Abstract
Even after 20 years of near gender parity among medical students, the gender composition of physician specialties varies dramatically with some becoming increasingly female-predominant while others remain overwhelmingly male. In their analysis of physician workforce data, the authors demonstrate that despite large increases in the number of female physicians over 4 decades, the degree of gender segregation between specialties has not declined. The authors describe lessons from the highly gender-segregated U.S. workforce as a whole to understand these demographic patterns in the physician workforce. Echoing U.S. workforce findings, women physicians are becoming overrepresented in certain specialties and this appears be associated with a relative decline in earnings for physicians in these specialties over time. The authors found a strong negative relationship between the proportion of female physicians in a specialty and its mean salary, with gender composition explaining 64% of the variation in salaries among the medical specialties.
Female physicians face biases in the workplace and fall behind male peers in leadership attainment, academic advancement, and earnings. Tenacious gender stereotypes and the conflation of gender and status contribute to these biases and reinforce occupational gender segregation. The clustering of women in certain specialties means these specialties will be disproportionately affected by gender bias. Recognizing the consequences of gender demographics within physician specialties is important to maintain the strong and diverse physician workforce needed to support the health care needs of the populations who depend on these specialties for care.
Near gender parity has existed among medical students for almost 2 decades, and 2017 marked the first year that over 50% of U.S. medical school matriculants were women.1 Forty-six percent of residents and fellows in Accreditation Council for Graduate Medical Education-accredited training programs that same year were women.2
Although they are increasing in number, female physicians still face biases and challenges in their work and learning environments. Harassment and assault are distressingly common.3 Female physicians,4 including physician researchers,5 bear heavier home and family workloads than their male physician counterparts. Women are less likely to progress in academic ranks6,7 or rise to leadership roles.7 In the clinical setting, identical patient-centered behaviors yield higher patient satisfaction for male than female physicians,8 placing women at a disadvantage by these metrics. Nonetheless, female physicians have been found to utilize more patient-centered approaches to care9 such as partnership-building and psychosocial talk.10 This may contribute to the observation that visits with female primary care physicians are typically about 10% longer, on average, than visits with male physicians.10 Several recent studies demonstrated better health outcomes with care delivered by female physicians compared with care delivered by male physicians,11–13 which may, at least in part, be a result of these practice differences. These patient-centered behaviors, however, are not fully captured by current Evaluation and Management coding guidelines, placing female physicians at a systematic disadvantage in relative value unit (RVU)-based productivity metrics. Perhaps not surprisingly, the epidemic of burnout among U.S. physicians is particularly acute among female physicians.14
Although the number of female physicians is increasing, these women are unevenly distributed into specialties, ranging from women representing over 60% of U.S. pediatricians to only 5% of orthopedic surgeons.2 As we consider gender bias in medicine, most of the focus has been on its impact on female physicians.15,16 In this Perspective, we consider the impact on the specialties where women are increasingly overrepresented. What will it mean for a specialty when the majority of its physician workforce faces gender bias?
Occupational Gender Segregation in the U.S. Workforce
Gender segregation is a prominent feature of the general U.S. workforce. As of 2012, 44% of men worked in occupations where >75% of the workers were male, whereas only 6% of women worked in those occupations; conversely, 40% of women worked in occupations where the workers are >75% female, but only 5% of men worked in those occupations.17 Segregation can be measured using a statistical parameter called the index of dissimilarity. When applied to occupational gender segregation, the index of dissimilarity is the percent of female (or male) workers that would need to change occupations in order for men and women to be equitably represented in all occupations (i.e., so that the gender composition of each occupation matches the gender makeup of the entire workforce).18 Values approaching 1 (100%) indicate a more segregated workforce and those approaching 0 a more integrated one. The index of dissimilarity gradually trended down in the U.S. through the 20th century as women entered the workforce, ultimately falling to approximately 0.52, but this progress stalled in the mid-1990s. While the index of dissimilarity has plateaued overall, in the youngest cohort of U.S. workers, gender segregation has actually modestly increased from a nadir of approximately 0.49 in 2002 to match the index of dissimilarity among older workers (0.52) [okay?] by 2009.18
The workforce as a whole has seen a gradual influx of women since 1900,19 and is now approaching a steady state near 50%. However, that same pattern toward a 50% equilibrium has not been seen in individual occupations. Instead, data over time demonstrate that once a significant number of women enter a previously male-predominant occupation, the occupation experiences a rapid swing to female predominance (and this phenomenon has not been observed in the reverse).19 This pattern is known as “tipping.” In examining this phenomenon in 14 occupations where the number of women increased by 50 percentage points or more from 1910 to 2000, Pan19 found that, after the number of women in a field reaches a certain critical threshold (a “tipping point”), entry of men into that field rapidly declines. Occupations that have switched from being male predominant to female predominant in this way include bank tellers, secretaries, and teachers. In white collar occupations, the observed tipping points ranged from 25% to 45% female. Tipping points were lower (13% to 30%) in blue collar occupations and in geographical regions where men score more highly on measures of sexism in the General Social Survey, a national representative survey conducted yearly since 1972.19 After considering alternative possibilities, Pan determined that the best explanation for these findings was a loss of occupational prestige following the influx of women.20
In considering gender dynamics in high-skill occupations, it is useful to consider the subset of fields requiring a doctoral degree. Analyzing doctoral degrees (PhDs and EdDs) in 202 fields between 1970 and 2002, England et al21 found the proportion of female doctoral degree recipients in the U.S. rose from 14% to 46%. Despite this large influx of women, the index of dissimilarity in these fields did not change over this 30-year period21 indicating that increased academic achievements by women have not yielded increased gender integration in the workplace. Notably, this study also saw evidence of a tipping phenomenon, finding that men were deterred from earning a doctoral degree in a field once that field reached a threshold of 24% women. Interestingly, they found feminization of a field eventually also deterred women from selecting that degree, but not until the female share reached 38%. Relevant and perhaps fundamental to these findings is the strong negative correlation between the extent to which a field is believed to require innate talents, such as brilliance, and the percentage of women PhDs in that field22 and how early in life these beliefs begin.23
Occupational gender segregation is a major contributor to the gender pay gap, as women are overrepresented in low-paid occupations and men are overrepresented in highly paid occupations. Three major theories for this finding have been considered:24 (1) equalizing differentials, (2) queueing, and (3) devaluation. Equalizing differentials supposes that women are selecting jobs that require less skill or less human capital due to having other priorities (e.g., related to children/family) and that these occupations appropriately have lower wages. However, this does not appear to be the explanation for the pay gap as a negative relationship between “female share” (the percentage of women in the workforce in a given occupation) and wages remains even when controlling for family responsibilities [okay?].24
Queueing theorizes that women are clustered in low-paying occupations due to gender bias in hiring practices. In this theory, men are favored by all employers and therefore compete better for higher-paying jobs, leaving lower paid jobs for women. This theory would be supported if, in longitudinal data, low wages of an occupation at time point A predicted a higher female share at later time point B. Conversely, the devaluation theory posits that work done by women is systematically devalued over time. Longitudinal data showing that earlier higher female share at time point A predicts lower wages at later time point B (the opposite of queueing) would support the devaluation theory. In analyzing 50 years of U.S. workforce data, Levanaon et al24 found brief evidence of queueing in the 1950s, but evidence of devaluation persisted in every decade betwen1950 and 2000, with each 10% increase in female share leading to a 0.5%–5% decline in earnings for an occupation.
It is notable that increasing educational attainment does not mitigate the gender pay gap. In fact, this pay gap is highest among workers with advanced degrees.25 Analysis of workforce earnings data18 shows that, at every level of skill, female-predominant occupations (>75% female) earn less than gender-integrated occupations (25%−75% female), which earn less than male-predominant occupations (>75% male). The negative impact on salary of increasing female share is most pronounced in high-skill occupations. The effect is such that a high-skilled occupation that was 100% female would be predicted to generate 54% of the mean income of a high-skilled occupation that was 100% male.18 An analysis of hourly wages by worker gender, skill level, and occupational gender mix showed that both men and women take a substantial earnings cut by selecting a female-predominant occupation over a male-predominant occupation of the same skill level. This effect was strongest for high-skilled men: on average, men who work in high-skilled female-dominant occupations earn one-third less per hour than men who work in a male-dominant high-skill occupation.17
The loss of prestige and the decline in earnings that are seen after an influx of women in an occupation are rooted in gender stereotypes and the social hierarchy in which men are conferred higher status than women.20 Traits and behaviors stereotypically associated with men (e.g., strong, independent, competitive) are imbued with higher status than those associated with women (e.g., warm, kind, helpful).26,27 Status, occupational prestige, and male gender stereotypes are intertwined. Participants in a study by Cejka and Eagly believed that male-predominant occupations require stereotypically male attributes for success and would be more attractive to male applicants, while female-predominant occupations require stereotypically female attributes and would be most attractive to female applicants.28 Occupations believed to require male attributes for success were also rated higher in prestige and earnings.28 In another study, positions with identical titles and descriptions in the same organization were deemed worthy of a higher salary in a male- vs. female-gendered context (e.g., clerk for hardware vs. clerk for china/crystal).29 At the individual level, multiple experimental studies have found that male applicants are offered higher salaries than identically qualified female applicants30,31 and, when asked to give an actual salary to someone who is “financially very successful,” participants in one study gave a lower dollar amount to a woman than a man with the same job title.32 It is telling that, after their transitions, the average earnings for transgender men increase slightly, while those for transgender women decline by nearly one-third.33
Specialty Gender Segregation in Medicine
The conclusion that gender parity among medical students signifies impending complete gender integration of the medical profession would be short-sighted. The same pattern seen in the workforce as a whole is manifest within medicine, where the male predominance of the broad occupation of “physician” is dissolving only to reappear at the specialty/subspecialty level. Reminiscent of the phenomenon of occupational tipping, the earliest specialties to reach a substantial share of female physicians can now be observed (by looking at the gender composition of their trainees2) to be swinging beyond the 50% steady state that would be predicted by the gender mix of medical students. Obstetrics and gynecology and pediatrics are key examples of this.
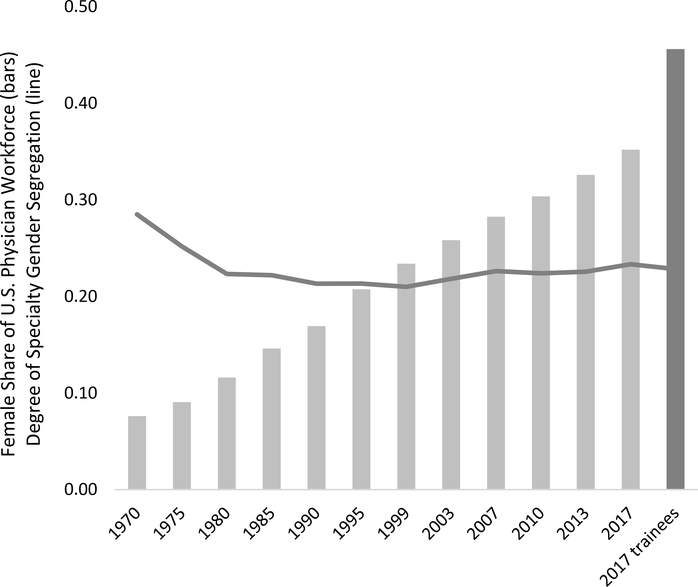
To determine the trends in physician specialty gender segregation over time, we calculated the index of dissimilarity on physician workforce data sets every 3–5 years from 1970 to 2017. In this setting, the index of dissimilarity represents the fraction of female (or male) physicians that would need to move from a specialty where they are overrepresented to one in which they are underrepresented for all specialties to have the same gender composition as the entire physician workforce. All of the data sets were derived from the American Medical Association (AMA) Physician Masterfile (1970–2003 as published by the AMA34,35 and 2007–2017 as published by the Association of American Medical Colleges2,36–38). Figure 1 shows the results of this analysis mapped onto the female share of physicians from each year. While a modest decrease in specialty gender segregation was achieved in the 1970s with the increase in female share from 8% to 12%, no further integration has been achieved in the past 40 years. This indicates that, while there are more women in all of the specialties, trainees continue to distribute into the specialties in ways that reinforce, rather than mitigate, pre-existing gender imbalances. In fact, the specialty gender segregation of the 2017 trainees (residents and fellows) is nearly identical to that of the 1980 physician workforce.
Figure 1.
The increasing female share of the U.S. physician workforce from 1970–20172,34,36–38,59 is shown in the light gray bars (the final dark gray bar indicates data on Accreditation Council on Graduate Medical Education-accredited residency and fellowship programs in 20172). The line indicates the specialty gender segregation, as measured by the index of dissimilarity (the percent of female workers that would need to change occupations in order for men and women to be equitably represented in all occupations), for each of these years. Despite the increase in female physicians (bars) there has been no decrease in gender segregation since 1980.
Specialty preferences already differ by gender at entry into medical school and persist throughout training.39 The potential reasons for gender-based differences in specialty choice echo gender-based preferences in the wider workforce where stereotypical beliefs about the skills, attributes, and values of men and women subtly shape career “choices.”22,40–45 In medicine, women are likely to be seen—by themselves and others—as a better fit for specialties viewed as requiring stereotypically female-gendered attributes like being nurturing and valuing relationships, while for men this sense of fit occurs for specialties viewed as requiring stereotypically male-gendered attributes like technical skills and physical strength. Conversely, the implicit lack of fit for women in male-typed specialties may incite social penalties against women for violating gendered expectations when they do choose these specialties.46–48 Gender-based assumptions also influence availability of mentoring and role models,49 advice received during career selection,39 the content of Medical Student Performance Evaluations,50,51 and the verbal messages given to medical students about career choice.52
Impacts of Specialty Gender Segregation
The well documented biases faced by female physicians predict measurable consequences for a specialty when it becomes female predominant. A number of specialties have reached the tipping point of approximately 25%−45% female that historically has been associated with a decline in men entering a field. Some insights can be gleaned from the specialties that have the highest female share: pediatrics and obstetrics and gynecology. The American College of Obstetrics and Gynecology identifies this gender shift as a defining feature of their workforce.53 It reports that the large increase in female faculty has been associated with increased representation on clinician-educator, as opposed to research-focused, career tracks with an attendant to decrease in promotion rates. Both obstetrics and gynecology53 and pediatrics54 workforce analyses have discussed the impact of the increasing numbers of part time physicians—who are more likely to be women—on workforce projections.
Analogous to the broader workforce, there is a gender pay gap in medicine that can be attributed to various factors, which generally break down into (1) specialty, (2) other work factors (hours worked, number and type of patient encounters, procedures done, practice type/location, payer mix, etc.), and (3) the “unexplained” gap that remains after controlling for specialty and work factors and is presumed to be attributable to gender bias. The unexplained gender pay gap in medicine has been documented many times with a wide range of estimates and in a variety of subgroups of physicians.6,55–59 A recent large study of academic physicians found an unexplained gender pay gap of $20,000 per year.60 Gender-based pay inequities have been demonstrated even at the level of department chair.61
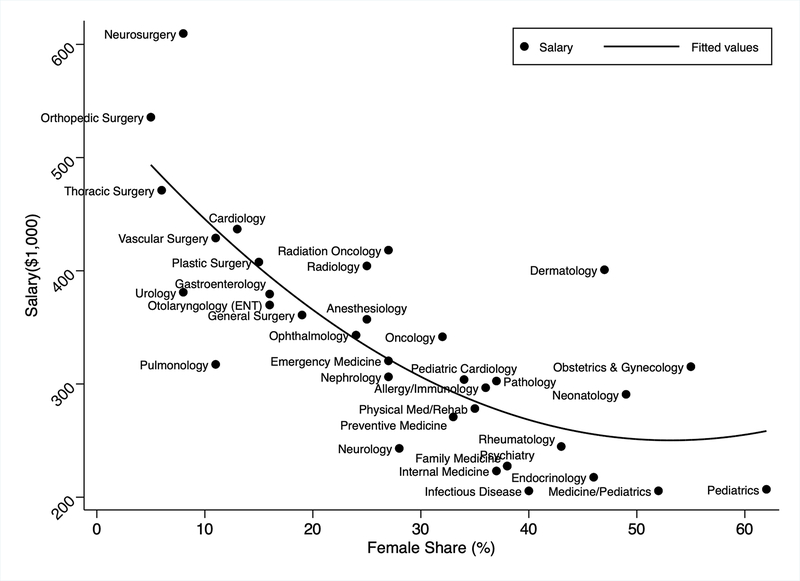
Earnings vary widely among medical specialties, with the highest paid specialties earning 3 times what the lowest paid specialties earn.62 As is seen in the workforce as a whole, women are disproportionately clustered in the lower-earning specialties. Figure 2 shows the relationship between the female share of each specialty2 and its salary (as published by Doximity62 in 2015). We found a strong negative correlation between the presence of female physicians in a specialty and its salary (rs = −0.798, P < .001), with gender composition explaining 64% of the variation in salary among the medical specialties.
Figure 2.
The published salaries of each medical specialty plotted against the female share of the specialty, showing a strong negative Spearman’s correlation with female share explaining 64% of the variation in salaries (rs = −0.798, P < .001).
As the medical profession recapitulates many of the gendered features of the workforce at large, it is worthwhile to consider whether the same forces may explain why female physicians are clustered in lower-paid specialties. Equalizing differentials does not seem likely, as pediatrics and obstetrics and gynecology do not represent career paths that require distinctly less human capital or that carry unusually family-friendly or predictable work hours. In fact, women were not found to be overrepresented in specialties that are known for more controllable hours.39 In terms of queueing, analysis of salaries and female share of 5 major specialties in 1975 (general practice, pediatrics, internal medicine, general surgery, and obstetrics and gynecology) does not show any apparent correlation between earnings63 and female share.34 Specifically, in 1975, the female share was highest in pediatrics (23%), which was the second-lowest earner, but the female share was fairly similar in the lowest-earning specialty (general practice at 5%), the mid-earner (internal medicine at 8%), and the highest earner (obstetrics and gynecology, also at 8%), suggesting that women were not disproportionally shuttled early on into the lowest-paid specialties due to residency selection bias.
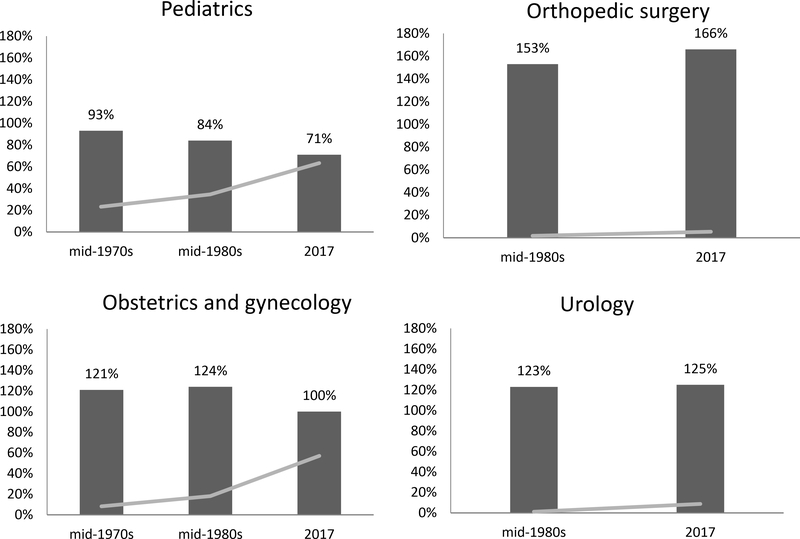
Evidence for devaluation would require reliable longitudinal salary data sets for the medical specialties spanning decades. Nonetheless, some trends can be identified comparing older published salary data63 to online salary reports such as Medscape’s Physician Compensation Report64 for the most female-predominant and male-predominant specialties2,34 (Figure 3). Doing so reveals that the most female-predominant specialty, pediatrics, earned 93% of the average physician salary in 197563 when it was 22% female, but earned only 71% of the median physician salary in 201764 when it was 63% female. Conversely, the most male-predominant specialty, orthopedic surgery, earned 160% of the average physician salary in the mid 1980s63 when it was 2% female and earned 180% the average physician salary in 201764 at 5% female. The decline in salary with a substantial influx of women seen in pediatrics (and not seen in orthopedic surgery, where the female share remains quite small) is consistent with devaluation theory but, given the differences in the clinical activities of these two specialties and the outsized relative value given to procedures, other factors may explain this finding.
Figure 3.
The dark bars show the average salary for each specialty normalized to the median physician salary at the time points indicated. The female share of each specialty at each time point is indicated by the gray line. The two specialties with a higher female share (left side) have demonstrated a greater than 20% decline in earnings relative to the median physician salary, whereas the 2 specialties with minimal female share (right side) have held steady or increased.
Obstetrics and gynecology and urology may offer a more equivalent comparison. The salaries in obstetrics and gynecology were 20%−25% higher than the mean physician salary in the mid-1970s and 1980s63 when the female share was 8% and 18%, respectively. However, by 2017 with a female share of 57%, an obstetrician/gynecologist became an average physician earner.64 In contrast, urology, earned 123% of the average physician salary in the mid-1980s63 when it was 1% female and 125% of the average salary in 201764 when the female share rose but was still low at 9%.
The approximately 20% decline in salary relative to the average physician seen in the 2 most female-predominant specialties, pediatrics and obstetrics and gynecology, over the past 4 decades equates to approximately $60,000/year in lost earnings for the physicians in those specialties in 2017. This estimate dwarfs published estimates of the “unexplained” (within-specialty) gender pay gap in medicine, in some cases several times over. This form of gender-based salary inequity affects all genders in a specialty. If this finding is explained by devaluation, one must conclude that (1) all studies that control for specialty are substantially underestimating the effect of gender bias on physician salaries, and (2) use of specialty-specific national averages to determine individual salaries serves to propagate gender-based salary inequity and is no longer justifiable.
Gender stereotypes can contribute to falling salaries as female share increases in a number of subtle ways. For example, calculation of RVUs, which form part of physician compensation, includes physicians’ responses to surveys about time and effort. As a specialty becomes female-predominant it is relevant that women are socialized to be modest and pay a price for violating this expectation.65,66 These prescriptive gender norms may lead women physicians to underestimate their actual ability and effort in such surveys67,68 and might account for the dramatic RVU reduction by the Center for Medicare and Medicaid Services for several gynecological procedures that occurred in 2015.69
Addressing Specialty Gender Bias Requires Systemic Change
While excellent progress has been made in graduating equal numbers of men and women from medical school, no progress has been made in gender segregation at the specialty level over the past 40 years. Efforts toward improving diversity and representation have focused on recruiting women into specialties where they are underrepresented, but less focus has been given to ensuring that men continue to pursue the specialties where women have already achieved equitable representation. The decline in male entry into these specialties is consistent with the phenomenon of tipping.
It cannot bode well for any specialty’s future to experience a significant drop in interest from half of the applicant pool. This is especially true if the remaining entrants are less likely to advance in academic ranks or rise to leadership positions, and are more likely to experience microaggressions and harassment, face biased expectations in clinical metrics, and have higher risk of burnout. Unless these biases dissipate, this picture will describe 70% or more of the future physician workforce of several specialties/subspecialties, including pediatrics, obstetrics and gynecology, allergy and immunology, and endocrinology. In addition, the effect of devaluation seen in the workforce as a whole—and strongly implied in available salary data in medicine—would predict unfavorable salary trends in these specialties. While both men and women rate financial factors quite low in specialty choice, men are still more likely than women to give it high importance.70 This has the potential to create a vicious cycle where declining prestige and sinking salaries due to the increasing female share and devaluation make it increasingly challenging to recruit male trainees into these specialties. According to data from the Electronic Residency Application Service, endocrinology—the only medical subspecialty to report a lower median salary than general internal medicine on the 2018 Medscape Physician Compensation Survey64—has clear evidence of a decline in interest, with a 12% decrease in female applicants coinciding with a precipitous 43% decrease in male applicants between 2010 and 2014.71
There are two general solutions to this issue we have raised: (1) eliminate gender segregation so that gender bias is equitably shared across specialties, and/or (2) eliminate gender bias so that female predominance is not a liability. Although specific interventions need to be studied, to achieve the former, some recommendations can be extrapolated from research aimed at recruiting more women into male-predominant fields. High visibility of role models and availability of mentors of both genders in all specialties will be important. Female-predominant specialties should ensure that faculty sponsors of medical student specialty interest groups include male residents/fellows and male faculty. Focusing on communal aspects of fields in science and engineering has been used to enhance the interest of girls and women in male predominant fields.40,42,72 In a similar vein, female-predominant specialties could emphasize the more stereotypically male aspects of their fields. This might include showcasing images of male physicians, emphasizing the need for technical skills, and highlighting opportunities for entrepreneurship and leadership.73 Infusion of male-typed words like “challenge,” “independence,” “risk-taking,” and “competitive” that might encourage a sense of fit for male applicants in descriptions of residencies and of the specialty could be tried.74,75 These interventions should increase the chances that interested male students can envision themselves in the specialty and continue to view that option as viable.40,41 However, the challenges described by men in obstetrics and gynecology76,77 suggest that patient expectations and biases may discourage men from entering these fields and will also need to be addressed. Drawing from research on social persuasion, one potential strategy is for clinics to consider posting social norming statements such as “the vast majority of patients in our clinic appreciate access to male and female providers” (or “providers from across the gender spectrum”). 78,79 Importantly, as long the strong correlation between gender composition and earning potential exists, financial factors will continue to influence specialty choice in a way that will be difficult to overcome. Although this is likely only one contributor, professional organizations could educate their members on the process of RVU generation and encourage female members to eschew overly modest responses that might negatively impact RVU determinations.
Others have written extensively on strategies to minimize gender bias.15,44,80,81 This is fundamental to the issue since gender “tipping” is driven by the perception of women having lower status than men. If the conflation of gender and status could be eliminated, this would very likely decrease gender segregation itself. It would also eliminate the impact of devaluation on salaries and the negative role the lower salaries play in recruitment.
Both of these approaches are unlikely to yield rapid progress because they require cultural transformation of existing gender norms which are ubiquitous, continually reinforced, and have shown relatively little change over decades.26 In the meantime, specialties are struggling. Health systems need to recognize the burden of gender bias on increasingly female-predominant specialties. The greater time demands placed on female physicians by patients must be accounted for in compensation plans and/or workload expectations. Correcting the global devaluation of the work of female-predominant specialties is more challenging, but systematically raising the reimbursement for cognitive activities (Evaluation and Management codes) and procedures performed on women82 and children would go a long way to close these between-specialty compensation inequities that are mostly explained by physician gender.
Obstetrics and gynecology and endocrinology are examples of specialties that are rapidly increasing in female share and already known to face workforce shortages.53,83 These specialties, among others, will be disproportionately affected by ongoing issues of gender bias in medicine as they tip toward female-predominant professions. The time is now for the medical community to make gender equity a top priority: for female physicians at large, for the specialties that now hinge on the success of their female workforce and—most important—for the patients who depend on these specialties for care.
Acknowledgments
Funding/Support: M. Carnes is supported by National Institutes of Health grant #R35 GM122557 to conduct research to diversify the scientific and medical workforce.
Footnotes
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Elaine Pelley, Division of Endocrinology, Diabetes, and Metabolism, Department of Medicine, School of Medicine and Public Health, University of Wisconsin-Madison, Madison, Wisconsin.
Molly Carnes, Departments of Medicine, Psychiatry, and Industrial & Systems Engineering and Director, Center for Women’s Health Research, School of Medicine and Public Health, University of Wisconsin–Madison, Madison, Wisconsin.
References
- 1.Heiser S More Women Than Men Enrolled in U.S. Medical Schools in 2017. Association of American Medical Colleges. Published December 18, 2017; https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Accessed June 10, 2020. [Google Scholar]
- 2.Association of American Medical Colleges. 2018 Physician Specialty Data Report. Association of American Medical Colleges Center for Workforce Studies; 2018; https://www.aamc.org/data-reports/workforce/report/physician-specialty-data-report. Accessed June 10, 2020. [Google Scholar]
- 3.Bates CK, Jagsi R, Gordon LK, et al. It is time for zero tolerance for sexual harassment in academic medicine. Acad Med. 2018;93(2):163–165. [DOI] [PubMed] [Google Scholar]
- 4.Parsons WL, Duke PS, Snow P, Edwards A. Physicians as parents: parenting experiences of physicians in Newfoundland and Labrador. Can Fam Physician. 2009;55(8):808–809 e804. [PMC free article] [PubMed] [Google Scholar]
- 5.Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Int Med. 2014;160(5):344–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ash AS, Carr PL, Goldstein R, Friedman RH. Compensation and advancement of women in academic medicine: is there equity? Ann Int Med. 2004;141(3):205–212. [DOI] [PubMed] [Google Scholar]
- 7.Reed DA, Enders F, Lindor R, McClees M, Lindor KD. Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86(1):43–47. [DOI] [PubMed] [Google Scholar]
- 8.Hall JA, Roter DL, Blanch-Hartigan D, Schmid Mast M, Pitegoff CA. How patient-centered do female physicians need to be? Analogue patients’ satisfaction with male and female physicians’ identical behaviors. Health Commun. 2015;30:894–900. [DOI] [PubMed] [Google Scholar]
- 9.Bertakis KD, Azari R. Patient-centered care: the influence of patient and resident physician gender and gender concordance in primary care. J Womens Health. 2012;21(3):326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Pub Health. 2004;25:497–519. [DOI] [PubMed] [Google Scholar]
- 11.Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018;115(34):8569–8574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:j4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019; 94(9):1681–1694. [DOI] [PubMed] [Google Scholar]
- 15.Butkus R, Serchen J, Moyer DV, et al. Achieving gender equity in physician compensation and career advancement: a position paper of the American College of Physicians. Ann Int Med. 2018;168(10):721–723. [DOI] [PubMed] [Google Scholar]
- 16.Carr PL, Raj A, Kaplan SE, Terrin N, Breeze JL, Freund KM. Gender differences in academic medicine: retention, rank, and leadership comparisons from the National Faculty Survey. Acad Med. 2018;93(11):1694–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hegewisch A, Hartmann H. Occupational segregation and the gender wage gap: a job half done. Washington, DC: Institute for Women’s Policy Research; 2014. http://www.iwpr.org/publications/pubs/occupational-segregation-and-the-gender-wage-gap-a-job-half-done. Accessed June 10, 2020. [Google Scholar]
- 18.Hegewisch A, Liepmann H, Hayes J, Hartmann H. Separate and not equal: Gender segregation in the labor market and the gender wage gap. Washington DC: Institute for Women’s Policy Research; 2010. http://www.iwpr.org/publications/pubs/separate-and-not-equal-gender-segregation-in-the-labor-market-and-the-gender-wage-gap. Accessed June 10, 2020. [Google Scholar]
- 19.Pan J Gender segregation in occupations: The role of tipping and social interactions. J Labor Econ. 2015;33(2): 365–408. [Google Scholar]
- 20.Ridgeway CL. Gender, status, and leadership. J Soc Issues. 2001;57(4):637–655. [Google Scholar]
- 21.England P, Allison P, Li S, et al. Why are some academic fields tipping toward female? The sex composition of U.S. fields of doctoral degree recipients, 1971–2002. Sociol Educ. 2007;80(1): 23–42. [Google Scholar]
- 22.Leslie SJ, Cimpian A, Meyer M, Freeland E. Expectations of brilliance underlie gender distributions across academic disciplines. Science. 2015;347(6219):262–265. [DOI] [PubMed] [Google Scholar]
- 23.Bian L, Leslie SJ, Cimpian A. Gender stereotypes about intellectual ability emerge early and influence children’s interests. Science. 2017;355(6323):389–391. [DOI] [PubMed] [Google Scholar]
- 24.Levanon A, England P, Allison P. Occupational feminization and pay: Assessing causal dynamics using 1950–2000 US Census Data. Social Forces. 2009;88(2):865–892. [Google Scholar]
- 25.Vagins D The Simple Truth About the Gender Pay Gap, Fall 2018 Edition. Washington, DC: American Association of University Women; 2018. [Google Scholar]
- 26.Haines EL, Deaux K, Lofaro N. The times they are a-changing … or are they not? A comparison of gender stereotypes,1983–2014. Psychol Women Q. 2016;40(3):353–363. [Google Scholar]
- 27.Conway M, Pizzamiglio MT, Mount L. Status, communality, and agency: implications for stereotypes of gender and other groups. J Pers Soc Psychol. 1996;71(1):25–38. [DOI] [PubMed] [Google Scholar]
- 28.Cejka MA, Eagly AH. Gender stereotypic images of occupations correspond to the sex segregation of employment. Personality & Social Psychology Bulletin. 1999;25(4):413–423. [Google Scholar]
- 29.Alksnis C, Desmarais S, Curtis J. Workforce segregation and the gender wage gap: Is ‘women’s’ work valued as highly as ‘men’s’? J Appl Soc Psychol. 2008;38(6):1416–1441. [Google Scholar]
- 30.Isaac C, Lee B, Carnes M. Interventions that affect gender bias in hiring: a systematic review. Acad Med 2009;84(10):1440–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moss-Racusin CA, Dovidio JF, Brescoll VL, Graham MJ, Handelsman J. Science faculty’s subtle gender biases favor male students. Proc Natl Acad Sci U.S.A. 2012;109(41):16474–16479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biernat M, Manis M, Nelson TE. Stereotypes and standards of judgment. J Pers Soc Psychol. 1991;60(4):485–499. [Google Scholar]
- 33.Schilt K, Wiswall M. Before and after: Gender transitions, human capital, and workplace experiences. B.E. J. Econ. Anal. Policy 2008;8(1):Article 39. doi: [Google Scholar]
- 34.Rich E Physician Characteristics and Distribution in the U.S. 1997/98. Chicago: American Medical Association; 1997. 10.7326/0003-4819-128-4-199802150-00053 [DOI] [Google Scholar]
- 35.American Medical Association. Physician Characteristics and Distribution in the U.S., 2005 Edition. Chicago: American Medical Assocaition; 2005. [Google Scholar]
- 36.Center for Workforce Studies. 2008 Physician Specialty Data. Washington, DC: Association of American Medical Colleges; November 2008. https://www.aamc.org/download/47352/data/specialtydata.pdf. Accessed June 10, 2020. [Google Scholar]
- 37.Center for Workforce Studies. 2012 Physician Specialty Data Book. Washignton, DC: Association of American Medical Colleges; November 2012. https://www.aamc.org/download/313228/data/2012physicianspecialtydatabook.pdf. Accessed June 10, 2020. [Google Scholar]
- 38.Center for Workforce Studies. 2014 Physician Specialty Data Book. Washington, DC: Association of American Medical Colleges; November 2014. https://www.aamc.org/download/473260/data/2014physicianspecialtydatabook.pdf. Accessed June 10, 2020. [Google Scholar]
- 39.Ku MC. When does gender matter?:Gender differences in specialty choice among physicians. Work Occup 2011;38(2):221–262. [Google Scholar]
- 40.Cheryan S, Master A, Meltzoff AN. Cultural stereotypes as gatekeepers: increasing girls’ interest in computer science and engineering by diversifying stereotypes. Front Psychol. 2015;6:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheryan S, Ziegler SA, Montoya AK, Jiang L. Why are some STEM fields more gender balanced than others? Psychol Bull 2017;143(1):1–35. [DOI] [PubMed] [Google Scholar]
- 42.Boucher KL, Fuesting MA, Diekman AB, Murphy MC. Can I work with and help others in this field? How communal goals influence interest and participation in STEM fields. Front Psychol. 2017; 8(Article 901). 10.3389/fpsyg.2017.00901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diekman AB, Brown ER, Johnston AM, Clark EK. Seeking congruity between goals and roles: a new look at why women opt out of science, technology, engineering, and mathematics careers. Psychol Sci. 2010;21(8):1051–1057. [DOI] [PubMed] [Google Scholar]
- 44.Colwell R, Bear A, Helman A (eds). Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine: Opening Doors. Washington, DC: The National Academies Press; 2020. [PubMed] [Google Scholar]
- 45.Block K, Croft A, Schmader T. Worth less?: Why men (and women) devalue care-oriented careers. Front Psychol. 2018; 9(Article 1353): https://doi:10.3389/fpsyg.2018.01353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heilman ME, Okimoto TG. Why are women penalized for success at male tasks?: the implied communality deficit. Journal of Appl Psychol. 2007;92(1):81–92. [DOI] [PubMed] [Google Scholar]
- 47.Kolehmainen C, Brennan M, Filut A, Isaac C, Carnes M. Afraid of being “witchy with a ‘b’“: a qualitative study of how gender influences residents’ experiences leading cardiopulmonary resuscitation. Acad Med. 2014;89(9):1276–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carnes M, Bartels CM, Kaatz A, Kolehmainen C. Why is John more likely to become department chair than Jennifer? Trans Am Clin Climatol Assoc. 2015;126:197–214. [PMC free article] [PubMed] [Google Scholar]
- 49.Kerr HL, Armstrong LA, Cade JE. Barriers to becoming a female surgeon and the influence of female surgical role models. Postgraduate medical journal. 2016;92(1092):576–580. [DOI] [PubMed] [Google Scholar]
- 50.Isaac C, Chertoff J, Lee B, Carnes M. Do students’ and authors’ genders affect evaluations? A linguistic analysis of Medical Student Performance Evaluations. Acad Med. 2011;86(1):59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ross DA, Boatright D, Nunez-Smith M, Jordan A, Chekroud A, Moore EZ. Differences in words used to describe racial and gender groups in Medical Student Performance Evaluations. PLoS One. 2017;12(8):e0181659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Giantini Larsen AM, Pories S, Parangi S, Robertson FC. Barriers to pursuing a career in surgery: An institutional survey of Harvard Medical School students (published online ahead of print October 9, 2019). Ann Surg.. doi: 10.1097/SLA.000000000000361 [DOI] [PubMed] [Google Scholar]
- 53.Rayburn W The Obstetrician-Gynecologist Workforce in the United States. The American Congress of Obstetricians and Gynecologists Office of Workforce Studies and Planning 2017; https://m.acog.org/~/media/BB3A7629943642ADA47058D0BDCD1521.pdf. Accessed July 10, 2019.
- 54.Basco WT, Rimsza ME. Pediatrician workforce policy statement. Pediatrics. 2013;132(2):390–397. [DOI] [PubMed] [Google Scholar]
- 55.Ness RB, Ukoli F, Hunt S, et al. Salary equity among male and female internists in Pennsylvania. Ann Int Med. 2000;133(2):104–110. [DOI] [PubMed] [Google Scholar]
- 56.Weeks WB, Wallace AE. Race and gender differences in general internists’ annual incomes. J Gen Int Med. 2006;21(11):1167–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Weeks WB, Wallace TA, Wallace AE. How do race and sex affect the earnings of primary care physicians? Health Aff 2009;28(2):557–566. [DOI] [PubMed] [Google Scholar]
- 58.Lo Sasso AT, Richards MR, Chou CF, Gerber SE. The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff. 2011;30(2):193–201. [DOI] [PubMed] [Google Scholar]
- 59.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. Jama. 2012;307(22):2410–2417. [DOI] [PubMed] [Google Scholar]
- 60.Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mensah M, Beeler W, Rotenstein L, et al. Sex differences in salaries of department chairs at public medical schools. JAMA Intern Med. 2020;180:789–792. doi: 10.1001/jamainternmed.2019.7540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hamblin J What Doctors Make. The Atlantic. January 27, 2015. https://www.theatlantic.com/health/archive/2015/01/physician-salaries/384846/, Accessed June 10, 2020.
- 63.Langenbrunner JC, Williams DK, Terrell SA. Physician incomes and work patterns across specialties: 1975 and 1983–84. Health Care Financ Rev. 1988;10(2):17–24. [PMC free article] [PubMed] [Google Scholar]
- 64.Medscape. Physician Compensation Report 2018. https://www.medscape.com/sites/public/physician-comp/2018. Accessed Accessed June 10, 2020.
- 65.Phelan JE, Moss-Racusin CA, Rudman LA. Competent yet out in the cold: Shifting criteria for hiring reflect backlash toward agentic women. Psychol Women Q 2008;32(4):406–413. [Google Scholar]
- 66.Moss-Racusin CA, Rudman LA. Disruptions in women’s self-promotion: The backlash avoidance model. Psychol Women Q. 2010;34(2):186–202. [Google Scholar]
- 67.Lind DS, Rekkas S, Bui V, Lam T, Beierle E, Copeland EM 3rd . Competency-based student self-assessment on a surgery rotation. J Surg Res. 2002;105(1):31–34. [DOI] [PubMed] [Google Scholar]
- 68.Carnes M Commentary: Deconstructing gender difference. Acad Med. 2010;85(4):575–577. [DOI] [PubMed] [Google Scholar]
- 69.Uppal S, Shahin MS, Rathbun JA, Goff BA. Since surgery isn’t getting any easier, why is reimbursement going down? An update from the SGO taskforce on coding and reimbursement. Gynecol Oncol. 2017;144(2):235–237. [DOI] [PubMed] [Google Scholar]
- 70.West CP, Drefahl MM, Popkave C, Kolars JC. Internal medicine resident self-report of factors associated with career decisions. J Gen Int Med. 2009;24(8):946–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pelley E, Danoff A, Cooper DS, Becker C. Female physicians and the future of endocrinology. J Clin Endo Metab. 2016;101(1):16–22. [DOI] [PubMed] [Google Scholar]
- 72.Diekman AB, Clark EK, Johnston AM, Brown ER, Steinberg M. Malleability in communal goals and beliefs influences attraction to stem careers: evidence for a goal congruity perspective. J Pers Soc Psychol. 2011;101(5):902–918. [DOI] [PubMed] [Google Scholar]
- 73.Jhamb S Think entrepreneur-think male: Unfolding the gendered characterization of requisite managerial, leadership, and entrepreneurial traits. Carbondale, IL: Southern Illinois University at Carbondale; 2018. [Google Scholar]
- 74.Carnes M Gender: macho language and other deterrents. Nature. 2006;442:868. [DOI] [PubMed] [Google Scholar]
- 75.Gaucher D, Friesen J, Kay AC. Evidence that gendered wording in job advertisements exists and sustains gender inequality. J Pers Soc Psychol. 2011;101(1):109–128. [DOI] [PubMed] [Google Scholar]
- 76.Karlamangla S Male doctors are disappearing from gynecology Not everybody is thrilled about it. LA Times, March 7, 2018. https://www.latimes.com/health/la-me-male-gynos-20180307-htmlstory.html Accessed June 10, 2020. [Google Scholar]
- 77.Lewin T Women’s health Is no longer a man’s world. The New York Times; February 7, 2001. https://www.nytimes.com/2001/02/07/us/women-s-health-is-no-longer-a-man-s-world.html. Accessed June 10, 2020. [Google Scholar]
- 78.Cialdini RB, Goldstein NJ. Social influence: compliance and conformity. Annu Rev Psychol. 2004;55:591–621. [DOI] [PubMed] [Google Scholar]
- 79.Duguid MM, Thomas-Hunt MC. Condoning stereotyping? How awareness of stereotyping prevalence impacts expression of stereotypes. J Appl Psychol. 2015;100(2):343–359. [DOI] [PubMed] [Google Scholar]
- 80.Carnes M The American College of Physicians is working hard to achieve gender equity, and everyone will benefit. Ann Int Med 2018;168(10):741–743. [DOI] [PubMed] [Google Scholar]
- 81.Carnes M, Devine PG, Baier Manwell L, et al. The effect of an intervention to break the gender bias habit for faculty at one institution: a cluster randomized, controlled trial. Acad Med. 2015;90(2):221–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Benoit MF, Ma JF, Upperman BA. Comparison of 2015 Medicare relative value units for gender-specific procedures: gynecologic and gynecologic-oncologic versus urologic CPT coding. Has time healed gender-worth? Gynecol Oncol. 2017;144(2):336–342. [DOI] [PubMed] [Google Scholar]
- 83.Vigersky RA, Fish L, Hogan P, et al. The clinical endocrinology workforce: current status and future projections of supply and demand. J Clin Endo Metab. 2014;99(9):3112–3121. [DOI] [PubMed] [Google Scholar]