Abstract
Objective:
Housing instability is prevalent among emergency department (ED) patients and is known to adversely affect health. We aimed to determine the incidence and timing of homeless shelter entry after an ED visit among patients who were not currently homeless.
Methods:
We conducted a random sample survey of ED patients at an urban public hospital from November 2016 – September 2017. Patients provided identifying information and gave informed consent for us to link their survey data with the New York City Department of Homeless Services shelter database. Shelter use was followed prospectively for 12 months following the baseline ED visit. We examined timing of shelter entry in the 12 months following the ED visit, excluding patients who were currently homeless at baseline.
Results:
Of 1,929 unique study participants who were not currently homeless, 96 (5.0%) entered a shelter within 12 months of their baseline ED visit. Much of the shelter entry occurred in the first month following the ED visit, with continued yet slower rates of entry in subsequent months. Patients in our sample who entered a shelter were predominantly male, non-Hispanic black, and commonly had past shelter and frequent ED use.
Conclusions:
In this single-center study, 5.0% of urban ED patients who were not currently homeless entered a homeless shelter within the year following their ED visit. Particularly if replicated elsewhere, this finding suggests that ED patients may benefit from efforts to identify housing instability and connect them with homelessness prevention programs.
Introduction
Emergency department (ED) patients commonly struggle with homelessness and housing instability. A systematic review found homelessness prevalence among ED patients ranging from 2.5%–13.8%.1 Less research has examined housing instability—a broad term encompassing housing needs short of literal homelessness, such as rent burden and frequent moves—but ED studies have reported prevalence of housing instability by varying definitions ranging from 18.1%–43.8%.1 Both homelessness and housing instability are associated with poorer health and more frequent ED use,2,3 and homelessness is associated with 72-hour ED revisits.4 While long recognized as a health and social safety net, a growing Social Emergency Medicine movement is reinvigorating the idea that EDs can and should address patients’ social needs such as homelessness that have strong effects on health.5
To our knowledge, no studies have examined future homelessness among ED patients who are not currently homeless at the time of their ED visit. Identifying literal homelessness is more straightforward than identifying risk for future homelessness; even housing caseworkers perform poorly in predicting which clients seeking services are most likely to become homeless in the future.6 Tracking housing status prospectively can be logistically challenging in emergency medicine research, due to issues such as loss to follow-up. Instead, past research has used various—generally unvalidated—self-reported measures for housing instability.1 The goal of the current investigation was to examine patients’ homeless shelter entry in the year following an ED visit by linking patient survey and longitudinal shelter administrative data.
Methods
Study Design and Setting
We conducted a prospective cohort study of patients presenting to an urban, public, teaching hospital ED and co-located urgent care area (110,000 total visits/year) in New York City (NYC) from November 2016–September 2017. ED patients completed a baseline survey and were followed prospectively for shelter entry using NYC administrative data. Participants provided informed consent and received a $15 incentive. NYU School of Medicine’s Institutional Review Board approved the study.
Selection of Participants
RAs were randomly assigned to a starting patient at the beginning of their shifts and then approached patients in a pre-specified order, following a numbered map of all potential patient locations. While staffing was not designed for RAs to approach every patient in the ED, this sampling scheme ensured that any given patient in the ED had an approximately equal chance of being approached by an RA during a given shift. RA shifts were scheduled seven days/week, at all hours, covering approximately 85 variable hours/week in a distribution designed to cover all time blocks in approximate proportion to ED patient arrival volume including overnights and weekends.
Patients were eligible if they were ≥18 years old and spoke English or Spanish. Patients were ineligible if they were medically unstable/in physical distress, too intoxicated to participate, in psychological distress, in police/prison custody, could not provide consent (e.g., dementia), lived outside NYC, or had already participated.
Measurements
Participants completed a baseline survey administered verbally by RAs, with responses recorded using REDCap electronic data capture. RAs were bilingual (English/Spanish). The survey was professionally translated into Spanish and back-translated to ensure accuracy. The survey was administered as part of a larger study and contained questions on a wide variety of domains, generally taken from previously validated or widely used questionnaires (see Appendix for full survey). In this paper we report results for basic demographics, self-reported number of visits to any ED in the past year, and other social needs. Participants provided their full name, date of birth (DOB), and, if they had one, social security number (SSN), to allow data linkage.
We used the NYC Department of Homeless Services’ (DHS) CARES database, which includes data on shelter use for more than 70,000 adults using NYC emergency shelters yearly. CARES captures approximately 90% of shelter use in NYC; some specialty shelters operated outside the DHS system are not included. CARES contains dates for shelter entries in the system starting in the mid-1980s. It also includes the reason for homelessness that clients gave at the application for shelter, as categorized and recorded by case workers from a list of 34 discrete categories.
The NYC Center for Innovation through Data Intelligence (CIDI)—an agency conducting cross-sector data analysis in the Office of the Mayor—performed data linkage. CIDI used SAS Link King to conduct deterministic and probabilistic matching between a dataset containing a unique participant study ID plus participant identifying information and CARES. Participants with a first and last name plus either a full DOB or SSN were matched with CARES. Approximately 87% of matches were exact matches on all match fields (including DOB, SSN, or both). SAS Link King uses “fuzzy” matching on names/DOBs that are closely related (e.g., off by 1+ character/s); 13% of matches were inexact matches of this sort, all of which CIDI manually reviewed to confirm the match was accurate. This matched dataset was then linked to the ED patient survey data using the unique participant study ID. A de-identified dataset was used for analysis.
Outcomes
The primary outcome was homeless shelter entry within 12 months of the baseline ED visit. Time to shelter entry was measured in days from the baseline ED visit to the first subsequent shelter entry recorded in CARES. We excluded patients who were literally homeless at baseline, which we defined as: 1) self-report of spending the previous night in a shelter, outdoors on the street, or in another place not meant for human habitation; or, 2) any shelter use in the past 7 days documented in CARES. We chose this definition based on data availability, expert and stakeholder recommendation, and U.S. Department of Housing and Urban Development definitions of literal homelessness and homelessness “episodes.”7 Conservatively, we included shelter stays that started the same day as the ED visit as potentially currently homeless, and therefore excluded them from analyses. Due to NYC’s “Right to Shelter” law, most people experiencing homelessness in NYC are sheltered (>95%).8
Analysis
We examined number of days to first shelter entry after the baseline ED visit. We used SAS PROC LIFETEST to plot the failure curve (cumulative incidence curve) of shelter entry. We present descriptive statistics for ED patients who entered a homeless shelter within 12 months of their baseline ED visit and those who did not.
Results
Study sample
RAs approached 6,097 patients, of whom 3,173 (52.0%) were ineligible (most commonly for not speaking English/Spanish [n=489]; in police/prison custody [n=361]; not willing to complete screening questions [n=357]; too ill [n=858], intoxicated [n=496], or psychologically distressed [n=196] to participate; already participated [n=176]; and lived outside NYC [n=157]). Of eligible patients, 2,396 (81.9%) agreed to participate. Duplicate records from patients who participated more than once (n=84) were excluded. Three participants did not give their DOB or SSN to allow for data linkage. Of 2,309 participants whose data could be linked, 316 (13.7%) reported spending the last night on the streets or in a shelter and 222 (9.6%) had a shelter stay in the past 7 days documented in CARES. The 380 total participants (16.5%) fitting either definition of current homelessness were excluded from further analysis, leaving a final analytic sample of n=1,929. Characteristics for these 380 currently homeless ED patients are described in the online appendix (eTable).
Shelter entry after ED visit
Among patients who were not currently homeless, 5.0% (n=96) entered a shelter within 1 year of their baseline ED visit (Figure 1). The most concentrated shelter entry occurred in the first 30 days after the ED visit (n=37 entries), with other entries spread throughout the rest of the year. Table 1 shows self-reported reasons for shelter entry.
FIGURE 1.
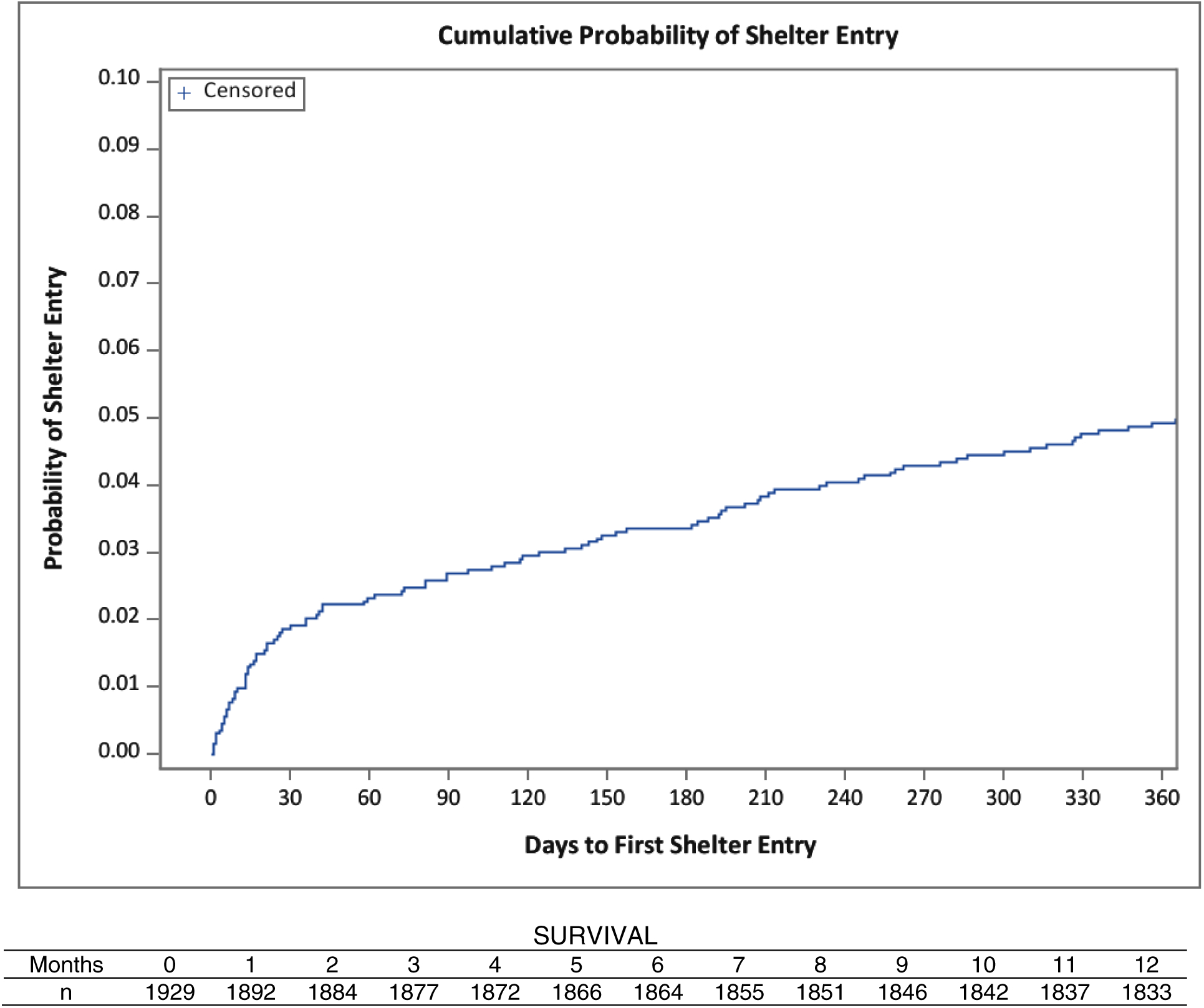
Timing of homeless shelter entry within one year of baseline emergency department visit
96 of 1,929 patients (5.0%) entered a homeless shelter within 12 months of the baseline ED visit, excluding patients who were homeless at baseline (using a conservative definition of self-report of spending the last night on the streets or in a shelter or any documented shelter stay in the past 7 days). We conservatively excluded n=5 patients who had a shelter entry the same day as the baseline ED visit (and who had not self-reported spending the last night on the streets or in a shelter), since it was unknown if the shelter entry occurred before or after the ED visit. If we instead assumed all 5 entered shelter after their ED visit, the shelter entry incidence would be 101/1,934 = 5.2%.
Survival is the inverse of hazard and shows the number of patients each month (30-day time period [35 days between months 11 and 12 to total to 365 days]) that had not yet entered shelter. Subtracting survival number for each month from 1,929 equals the number who had entered shelter by that month following the ED visit.
TABLE 1.
Most common reasons for shelter entry among emergency department patient sample (n=90)a
| n (%) | |
|---|---|
| Discord | 25 (27.8) |
| Otherb | 12 (13.3) |
| Discharge from non-hospital facility or programc | 6 (6.7) |
| Criminal situation at prior residence | 6 (6.7) |
| Loss of income | 6 (6.7) |
| Entering shelter from street homelessness | 6 (6.7) |
| Eviction or vacate order | 6 (6.7) |
| Overcrowding | 4 (4.4) |
| Release from jail or prison | 4 (4.4) |
| Left (prior) facility/program on own accord | 3 (3.3) |
| Discharge from medical hospital | 2 (2.2) |
| Discharge from psychiatric hospital | 2 (2.2) |
| Domestic violence | 2 (2.2) |
| Second tenant | 2 (2.2) |
| Vacate order | 2 (2.2) |
Reason missing for 6 participants. Not listed: 5 additional reasons with only one respondent for each. Reason for homelessness is the reason the client states for why they are applying for shelter, as categorized and recorded by case workers from a list of 34 discrete categories, and therefore encompasses both individual self-report and case worker judgment.
No additional details are available in the administrative data for the “other” category.
Could include detoxification, nursing home, rehabilitation, or other.
Characteristics of shelter entrants and non-entrants (Table 2)
TABLE 2.
Characteristics of patients who did vs. did not enter a homeless shelter within one year of the baseline emergency department visit
| Shelter entrant n=96 n (%) | Not shelter entrant n=1833 n (%) | |
|---|---|---|
| Age, years, mean (sd) | 47.7 (13.3) | 45.6 (16.7) |
| Gender | ||
| Male | 80 (84.2) | 900 (49.2) |
| Female | 14 (14.7) | 923 (50.4) |
| Transgender | 1 (1.1) | 7 (0.4) |
| Race/ethnicity | ||
| Hispanic/Latino | 28 (29.5) | 1106 (60.7) |
| Non-Hispanic Black | 49 (51.6) | 320 (17.6) |
| Non-Hispanic White | 10 (10.5) | 216 (11.8) |
| Other | 8 (8.4) | 181 (9.9) |
| Has children ≤18 years in household | 13 (13.5) | 503 (27.5) |
| Prior shelter historya | 54 (56.3) | 27 (1.5) |
| Insurance | ||
| Uninsured | 8 (8.3) | 555 (30.3) |
| Medicaidb | 52 (54.2) | 564 (30.8) |
| Medicare | 7 (7.3) | 133 (7.3) |
| Dual Medicaid/Medicare | 11 (11.5) | 160 (8.7) |
| Private / Other | 18 (18.8) | 418 (22.8) |
| 4+ ED visits in past yearc | 41 (42.7) | 469 (25.6) |
| Where reported slept the last night | ||
| Own apartment, subsidized | 9 (9.5) | 413 (22.5) |
| Own apartment, not subsidized | 28 (29.5) | 1085 (59.2) |
| Someone else’s apartment | 28 (29.5) | 209 (11.4) |
| Hotel, SRO, or boarding home | 4 (4.2) | 9 (0.5) |
| Institution (hospital, nursing home, etc.) | 21 (22.1) | 84 (4.6) |
| Other | 5 (5.3) | 32 (1.7) |
| Other social needsd | ||
| Inability to meet essential expenses | 50(52.1) | 642 (35.0) |
| Employment issues | 25 (26.0) | 369(20.1) |
| Legal issues | 29 (30.5) | 213(11.7) |
| Food insecurity | 61 (63.5) | 803 (43.8) |
Missing data ≤3% for all variables.
At least 1 prior stay in NYC shelter recorded in CARES administrative data, exclusive of the prior 7 days. All other results shown in the table are from patient self-reported surveys.
New York is a Medicaid expansion state, so low-income single adults are eligible for Medicaid. Undocumented immigrants, however, are not generally eligible for regular Medicaid in New York.
By self-report, including current visit.
Past 12 months. Question on ability to meet household expenses taken from the Survey of Income and Program Participation Wave 9 (2008). Questions on employment and legal issues asked if participant “had any issues or needed help” and were modified from Aidala AA, et al. New York City FUSE II Evaluation Report (available at: http://www.csh.org/wp-content/uploads/2014/01/FUSE-Eval-Report-Final_Linked.pdf). Food insecurity represents a positive response to any of 4 questions from the USDA U.S. Food Security Survey. The full study survey is available in the online Appendix.
Shelter entrants in our sample were predominantly male, non-Hispanic black, and insured by Medicaid. Shelter entrants commonly reported having ≥4 ED visits in the past year. For most, this was not their first episode of homelessness; 56.3% had prior documented NYC shelter use. All study participants, and particularly shelter entrants, commonly reported experiencing other social needs such as food insecurity.
Limitations
The study was conducted at a single NYC public hospital located near a large homeless men’s intake shelter. While a small number of patients with frequent ED use at the study hospital are targeted for care management, patients are not routinely screened for housing instability and it is unlikely that direct referral from the ED to the shelter contributed significantly to our findings. Second, studies like ours that draw their sample from current ED patients will “oversample” frequent ED users, who may have more difficulties with housing. Further, due to our study’s inclusion and exclusion criteria we do not claim to have obtained a representative sample of all ED patients. Third, while our definition of literal homelessness at baseline was aligned with U.S. Department of Housing and Urban Development (HUD) guidelines, there are other possible ways to define homelessness and using another definition might have produced different results. Fourth, we did not have data on unsheltered homelessness, but our analysis was focused on shelter entry by design. Because of NYC’s Right to Shelter law, unsheltered homelessness represents <5% of total homelessness.8 To the extent that ratios of unsheltered to sheltered homelessness differ in other localities, EDs elsewhere might observe different rates of shelter entry after ED use. We do not have data on more “hidden” forms of homelessness such as living doubled up with friends or family, or staying in institutions such as prisons or hospitals. Finally, we did not have information on whether patients were admitted to the hospital during their baseline ED visit. Examining the role of hospitalization in contributing to new shelter entry is an important topic for future research.
Discussion
Five percent of patients in our sample who were not homeless at the time of their ED visit entered a shelter within one year, with over one-third entering in the first month following the ED visit. These findings indicate that a noteworthy number of patients were housing unstable at the time of their ED visit, and build upon the small body of prior research finding high rates of self-reported housing instability among ED patients.1 Approximately 4.1% of Americans report either literal homelessness or living doubled up with others in a given year, less than the one-year prevalence of homeless shelter entry alone observed in our study.9 Characteristics of ED patients entering shelters, at least from one public hospital adult ED, differed from those of the NYC shelter population at large; ED patients entering shelter were predominantly single males, whereas in NYC overall families with children make up two-thirds of the shelter population.8 ED patients who entered shelter reported a wide variety of reasons for applying for shelter, which has important implications for future prevention efforts.
Homelessness has profound effects on health and health services use.10 Knowledge of patients’ housing status can guide ED providers in making appropriate treatment and disposition plans. Our findings also suggest that the ED visit may be a critical juncture for interventions to prevent homelessness and its subsequent negative downstream health effects. For example, ED patients could be screened for risk of future homelessness and connected with community resources designed to provide housing stability supports. It is notable that 16.5% of patients were literally homeless at baseline; these patients were excluded from analyses for this study. This, plus the fact over half of the patients in our study who entered a shelter in the next year had been homeless in the past, suggests that attention to episodic and chronic patterns of homelessness are also needed for ED patients. In the future, we plan to use our linked dataset to conduct more detailed analyses and to develop homelessness risk screening tools. Such efforts are aligned with increasing health system focus on social determinants of health.
Our methods may be useful for other researchers. To our knowledge, we are the first group that has linked survey data collected from ED patients with homeless services administrative data. This unique data linkage allowed us to “follow” patient outcomes prospectively without having to contact patients after their initial study enrollment/baseline ED visit. Such methods may be useful for emergency medicine researchers since ED patients can be challenging to contact for follow-up visits. Further, our methods highlight the feasibility of combining data across different sectors to enhance our understanding of ED patients.
In summary, we found that a notable number of patients enter homeless shelters in the weeks and months following their ED visits. Future research is warranted on the ED’s potential role in screening for and intervening upon housing instability.
Supplementary Material
Acknowledgments:
We would like to thank the EMxSDOH Lab Research Assistants and other volunteers and Donna Castelblanco.
Grant Support: Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health (K23DA039179, PI Doran), the United Hospital Fund (PI Doran), and the Doris Duke Charitable Trust—NYULMC (PI Doran). The content is solely the responsibility of the authors and does not represent the official views of any funder.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: No authors report financial conflicts of interest. Eileen Johns and Maryanne Schretzman work for the New York City Center for Innovation through Data Intelligence, in the Office of the Mayor. Sara Zuiderveen works for the New York City Human Resources Administration.
Contributor Information
Kelly M. Doran, Departments of Emergency Medicine and Population Health, NYU School of Medicine, New York, NY;.
Sara Zuiderveen, New York City Human Resources Administration, New York, NY;.
Marybeth Shinn, Department of Human and Organizational Development, Peabody College, Vanderbilt University, Nashville, TN;.
Rajneesh Gulati, Department of Emergency Medicine, NYU School of Medicine / Bellevue Hospital Center, New York, NY;.
Ian Wittman, Department of Emergency Medicine, NYU School of Medicine, New York, NY;.
Dennis Culhane, School of Social Policy and Practice, University of Pennsylvania, Philadelphia, PA;.
Donna Shelley, NYU College of Global Public Health, New York, NY;.
Tod Mijanovich, Department of Applied Statistics, Social Sciences, and Humanities, NYU Steinhardt School, New York, NY.
References
- 1.Malecha PW, Williams JH, Kunzler NM, et al. Material needs of emergency department patients: a systematic review. Acad Emerg Med. 2018; 25:330–59. [DOI] [PubMed] [Google Scholar]
- 2.Harris M, Gadermann A, Norena M, et al. Residential moves and its association with substance use, healthcare needs, and acute care use among homeless and vulnerably housed persons in Canada. Int J Public Health. 2019;64:399–409. [DOI] [PubMed] [Google Scholar]
- 3.Salhi BA, White MH, Pitts SR, et al. Homelessness and emergency medicine: a review of the literature. Acad Emerg Med. 2018;25:577–593. [DOI] [PubMed] [Google Scholar]
- 4.Ku BS, Scott KC, Kertesz SG, et al. Factors associated with use of urban emergency departments by the U.S. homeless population. Public Health Reports. 2010;125:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doran KM. Commentary: How can emergency departments help end homelessness? A challenge to Social Emergency Medicine. Ann Emerg Med. 2019;74:S41–s44. [DOI] [PubMed] [Google Scholar]
- 6.Shinn M, Greer AL, Bainbridge J, et al. Efficient targeting of homelessness prevention services for families. Am J Public Health. 2013;103 Suppl 2:S324–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Department of Housing and Urban Development. 24 CFR 578.3 - Definitions. Cited 31 July 2018 Available from: https://www.law.cornell.edu/cfr/text/24/578.3.
- 8.The City of New York. 2017. Turning the Tide on Homelessness in New York City. 2017. Cited 30 Aug 2019 Available from: http://www1.nyc.gov/site/dhs/about/tide.page.
- 9.Smith TW, Davern M, Freese J, et al. General social surveys, 1972–2016 cumulative codebook (National Data Program for the Social Sciences Series, no. 24). 2017. Cited 30 Aug 2019 Available from: https://library.uvm.edu/sites/default/files/gss/2016_GSS_Codebook.pdf.
- 10.Lebrun-Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013;48:992–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


