increased colonic bile acid exposure: a relevant factor for symptoms and treatment in IBS. Gut 2015;64:84–92. [DOI] [PubMed] [Google Scholar]
- 65.Camilleri M, Acosta A, Busciglio I, et al. Effect of colesevelam on faecal bile acids and bowel functions in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2015;41:438–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Odunsi-Shiyanbade ST, Camilleri M, McKinzie S, et al. Effects of chenodeoxycholate and a bile acid sequestrant, colesevelam, on intestinal transit and bowel function. Clin Gastroenterol and Hepatol 2010;8:159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lin S, Sanders DS, Gleeson JT, et al. Long-term outcomes in patients diagnosed with bile-acid diarrhoea. Eur J Gastroenterol Hepatol 2016;28:240–5. [DOI] [PubMed] [Google Scholar]
- 68.Beigel F, Teich N, Howaldt S, et al. Colesevelam for the treatment of bile acid malabsorption-associated diarrhea in patients with Crohn’s disease: A randomized, double-blind, placebo-controlled study. J Crohn’s & Colitis 2014;8:1471–9. [DOI] [PubMed] [Google Scholar]
- 69.Fernandez-Banares F, Rosinach M, Piqueras M, et al. Randomised clinical trial: colestyramine vs. hydroxypropyl cellulose in patients with functional chronic watery diarrhoea. Aliment Pharmacol Ther 2015;41:1132–40. [DOI] [PubMed] [Google Scholar]
- 70.Brydon G, Ganguly R, Ghosh S. The effect of hydroxypropylcellulose on bile acid induced watery diarrhoea. Gut 2003;52(Suppl. 1):A9. [Google Scholar]
- 71.Mroz MS, Keating N, Ward JB, et al. Farnesoid X receptor agonists attenuate colonic epithelial secretory function and prevent experimental diarrhoea in vivo. Gut 2014;63:808–17. [DOI] [PubMed] [Google Scholar]
- 72.Walters J, Johnston I, Nolan J, et al. The response of patients with bile acid diarrhoea to the farnesoid X receptor agonist obeticholic acid. Aliment Pharmacol Ther 2015;41:54–64. [DOI] [PubMed] [Google Scholar]
- 73.Camilleri M, Linker Nord S, Burton D, et al. A double-blind, randomized, placebo-controlled, crossover, multiple-dose study of tropifexor, a non-bile acid FXR agonist, in patients with primary bile acid diarrhea. Gastroenterology 2019;156(Suppl. 1):S204–5. [Google Scholar]


