Abstract
Type 1 diabetes (T1D) has increased over the past half century and has now become the second most frequent autoimmune disease in childhood and one of major public health concern worldwide. Evidence suggests that modern lifestyles and rapid environmental changes are driving factors that underlie this increase. The integration of these two factors brings about changes in food intake. This, in turn, alters epigenetic regulations of the genome and intestinal microbiota composition, which may ultimately play a role in pathogenesis of T1D. Recent evidence shows that dysbiosis of the gut microbiota is closely associated with T1D and that a dietary intervention can influence epigenetic changes associated with this disease and may modify gene expression patterns through epigenetic mechanisms. In this review focus on how a diet can shape the gut microbiome, its effect on the epigenome in T1D, and the future of T1D management by microbiome therapy.
Keywords: type 1 diabetes, gut microbiota, epigenetics, diet, prebiotics, probiotics
Introduction
Type 1 Diabetes (T1D) is one of the two major autoimmune disorders in infants and adolescents. The T1D prevalence of 1:300 is increasing over the world, representing 5% to 10% of all diabetes mellitus cases (1). T1D is a chronic endocrine and metabolic disorder of carbohydrate metabolism, characterized by the autoimmune T cell-mediated damage of pancreatic β-cells (2). T1D results from the progressive loss of insulin producing β-cells in the islets of Langerhans in the pancreas, commonly in genetically predisposed individuals (3). Both innate and adaptive immune responses are involved in the destruction of beta cells, and insulin therapy becomes mandatory when 80% of the cells are affected (4). It is important to note the contribution of defects in immune regulation and genetic susceptibility that provides insight into the pathogenesis of the disease, which remains largely misunderstood (5). Literature has shown that there are substantial genetic and environmental influences on the onset of type 1 diabetes. In fact, different factors are involved in the development of T1D, including the genome, the gut microbiota and diet (6–8).
Furthermore, various studies have shown that macronutrients and micronutrients and their bioactive components, as well as probiotics, could prevent and manage diabetes mellitus and its complications by a variety of mechanisms. These range from the modulation of insulin secretion and action, to the protection of the β-cells, decrease of inflammation, and the modulation of gut microbiota (6, 9–11). In recent years, the involvement of the gut microbiota in the pathogenesis of several diseases and its role in the management of these diseases has gained much attention (12–18). Today, it is known that the gut microbiota, which refers to all microorganisms inhabiting the gut, is involved in many pathologies and targeting the gut microbiota has become a novel therapeutic strategy (19).
There are about 500–1,000 species in the gut microbiota of humans, with ~100 trillion bacterial cells in the adult intestine (20, 21). Gut microbiota is defined as the environment of commensal microorganisms (bacteria, fungi, viruses, protozoa) residing within the human gastrointestinal tract, interacting with host metabolism, immunity, and other vital physiological functions (22). Four phyla of bacteria represent the major component of the gut microbiota in the gastrointestinal tract; they are Bacteroidetes, Firmicutes, Proteobacteria, and Actinobacteria (23). Bacteroidetes and Firmicutes constitute the most abundant phyla in the adult intestine, while Actinobacteria are the most abundant phyla in breast fed infants (24, 25). Recent data have demonstrated that an alteration or aggravated dysbiosis of intestinal microbiota is implicated in T1D onset in European, American, and Mexican children (26). It has been shown that the diversity of gut microbiota is significantly reduced in patients with T1D, which substantiates the hypothesis that reduced microbiota diversity exacerbates disease pathogenesis (23). One hypothesis is that altered microbiota composition in infancy introduces perturbations in immune system development by promoting intestinal permeability and inflammation (27). Modulating the interface between diet and commensal microorganisms has been shown to correlate with the pathogenesis of T1D, and its onset in genetically susceptible individuals; especially by regulating the epigenetic mechanisms and the abundance of specific bacterial species (Bifidobacteria, Firmicutes, etc.) since they relate to T cell regulation (23). In the current review, we will first describe the role of epigenetics in T1D, before exposing the interactions between the gut microbiota and the epigenome. We will discuss the possible role of diet in modulating the gut microbiome, and current pre-clinical evidence that supports the approach of targeting the gut microbiome in management or treatment of T1D.
Epigenetics in T1D
The symbiotic interplay between commensal bacterial communities and the host involves sophisticated molecular mechanisms of regulation at the epigenetic level. This involves the modification of gene expression as opposed to direct interference with the encoded DNA sequences. Metabolic pathways involved in gut microbiota crosstalk are essential in modifying the heritable changes in gene expression (28). These changes involve most notably patterns of DNA methylation, histone modification, and microRNA (miRNA) regulation (28–30). These different categories of epigenetic modification are found to be associated with insulin secretion and emerging conditions leading to T1D. Illustrations of this can be found in the studies discussed below.
Methylation of the DNA in the coding region of a target gene leads to CpG dinucleotides formation affecting the expression of this gene. Furthermore, hyper and hypo-methylation can be differentiated. While hypermethylation has shown to be responsible for gene silencing, hypomethylation has been shown to induce higher gene expression (23). Various studies have reported such an association between methylated genes and T1D (31–33). The best findings that gene methylation can condition T1D as an epigenetic factor are found in studies carried out in monozygotic twins. Raykan and colleagues conducted DNA methylation analysis of purified CD14+ monocytes from 15 T1D-discordant monozygotic twin pairs, and reported the hypermethylation of 54 genes and hypomethylation in 74 genes (34). In fact, the monocytes are immune effector cells that give rise to tissue macrophages that have been associated with the destruction of the islets cells and thus causing insulin deficiency (34). The authors identified 58 hypomethylation and 74 hypomethylation in variable positions and associated with T1D. Among the hypomethylated genes we can identify for example the hypomethylation of HLA class II gene, HLA-DQB1, which carries the highest single genetic risk for T1D (34). Similarly, another study conducted by Stefan and colleagues focused on DNA methylation profiles in B-cells from 3 monozygotic twins concordant and discordant for the disease (35). In this study, the authors identified 88 CpG sites in which 55 were hypermethylated and 33 were hypomethylated. This showed significant differences in DNA methylation between children with and without the disease; most significantly the hypermethylation of HLA-DOB and HLA-DQA2 genes (35). Another study conducted by Elbouwarej and colleagues provided strong evidence that hypomethylation of CpG sites within the promoter region in discordant monozygotic twins is related to T1D (36). Moreover, it has been shown that the decrease in the immune tolerance in T1D can be regulated by DNA methylation. A study conducted by Li and colleagues showed that the genomic DNA methylation in CD4+ T cells from the latent autoimmune diabetes in adults (LADA) with a subgroup of type 1 diabetes, was significantly increased compared to the controls (37). Also, the same study showed a decrease in the level of the hypermethylated FOXP3 promoter in CD4+ T cells of LADA patients compared with controls; a biomarker of T1D (37). On the other hand, many studies showed variation of DNA methylation within the insulin region (INS), which represent the second most important locus associated with T1D (38–42). In fact, the variation of the DNA methylation within the INS gene is suspected to regulate INS gene transcription in the pancreatic β-cells as well as the medullary thymic epithelial cells. These two tissues are known to be the sites where INS gene is expressed and to be the center of the mechanisms of T1D (43). One study highlighted the relationship between the immune response the DNA methylation changes at Ins1 and Ins2 genes that occurs in both β-cells of non-obese diabetic mice and human β-cells (41). This study suggests that increases in cytokine levels associated with T1D was associated with DNA methylation and decreased in insulin mRNA levels in β-cells (41).
Histone proteins allow the tight condensation of nuclear DNA into chromatin. Furthermore, their modifications cause an alteration in chromatin stability followed by abnormal DNA repair. Many enzymes are involved in epigenetic modulation of histones. These include: acetyltransferases (HATs) which add an acetyl group, histone deacetylases (HDAC) which removes them, histone methyltransferases (MHTs) which add methyl groups to lysine, and arginine residues in histone proteins that may enhance or diminish accessibility of DNA, and histone demethyltransferases (DMHTs) which removes them (44). Studies by Miao showed that various histone modifications are associated with T1D (45, 46). In these studies, a variety of different histone modification of genes (H3K9Ac, H4K16Ac, H3K4me3, H3K9me2,3, H3K27me3) were evident in T1D patients (45, 46). Monocytes from T1D patients had lower levels of H3K9Ac 4 kb upstream of HLA-DRB1 and higher levels of H3K9Ac 4 kb upstream of HLA-DQB1 (46). Similarly, a study conducted on the genomic DNA methylation in CD4+ T cells from LADA investigated whether the histone acetylation of CD4+ T may be involved in the development of LADA. The study showed that the expression of acetyltransferase CREBBP in LADA patients decreased, and that the expression of histone deacetylases HDAC1 and HDAC7 increased (47). Liu and colleagues concluded that a reduction in the histone H3 acetylation contributed to the pathogenesis of LADA (47).
Other epigenetic regulatory mechanisms make use of miRNAs that are involved in the posttranscriptional level of gene expression regulation through direct mRNA degradation or inhibition. A number of studies have revealed that miRNA can participate in the autoimmune damage of β-cells, regulation of insulin synthesis and secretion, and consequently in the pathogenesis of T1D (48, 49). Similarly, it has been shown that an increase in the level of miRNA-21, 29, 34a, and 146a was associated with β-cells dysfunction induced by proinflammatory cytokines (50, 51). Moreover, the study of the genome-wide miRNA expression profiles of T regulatory cells in T1D patients showed a significant increase of the level of miRNA-510 accompanied by a decrease in the level of miRNA-342 and miRNA-191 (52). Furthermore, various studies using cultured cells and animal models of T1D revealed that miRNAs can participate in the autoimmune damage of β-cells and the regulation of insulin secretion and synthesis (46). In fact, Ruan and colleagues showed that 2 genes of the NF-kB family activated the miR-21 gene promoter and thereby increased miR-21 RNA levels; this consequently decreased the level of programmed cell death protein 4 (PDCD4). The deficiency of PDCD4 in pancreatic β-cells renders them resistant to death (46). Thus, the NF-κB–miR-21–PDCD4 axis plays a crucial role in T1D and represents a unique therapeutic target for treating the disease.
Effects of Microbial Metabolites on the Epigenome and T1D
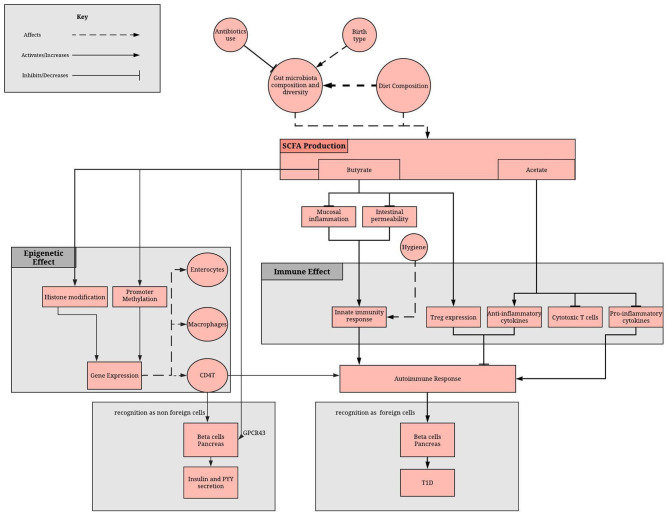
Recent evidence has suggested that the gut microbiota is an important mediator between diet and the establishment of the host epigenome and described how some of the secreted metabolites can affect DNA methylation and histone modifications in host for several diseases (53). However, the molecular mechanisms underlying this complex crosstalk, that is fundamental in achieving and maintaining homeostasis with the host, remain largely unknown (54–56). Butyrate, acetate, polyphenols and vitamins all play important roles in epigenetic regulation of T1D (Figure 1). They are either derivatives of gut microbes and/or are affected by gut dysbiosis.
Figure 1.
Role of the gut microbiome in epigenome and immune system regulation via the SCFA. SCFA production depends on gut microbiota composition and diet. SCFAs, mainly butyrate and acetate, reduces the inflammatory and increases the anti-inflammatory response of the adaptive immunity. Moreover, butyrate methylates promoter regions, affecting gene expression in enterocytes, macrophage and immune cells. A lack of SCFA can result in disruption of these processes, which can result in failure to recognize beta cells as non-foreign cells and therefore an autoimmune damage of pancreatic beta cells.
Butyrate has shown to inhibit the activity of HDAC through its ability to suppress NF-κB activation, repressing the synthesis of interferon gamma and increasing the expression of peroxisome proliferator activated receptor-γ (57). A study conducted in 2015 showed that gut microbiota has an influence on the epigenome of T1D, where dysbiosis in T1D was accompanied by a decrease in butyrate production leading to the development of a permeable gut followed by development of autoimmunity for T1D (57). Another study supported this finding and provided evidence that butyrate has a protective effect on the development of anti-islet cell autoimmunity, associated with differences in the composition of mucin-degrading bacteria and the early introduction of complex food in a cohort of 44 children with and without persistent anti-islet cell autoantibodies (53). A study conducted by Khan and colleagues aimed to investigate the protective role of butyrate on islet β-cell function, proliferation, apoptosis, and glucose homeostasis in T1D mice and revealed that treatment with a salt of butyrate (sodium butyrate) enhanced insulin levels and glucose homeostasis, while reducing blood glucose through HADC inhibition and histone acetylation (58). HDAC inhibition has been associated with insulin gene regulation, β-cell proliferation, and differentiation, as well as the protection of beta cells from apoptosis, thereby counteracting the effects of diabetes. Prior to treatment with butyrate, it was found that almost all the beta islet cells in the diabetic mice were deprived of the endocrine cells, but results post treatment revealed that the cellular damage of islets had been ameliorated, highlighting the protective role of butyrate at both the molecular and tissue level (58). Further, the protective role of butyrate treatment was confirmed by evaluating the expression of transcription factors involved in glucose homeostasis, such as FOXO1. The aforementioned transcription factor plays an imperative role in the regulation of gluconeogenesis and glycogenolysis by switching on genes involved in the transcription of glucose-6-phosphatase, fructose-1,6-bisphosphatase and other enzymes involved in the said metabolic pathways (58). This indirectly increases hepatic glucose production. Further research illustrated that butyrate had significantly downregulated the expression of the FOXO1 transcription factor through mechanisms involving phosphorylation, facilitating insulin signaling and contributing to the improvement of glucose homeostasis.
Acetate is involved in maintaining homeostasis within the mammalian gut, wielding a potent role in the modulation of inflammatory cytokines by downregulating their expression but achieving the opposite effect for anti-inflammatory cytokines (59). An experiment carried out on NOD mice using the immunomodulatory peptide drug Glatiramer Acetate (GA), reported that it was effective at reducing the diabetic rate in the mice and ameliorating insulitis. This coincided with the increased expression of the transcription factor FOXP3, which is involved in regulating the proliferation and differentiation of Treg cells, and was revealed to have mediated the elevated production of IL-4 (60). Thus, the study connotes that GA and dietary acetate can be utilized as potential treatment for T1D through the induction of Tregs (CD4+CD25+ in particular) and that their enhanced function is partly due to the increased production of the anti-inflammatory cytokine IL-4.
Polyphenols are commonly found in fruits and vegetables, and are also produced as a product of the microbial metabolism of dietary foods in the GIT, where they are converted into various aromatic SCFAs such as phenylbutyrate. Additionally, polyphenols are known to inhibit HDAC activity, which may serve as a therapeutic benefit in neurodegenerative diseases such as Alzheimer's, Parkinson's, and Huntington's disease (61). Recent research has proposed that the metabolites exhibit anti- inflammatory properties and can therefore be used to avert chronic inflammation. Furthermore, they are believed to promote the secretion of immunoglobulins and maintain the function of the mucosal barrier of the gut (62). Despite the positive outcomes from extensive research, however, the exact mechanism of polyamine's actions is yet to be elucidated.
Vitamins, including folic acid, B2, B12, and B6, have been shown to be dietary- and microbiota-dependent, being susceptible to dietary intervention and gut dysbiosis (63). These vitamins play a fundamental role in generating S-Adenosylmethionine (SAM), the main methyl-donating substrate for DNMTs and HHMTs, the enzymes used to modulate the histones. In this context, it has been shown that many commensal gut bacteria such as Lactobacillus and Bifidobacterium species are very important in folic acid production, which confer them high consideration to be used as probiotics as we will show later (64).
Taken together, these data suggest that short chain fatty acids (SCFA), such as acetate and butyrate, which are products of the fermentation of non-digestible carbohydrates, such as dietary fibers and resistant starch, seems to possess predominantly beneficial effects including: the reduction of mucosal inflammation in the GIT, strengthening of the epithelial defense barrier to avoid pathogenic infections, and the prevention of insulin resistance and diabetes, among several others. Altered microbiota and SCFAs deficiency has been shown to be primary causal factors triggering T1D (65).
Consequently, a diet low in fat and gluten and high in resistant starch may be the primary driver of increasing the bacterial community responsible for producing butyrate (57). A diet rich of omega-3 polyunsaturated fatty acids (PUFA) induces a decrease in Faecalibacterium, often associated with an increase in the Bacteroidetes and butyrate-producing bacteria, as well as an increase in the production of anti-inflammatory compounds (66). The aforementioned studies provide a step in the direction of a functional understanding of the role played by the gut microbiome in the pathogenesis of T1D and indirectly the influence of the gut microbiota and the secreted metabolites on the epigenome of T1D. However, these finding needs to be validated by larger sample size cohorts and also include metagenomics data.
Gut Microbiome and T1D
The residential community of the host gut microbiota is responsible for a variety of physiological functions associated with maintaining normal systemic and intestinal immunity, and also metabolic homeostasis (67). Gut microbiota diversity has been strongly implicated in the disease etiology of T1D and many studies have shown gut microbiota composition differences between healthy hosts and T1D hosts or people with heightened T1D risk (24).
Consistent with animal models, a number of clinical studies support that changes in gut microbiota diversity are strongly associated and might even be involved in etiology of human T1D (Table 1). It is responsible in particular for disease progression in infants, as well as patients who are at an especially high risk, usually due to genetic predisposition. A considerable number of children who progress to clinical T1D before puberty showed detectable levels of autoantibodies associated with T1D even before the age of 3 years (69).
Table 1.
Pre-clinical and clinical studies on dysbiosis in T1D.
| Study | Study design | Main observations in gut microbiome |
|---|---|---|
| Wirth et al. (68) | Rat model- control vs. streptozotocin -induced T1D. | T1D rats showed heightened levels of Proteobacteria and a reduction in normally dominant phyla (Firmicutes and Bacteroidetes). |
| Siljander et al. (69) | Case control study in 15 children with T1D, 15 children with maturity-onset diabetes pf the young 2 (MODY2) and 15 healthy children. | T1D was associated with a significantly lower microbiota diversity than controls, a significantly higher relative abundance of Bacteroides, Ruminococcus, Veillonella, Blautia, and Streptococcus genera, and a lower relative abundance of Bifidobacterium, Roseburia, Faecalibacterium, and Lachnospira. Proinflammatory cytokines, lipopolysaccharides (LPS). Gut permeability was significantly increased in T1D. T1D when compared with healthy control subjects. |
| Brugman et al. (70) | “In Bio-Breeding” diabetes-prone (BB-DP) rats. | Before the onset of T1D, there was a difference in the composition of gut microbiota between the rats that went on to develop T1D and those that did not. |
| Roesch et al. (71) | BB-DP rat model T1D vs. controls. | T1D had higher levels of Bacteroides, Eubacterium, and Ruminococcus accompanied by lower levels of Lactobacillus, Bryantella, Bifidobacterium, and Turicibacter. |
| Davis-Richardson et al. (72) | 76 subjects with high genetic risk for T1D. Stool analysis from 4–6 month to 2 years old. | Results showed that 29 out of the 76 subjects, showed a specific increase in the relative abundance of Bacteroides dorei; associated to the onset of T1D in the Finnish children. |
| Murri et al. (73) | Case study that included 16 healthy children and 16 children with T1D. | Observed an abundance of Actinobacteria and Firmicutes and a lower ratio of Firmicutes to Bacteroidetes in the children with T1D than in the healthy children. |
| Giongo et al. (74) | Case study of four children using matched case controls. | Decrease in Firmicutes levels and an increase in the Bacteroidetes levels as children developed autoimmune disorders. |
| Vatanen et al. (26) | Analysis of metagenome in 783 children with T1D or predisposition or first degree relative with T1D. | Controls showed more genes that were related to fermentation and the biosynthesis of short-chain fatty acids (SCFAs) (26). |
It has been proposed that the loss of higher diversity in patients with T1D when compared with healthy control subjects might be related to the autoimmune process (69, 75). The changes in gut microbiota composition early in development is useful in predicting the onset of T1D-related autoimmunity, particularly in infants who are genetically predisposed (69, 72, 75).
This might explain why some have proposed a role of the mode of delivery in T1D incidence, while in fact, it is probably a cofounding factor, where the observed increase abundance of Bacterioides in vaginally delivered infants, compared to those born by C section, is due to the infant's contact with the mother's vaginal microbiota upon passing through the birth canal (76–78).
The importance of gut microorganisms is manifest in the vital functions they perform; this includes intestinal epithelium protection, intestinal repair, prevention of the excessive abundance of certain strains of microorganisms and aggravated competition of others, and most notably, carbohydrate fermentation (79). The latter process is especially important in that it yields SCFAs as microbial metabolites which are implicated in a variety of regulatory functions, including modulation of the immune system (80). In fact, gut microbiota are important modulators of both systemic and intestinal immunity since they affect the migration and function of both leukocytes and lymphocytes. They facilitate the discrimination between host cells and pathogenic microbes, which is modulated by the expression of regulatory T cells. In this context, various studies identified Bacteroides, which is an acetate and propionate producing bacteria, as the main genus leading to T1D associated dysbiosis (69, 81, 82). In fact, Bacteroides are proposed to contribute to chronic inflammation by the impairment of the barrier function of the epithelial cell layer (82). Although, many of the Bacteroides can be the origin of the presence of significant higher level of LPS in T1D, which act as a molecular link between gut microbiota, inflammation, and T1D (6, 69), it is important to note that not all Bacteroides species induce the same level of endotoxemia.
Unbalanced gut microbiota was shown to affect also the integrity and permeability of the gut barrier (79). In experimental conditions, early onset autoimmune diabetes has shown to be accompanied by abnormalities of the gut barrier in the form of increased intestinal permeability. It is also accompanied by a decrease in mucus production, which constitutes another important barrier and controls the type of commensal bacteria residing in the epithelium (83–86). Taken together, the abundance, the diversity, the stability, and the connectivity of gut microbiota are associated with T1D development.
Diet, Gut Microbiota, and T1D
Diet is one of the major factors that shape the composition of the intestinal microbiota (44). The diverse bacterial community colonizing different regions of the gastrointestinal tract has been associated with the exposure of the host to certain metabolites following the fermentation of dietary intakes (5). Many studies have shown that exposure to different types of diet at different stages of life may be connected to the development of preclinical and clinical T1D (87–89). As an example, it has been shown that maternal intake of fatty acids and their food sources during lactation may affect the preclinical and clinical type 1 diabetes development in the offspring (89).
The gut microbiota is involved in a number of physiological activities, in addition to its ability to influence lipid and glucose metabolism, and the mucosal immune response. Therefore, it contributes to both systemic immunity and inflammation in the gastro intestinal track (GIT). This is achieved through targeting the endocrine, immune and neuronal cells of the liver and GIT through the metabolites produced by the bacterial fermentation (90). A study conducted by Marino and colleagues involved implementation of a diet-based approach to induce dysbiosis in NOD mice. It was found that the mice developed T1D, which was preceded by the infiltration of the pancreatic islets of Langerhans by abnormal lymphocytes (insulitis). The study demonstrated that a diet high in the two SCFAs (butyrate and acetate) significantly inhibited the onset of the disease (65). The NOD mice were fed diets enriched with either acetylated or butylated high-amylose maize starch; these release significant amounts of their corresponding metabolites as a result of bacterial fermentation. The results indicated that both diets increased the levels of the two metabolites in both feces and blood, thereby protecting the mice from the manifestation of insulitis and T1D (65). Furthermore, the acetate rich diet is thought to predominantly inhibit the proliferation of effector T cells, compromising the activation of cytotoxic T cells and B lymphocytes, ultimately diminishing the effectiveness of the immune system (65, 91). Additionally, the mice exhibited a reduced availability of cells that were unable to perform their function as antigen presenting cells and showed an elevated level of Bacteroides amongst the gut microbiota, which contributes to protection against T1D. The aforementioned effects, however, were absent in the mice fed with a butyrate rich diet. Instead, the mice exhibited an expansion of regulatory T cells (Tregs) and an increase in the expression of occludin; a membrane protein that resides at tight junctions along the colon. Therefore, the diet significantly stabilized the integrity of the mucosal barrier (65). Furthermore, Sun and colleagues showed that the production of butyrate as fermented metabolite was associated with the expression of cathelicidin-related antimicrobial peptide (CRAMP) in the β-cells of NOD mice (92). Actually, this peptide presents a protective effect against T1D development (92). Furthermore, compared to the children who eventually developed T1D, the butyrate-producing bacteria were more abundant in the control group (82). It is therefore conceivable that the ratio of butyrate-producing to other SCFA-producing gut bacteria play a role in T1D.
Previous studies have indicated that proteins can alter the gut microbial composition and affect T1D development in humans and animals (93). A pilot study involving 230 infants at risk of T1D showed that supplementation with a diet rich in hydrolyzed casein (proteins accounting for up to 45% in human milk), was accompanied by a 50% reduction in the incidence of islet autoimmunity (94, 95). The protective effect of the hydrolyzed casein intake may be explained by the decrease in permeability of the epithelium cells by the peptides released after hydrolysis (96). Furthermore, it has been shown that a diet supplemented with gluten can lead to coeliac disease (CD) and may also influence the development of T1D (97, 98). In this respect, Cosnes and colleagues showed that a gluten-free diet plays a role in preventing the development of autoimmune disease (99). A study conducted on NOD mice showed that compared with a gluten-containing diet, a gluten-free diet can delay the onset and decrease the incidence of T1D along with increasing the number of T regulatory cells (100). In the same study, Marietta and colleagues found a decreased number of Bifidobacterium, Tannerella, and Barnesiella species, and an increased number of Akkermansia in the intestine in the presence of a gluten free diet, suggesting the protective role of this diet. Moreover, adding gluten to the gluten-free diet modulates the intestinal microbial composition by increasing the numbers of Bifidobacterium, Tannerella, and Barnesiella species and decreasing the number of Akkermansia. Thus, these data demonstrate that gluten-free diet plays a role in modulating the function of β-cells by changing the intestinal microbiota, which may influence the incidence of T1D.
While the macronutrients participate in shaping and modifying the gut microbiota, it is imperative that the effects of micronutrients receive attention for their contributions, particularly vitamin A, zinc, and iron. A deficiency in vitamin A alters the ratio of Firmicutes to Bacteroidetes and decreases the level of bacteria responsible for the synthesis of butyrate. This, in turn, causes hosts to become susceptible to the development of various chronic diseases, including diabetes (101). Additionally, the retinoic acid metabolite of vitamin A is capable of inhibiting the differentiation of pro-inflammatory Th17 cells derived from IL-6 (amongst the other necessary development cytokines). It also promotes the differentiation of anti-inflammatory Treg immune cells, which are involved in obstructing the manifestation of T1D. The defenses provided by a sufficient iron intake were found to increase the Enterobacteria and reduce the population of Lactobacilli in African children, both of which are involved in shaping the gut microbiome. This results in the secretion of less lactic acid in the GIT, thus promoting the proliferation of a greater diversity of bacterial species; consequently avoiding dysbiosis (6). Moreover, supplementation of zinc has been shown to increase bacterial diversity and activity in the ileum of piglets (102), but a deficiency of zinc can impede the inflammatory response, increasing the development of T1D (103). Finally, the intake and metabolism of the polyphenols has been shown to increase the abundance of bacterial species in the microbiome, such as Bifidobacterium and Lactobacillus spp., enhancing the production of SCFAs, again beneficiary in managing the development of T1D (104–106).
These findings illustrate that diabetes is a multisystemic disorder, and risk and can be reduced by ensuring an intake of a healthy balance of essential dietary nutrients.
Future of T1D Management by Microbiome Therapy
Modulation of T1D Susceptibility by Probiotics
According to the FDA and WHO, probiotics are defined as “live micro-organisms which can provide health benefits on the host when administered in adequate amounts” (107, 108). Traditionally, there are many different probiotics that are widely used: Lactobacillus rhamnosus, Lactobacillus reuteri, bifidobacteria, and certain strains of Lactobacillus casei, Lactobacillus acidophilus-group, Bacillus coagulans, Escherichia coli strain Nissle 1917, and certain enterococci, especially Enterococcus faeciumSF68 (109). Probiotics may be added individually or in mixture of different strains that work in synergy and have additive benefits (109). The function of these probiotics varies within the same species, and may exhibit different benefits when used individually or in formulation. Furthermore, benefits may also differ according to patient group (106).
Since probiotics have been recognized for their beneficial effects on health, they have been used as potential dietary supplements (110). Probiotic health benefits are not only limited to the intestinal tract, but also include amelioration of many diseases and disorders including CVD, T2M, and T1M (111–114). The administration of certain strains of probiotics has resulted in several health benefits for T1D model animals as well as patients as outlined in Tables 2, 3. In fact, de Olveira and colleagues demonstrated that the consumption of probiotics decreases/eliminates dysbiosis and the breakdown of the gut epithelial barrier leading to the normal regulation of the gut membrane integrity and permeability (129). This effect was confirmed by a study of T1D in Bio-Breeding, Disease Prone (BB-DP) rats, where Lactobacilus johnsonii N6.2 was used as a probiotic (116). Several probiotic strains were also used to inhibit the proinflammatory and inflammatory cytokines as showed in different T1D animal models (116, 119, 122, 123, 125, 127). As an example, Lactobacillus kefiranofaciens M and Lactobacillus kefiri K used for STZ-induced C57BL/6 diabetic mice inhibits the proinflammatory and inflammatory cytokines TNFα and TH1 while increasing the production of anti-inflammatory cytokines IL-10 in pancreas (122). Also, the consumption of probiotic fermented milk, with Lactobacillus rhamnosus MTCC: 5957, Lactobacillus rhamnosus MTCC: 5897 and Lactobacillus fermentum MTCC, was associated with significant reduction in serum inflammatory cytokines like IL-6 and TNFα in STZ-induced diabetic rat Moreover, Bifidobacterium spp. was also responsible for reducing blood glucose levels significantly and increasing the protein expressions of insulin receptor β, which promotes the recovery of β-cells of pancreas, increasing insulin sensitivity in STZ-induced C57BL/6 diabetic mice. This is achieved by enhancing the function of the insulin signaling pathway. In summary, Bifidobacterium spp. can be considered as a promising bacteria for treating T1D (120). Since it has been known that SCFAs are able to ameliorate intestinal epithelial barrier integrity, which is responsible partly for protection against T1D (80), many scientists are interested to study the effect of some probiotics that modulate the gut microbiota leading to the increase of the production of this metabolite. The administration of Lactobacillus and Enterococcus probiotic strains from infant gut-origin increases short-chain fatty acid production via modulation of mice and human gut microbiome (130).
Table 2.
Summary of major animal studies of probiotic interventions, their mechanism of action and their outcomes related to T1D.
| Name of Probiotic strains | Study type | Probiotic type and dose | Duration of intervention | Mechanism of action | Outcomes | Reference | Year |
|---|---|---|---|---|---|---|---|
| VSL#3 (VSL Pharmaceuticals, Ft Lauderdale, FL, USA): 3 × 1011 CFU /g of bifidobacteria (B. longum, B. infantis, and B. breve), lactobacilli (L. acidophilus, L. casei, L. delbrueckii subsp. L. bulgaricus, and L. plantarum) and Streptococcus salivarius subsp. thermophilus. | NOD mice | Three times a week of 3 mg/mouse, re-suspended in 100 μl PBS | 28 weeks (from 4 to 32 weeks of age) | - Increases production of IL-10 from Peyer's patches and the spleen and with increase of IL-10 expression in the pancreas - Modulates GALT |
- VSL#3 prevented autoimmune diabetes development in NOD mice - VSL#3 protected mice and induced immunomodulation by a reduction in insulitis severity |
(115) | 2005 |
| Lactobacillus johnsonii N6.2 | T1D in BB-DP Rats | 1 × 108 CFU per animal/day | 21 day | - Changes in the native microbiota, host mucosal proteins, and host oxidative stress response - Decreases oxidative intestinal environment was evidenced by decreased expression of several oxidative response proteins in the intestinal mucosa (Gpx1, GR, Cat) - Decreases of the level of the pro-inflammatory cytokine IFNγ - Increases of the level of the tight junction protein claudin |
- Delays or inhibits the onset of type 1 diabetes in BioBreeding diabetes prone rats. | (116) | 2010 |
| Lactobacillus johnsonii N6.2-Mediated | T1D in BB-DP Rats | 1 × 108 CFU/day through oral gavage | - BBDP rats received oral treatments daily until sacrifice at diabetes onset, or the culmination of the experiment at 140 day | - Diabetes resistance in LjN6.2-fed BBDP rodents was correlated to a Th17 cell bias within the mesenteric lymph nodes - Cytokines IL-6 and IL-23, respectively, were significantly higher within the mesenteric lymph nodes of LjN6.2-fed BBDP. |
- Confirms resistance of T1D and the results published in (117) | (114) | 2011 |
| Lactococcus lactis | NOD mice | Not mentioned | Not mentioned | - Increases the frequencies of local Tregs accumulated in the pancreatic islets, - Suppresses immune response in an autoantigen-specific way - Preserves functional pancreatic islets and reduces in insulitis severity |
- Reversal of autoimmune diabetes by restoration of antigen-specific tolerance: - Treatment strategy for 1TD in human |
(117) | 2012 |
| Lactobacillus plantarum TN627 | Alloxan-induced diabetes in rats | 0.9 × 109 CFU/ml/day | Not mentioned | - Improves the immunological parameters, - Protects the pancreatic tissues, and reduce the pancreatic and plasmatic α-amylase activities and level of plasma glucose in the treated as compared to the control group of rats - Reduces the pancreatic and plasmatic lipase activities and serum triglyceride and LDL-cholesterol rates - Increases the level of HDL-Cholesterol - Protects the liver and kidney functions by decreasing in serum aspartate transaminase, alanine transaminase, lactate dehydrogenase, and gamma-glutamyl transpeptidase activities, as well as creatinine and urea contents. |
- Exhibits attractive in vivo antidiabetic effects that may be helpful in preventing diabetic complications in adult rats | (118) | 2013 |
| Bacterial LPS or Zymosan | NOD mice | 25 μg/mouse/day in PBS | 25 μg/mouse/day in PBS on days 1, 3, 5, 16, 18, and 20 after 12 weeks-old mice | - TLR2 and Dectin 1 engagement by zymosan promotes regulatory T-cell (Treg) responses against the pancreatic β-cell–specific antigen (Ag) - Zymosan induces a mixture of pro - and anti-inflammatory factors and Tregs, both in vitro and in vivo - Increased frequencies of IL-10–, IL-17–, IL-4–, and Foxp3-positive T cells, especially in the pancreatic lymph node |
- Zymosan can be used as an immune regulatory adjuvant for modulating the T-cell response to pancreatic β-cell-Ag - Reverses early-stage hyperglycemia in T1D |
(119) | 2015 |
| Bifidobacterium spp. | STZ-induced C57BL/6 diabetic mice | Not mentioned | 5 weeks | - Reduces the blood glucose levels significantly - Increases the protein expressions of insulin receptor beta, insulin receptor substrate 1, protein kinase B (Akt/PKB), IKKα, and IκBα - Decreases both macrophage chemoattractant protein-1 (MCP-1) and interleukin-6 (IL-6) expression |
- Promote the recovery of β-cells of pancreas or increase insulin sensitivity in mice by enhancing the function of the insulin signaling pathway may be the promising bacteria for treating diabetes | (120) | 2015 |
| Lactobacillus reuteri | STZ-induced C57BL/6 diabetic mice | 109 CFU / 0.3 ml directly into the stomach of mice 3 times per week | 4 weeks | - Develops anti-inflammatory property by inhibiting osteoblast TNF-α signaling - Prevents TNF-α-mediated suppression of Wnt10b and osteoblast maturation markers |
- Blocks the loss of bones open new avenues for use of probiotics to benefit the bone. | (121) | 2015 |
| Lactobacillus kefiranofaciens M and Lactobacillus kefiri K | STZ-induced C57BL/6 diabetic mice | 1 × 108 CFU per day | 8 weeks | - Stimulates the secretion of GLP-1, inhibiting the proinflammatory and inflammatory cytokines, elevating the production of IL-10, and modifying the intestinal microbiota - Decreases of the level of the pro-inflammatory cytokine TNFa and TH1 |
- Potential ability of enhancing GLP-1 to mitigate the progression of type 1 diabetes in vitro and in vivo | (122) | 2015 |
| Oral Probiotic VSL#3 | NOD mice | VSL#3 was administered through oral gavage three times a week | 6 weeks (starting at 4 weeks until 20 weeks of age) | - Inhibits IL-1β expression while enhancing release of protolerogenic components of the inflammasome, such as indoleamine 2,3-dioxygenase (IDO) and IL-33 - Promotes differentiation of tolerogenic CD103+ DCs and reduces differentiation/expansion of Th1 and Th17 cells in the intestinal mucosa and at the sites of autoimmunity within the pancreatic lymph nodes (PLN) - Reduces the Teff/Treg cell balance in the gut mucosa and PLN |
- Prevents autoimmune diabetes by modulating microbiota | (123) | 2016 |
| Lactobacillus brevis KLDS 1.0727 and KLDS 1.0373 | STZ-induced C57BL/6 T1D mice | Not mentioned | 4 weeks | - Capability of KLDS 1.0727 and KLDS 1.0373 strains as gad gene carriers to overexpress GABA significant effect on glucose level reduction in blood or insulin in plasma | - Inhibits the development of T1D in diabetic mice model | (124) | 2018 |
| Probiotic fermented milk with: Lactobacillus rhamnosus MTCC: 5957, Lactobacillus rhamnosus MTCC: 5897 isolated from dairy product (isolated from household curd) and Lactobacillus fermentum MTCC isolated from breast-fed human infant feces | STZ-induced diabetic rat | Not mentioned | 6 weeks | - Decreases in the levels of blood glucose and HbA1c - Increases in the body weight, serum insulin, HDL-C levels in diabetic rats - Decreases in the inflammation, oxidative stress, and gluconeogenesis |
- Can be useful for the complementary treatment strategies of diabetes and its associated complications | (125) | 2018 |
Table 3.
Summary of major human studies of probiotic interventions, their mechanism of action and their outcomes related to T1D.
| Name of Probiotic strains | Study type | Probiotic type and dose | Duration of intervention | Mechanism of action | Outcomes | Reference | Year |
|---|---|---|---|---|---|---|---|
| Lactobacillus johnsonii N6.2 | A double-blind, randomized clinical trial in 42 healthy individuals with no known risk factors for T1D | 1 capsule/day containing 108 colony-forming units of L. johnsonii N6.2 or placebo | 8 weeks | - Significantly decreased the occurrence of abdominal pain, indigestion, and cephalic syndromes - Icreased serum tryptophan levels increased resulting in a decreased K:T ratio - Monocytes and natural killer cell numbers were increased significantly - Increases of circulating effector Th1 cells (CD45RO+CD183+CD196–) and cytotoxic CD8+ T cells |
- Potential and safety therapeutic in prevention risk for T1D. | (126) | 2017 |
| Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb12 | 96 children aged 8 to 17 years with newly diagnosed T1D | 109 UCF/day or placebo | 6 months | - Modulate the immune system for preventing islet cell destruction - Improved the gut mucosal barrier |
- Preserves cell function by reducing the risk of autoimmunity - Reduce/inhibits the growth of pathogens |
(127) | 2017 |
| Probiotics | 1039 individuals (mean age 46 ± 14 years, 45% men) with T1D and without end-stage renal disease | Not mentioned | 2 years | - Decrease in obesity, body mass index - Regulated HDL-cholesterol, triglyceride components and blood pressure |
- Better health related to diabetic disease | (128) | 2017 |
In addition to the use of probiotics in animal models, the use of probiotics in humans at risk for T1D and in human T1D sufferers has also been investigated (Table 3). In fact, concerning those with elevated risk of T1D, studies revealed that an early supplementation of probiotics might lead to a decrease in the risk of islet β-cell autoimmunity (126, 131). Moreover, it has been shown that the use of probiotics in T1D adults was associated with a better glycemic control, reduced TLR4 inflammatory signaling, and also increased synthesis of glucagon-like peptide-1 (GLP-1), which is a hormone that stimulates the secretion of pancreatic beta cells leading to a decrease in blood sugar levels (132, 133). All these changes were associated with decreased incidences of T1D. A double-blind, randomized clinical trial in 42 healthy individuals with no known risk factors for T1D showed that the administration of 1 capsule/day containing 108 UCF of L. johnsonii N6.2 or placebo for 8 weeks increased the circulating effector Th1 cells (CD45RO+CD183+CD196–) and cytotoxic CD8+ T cells. The data provided by this study, shows promise for the safety and feasibility of using L. johnsonii N6.2 in prevention trials involving subjects at risk for T1D (126). Another lactobacillus strain, Lactobacillus rhamnosus, in combination with another strain Bifidobacterium lactis Bb12, was administrated to 96 children aged 8 to 17 years with newly diagnosed T1D. A dose of 109 UCF/day was given for 6 months. The mixture of these two strains can modulate the immune system thus preventing islet cell destruction and improving the gut mucosal barrier; this consequently reduces the risk of autoimmunity and reduces/inhibits the growth of pathogens (127). Furthermore, studies from 6 clinical centers in Europe and United States examined the association between supplemental probiotic use during the first year of life (0–27 days) and islet autoimmunity among children at increased genetic risk of T1D (131). Although, these TEDDY studies showed that early probiotic supplementation either by dietary supplements or though infant formula may reduce the risk of islet autoimmunity in children at the highest genetic risk of T1D, the result needs to be confirmed in further studies before any recommendation of probiotics use is made. Furthermore, it has been shown that the use of probiotics by T1D adult patients (mean age 46 ± 14 years, 45% men) is associated with better glycemic control and amelioration of metabolic syndrome, such as high triglyceride levels, high blood pressure (128). Altogether, these facts suggest (1) that early life exposure to probiotics can reduce the risk of T1D progression and (2) the potential of different probiotic strains in managing T1D via ameliorating the gut microbiota-immune system axis may have prompted the multiple, ongoing, new clinical human trials using probiotics to prevent/treat T1D. These studies are summarized in Supplementary Table 1.
Modulation of T1D Susceptibility by Prebiotics
Like probiotics, some selective prebiotics have also been reported to be beneficial as shown in various animal and human studies (134–138). In 2017, Gibson and colleagues revisited the definition of prebiotics as “a substrate that is selectively utilized by host microorganisms conferring a health benefit” (139). In order to consider a food supplement as a prebiotic, it must have the following three criteria: (1) resistance to gastric acidity, hydrolysis by mammalian enzymes, and gastrointestinal absorption; (2) fermentation by intestinal microflora; and (3) selective stimulation of the growth and/or activity of intestinal bacteria associated with health and well-being (139, 140). Presently the most widely accepted prebiotics that fulfill the above criteria are lactulose, inulin, fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS) and the human milk oligosaccharides (HMO) (Table 4) (141–148). Despite the several updates concerning the concept of prebiotics over the years, it remains controversial whether a specific prebiotic must stimulate only one or various bacteria at the same time. Recent studies provided evidence that probiotics show some specificity for the prebiotics they may utilize (141–143). In fact, the ability to metabolize carbohydrates/prebiotics by intestinal bacteria was attributed to specific enzymes produced by these bacteria (Table 4). This further suggests that these bacteria present specific gene clusters in their genome that encode for enzymes involved in the metabolism of prebiotics; examples include β-Galactosidase from Bifidobacterium adolescentis (141), and β-fructofuranosidase by some Bacteroides (149). In human and animal models, the major fermented products of carbohydrate metabolism produced by gut microbiota are SCFAs. These bacterial metabolites appear to promote the development of a healthy immune system as shown by in vivo studies in animal models (Table 5) and humans (Table 6).
Table 4.
Major prebiotics, their sources and the basis of bacterial specificity.
| Prebiotics | Sources | Specific related bacterial enzyme | Specific bacterial group | Fermented products | References |
|---|---|---|---|---|---|
| Inulin type fructans Inulin Oligofructose |
β-fructofuranosidase (fructanase) | Bifidobacteria Lactobacilli Bacteroides |
Acetate, lactate Lactate Acetate, propionate |
(146) (143) (149) |
|
| Chicory (inulin) | |||||
| Enzymatic hydrolysis of inulin Oligofructose | |||||
| Fructo-oligosaccharides (FOS) | Enzymatic synthesis from sucrose FOS | β-Galactosidase | Bifidobacterial | Acetate, lactate | (141, 142, 144, 145) |
Table 5.
Summary of major animal studies of prebiotic interventions, their mechanism of action and their outcomes related to T1D.
| Name of Probiotic strains | Study type | Prebiotic type and dose | Duration of intervention | Mechanism of action | Outcomes | Reference | Year |
|---|---|---|---|---|---|---|---|
| Low antigen, hydrolyzed casein (HC)-based diet | LEW.1AR1-iddm ramodel | Fed daily | 50 to 90 days | - Decreases in CD4+ Foxp3+ regulatory T (Treg) cells in pancreatic lymph nodes (PLN) - Decreases the expression of CD3+ T cells, CD163+ M2 macrophages and Foxp3+ Treg cells in the jejunum - decreases the Ifng/Il4 ratio, suggesting that the HC diet impacted M1/M2-associated cytokine balance - Corrects the gut immune cell deficits and increases the immunoregulatory capacity |
- Prevention against T1D | (150) | 2015 |
| Dietary Resistant Starch | STZ-induced T1D Sprague-Dawley rats | 550 g/kg diet | 4 weeks | - Enhances GLP-1 and peptide YY secretion in vivo, which enhance β cell proliferation and insulin secretion improved the gut mucosal barrier - Protects the nephron |
- Delayed the progression of diabetic nephropathy and maintained vitamin D balance in streptozotocin (STZ)-induced type 1 diabetic (T1D) rats develops normalized growth pattern in T1D | (151) | 2016 |
| Inulin-type fructans (ITFs), natural soluble dietary fibers with different degrees of fermentability from chicory root | NOD mice | Not mentioned | 24weeks | - Increases CD25+Foxp3+CD4+ regulatory T cells, - Decreases IL17A+CD4+ Th17 cells, - Modulates cytokine production profile in the pancreas, spleen, and colon. - Increases the expression of barrier reinforcing tight junction proteins occludin and claudin-2, antimicrobial peptides β-defensin-1, and cathelicidin-related antimicrobial peptide - Enhances SCFAs production - Enhances Firmicutes/Bacteroidetes ratio to an antidiabetogenic balance and enriched modulatory Ruminococcaceae and Lactobacilli. |
- Protects against autoimmune diabetes by modulating gut immunity, barrier function, and microbiota homeostasis. –> delays T1D development | (152) | 2017 |
| Wheat flour | NOD mice | Fed daily | 72 days | - Lacks the epitopes linked with T1D - Reduces the levels of IFN-γ, a proinflammatory cytokine involved in the autoimmune pathogenesis of T1D - Increases the levels of IL-10, an anti-inflammatory cytokine potentially implicated in hindering T1D development |
- Reduces the incidence of T1D. | (153) | 2017 |
| GABA therapy | STZ-induced C57BL/6 diabetic mice | Fed daily | 11 weeks | - Increases Klotho levels in the serum, kidneys and pancreatic islets. - Stimulates the production and secretion of Klotho by human islet cells in vitro. - Stimulates the proliferation and insulin secretion by human islets - Klotho suppresses NF-κB activation - Increases insulin secretion |
- Important implications for the treatment of T1D | (154) | 2017 |
| Caffeic acid-rich fraction from Prunella vulgaris L plant | Alloxan-induced diabetic mice | Fed daily | 8 weeks | - Reduces blood glucose levels and improved in-vivo oxidative-stress - Inhibits the carbohydrate-hydrolyzing enzymes (alpha-amylase and alpha-glucosidase) - Reduces HbA1c levels - Increases serum-insulin levels |
- Possess antidiabetogenic and antinociceptive properties could be a potential therapeutic agent to ameliorate T1D and related complications. | (155) | 2018 |
| Human milk oligosaccharides consisting of both long-chain, as well as short-chain structures | NOD mice | Fed daily | 6 weeks | - Increases anti-inflammatory microbiota-generating metabolite [i.e., short chain fatty acids (SCFAs)] - Induces anti-diabetogenic cytokine profiles - Induces the development of tolerogenic dendritic cells (tDCs), priming of functional regulatory T cells, which support the protective effects - Increases butyrate production promoting mucin synthesis improving the intestinal barrier integrity |
- Delays and suppresses T1D development in non-obese diabetic mice and reduces the development of severe pancreatic insulitis in later life - Vital in the protection of children at risk for T1D, supporting immune and gut microbiota development in early life. |
(156) | 2018 |
Table 6.
Summary of major human studies of prebiotic interventions, their mechanism of action and their outcomes related to T1D.
| Name of Probiotic strains | Study type | Prebiotic type and dose | Duration of intervention | Mechanism of action | Outcomes | Reference | Year |
|---|---|---|---|---|---|---|---|
| Dietary fiber | 106 outpatients with type 1 diabetes; age 40 ± 11 years | fiber intake > 20 g/day | - | - Develop anti-inflammatory properties - Shows inverse association between some nutritional habits and highly sensitive -C-reactive protein (hs-CRP) |
- Suggests that an increased consumption of dietary fiber > 30 g/day may play a role in reducing inflammation in individuals with type 1 diabetes. - Lower the risk of coronary disease |
(157) | 2014 |
| Oligofructose enriched inulin | Randomized, double-blind, placebo-controlled trial in children aged 8 to 17 years with T1D for at least 1 year | Placebo (maltodextrin 3.3 g orally/day) or prebiotics (oligofructose-enriched inulin 8 g orally/day; Synergy1, Beneo, Mannheim, Germany) | 12 weeks | - Changes gut microbiota, gut permeability and inflammation. - Decreases endotoxemia and reduces insulin resistance - Improves glycemic control |
- Potentially novel, inexpensive, low-risk treatment addition for T1D | (134) | 2016 |
| Adjunct therapy with dapagliflozin | 33 youths (14 males, median age 16 years, diabetes duration 8 years) | 10 mg DAPA or placebo during dosing visits | - | - Reduces the insulin dose required as a medication - Improves the glycemic control by targeting the glucose level - Increases the urine glucose excretion |
- Potential therapy in the pediatric age group by lowering insulin dose and increasing glucose excretion. | (135) | 2017 |
| Dietary fiber intake | 111 outpatients with T1D | daily intake (<14 g fiber/1,000 kcal) or (≥14 g/1,000 kcal) | dietary intake was evaluated by 3-day weighed-diet records | - Reduction in the use of medicine for diabetes (insulin) and hypertension (ACE inhibitors) treatment - Shows lower the blood pressure - Shows lower body mass index (BMI) - No significant association between increased fiber intake (≥14 g/1,000 kcal/day) and serum levels of total cholesterol, HDL cholesterol, or LDL cholesterol. |
- Associated with lower blood pressure levels in patients with type 1 diabetes | (136) | 2018 |
In the last 5 years an increasing number of studies using animal models have shown that the intake of dietary fibers plays an important role in maintaining gut microbiota homeostasis; this leads to a delay in the development of T1D (Table 5). For example, feeding LEW.1AR1-iddm rats with a low antigen, hydrolyzed casein-based diet was shown to correct gut immune cell deficits and increase immunoregulatory capacity leading to protection against T1D (150). Similarly, feeding NOD mice with wheat flour for 72 days shows the same effect with a decrease in the levels of IFN-γ (a proinflammatory cytokine involved in the autoimmune pathogenesis of T1D) and an increase in the levels of IL-10 (an anti-inflammatory cytokine potentially implicated in hindering T1D development) (127). One study involved the feeding of NOD mice with chicory root, which is rich in Inulin-type fructans ITFs; a natural soluble dietary fiber with different degrees of fermentability. This 24-week treatment was protective against autoimmune diabetes due to its action of modulating gut immunity, improving barrier function, and promoting microbiota homeostasis. These factors resulted in the delay of T1D development (152). Furthermore, the intake of this prebiotic was found to enhance SCFAs which modulate the production of cytokines in the pancreas, spleen, and colon. Also, the intake of ITFs enhances the Firmicutes/Bacteroidetes ratio to an antidiabetogenic balance and enriches modulatory Ruminococcaceae and Lactobacilli. Altogether, these changes consequently increase the expression of the gut barrier by reinforcing tight junction proteins thus decreasing its permeability. Feeding NOD mice with Human milk oligosaccharides (HMOS), consisting of both long-chain, as well as short-chain structures, has also been found to increase the anti-inflammatory microbiota-generating metabolite SCFAs (156). In fact, the increase of butyrate production has been shown to promote mucin synthesis, thus improving intestinal barrier integrity. This has been found to delay and suppress T1D development in NOD mice, and to reduce the development of severe pancreatic insulitis in later life. This suggests that the supplementation of HMOS may be vital in the protection of children at risk for T1D by supporting their immune system and their gut microbiota development in early life. Supplementation of dietary resistant starch (the caffeic acid-rich fraction from Prunella vulgaris L plant) and the use of GABA therapy proved that those prebiotics had beneficial effects on animals and that they could form a potential therapeutic agents to ameliorate T1D and related complications (151, 154, 155).
The use of prebiotics in human subjects with T1D has also been investigated (Table 6). In a single-center, randomized, double-blind, placebo-controlled trial in children aged 8 to 17 years with T1D, the consumption of oligofructose and-enriched inulin for at least 1 year was shown to positively modulate intestinal permeability and reduce of inflammation by increasing the number of Bacteroidetes and lactic producing bacteria, thus improving glycemic control and reducing the chances of T1D occurrence (134, 138). Another study of 106 outpatients with type 1 diabetes and having an age of 40 ± 11 years, involved supplementation with dietary fibers; outcomes included a lower risk of coronary disease (157). Furthermore, this study suggested that an increased consumption of dietary fiber (>30 g/day) may play a role in reducing inflammation in individuals with T1D. Another study published in 2018, involved a group of 111 outpatients with T1D. Following a high fiber, prebiotic, dietary supplement, there was a subsequent reduction in the use of medicine for diabetes (insulin) and hypertension treatment (ACE inhibitors), and also a lowering of blood pressure (136). Moreover, in a randomized, double-blind, placebo-controlled, pilot study of children aged 8 to 17 years with T1D, the intake of oligofructose enriched inulin was accompanied by: (1) altered gut microbiota, gut permeability, and inflammation, (2) decreased endotoxemia and reduction of insulin resistance, and (3) improved glycemic control (134). This prebiotic may be a potentially novel, inexpensive, low-risk treatment addition for T1D. The positive effects of the intake of oligofructose can be explained as follows. This prebiotic is metabolized by different bacteria species like Bifidobacteria, Lactobacilli, or Bacteroides under the presence of the β-fructofuranosidase enzyme. It follows that they will produce different metabolites (acetate, lactate, and propionate) (140, 143, 149). Although the produced SCFAs has been shown to alter the host immune system and ameliorate T1D (104), a recent randomized controlled trial showed that oral butyrate administration for 1 month to 30 individuals with longstanding T1D did not result in any significant changes in innate immunity and islet autoimmunity (158).
Altogether, these facts demonstrate the potential of different prebiotics in preventing and managing T1D. As in the case with probiotics, their promise may explain the new, multiple, ongoing clinical human trials using prebiotics to prevent/treat T1D, which are summarized in Supplementary Table 2.
Modulation of T1D Susceptibility by Symbiosis
Previous studies have shown that probiotics and prebiotics may improve glucose metabolism. In order to improve their potential therapeutic efficacy, they may be used together as “symbiotics.” This means that probiotics and prebiotics can complement each other or even work in synergy to provide a combined effect. There are several recent studies that have shown positive synergetic effects of symbiotics using animal studies and clinical human studies for different diseases including T1D (159–166). For example, the supplementation of a combination of Bifidobacterieum animalis ssp. Lactis (B420) as a probiotic and polydextrose as a prebiotic has been investigated using Ketogenic diet-induced C57Bl/6J diabetic mice. After this 4-week supplement regime, the mice showed an increased concentration of portal GLP-1, a decreased glycemic response, and lower plasma glucose concentration (Supplementary Table 3) (159). This improved the efficacy of metformin, a benefit for combining probiotics and/or prebiotics with antidiabetic drugs, which show promise for transferring this study to the clinical level.
Limitations and Lessons Learned From Experimental Studies
Fundamental and pre-clinical studies support the promising role of probiotics in the management and treatment of diabetes. An important study by Cheng and colleagues showed that a short-duration diet that mimics fasting can induce regeneration of β-cells and rescue mice from not only T2D but also T1D (167).
Although both animal and human studies showed the promising effect of diet and pro/prebiotics in managing T1D, we should bear in mind that autoimmune diabetes observed in mice is not identical to those observed in humans (168). In fact, a major difference between these two species is the time of the T1D development. While NOD mice typically show the disease close to their maturity, human seroconversions peak has been shown to occur during the first 3 years of life (168). Moreover, what makes the comparison even more complicated is that nearly all autoimmune diabetic cases occur in adult NOD mice, whereas approximately half of the cases appear before adult age in humans (168).
Also, we should emphasize that most of the available clinical trials come from studies that have used different methodologies, which makes comparison difficult. Although the obtained outcomes hinder a clear conclusion, it reveals a clear trend. For example, the trials differ greatly in sample size; furthermore, homogeneity of the patients in terms of demographics, symptoms, and dietary habits is lacking. There are also inconsistencies in strains, dose, and duration of probiotic/prebiotic intervention that limit the possibility of identifying which probiotic/species/strain or therapy has contributed the most to prevent/delay the disease in humans with high risk and/or help in managing the disease in T1D patients. Moreover, human studies mainly reveal associations between diet, gut microbiota and T1D rather than causal relationship.
Furthermore, attention should be given to the safety of probiotics in clinical practice. In fact, although probiotics have an excellent overall safety record, they should be used with caution in susceptible individuals, particularly neonates born prematurely or with immune deficiency. This is because excessive immune stimulation may be caused by probiotics in vulnerable individuals (169). Moreover, some secondary effects have been presented in the presence of some probiotic strains. Fungal sepsis caused by S. boulardii has also been reported (170), along with minor bacteremia, sepsis, and cholangitis induced by Bacillus subtilis and by lactobacilli L. rhamnosus GG or L. casei (169–171).
An important feature of TD1 in humans is that by the time of diagnosis, it is difficult to revert it, and the influence of the diet and/or microbiome therapy might be dependent on the relative time-to-diagnosis. Some have suggested that microbiome therapy could constitute a preventive measure before seropositivity; others suggested the possibility of reversing T1D through isolated case reports. Indeed, a recent study showed that two cases of T1D in pediatric subjects were treated with supplementation of high dose vitamin D and omega 3 and a similar pattern of remission of the disease was observed, resulting in restoration and subsequent persistence of optimal metabolic control, one and 2 years after T1D onset (172). The study also showed that a minimal basal insulin administration (0.1 IU/kg/die) in a single evening injection was required. Although this study showed promise for this diet, larger controlled studies are needed to determine the effect of the proposed intervention to slow down or halt the progression of autoimmunity. Furthermore, although patients with T1D showed a reduced microbial diversity and a proinflammatory intestinal dysbiosis, studies revealed that microbiome therapy may contribute to the reduction of intestinal permeability, the reduction of inflammation and to the improvement of glycemic control in T1D patients. Moreover, we should bear in mind that during the first 3 years of life the gut microbiome undergoes dynamic changes before becoming more stable, which provides a time window between birth and 3 years of age to apply a diet and a supplementation of pre/probiotics to children with predisposition of T1D or first-degree relative(s) with T1D. In fact, during that period, guidance in developing an equilibrate gut microbiome, and training for the developing immune system are required in order to establish self-tolerance and to control inflammatory responses.
Conclusions and Future Plans
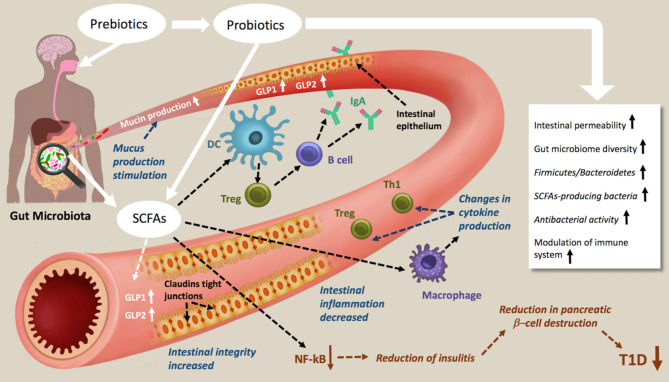
The change in expression of genes is non-genetically determined and depends largely on environmental factors. Recent advances in understanding the role of the gut microbiome in building immunity and its involvement in pathogenesis suggests an important approach to managing and treating T1D. Diet and nutrition play an important role in the modulation of the gut microbiome, and it is now clear that dietary fibers and the introduction of pre and probiotics could constitute powerful tools to correct the dysbiosis found in T1D patients. Metabolites produced by beneficial microbes, such as the SCFA can affect the epigenome, along with the differentiation and functioning of various cell types, including enterocytes, immune cells and pancreatic cells (Figure 2). Despite the available evidence on the impact of dietary gut microbial metabolites on the epigenome of T1D and the existing of significant association between diet, gut microbiota and epigenetics of host cells, a better understanding of epigenetic mechanisms is still necessary for the identification of the epigenetic pathways involved in T1D. Finally, the modulation of the gut microbiome for treating T1D shows great promise; this explains the launch of clinical trials aiming at repairing dysbiosis, either by dietary intervention or fecal transplants (173, 174). Although, the results of these trials might play an important role in our understanding of the environmental factors involved in the pathogenesis of T1D (27, 175, 176), establishing and validating functional regimens, like probiotics and prebiotics, in long term studies is necessary.
Figure 2.
Schematic representations of prebiotic and probiotic actions in type 1 diabetes. Prebiotic and probiotic consumption increases the Gut microbiome diversity the Firmicutes/Bacteroidetes, the antibacterial activity, decreases the intestinal permeability and modulate the immune system. As results of increasing SCFAs production, mucin production, intestinal integrity and tight junction are increased, intestinal inflammation decreased. The NF-kB activation pathways are blocked, which lead to a reduction of insulitis, reduction in pancreatic β-cell destruction and therefore amelioration of T1D.
Furthermore, future studies should be better coordinated and well-characterized, with high quality and long-term sampling and data collection starting from pregnancy to the onset of T1D in high risk children. This may reveal the mechanisms by which diet and/or administration or pre/probiotics prevent and protect against T1D. Furthermore, we advocate for standardized and reproducible methods for DNA and RNA studies, followed by new approaches such as metagenomics, metaproteomic, and metabolomics applied to a large cohort of patients as well as intervention studies. This may, in the future, elevate our understanding of this topic and move this area of research from a description of effect, sometimes indirect, to translational applications.
Author Contributions
AC conceived the study, critically supervised the project, revised the text, wrote some parts of the review and prepared the tables and the figure. CM helped in editing the text and sketched the figure. GB helped in editing the text and gave support in the literature review and writing. AA, TA and AA-S were responsible for scientific writing of the first two parts of the draft manuscript. All authors contributed to the proofreading of the manuscript and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conductedin the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. The work had financial support from Weill Cornell Medicine Qatar through a Student Research mentorship Program: SRMP-003-04: Identification and characterization of biological properties of probiotic content of Qatar's dairy products.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2020.563605/full#supplementary-material
References
- 1.Pettitt DJ, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence JM, et al. Prevalence of diabetes in US Youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. (2014) 37:402–8. 10.2337/dc13-1838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katsarou A, Gudbjörnsdottir S, Rawshani A, Dabelea D, Bonifacio E, Anderson BJ, et al. Type 1 diabetes mellitus. Nat Rev Dis Prim. (2017) 3:17016. 10.1038/nrdp.2017.16 [DOI] [PubMed] [Google Scholar]
- 3.Gülden E, Wong FS, Wen L. The gut microbiota and type 1 diabetes. Clin Immunol. (2015) 159:143–53. 10.1016/j.clim.2015.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomes AC, Bueno AA, De Souza RGMH, Mota JF. Gut microbiota, probiotics and diabetes. Nutr J. (2014) 13:60. 10.1186/1475-2891-13-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atkinson MA. The pathogenesis and natural history of type 1 diabetes. Cold Spring Harb Perspect Med. (2012) 2:a007641. 10.1101/cshperspect.a007641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han H, Li Y, Fang J, Liu G, Yin J, Li T, et al. Gut microbiota and type 1 diabetes. Int J Mol Sci. (2018) 19:995. 10.3390/ijms19040995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pociot F, Lernmark Å. Genetic risk factors for type 1 diabetes. Lancet. (2016) 387:2331–9. 10.1016/S0140-6736(16)30582-7 [DOI] [PubMed] [Google Scholar]
- 8.Rewers M, Ludvigsson J. Environmental risk factors for type 1 diabetes. Lancet. (2016) 387:2340–8. 10.1016/S0140-6736(16)30507-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meng JM, Cao SY, Wei XL, Gan RY, Wang YF, Cai SX, et al. Effects and mechanisms of tea for the prevention and management of diabetes mellitus and diabetic complications: an updated review. Antioxidants. (2019) 8:170. 10.3390/antiox8060170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu L, Li Y, Dai Y, Peng J. Natural products for the treatment of type 2 diabetes mellitus: pharmacology and mechanisms. Pharmacol Res. (2018) 130:451–65. 10.1016/j.phrs.2018.01.015 [DOI] [PubMed] [Google Scholar]
- 11.Prabhakar PK, Doble M. Mechanism of action of natural products used in the treatment of diabetes mellitus. Chin J Integr Med. (2011) 17:563–74. 10.1007/s11655-011-0810-3 [DOI] [PubMed] [Google Scholar]
- 12.Hu X, Li S, Fu Y, Zhang N. Targeting gut microbiota as a possible therapy for mastitis. Eur J Clin Microbiol Infect Dis. (2019) 38:1409–23. 10.1007/s10096-019-03549-4 [DOI] [PubMed] [Google Scholar]
- 13.Hu Y, Peng J, Li F, Wong FS, Wen L. Evaluation of different mucosal microbiota leads to gut microbiota-based prediction of type 1 diabetes in NOD mice. Sci Rep. (2018) 8:15451. 10.1038/s41598-018-33571-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seganfredo FB, Blume CA, Moehlecke M, Giongo A, Casagrande DS, Spolidoro JVN, et al. Weight-loss interventions and gut microbiota changes in overweight and obese patients: a systematic review. Obes Rev. (2017) 18:832–51. 10.1111/obr.12541 [DOI] [PubMed] [Google Scholar]
- 15.Zhang YJ, Li S, Gan RY, Zhou T, Xu DP, Bin LH. Impacts of gut bacteria on human health and diseases. Int J Mol Sci. (2015) 16:7493–519. 10.3390/ijms16047493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meng X, Li S, Li Y, Gan RY, Bin LH. Gut microbiota's relationship with liver disease and role in hepatoprotection by dietary natural products and probiotics. Nutrients. (2018) 10:1457. 10.3390/nu10101457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang WHW, Kitai T, Hazen SL. Gut microbiota in cardiovascular health and disease. Circ Res. (2017) 120:1183–96. 10.1161/CIRCRESAHA.117.309715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X, Watanabe K, Kimura I. Gut microbiota dysbiosis drives and implies novel therapeutic strategies for diabetes mellitus and related metabolic diseases. Front Immunol. (2017) 8:1882. 10.3389/fimmu.2017.01882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scaldaferri F, Pizzoferrato M, Gerardi V, Lopetuso L, Gasbarrini A. The gut barrier: new acquisitions and therapeutic approaches. J Clin Gastroenterol. (2012) 46:S12–7. 10.1097/MCG.0b013e31826ae849 [DOI] [PubMed] [Google Scholar]
- 20.Sommer F, Bäckhed F. The gut microbiota–masters of host development and physiology. Nat Rev Microbiol. (2013) 11:227–38. 10.1038/nrmicro2974 [DOI] [PubMed] [Google Scholar]
- 21.Yang X, Xie L, Li Y, Wei C. More than 9,000,000 unique genes in human gut bacterial community: estimating gene numbers inside a human body. PLoS ONE. (2009) 4:9–10. 10.1371/journal.pone.0006074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zmora N, Suez J, Elinav E. You are what you eat: diet, health and the gut microbiota. Nat Rev Gastroenterol Hepatol. (2019) 16:35–56. 10.1038/s41575-018-0061-2 [DOI] [PubMed] [Google Scholar]
- 23.Esposito S, Toni G, Tascini G, Santi E, Berioli MG, Principi N. Environmental factors associated with type 1 diabetes. Front Endocrinol. (2019) 10:592. 10.3389/fendo.2019.00592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng P, Li Z, Zhou Z. Gut microbiome in type 1 diabetes: a comprehensive review. Diabetes Metab Res Rev. (2018) 34:e3043. 10.1002/dmrr.3043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hidalgo-Cantabrana C, Delgado S, Ruiz L, Ruas-Madiedo P, Sánchez B, Margolles A. Bifidobacteria and their health-promoting effects. Microbiol Spectr. (2017) 5 10.1128/9781555819705.ch3 [DOI] [PubMed] [Google Scholar]
- 26.Vatanen T, Franzosa EA, Schwager R, Tripathi S, Arthur TD, Vehik K, et al. The human gut microbiome in early-onset type 1 diabetes from the TEDDY study. Nature. (2018) 562:589–94. 10.1038/s41586-018-0620-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Durazzo M, Ferro A, Gruden G. Gastrointestinal microbiota and type 1 diabetes mellitus: the state of art. J Clin Med. (2019) 8:1843. 10.3390/jcm8111843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miro-Blanch J, Yanes O. Epigenetic regulation at the interplay between gut microbiota and host metabolism. Front Genet. (2019) 10:638. 10.3389/fgene.2019.00638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Z, Lu Q, Wang Z. Epigenetic alterations in cellular immunity: new insights into autoimmune diseases. Cell Physiol Biochem. (2017) 41:645–60. 10.1159/000457944 [DOI] [PubMed] [Google Scholar]
- 30.Wu H, Liao J, Li Q, Yang M, Zhao M, Lu Q. Epigenetics as biomarkers in autoimmune diseases. Clin Immunol. (2018) 196:34–9. 10.1016/j.clim.2018.03.011 [DOI] [PubMed] [Google Scholar]
- 31.Nyaga DM, Vickers MH, Jefferies C, Perry JK, O'Sullivan JM. The genetic architecture of type 1 diabetes mellitus. Mol Cell Endocrinol. (2018) 477:70–80. 10.1016/j.mce.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 32.Zullo A, Sommese L, Nicoletti G, Donatelli F, Mancini FP, Napoli C. Epigenetics and type 1 diabetes: mechanisms and translational applications. Transl Res. (2017) 185:85–93. 10.1016/j.trsl.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 33.Wang Z, Xie Z, Lu Q, Chang C, Zhou Z. Beyond genetics: what causes type 1 diabetes. Clin Rev Allergy Immunol. (2017) 52:273–86. 10.1007/s12016-016-8592-1 [DOI] [PubMed] [Google Scholar]
- 34.Xiang Z, Yang Y, Chang C, Lu Q. The epigenetic mechanism for discordance of autoimmunity in monozygotic twins. J Autoimmun. (2017) 83:43–50. 10.1016/j.jaut.2017.04.003 [DOI] [PubMed] [Google Scholar]
- 35.Stefan M, Zhang W, Concepcion E, Yi Z, Tomer Y. DNA methylation profiles in type 1 diabetes twins point to strong epigenetic effects on etiology. J Autoimmun. (2014) 50:33–7. 10.1016/j.jaut.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elboudwarej E, Cole M, Briggs FBS, Fouts A, Fain PR, Quach H, et al. Hypomethylation within gene promoter regions and type 1 diabetes in discordant monozygotic twins. J Autoimmun. (2016) 68:23–9. 10.1016/j.jaut.2015.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y, Zhao M, Hou C, Liang G, Yang L, Tan Y, et al. Abnormal DNA methylation in CD4+ T cells from people with latent autoimmune diabetes in adults. Diabetes Res Clin Pract. (2011) 94:242–8. 10.1016/j.diabres.2011.07.027 [DOI] [PubMed] [Google Scholar]
- 38.Redondo MJ, Steck AK, Pugliese A. Genetics of type 1 diabetes. Pediatr Diabetes. (2018) 19:346–53. 10.1111/pedi.12597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cerna M. Epigenetic regulation in etiology of type 1 diabetes mellitus. Int J Mol Sci. (2020) 21:36. 10.3390/ijms21010036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fradin D, Le Fur S, Mille C, Naoui N, Groves C, Zelenika D, et al. Association of the CpG methylation pattern of the proximal insulin gene promoter with type 1 diabetes. PLoS ONE. (2012) 7:e36278. 10.1371/journal.pone.0036278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rui J, Deng S, Lebastchi J, Clark PL, Usmani-Brown S, Herold KC. Methylation of insulin DNA in response to proinflammatory cytokines during the progression of autoimmune diabetes in NOD mice. Diabetologia. (2016) 59:1021–9. 10.1007/s00125-016-3897-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akirav EM, Lebastchi J, Galvan EM, Henegariu O, Akirav M, Ablamunits V, et al. Detection of β cell death in diabetes using differentially methylated circulating DNA. Proc Natl Acad Sci USA. (2011) 108:19018–23. 10.1073/pnas.1111008108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee HS, Hwang JS. Genetic aspects of type 1 diabetes. Ann Pediatr Endocrinol Metab. (2019) 24:143–8. 10.6065/apem.2019.24.3.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hullar MAJ, Fu BC. Diet, the gut microbiome, and epigenetics. Cancer J. (2014) 20:170–5. 10.1097/PPO.0000000000000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miao F, Smith DD, Zhang L, Min A, Feng W, Natarajan R. Lymphocytes from patients with type 1 diabetes display a distinct profile of chromatin histone H3 lysine 9 dimethylation an epigenetic study in diabetes. Diabetes. (2008) 57:3189–98. 10.2337/db08-0645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miao F, Chen Z, Zhang L, Liu Z, Wu X, Yuan YC, et al. Profiles of epigenetic histone post-translational modifications at type 1 diabetes susceptible genes. J Biol Chem. (2012) 287:16335–45. 10.1074/jbc.M111.330373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu XY, Xu JF. Reduced histone H3 acetylation in CD4+ T lymphocytes: potential mechanism of latent autoimmune diabetes in adults. Dis Markers. (2015) 2015:3–4. 10.1155/2015/285125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng Y, Wang Z, Zhou Z. MiRNAs: Novel regulators of autoimmunity-mediated pancreatic β-cell destruction in type 1 diabetes. Cell Mol Immunol. (2017) 14:488–96. 10.1038/cmi.2017.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garo LP, Murugaiyan G. Contribution of MicroRNAs to autoimmune diseases. Cell Mol Life Sci. (2016) 73:2041–51. 10.1007/s00018-016-2167-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roggli E, Britan A, Gattesco S, Lin-Marq N, Abderrahmani A, Meda P, et al. Involvement of microRNAs in the cytotoxic effects exerted by proinflammatory cytokines on pancreatic β-cells. Diabetes. (2010) 59:978–86. 10.2337/db09-0881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roggli E, Gattesco S, Caille D, Briet C, Boitard C, Meda P, et al. Changes in microRNA expression contribute to pancreatic β-cell dysfunction in prediabetic NOD mice. Diabetes. (2012) 61:1742–51. 10.2337/db11-1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hezova R, Slaby O, Faltejskova P, Mikulkova Z, Buresova I, Raja KRM, et al. microRNA-342, microRNA-191 and microRNA-510 are differentially expressed in T regulatory cells of type 1 diabetic patients. Cell Immunol. (2010) 260:70–4. 10.1016/j.cellimm.2009.10.012 [DOI] [PubMed] [Google Scholar]
- 53.Endesfelder D, Castell WZ, Ardissone A, Davis-Richardson AG, Achenbach P, Hagen M, et al. Compromised gut microbiota networks in children with anti-islet cell autoimmunity. Diabetes. (2014) 63:2006–14. 10.2337/db13-1676 [DOI] [PubMed] [Google Scholar]
- 54.Alenghat T, Artis D. Epigenomic regulation of host-microbiota interactions national center for biotechnology information. Trend Immunol. (2014) 35:518–25. 10.1016/j.it.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qin Y, Wade PA. Crosstalk between the microbiome and epigenome: messages from bugs. J Biochem. (2018) 163:105–12. 10.1093/jb/mvx080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gerhauser C. Impact of dietary gut microbial metabolites on the epigenome. Philos Trans R Soc B Biol Sci. (2018) 373:20170359. 10.1098/rstb.2017.0359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis-Richardson AG, Triplett EW. A model for the role of gut bacteria in the development of autoimmunity for type 1 diabetes. Diabetologia. (2015) 58:1386–93. 10.1007/s00125-015-3614-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan S, Jena GB. Protective role of sodium butyrate, a HDAC inhibitor on beta-cell proliferation, function and glucose homeostasis through modulation of p38/ERK MAPK and apoptotic pathways: study in juvenile diabetic rat. Chem Biol Interact. (2014) 213:1–12. 10.1016/j.cbi.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 59.Soliman ML, Puig KL, Combs CK, Rosenberger TA. Acetate reduces microglia inflammatory signaling in vitro. J Neurochem. (2012) 123:555–67. 10.1111/j.1471-4159.2012.07955.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. (2019) 17:181–92. 10.1038/s41579-018-0118-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim HJ, Bae SC. Histone deacetylase inhibitors: molecular mechanisms of action and clinical trials as anti-cancer drugs. Am J Transl Res. (2011) 3:166–79. [PMC free article] [PubMed] [Google Scholar]
- 62.Kibe R, Kurihara S, Sakai Y, Suzuki H, Ooga T, Sawaki E, et al. Upregulation of colonic luminal polyamines produced by intestinal microbiota delays senescence in mice. Sci Rep. (2014) 4:4548. 10.1038/srep04548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Greenblum S, Turnbaugh PJ, Borenstein E. Metagenomic systems biology of the human gut microbiome reveals topological shifts associated with obesity and inflammatory bowel disease. Proc Natl Acad Sci USA. (2012) 109:594–9. 10.1073/pnas.1116053109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dai Z, Zhang J, Wu Q, Chen J, Liu J, Wang L, et al. The role of microbiota in the development of colorectal cancer. Int J Cancer. (2019) 145:2032–41. 10.1002/ijc.32017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mariño E, Richards JL, McLeod KH, Stanley D, Yap YA, Knight J, et al. Gut microbial metabolites limit the frequency of autoimmune T cells and protect against type 1 diabetes. Nat Immunol. (2017) 18:552–62. 10.1038/ni.3713 [DOI] [PubMed] [Google Scholar]
- 66.Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol. (2009) 9:313–23. 10.1038/nri2515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Needell JC, Zipris D. The role of the intestinal microbiome in type 1 diabetes pathogenesis. Curr Diab Rep. (2016) 16:89. 10.1007/s11892-016-0781-z [DOI] [PubMed] [Google Scholar]
- 68.Wirth R, Bódi N, Maróti G, Bagyánszki M, Talapka P, Fekete É, et al. Regionally distinct alterations in the composition of the gut microbiota in rats with streptozotocin-induced diabetes. PLoS ONE. (2014) 9:e110440. 10.1371/journal.pone.0110440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Siljander HTA, Simell S, Hekkala A, Lähde J, Simell T, Vähäsalo P, et al. Predictive characteristics of diabetes-associated autoantibodies among children with HLA-conferred disease susceptibility in the general population. Diabetes. (2009) 58:2835–42. 10.2337/db08-1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brugman S, Klatter FA, Visser JTJ, Wildeboer-Veloo ACM, Harmsen HJM, Rozing J, et al. Antibiotic treatment partially protects against type 1 diabetes in the Bio-Breeding diabetes-prone rat. Is the gut flora involved in the development of type 1 diabetes? Diabetologia. (2006) 49:2105–8. 10.1007/s00125-006-0334-0 [DOI] [PubMed] [Google Scholar]
- 71.Roesch LF, Lorca GL, Casella G, Giongo A, Naranjo A, Pionzio AM, et al. Culture-independent identification of gut bacteria correlated with the onset of diabetes in a rat model. ISME J. (2009) 3:536–48. 10.1038/ismej.2009.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Davis-Richardson AG, Ardissone AN, Dias R, Simell V, Leonard MT, Kemppainen KM, et al. Bacteroides dorei dominates gut microbiome prior to autoimmunity in Finnish children at high risk for type 1 diabetes. Front Microbiol. (2014) 5:678. 10.3389/fmicb.2014.00678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murri M, Leiva I, Gomez-Zumaquero JM, Tinahones FJ, Cardona F, Soriguer F, et al. Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case-control study. BMC Med. (2013) 11:46. 10.1186/1741-7015-11-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Giongo A, Gano KA, Crabb DB, Mukherjee N, Novelo LL, Casella G, et al. Toward defining the autoimmune microbiome for type 1 diabetes. ISME J. (2011) 5:82–91. 10.1038/ismej.2010.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.de Goffau MC, Luopajärvi K, Knip M, Ilonen J, Ruohtula T, et al. Fecal microbiota composition differs between children with β-Cell autoimmunity and those without. Diabetes. (2013) 1328–44. 10.2337/db12-0526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Clausen TD, Bergholt T, Eriksson F, Rasmussen S, Keiding N, Løkkegaard EC. Prelabor cesarean section and risk of childhood type 1 diabetes: a nationwide register-based cohort study. Epidemiology. (2016) 27:547–55. 10.1097/EDE.0000000000000488 [DOI] [PubMed] [Google Scholar]
- 77.Azad MB, Konya T, Maughan H, Guttman DS, Field CJ, Chari RS, et al. Gut microbiota of healthy Canadian infants: profiles by mode of delivery and infant diet at 4 months. Cmaj. (2013) 185:385–94. 10.1503/cmaj.121189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bonifacio E, Warncke K, Winkler C, Wallner M, Ziegler AG. Cesarean section and interferon-induced helicase gene polymorphisms combine to increase childhood type 1 diabetes risk. Diabetes. (2011) 60:3300–6. 10.2337/db11-0729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guo S, Al-Sadi R, Said HM, Ma TY. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD14. Am J Pathol. (2013) 182:375–87. 10.1016/j.ajpath.2012.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bach Knudsen K, Lærke H, Hedemann M, Nielsen T, Ingerslev A, Gundelund Nielsen D, et al. Impact of diet-modulated butyrate production on intestinal barrier function and inflammation. Nutrients. (2018) 10:1499. 10.3390/nu10101499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mejía-León ME, Calderón de la Barca AM. Diet, microbiota and immune system in type 1 diabetes development and evolution. Nutrients. (2015) 7:9171–84. 10.3390/nu7115461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brown CT, Davis-Richardson AG, Giongo A, Gano KA, Crabb DB, Mukherjee N, et al. Gut microbiome metagenomics analysis suggests a functional model for the development of autoimmunity for type 1 diabetes. PLoS ONE. (2011) 6:e25792. 10.1371/journal.pone.0025792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Miranda MCG, Oliveira RP, Torres L, Aguiar SLF, Pinheiro-Rosa N, Lemos L, et al. Frontline science: abnormalities in the gut mucosa of non-obese diabetic mice precede the onset of type 1 diabetes. J Leukoc Biol. (2019) 106:513–29. 10.1002/JLB.3HI0119-024RR [DOI] [PubMed] [Google Scholar]
- 84.Caviglia GP, Rosso C, Ribaldone DG, Dughera F, Fagoonee S, Astegiano M, et al. Physiopathology of intestinal barrier and the role of zonulin. Minerva Biotecnol. (2019) 31:83–92. 10.23736/S1120-4826.19.02554-0 [DOI] [Google Scholar]
- 85.Neu J, Reverte CM, Mackey AD, Liboni K, Tuhacek-Tenace LM, Hatch M, et al. Changes in intestinal morphology and permeability in the biobreeding rat before the onset of type 1 diabetes. J Pediatr Gastroenterol Nutr. (2005) 40:589–95. 10.1097/01.MPG.0000159636.19346.C1 [DOI] [PubMed] [Google Scholar]
- 86.Vaarala O, Atkinson MA, Neu J. The “perfect storm” for type 1 diabetes: the complex interplay between intestinal microbiota, gut permeability, and mucosal immunity. Diabetes. (2008) 57:2555–62. 10.2337/db08-0331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Virtanen SM. Dietary factors in the development of type 1 diabetes. Pediatr Diabetes. (2016) 17:49–55. 10.1111/pedi.12341 [DOI] [PubMed] [Google Scholar]
- 88.Parikka V, Näntö-Salonen K, Saarinen M, Simell T, Ilonen J, Hyöty H, et al. Early seroconversion and rapidly increasing autoantibody concentrations predict prepubertal manifestation of type 1 diabetes in children at genetic risk. Diabetologia. (2012) 55:1926–36. 10.1007/s00125-012-2523-3 [DOI] [PubMed] [Google Scholar]
- 89.Niinistö S, Takkinen HM, Uusitalo L, Rautanen J, Vainio N, Ahonen S, et al. Maternal intake of fatty acids and their food sources during lactation and the risk of preclinical and clinical type 1 diabetes in the offspring. Acta Diabetol. (2015) 52:763–72. 10.1007/s00592-014-0673-0 [DOI] [PubMed] [Google Scholar]
- 90.Prodam F, Chiocchetti A, Dianzani U. Diet as a strategy for type 1 diabetes prevention. Cell Mol Immunol. (2018) 15:1–4. 10.1038/cmi.2017.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Comi C, Fleetwood T, Dianzani U. The role of T cell apoptosis in nervous system autoimmunity. Autoimmun Rev. (2012) 12:150–6. 10.1016/j.autrev.2011.08.011 [DOI] [PubMed] [Google Scholar]
- 92.Sun J, Furio L, Mecheri R, van der Does AM, Lundeberg E, Saveanu L, et al. Pancreatic β-cells limit autoimmune diabetes via an immunoregulatory antimicrobial peptide expressed under the influence of the gut microbiota. Immunity. (2015) 43:304–17. 10.1016/j.immuni.2015.07.013 [DOI] [PubMed] [Google Scholar]
- 93.Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Nature. (2012) 489:242–9. 10.1038/nature11552 [DOI] [PubMed] [Google Scholar]
- 94.Abdellatif AM, Sarvetnick NE. Current understanding of the role of gut dysbiosis in type 1 diabetes. J Diabetes. (2019) 11:632–44. 10.1111/1753-0407.12915 [DOI] [PubMed] [Google Scholar]
- 95.Mojibian M, Glavas MM, Kieffer TJ. Engineering the gut for insulin replacement to treat diabetes. J Diabetes Investig. (2016) 7:87–93. 10.1111/jdi.12479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Knip M, Virtanen SM, Becker D, Dupré J, Krischer JP, Åkerblom HK. Early feeding and risk of type 1 diabetes: experiences from the Trial to Reduce Insulin-dependent diabetes mellitus in the Genetically at Risk (TRIGR). Am J Clin Nutr. (2011) 94:20894. 10.3945/ajcn.110.000711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gutierrez-Achury J, Zhernakova A, Pulit SL, Trynka G, Hunt KA, Romanos J, et al. Fine mapping in the MHC region accounts for 18% additional genetic risk for celiac disease. Nat Genet. (2015) 47:577–8. 10.1038/ng.3268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Antvorskov JC, Josefsen K, Engkilde K, Funda DP, Buschard K. Dietary gluten and the development of type 1 diabetes. Diabetologia. (2014) 57:1770–80. 10.1007/s00125-014-3265-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cosnes J, Cellier C, Viola S, Colombel JF, Michaud L, Sarles J, et al. Incidence of autoimmune diseases in celiac disease: protective effect of the gluten-free diet. Clin Gastroenterol Hepatol. (2008) 6:753–8. 10.1016/j.cgh.2007.12.022 [DOI] [PubMed] [Google Scholar]
- 100.Marietta E V., Gomez AM, Yeoman C, Tilahun AY, Clark CR, Luckey DH, et al. Low incidence of spontaneous type 1 diabetes in non-obese diabetic mice raised on gluten-free diets is associated with changes in the intestinal microbiome. PLoS ONE. (2013) 8:19. 10.1371/journal.pone.0078687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tian Y, Nichols RG, Cai J, Patterson AD, Cantorna MT. Vitamin A deficiency in mice alters host and gut microbial metabolism leading to altered energy homeostasis. J Nutr Biochem. (2018) 54:28–34. 10.1016/j.jnutbio.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vahjen W, Pieper R, Zentek J. Increased dietary zinc oxide changes the bacterial core and enterobacterial composition in the ileum of piglets. J Anim Sci. (2011) 89:2430–9. 10.2527/jas.2010-3270 [DOI] [PubMed] [Google Scholar]
- 103.Xia T, Lai W, Han M, Han M, Ma X, Zhang L. Dietary ZnO nanoparticles alters intestinal microbiota and inflammation response in weaned piglets. Oncotarget. (2017) 8:64878–91. 10.18632/oncotarget.17612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fukuda S, Toh H, Hase K, Oshima K, Nakanishi Y, Yoshimura K, et al. Bifidobacteria can protect from enteropathogenic infection through production of acetate. Nature. (2011) 469:543–7. 10.1038/nature09646 [DOI] [PubMed] [Google Scholar]
- 105.Luu M, Visekruna A. Short-chain fatty acids: Bacterial messengers modulating the immunometabolism of T cells. Eur J Immunol. (2019) 49:842–8. 10.1002/eji.201848009 [DOI] [PubMed] [Google Scholar]
- 106.Tsai Y-L, Lin T-L, Chang C-J, Wu T-R, Lai W-F, Lu C-C, et al. Probiotics, prebiotics and amelioration of diseases. J Biomed Sci. (2019) 26:3. 10.1186/s12929-018-0493-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Reid D. Probiotics. (2005) 51:1455–7. 10.2174/1381612053382395 [DOI] [Google Scholar]
- 108.Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document: the international scientific association for probiotics and prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. (2014) 11:506–14. 10.1038/nrgastro.2014.66 [DOI] [PubMed] [Google Scholar]
- 109.Pandey KR, Naik SR, Vakil B V. Probiotics, prebiotics and synbiotics- a review. J Food Sci Technol. (2015) 52:7577–87. 10.1007/s13197-015-1921-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nagpal R, Kumar A, Kumar M, Behare P V., Jain S, Yadav H. Probiotics, their health benefits and applications for developing healthier foods: a review. FEMS Microbiol Lett. (2012) 334:1–15. 10.1111/j.1574-6968.2012.02593.x [DOI] [PubMed] [Google Scholar]
- 111.Moludi J, Maleki V, Jafari-Vayghyan H, Vaghef-Mehrabany E, Alizadeh M. Metabolic endotoxemia and cardiovascular disease: a systematic review about potential roles of prebiotics and probiotics. Clin Exp Pharmacol Physiol. (2020) 47:927–39. 10.1111/1440-1681.13250 [DOI] [PubMed] [Google Scholar]
- 112.Akbari V, Hendijani F. Effects of probiotic supplementation in patients with type 2 diabetes: systematic review and meta-analysis. Nutr Rev. (2016) 74:774–84. 10.1093/nutrit/nuw039 [DOI] [PubMed] [Google Scholar]
- 113.Kesika P, Sivamaruthi BS, Chaiyasut C. Do probiotics improve the health status of individuals with diabetes mellitus? A review on outcomes of clinical trials. Biomed Res Int. (2019) 2019:1–11. 10.1155/2019/1531567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lau K, Benitez P, Ardissone A, Wilson TD, Collins EL, Lorca G, et al. Inhibition of type 1 diabetes correlated to a Lactobacillus johnsonii N6.2-mediated Th17 bias. J Immunol. (2011) 186:3538–46. 10.4049/jimmunol.1001864 [DOI] [PubMed] [Google Scholar]
- 115.Calcinaro F, Dionisi S, Marinaro M, Candeloro P, Bonato V, Marzotti S, et al. Oral probiotic administration induces interleukin-10 production and prevents spontaneous autoimmune diabetes in the non-obese diabetic mouse. Diabetologia. (2005) 48:1565–75. 10.1007/s00125-005-1831-2 [DOI] [PubMed] [Google Scholar]
- 116.Valladares R, Sankar D, Li N, Williams E, Lai K-K, Abdelgeliel AS, et al. Lactobacillus johnsonii N6.2 mitigates the development of type 1 diabetes in BB-DP rats. PLoS ONE. (2010) 5:e10507. 10.1371/journal.pone.0010507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Takiishi T, Korf H, Van Belle TL, Robert S, Grieco FA, Caluwaerts S, et al. Reversal of autoimmune diabetes by restoration of antigen-specific tolerance using genetically modified Lactococcus lactis in mice. J Clin Invest. (2012) 122:1717–25. 10.1172/JCI60530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bejar W, Hamden K, Ben Salah R, Chouayekh H. Lactobacillus plantarum TN627 significantly reduces complications of alloxan-induced diabetes in rats. Anaerobe. (2013) 24:4–11. 10.1016/j.anaerobe.2013.08.006 [DOI] [PubMed] [Google Scholar]
- 119.Karumuthil-Melethil S, Sofi MH, Gudi R, Johnson BM, Perez N, Vasu C. TLR2- and Dectin 1-associated innate immune response modulates T-cell response to pancreatic β-cell antigen and prevents type 1 diabetes. Diabetes. (2015) 64:1341–57. 10.2337/db14-1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Le TKC, Hosaka T, Nguyen TT, Kassu A, Dang TO, Tran HB, et al. Bifidobacterium species lower serum glucose, increase expressions of insulin signaling proteins, and improve adipokine profile in diabetic mice. Biomed Res. (2015) 36:63–70. 10.2220/biomedres.36.63 [DOI] [PubMed] [Google Scholar]
- 121.Zhang J, Motyl KJ, Irwin R, MacDougald OA, Britton RA, McCabe LR. Loss of bone and Wnt10b expression in male type 1 diabetic mice is blocked by the probiotic Lactobacillus reuteri. Endocrinology. (2015) 156:3169–82. 10.1210/EN.2015-1308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wei S-H, Chen Y-P, Chen M-J. Selecting probiotics with the abilities of enhancing GLP-1 to mitigate the progression of type 1 diabetes in vitro and in vivo. J Funct Foods. (2015) 18:473–86. 10.1016/j.jff.2015.08.016 [DOI] [Google Scholar]
- 123.Dolpady J, Sorini C, Di Pietro C, Cosorich I, Ferrarese R, Saita D, et al. Oral probiotic VSL#3 prevents autoimmune diabetes by modulating microbiota and promoting Indoleamine 2,3-dioxygenase-enriched tolerogenic intestinal environment. J Diabetes Res. (2016) 2016:7569431. 10.1155/2016/7569431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Abdelazez A, Abdelmotaal H, Evivie SE, Melak S, Jia F-F, Khoso MH, et al. Screening potential probiotic characteristics of lactobacillus brevis strains in vitro and intervention effect on type i diabetes in vivo. Biomed Res Int. (2018) 2018:7356173. 10.1155/2018/7356173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yadav R, Dey DK, Vij R, Meena S, Kapila R, Kapila S. Evaluation of anti-diabetic attributes of Lactobacillus rhamnosus MTCC: 5957, Lactobacillus rhamnosus MTCC: 5897 and Lactobacillus fermentum MTCC: 5898 in streptozotocin induced diabetic rats. Microb Pathog. (2018) 125:454–62. 10.1016/j.micpath.2018.10.015 [DOI] [PubMed] [Google Scholar]
- 126.Marcial GE, Ford AL, Haller MJ, Gezan SA, Harrison NA, Cai D, et al. Lactobacillus johnsonii N6.2 modulates the host immune responses: a double-blind, randomized trial in healthy adults. Front Immunol. (2017) 8:655. 10.3389/fimmu.2017.00655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Groele L, Szajewska H, Szypowska A. Effects of Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb12 on beta-cell function in children with newly diagnosed type 1 diabetes: protocol of a randomised controlled trial. BMJ Open. (2017) 7:e017178. 10.1136/bmjopen-2017-017178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ahola AJ, Harjutsalo V, Forsblom C, Freese R, Mäkimattila S, Groop H. The self-reported use of probiotics is associated with better glycaemic control and lower odds of metabolic syndrome and its components in type 1 diabetes. J Probiot Health. (2017) 5:4 10.4172/2329-8901.1000188 [DOI] [Google Scholar]
- 129.de Oliveira GLV, Leite AZ, Higuchi BS, Gonzaga MI, Mariano VS. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology. (2017) 152:1–12. 10.1111/imm.12765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nagpal R, Wang S, Ahmadi S, Hayes J, Gagliano J, Subashchandrabose S, et al. Human-origin probiotic cocktail increases short-chain fatty acid production via modulation of mice and human gut microbiome. Sci Rep. (2018) 8:12649. 10.1038/s41598-018-30114-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chung SJ, Armasu SM, Biernacka JM, Lesnick TG, Rider DN, Cunningham JM, et al. Association of early exposure of probiotics and islet autoimmunity in the TEDDY study ulla. JAMA Pediatr. (2016) 170:20–8. 10.1001/jamapediatrics.2015.2757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Burrows MP, Volchkov P, Kobayashi KS, Chervonsky A V., Medzhitov R. Microbiota regulates type 1 diabetes through toll-like receptors. Proc Natl Acad Sci USA. (2015) 112:9973–7. 10.1073/pnas.1508740112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Yadav H, Lee JH, Lloyd J, Walter P, Rane SG. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J Biol Chem. (2013) 288:25088–97. 10.1074/jbc.M113.452516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ho J, Reimer RA, Doulla M, Huang C. Effect of prebiotic intake on gut microbiota, intestinal permeability and glycemic control in children with type 1 diabetes: study protocol for a randomized controlled trial. Trials. (2016) 17:347. 10.1186/s13063-016-1486-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Biester T, Aschemeier B, Fath M, Frey M, Scheerer MF, Kordonouri O, et al. Effects of dapagliflozin on insulin-requirement, glucose excretion and ß-hydroxybutyrate levels are not related to baseline HbA1c in youth with type 1 diabetes. Diabetes Obes Metab. (2017) 19:1635–9. 10.1111/dom.12975 [DOI] [PubMed] [Google Scholar]
- 136.Beretta MV, Bernaud FR, Nascimento C, Steemburgo T, Rodrigues TC. Higher fiber intake is associated with lower blood pressure levels in patients with type 1 diabetes. Arch Endocrinol Metab. (2018) 62:47–54. 10.20945/2359-3997000000008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Markowiak P, Slizewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. (2017) 9:1021. 10.3390/nu9091021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Mishra SP, Wang S, Nagpal R, Miller B, Singh R, Taraphder S, et al. Probiotics and prebiotics for the amelioration of type 1 diabetes: present and future perspectives. Microorganisms. (2019) 7:67. 10.3390/microorganisms7030067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, et al. Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. (2017) 14:491–502. 10.1038/nrgastro.2017.75 [DOI] [PubMed] [Google Scholar]
- 140.Roberfroid M. Prebiotics: the concept revisited. J Nutr. (2007) 137(3 Suppl. 2):830S-7S. 10.1093/jn/137.3.830S [DOI] [PubMed] [Google Scholar]
- 141.Hinz SWA, van den Broek LAM, Beldman G, Vincken J-P, Voragen AGJ. β-Galactosidase from Bifidobacterium adolescentis DSM20083 prefers β(1,4)-galactosides over lactose. Appl Microbiol Biotechnol. (2004) 66:276–84. 10.1007/s00253-004-1745-9 [DOI] [PubMed] [Google Scholar]
- 142.Depeint F, Tzortzis G, Vulevic J, I'Anson K, Gibson GR. Prebiotic evaluation of a novel galactooligosaccharide mixture produced by the enzymatic activity of Bifidobacterium bifidum NCIMB 41171, in healthy humans: a randomized, double-blind, crossover, placebo-controlled intervention study. Am J Clin Nutr. (2008) 87:785–91. 10.1093/ajcn/87.3.785 [DOI] [PubMed] [Google Scholar]
- 143.Kolida S, Meyer D, Gibson GR. A double-blind placebo-controlled study to establish the bifidogenic dose of inulin in healthy humans. Eur J Clin Nutr. (2007) 61:1189–95. 10.1038/sj.ejcn.1602636 [DOI] [PubMed] [Google Scholar]
- 144.Vulevic J, Rastall RA, Gibson GR. Developing a quantitative approach for determining the in vitro prebiotic potential of dietary oligosaccharides. FEMS Microbiol Lett. (2004) 236:153–9. 10.1111/j.1574-6968.2004.tb09641.x [DOI] [PubMed] [Google Scholar]
- 145.Tzortzis G, Vulevic J. Galacto-Oligosaccharide prebiotics. In: Charalampopoulos D, Rastall R. A. Editors. Prebiotics and Probiotics Science and Technology. New York, NY: Springer New York; (2009) p. 207–44. [Google Scholar]
- 146.Roberfroid M, Gibson GR, Hoyles L, McCartney AL, Rastall R, Rowland I, et al. Prebiotic effects: metabolic and health benefits. Br J Nutr. (2010) 104:S1–63. 10.1017/S0007114510003363 [DOI] [PubMed] [Google Scholar]
- 147.Wilson B, Whelan K. Prebiotic inulin-type fructans and galacto-oligosaccharides: definition, specificity, function, and application in gastrointestinal disorders. J Gastroenterol Hepatol. (2017) 32:64–8. 10.1111/jgh.13700 [DOI] [PubMed] [Google Scholar]
- 148.Yoo J, Kim S. Probiotics and prebiotics: present status and future perspectives on metabolic disorders. Nutrients. (2016) 8:173. 10.3390/nu8030173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sonnenburg ED, Zheng H, Joglekar P, Higginbottom SK, Firbank SJ, Bolam DN, et al. Specificity of polysaccharide use in intestinal bacteroides species determines diet-induced microbiota alterations. Cell. (2010) 141:1241–52. 10.1016/j.cell.2010.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Crookshank JA, Patrick C, Wang G-S, Ariana Noel J, Scott FW. Gut immune deficits in LEW.1AR1- iddm rats partially overcome by feeding a diabetes-protective diet. Immunology. (2015) 145:417–28. 10.1111/imm.12457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Koh GY, Rowling MJ, Schalinske KL, Grapentine K, Loo YT. Consumption of dietary resistant starch partially corrected the growth pattern despite hyperglycemia and compromised kidney function in streptozotocin-induced diabetic rats. J Agric Food Chem. (2016) 64:7540–5. 10.1021/acs.jafc.6b03808 [DOI] [PubMed] [Google Scholar]
- 152.Chen K, Chen H, Faas MM, de Haan BJ, Li J, Xiao P, et al. Specific inulin-type fructan fibers protect against autoimmune diabetes by modulating gut immunity, barrier function, and microbiota homeostasis. Mol Nutr Food Res. (2017) 61:1601006. 10.1002/mnfr.201601006 [DOI] [PubMed] [Google Scholar]
- 153.Gorelick J, Yarmolinsky L, Budovsky A, Khalfin B, Klein J, Pinchasov Y, et al. The impact of diet wheat source on the onset of type 1 diabetes mellitus—lessons learned from the Non-Obese Diabetic (NOD) mouse model. Nutrients. (2017) 9:482. 10.3390/nu9050482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Prud'homme GJ, Glinka Y, Kurt M, Liu W, Wang Q. The anti-aging protein Klotho is induced by GABA therapy and exerts protective and stimulatory effects on pancreatic beta cells. Biochem Biophys Res Commun. (2017) 493:1542–7. 10.1016/j.bbrc.2017.10.029 [DOI] [PubMed] [Google Scholar]
- 155.Raafat K, Wurglics M, Schubert-Zsilavecz M. Prunella vulgaris L. active components and their hypoglycemic and antinociceptive effects in alloxan-induced diabetic mice. Biomed Pharmacother. (2016) 84:1008–18. 10.1016/j.biopha.2016.09.095 [DOI] [PubMed] [Google Scholar]
- 156.Xiao L, van't Land B, Engen PA, Naqib A, Green SJ, Nato A, et al. Human milk oligosaccharides protect against the development of autoimmune diabetes in NOD-mice. Sci Rep. (2018) 8:3829. 10.1038/s41598-018-22052-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bernaud FSR, Beretta M, do Nascimento C, Escobar F, Gross JL, Azevedo MJ, et al. Fiber intake and inflammation in type 1 diabetes. Diabetol Metab Syndr. (2014) 6:66. 10.1186/1758-5996-6-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.de Groot PF, Nikolic T, Imangaliyev S, Bekkering S, Duinkerken G, Keij FM, et al. Oral butyrate does not affect innate immunity and islet autoimmunity in individuals with longstanding type 1 diabetes: a randomised controlled trial. Diabetologia. (2020) 63:597–10. 10.1007/s00125-019-05073-8 [DOI] [PubMed] [Google Scholar]
- 159.Stenman LK, Waget A, Garret C, Briand F, Burcelin R, Sulpice T, et al. Probiotic B420 and prebiotic polydextrose improve efficacy of antidiabetic drugs in mice. Diabetol Metab Syndr. (2015) 7:75. 10.1186/s13098-015-0075-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Rammohan A, Sathyanesan J, Rajendran K, Pitchaimuthu A, Perumal SK, Balaraman K, et al. Synbiotics in surgery for chronic pancreatitis. Ann Surg. (2015) 262:31–7. 10.1097/SLA.0000000000001077 [DOI] [PubMed] [Google Scholar]
- 161.Waitzberg DL, Logullo LC, Bittencourt AF, Torrinhas RS, Shiroma GM, Paulino NP, et al. Effect of synbiotic in constipated adult women – A randomized, double-blind, placebo-controlled study of clinical response. Clin Nutr. (2013) 32:27–33. 10.1016/j.clnu.2012.08.010 [DOI] [PubMed] [Google Scholar]
- 162.Fujimori S, Gudis K, Mitsui K, Seo T, Yonezawa M, Tanaka S, et al. A randomized controlled trial on the efficacy of synbiotic versus probiotic or prebiotic treatment to improve the quality of life in patients with ulcerative colitis. Nutrition. (2009) 25:520–5. 10.1016/j.nut.2008.11.017 [DOI] [PubMed] [Google Scholar]
- 163.Asemi Z, Khorrami-Rad A, Alizadeh S-A, Shakeri H, Esmaillzadeh A. Effects of synbiotic food consumption on metabolic status of diabetic patients: a double-blind randomized cross-over controlled clinical trial. Clin Nutr. (2014) 33:198–203. 10.1016/j.clnu.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 164.Steed H, Macfarlane GT, Blackett KL, Bahrami B, Reynolds N, Walsh S V., et al. Clinical trial: the microbiological and immunological effects of synbiotic consumption - a randomized double-blind placebo-controlled study in active Crohn's disease. Aliment Pharmacol Ther. (2010) 32:872–83. 10.1111/j.1365-2036.2010.04417.x [DOI] [PubMed] [Google Scholar]
- 165.Rogha M, Esfahani MZ, Zargarzadeh AH. The efficacy of a synbiotic containing Bacillus Coagulans in treatment of irritable bowel syndrome: a randomized placebo-controlled trial. Gastroenterol Hepatol Ben Bench. (2014) 7:156–63. [PMC free article] [PubMed] [Google Scholar]
- 166.Islek A, Sayar E, Yilmaz A, Ozhak Baysan B, Mutlu D, Artan R. The role of Bifidobacterium lactis B94 plus inulin in the treatment of acute infectious diarrhea in children. Turkish J Gastroenterol. (2015) 25:628–33. 10.5152/tjg.2014.14022 [DOI] [PubMed] [Google Scholar]
- 167.Cheng CW, Villani V, Buono R, Wei M, Kumar S, Yilmaz OH, et al. Fasting-mimicking diet promotes Ngn3-driven β-cell regeneration to reverse diabetes. Cell. (2017) 168:775–88.e12. 10.1016/j.cell.2017.01.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Siljander H, Honkanen J, Knip M. Microbiome and type 1 diabetes. EBioMedicine. (2019) 46:512–21. 10.1016/j.ebiom.2019.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Boyle RJ, Robins-Browne RM, Tang ML. Probiotic use in clinical practice: what are the risks? Am J Clin Nutr. (2006) 83:1256–64. 10.1093/ajcn/83.6.1256 [DOI] [PubMed] [Google Scholar]
- 170.Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Therap Adv Gastroenterol. (2013) 6:39–51. 10.1177/1756283X12459294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Doron S, Snydman DR. Risk and safety of probiotics. Clin Infect Dis. (2015) 60(Suppl. 2):S129–34. 10.1093/cid/civ085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Cadario F, Savastio S, Ricotti R, Rizzo AM, Carrera D, Maiuri L, et al. Administration of Vitamin D and high dose of omega 3 to sustain remission of type 1 diabetes. Eur Rev Med Pharmacol Sci. (2018) 22:512–5. 10.26355/eurrev_201801_14203 [DOI] [PubMed] [Google Scholar]
- 173.Search of: Diabetes | Fecal Transplant - List Results - ClinicalTrials.gov. Available online at: https://clinicaltrials.gov/ct2/results?cond=fecal+transplant&term=diabetes&cntry=&state=&city=&dist (accessed April 25, 2020)
- 174.Search of: diet probiotic | Diabetes - List Results - ClinicalTrials.gov. Available online at: https://clinicaltrials.gov/ct2/results?cond=Diabetes&term=diet%2C+probiotic&cntry=&state=&city=&dis (accessed April 25, 2020)
- 175.Chen Z, Guo L, Zhang Y, Walzem RL, Pendergast JS, Printz RL, et al. Incorporation of therapeutically modified bacteria into Gut microbiota inhibits obesity. J Clin Invest. (2014) 124:3391–406. 10.1172/JCI72517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Kootte RS, Vrieze A, Holleman F, Dallinga-Thie GM, Zoetendal EG, de Vos WM, et al. The therapeutic potential of manipulating gut microbiota in obesity and type 2 diabetes mellitus. Diabetes Obes Metab. (2012) 14:112–20. 10.1111/j.1463-1326.2011.01483.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.