Abstract
Background:
Although oxygen is one of the oldest drugs available, it is still one of the most inappropriately administered drugs leading to over utilization of this very expensive resource.
Materials and Methods:
This prospective observational study was done in a large emergency department (ED) in India. The pattern of oxygen usage was studied before and after the strict implementation of an oxygen treatment algorithm. The algorithm was taught to all doctors and nurses and its implementation was monitored regularly. The main outcome measures were proportion of patients receiving oxygen therapy, inappropriate usage, and avoidable direct medical cost to the patient.
Results:
The 3-week pre-protocol observation phase in April 2016 included 3769 patients and the 3-week post-protocol observation phase in April 2017 included 4608 patients. The baseline demographic pattern was similar in both the pre-protocol and post-protocol groups. After the strict implementation of the algorithm, the number of patients receiving oxygen therapy decreased from 9.63% to 4.82%, a relative decrease of 51.4%. The average amount of total oxygen used decreased from 55.4 liters per person in pre-protocol group to 42.1 liters per person in the post-protocol group with a mean difference of 13.28 (95% CI 5.30-21.26; P = 0.001). Inappropriate oxygen usage decreased from 37.2% to 8.6%. There was a significant decrease in inappropriate oxygen use for indications like low sensorium (60.8% vs 21.7%) and trauma (88.5% vs 15.8%). The mortality rate in the pre-protocol phase was 2.7% as compared with 3.2% in the post-protocol phase. The total duration of inappropriate oxygen usage significantly decreased from 987 h to 89 h over the 21-day study period.
Conclusion:
The implementation of an oxygen therapy algorithm significantly reduces inappropriate oxygen use and decreases treatment cost to the patient with no additional mortality risk.
KEY WORDS: emergency department, inappropriate use, overuse, oxygen, oxygen therapy
Introduction
Oxygen is one of the oldest drugs available to mankind. However, it is also one of the most inappropriately administered drugs.[1,2,3] It is a very commonly used therapeutic agent and is used in the treatment of hypoxaemia. Oxygen, like any other drugs, should only be administered when indicated, and at the appropriate dose, as its unmonitored and unrestricted use can be potentially harmful to patients.[4,5,6] Definite treatment guidelines have been laid down by the British Thoracic Society (BTS), 2008 which recommends the use of O2 as a drug in that it had to be specifically prescribed and continuously monitored.[7,8,9] According to these guidelines, supplemental oxygen is indicated if oxygen saturation is <94%, or <88% in COPD patients. The literature to date is sufficiently convincing to recommend caution in administering supplemental oxygen. Excess of oxygen therapy might lead to physical, cytotoxic and functional risks, and the harmful effects of excessive oxygen therapy have been clearly described in case of COPD, obesity hyperventilation syndrome and myocardial infarction in the literature.[4,5,6,10] High oxygen therapy has been shown to adversely impact the surfactant on the pulmonary alveoli, thereby destabilizing the alveolar surface, resulting in atelectasis.[11,12] Oxygen therapy, dry and cold has the potential risk of drying up secretions and damaging the airway mucosal membranes, thereby accentuating sensation of dryness and discomfort to patients. This too favors development of atelectasis. Even in the surgical anaesthesia setting, administration of high concentration of oxygen is shown to induce reabsorption atelectasis.[13,14,15] It is important that the administered oxygen that reaches the trachea should be at physiologic conditions (32-34°C and 100% relative humidity).[16] The cause for development of pneumonia or atelectasis as a side effect of oxygen therapy is multifactorial. Severe hypoxemia should be treated promptly but slowly with stepwise increases in oxygen concentration, avoiding arterial hyperoxemia. It appears reasonable to aim at a peripheral oxygen saturation of 94-98%, particularly if the clinical condition of the patient is stable at that point.
Despite this, there has been unrestricted use of O2 therapy over the past few years, and it is still controversial.[11] In most hospitals, and particularly in the ED, specific treatment guidelines for the therapeutic use of O2 are not followed. The lack of strict adherence in most places is probably due to an over cautious approach to prevent hypoxia. We conducted this prospective observational study to document the current usage of oxygen therapy, its appropriateness and the decrease in inappropriate oxygen usage after implementing a standard algorithm.
Materials and Methods
We conducted this prospective observational study which included a pre-protocol phase and a post protocol phase. This study was done in the ED of Christian Medical College, Vellore which is a 2,700-bed tertiary care teaching hospital in South India. The adult ED has 49 beds with 75,000 admissions yearly, on an average, 200-220 per day. Our ED has 40 registrars, 7 consultants and 75 nurses, aged between 30 and 50 years. The doctors have an equal sex distribution and the nurses were predominantly of the female sex. All patients who were administered humidified oxygen therapy by the ED team during the study period were included in the study. Patients admitted in the ED but not administered oxygen was excluded. The decision to administer oxygen was purely the discretion of the ED team and was not influenced by the investigating team.
During the pre-protocol period of 21 days (April 1-21, 2016) the usage of oxygen, the perceived indication by the ED team, duration of therapy, appropriateness and cost incurred by the patient (cost of oxygen therapy, oxygen mask, monitoring charges) were documented by the primary investigators. The ED physicians and nurses were not aware of the audit being done. After this, an Oxygen treatment algorithm [Figure 1] was introduced and the ED team was educated every month for a year. The algorithm was reiterated to the ED team every month through monthly academic sessions. Specific training was given to the ED physicians and nursing staff, to use the algorithm as a basis for independently deciding when to administer O2 therapy. All staffs were given pocket cards of the algorithm, which were also posted in all treatment stations. Adherence to the protocol was monitored daily by the ED consultants on the floor. Following this, a post-protocol survey was done from April 1-21, 2017 documenting the same parameters. The results of the 2 surveys were compared and analyzed. The primary outcome was decrease in the percentage of oxygen administration during the post-protocol phase. Secondary outcomes included appropriateness of administration of oxygen and duration of oxygen therapy in both the periods of oxygen. Any adverse effects before and after implementation of the protocol and the ED mortality rate were documented. On the basis of a previous study by Sieber et al., to achieve a target decrease in oxygen usage by 3% (15-12%) the sample size was calculated.[17] On the basis of a P value of less than 0.05 and a power of 0.8, and using a 2-proportion hypothesis testing, a sample size of 2036 patients presenting to the ED were needed in the pre-protocol and post-protocol groups to detect a statistically significant reduction in the proportion of patients receiving O2 therapy from 15 to 12%.
Figure 1.
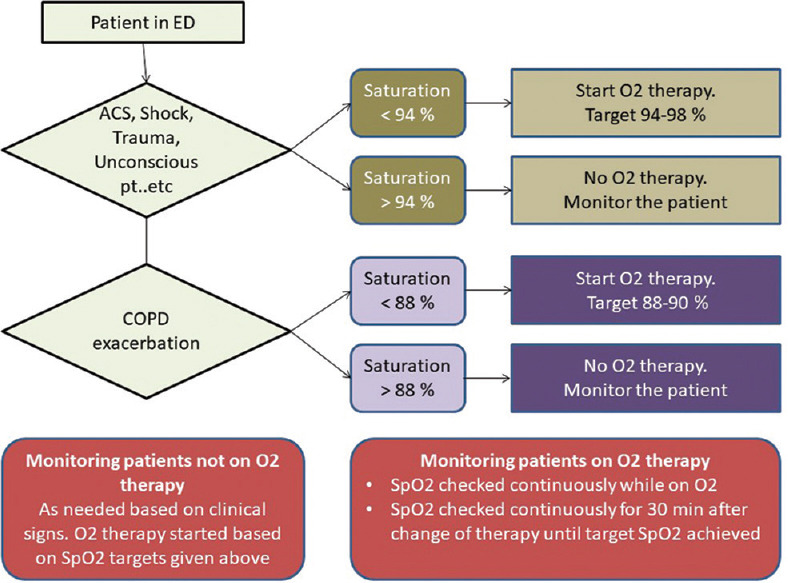
Oxygen therapy algorithm
Statistical analysis
The data was entered into a pre-designed clinical research proforma, and then analyzed using Statistical Package for Social Sciences software for Windows (SPSS Inc. Released 2007, version 16.0. Chicago). For comparison between the groups, the continuous variables are presented as mean (standard deviation) or as median (range) depending upon the distribution of the data. Categorical and nominal variables are presented as percentages.
Ethical consideration
Patient confidentiality was maintained using identifiers, and a password-protected access to the data for a limited number of individuals was maintained to ensure protection of privacy. This study was approved by the Institutional Review Board and ethics committee (IRB Min. No. 10236 dated 24.08.2016) and waiver of consent from the patients was obtained from the IRB.
Results
During the 3-week pre-protocol period, 3769 patients presented to the ED, whereas 4608 patients presented during the post-protocol period. The baseline characteristics including triage priority and additional ventilator supports in the ED in the pre and post protocol periods are shown in Table 1.
Table 1.
Demographic details of the study population in pre and post protocol periods
| Pre-protocol period | Post-protocol period | |
|---|---|---|
| Number of patients presenting to the ED | 3769 | 4608 |
| Number of patients administered oxygen | 363 (9.6%) | 222 (4.8%) |
| Gender | ||
| Male | 241 (66.4%) | 141 (63.5%) |
| Female | 122 (33.6%) | 81 (36.5%) |
| Mean age in years (SD) | 50.2 (17) | 54.6 (17.5) |
| Triage | ||
| Priority 1 | 244 (67.2%) | 155 (69.8%) |
| Priority 2 | 119 (32.8%) | 67 (30.2%) |
| Additional intervention | ||
| Non-invasive ventilation | 67 (18.5%) | 43 (19.4%) |
| Invasive ventilation | 66 (18.2%) | 38 (17.1%) |
In the pre-protocol period, 9.63% (363/3769) of patients were administered oxygen by the ED team which significantly decreased to 4.82% (222/4608) (P < 0.001) after implementation of the oxygen therapy algorithm, a relative decrease of 51.4%. The average amount of total oxygen used decreased from 55.4 liters per person in pre-protocol group to 42.1 liters per person in the post-protocol group with a mean difference of 13.28 (95% CI 5.30-21.26) with a significant P value of 0.001.
Reason for initiation of oxygen therapy in both the pre-protocol and post-protocol periods is shown in Table 2. Common reasons included breathlessness, low sensorium, polytrauma with low sensorium/facial trauma and for invasive ventilation.
Table 2.
Common reasons for initiation of oxygen therapy in pre- and post-protocol periods by the ED team
| Reasons for initiation of oxygen therapy | Pre-protocol period n=363 | Post-protocol period n=222 |
|---|---|---|
| Breathlessness | 206 (56.7%) | 128 (57.6%) |
| Low sensorium | 51 (14%) | 23 (10.3%) |
| Invasive ventilation | 40 (11%) | 12 (5.4%) |
| Poly trauma | 26 (7.1%) | 19 (8.5%) |
| Others | 23 (6.3%) | 29 (13.0%) |
| Chest pain | 2 (0.5%) | 8 (0.9%) |
| Seizures | 16 (4.4%) | 3 (1.3%) |
Appropriateness for initiation of oxygen therapy was determined by independent review of the charts by 2 ED consultants in both the periods. Oxygen therapy initiated for hypoxia or for ventilator support was considered to be appropriate. It was found that oxygen was inappropriately administered in 37.2% of patients in the pre-protocol period and this significantly decreased to 8.6% after implementation of the oxygen therapy algorithm [Figure 2]. The reasons for which a significant decrease in inappropriate use was noted between the 2 periods were breathlessness (23.8% vs 4.1%), low sensorium (60.8% vs 21.7%), seizures (87.5% vs 33.3%) and polytrauma (88.5% vs 15.8%) [Figure 3]. We calculated the duration of oxygen therapy that was administered inappropriately. In the 3-week period, oxygen was administered without a correct indication for 987 hours in the pre-protocol period and the misuse decreased significantly by 91% to 89 hours in the post-protocol period.
Figure 2.
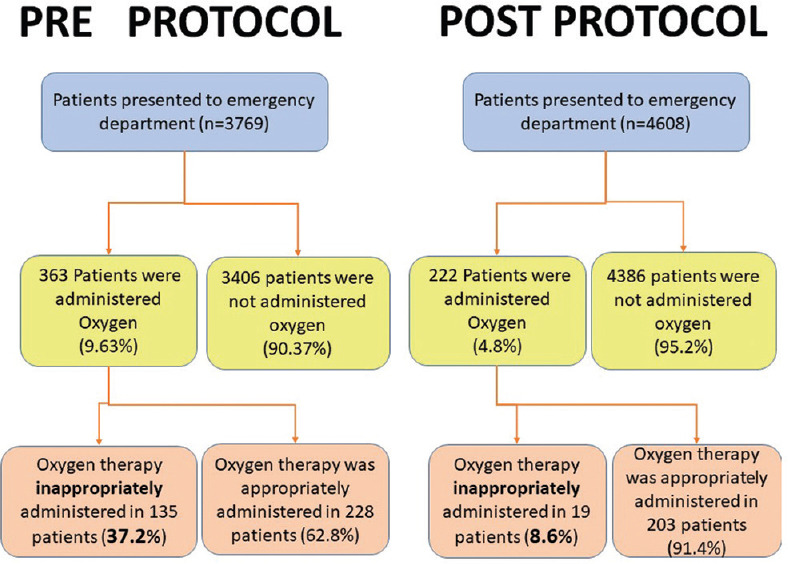
Oxygen administration and inappropriate use in pre and post protocol periods
Figure 3.
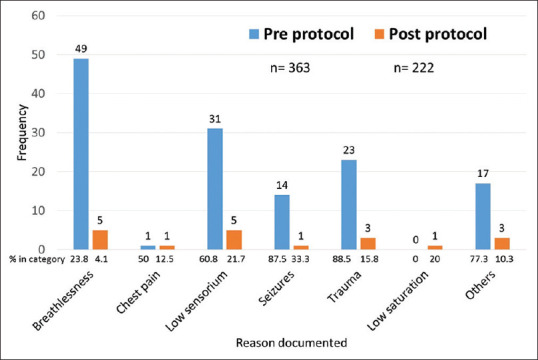
Documented reason for initiation of oxygen therapy when not indicated in the pre and post protocol periods
In the pre-protocol period, two thirds (65.3%) required hospital admission, 20.1% were discharged stable from the ED and 11.8% left against medical advice. More than half (56.1%) of the patients who were discharged stable from ED did not actually require oxygen therapy. ED mortality rate was 2.7% and an additional 11.8% died during hospitalization [Table 3].
Table 3.
ED outcome and hospital outcome of patients in the pre-protocol and post protocol periods
| Pre-protocol period | Post-protocol period | |
|---|---|---|
| ED outcome | n=363 | n=222 |
| Admitted in the hospital | 237 (65.3%) | 132 (59.5%) |
| Discharged stable from ED | 73 (20.1%) | 36 (16.2%) |
| Died in ED | 10 (2.7%) | 7 (3.2%) |
| Left against medical advice | 43 (11.8%) | 47 (21.2%) |
| Hospital outcome | n=237 | n=128 |
| Discharged stable | 199 (83.9%) | 103 (80.4%) |
| Died in the hospital | 38 (17.7%) | 25 (19.5%) |
In the post-protocol period, two thirds (59.5%) required hospital admission, 16.2% were discharged stable from the ED and 21.2% left against medical advice. Less than a quarter (22.3%) of the patients who were discharged stable from ED did not actually require oxygen therapy. ED mortality rate was 3.2% and an additional 19.5% died during hospitalization.
Discussion
Our study clearly showed the pattern of oxygen use in the ED, it's over use and the impact of a therapy algorithm on the reduction of its misuse. In the pre-protocol period, there was a significant over use of oxygen administration by the ED team. This is consistent with many studies done across the world.[1,2,4,10] Although hypoxia is should be the predominant indication for initiation of oxygen therapy, most physicians and nurses often administer oxygen with out any clinical or physiological indications for conditions like chest discomfort, low sensorium or for polytrauma with the hope that it would prevent hypoxic episodes. This over cautious approach may be considered practical in busy ED and critical care areas with minimal resources for frequent monitoring of patients, though it does not justify the potential harm due to oxygen therapy itself.
Studies and audits in the past have shown poor documentation on oxygen administration in busy and overcrowded places like the ED.[2] Although oxygen saturation is measured and documented, seldom is documented whether the patient is on oxygen or not at that time. This was reflected in a study by Asciak et al. who found that documentation of oxygen administration at the ED was only present in 23.5% cases and formal instructions on oxygen use were documented in 85.9% and that only half had details.[18] Therefore, to overcome this, we determined our findings by direct observation of patient care by the primary investigation team and hence were able to get information on factors like the duration and appropriateness of oxygen therapy. This is a significant strength of our study.
Studies from Australia and Switzerland showed that 11-15% of patients presenting with emergencies were administered Oxygen in the ED.[11,19] At 9.63%, the proportion of patients administered oxygen during the pre-protocol period in our ED was a welcome surprise. However, no such data is available from other ED s of India for comparison. The 50% reduction in oxygen administration to 4.82 in the post-protocol period was a significant result of our study. This result can solely be attributed to the introduction of the Oxygen therapy algorithm and the rigorous education and training given to the ED physicians and nurses for a full 12-month period.
A similar study on the effectiveness of oxygen therapy algorithm was done by Sieber et al. and had similar results. After the intervention, the proportion of patients with supplemental O2 therapy was reduced from 11% (246) to 9% (182) (P < 0.003), a relative decrease of 18%.[17] Undesired effects were similar in nature and frequency in the two observation periods. The study conducted in our ED is in concordance with the given study.
In our study, all patients on oxygen therapy were continuously monitored and the rate of flow of oxygen and additional ventilator support was provided as per the discretion of the treating ED team. Hence fluctuations in saturation were not noted and all patients were considered as being administered oxygen therapy and the duration of therapy was noted. The main outcome considered between the 2 groups in terms of adverse effects was ED mortality (2.7% vs 3.2%) which was not statistically significant.
Another important factor to consider is the cost of oxygen therapy. Oxygen can be considered to be one of the most expensive “drugs” and its unnecessary use only adds to the already financially constrained patients. In our study, the total cost of inappropriate oxygen use was reduced by almost 10 times after the implementation of the protocol. This change can lead to decreased cost burden to the patient in terms of treatment cost, and to the hospital in terms of Oxygen storage and transportation cost, labor charges, professional charges, time for administration and additional human resources. The Oxygen administration can be significantly reduced with minimal/no adverse effects by following simple steps as described by the clinical guidelines. There were patients who had received oxygen for tachypnea without hypoxia which has now become a common clinical scenario, this inappropriate usage of oxygen has to be avoided for the benefit of patients as well as hospital. An experienced clinician has to understand the correct timings and indications for the usage of oxygen instead of taking an over cautious approach. Also, the inappropriate administration might predispose patients to potential dangers of overdose of supplemental oxygen in patients with medical emergencies.
Therefore, this study concludes that that excess of oxygen administration in ED can be easily cut down to prevent unwanted adverse effects, as well as excess cost borne by the patients and the institution. The strength of our study is the very large sample size and the prospective nature of data analysis. One of the limitations of our study was that we did not differentiate between oxygen therapy by mask and by ventilator support and all of them were considered to be administered oxygen. As patients were monitored continuously, only the duration of therapy was calculated while fluctuations in saturation were not documented.
Conclusion
The implementation of an oxygen therapy algorithm significantly reduces inappropriate oxygen use and decreases the duration of oxygen therapy which would translate to decreased cost of treatment to the patient without any risk of side effects or mortality.
Research quality and ethics statement
The authors of this manuscript declare that this scientific work complies with reporting quality, formatting and reproducibility guidelines set forth by the EQUATOR Network. The authors also attest that this clinical investigation was determined to require Institutional Review Board/Ethics Committee review, and the corresponding protocol/approval number is IRB Min. No. 10236 dated 24.08.2016.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hale KE, Gavin C, O'Driscoll BR. Audit of oxygen use in emergency ambulances and in a hospital emergency department. Emerg Med J. 2008;25:773–6. doi: 10.1136/emj.2008.059287. [DOI] [PubMed] [Google Scholar]
- 2.Boyle M, Wong J. Prescribing oxygen therapy. An audit of oxygen prescribing practices on medical wards at North Shore Hospital, Aukland, New Zealand. N Z Med J. 2006;119:U2080. [PubMed] [Google Scholar]
- 3.Dodd ME, Kellet F, Davis A, Smpson JCG, Webb A, Haworth CS, et al. Audit of oxygen prescribing before and after the introduction of a prescription chart. BMJ. 2000;321:864–5. doi: 10.1136/bmj.321.7265.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cornet AD, Kooter AJ, Peters MJ, Smulders YM. Supplemental oxygen therapy in medical emergencies: More harm than benefit? Arch Intern Med. 2012;172:289–90. doi: 10.1001/archinternmed.2011.624. [DOI] [PubMed] [Google Scholar]
- 5.Cornet AD, Kooter AJ, Peters MJL, Smulders YM. The potential harm of oxygen therapy in medical emergencies. Crit Care. 2013;17:313. doi: 10.1186/cc12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranchord AM, Argyle R, Beynon R, Perrin K, Sharma V, Weatherall M, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: A pilot randomized controlled trial. Am Heart J. 2012;163:168–75. doi: 10.1016/j.ahj.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 7.O'Driscoll BR, Howard LS, Davison AG. BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl 6):vi1–68. doi: 10.1136/thx.2008.102947. [DOI] [PubMed] [Google Scholar]
- 8.Smith GB, Prytherch DR, Watson D, Forde V, Windsor A, Schmidt PE, et al. SpO2 values in acute medical admissions breathing air? Implications for the British thoracic society guideline for emergency oxygen use in adult patients. Resuscitation. 2012;83:1201–5. doi: 10.1016/j.resuscitation.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Hunt J. Oxygen therapy administration Policy and Guidelines: The administration of short burst, sustained (medium term) and emergency oxygen to adults in hospital. Royal United Hospital Bath, NHS: Bath, UK; 2013. [Last accessed on 2020 Feb 11]. Available from: http://wwwruhnhsuk/about/policies/docu ments/clinical_policies/blue_clin ical/blue_7017pdf . [Google Scholar]
- 10.Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: Randomized controlled trial. BMJ. 2010;341:c5462. doi: 10.1136/bmj.c5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smallwood CD, Boloori-Zadeh P, Silva MR, Gouldstone A. High oxygen concentrations adversely affect the performance of pulmonary surfactant. Respir Care. 2017;62:1085–90. doi: 10.4187/respcare.05388. [DOI] [PubMed] [Google Scholar]
- 12.Holm BA, Matalon S, Notter RH. Pulmonary surfactant effects and replacement in oxygen toxicity and other ARDS-type lung injuries. In: Lachmann B, editor. Surfactant Replacement Therapy. Springer, Berlin, Heidelberg; 1988. pp. 224–44. doi.org/10.1007/978-3-642-73305-5_27. [Google Scholar]
- 13.Östberg E, Auner U, Enlund M, Zetterström H, Edmark L. Minimizing atelectasis formation during general anaesthesia-oxygen washout is a non-essential supplement to PEEP. Ups J Med Sci. 2017;122:92–8. doi: 10.1080/03009734.2017.1294635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karcz M, Papadakos PJ. Respiratory complications in the postanesthesia care unit: A review of pathophysiological mechanisms. Can J Respir Ther. 2013;49:21–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Edmark L, Kostova-Aherdan K, Enlund M, Hedenstierna G. Optimal oxygen concentration during induction of general anesthesia. Anesthesiology. 2003;98:28–33. doi: 10.1097/00000542-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Sottiaux TM. Consequences of under- and over-humidification. Respir Care Clin N Am. 2006;12:233–52. doi: 10.1016/j.rcc.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Seiber R, Oosterwalder J. Treatment algorithm reduces oxygen use in the Emergency Department. Eur J Emerg Med. 2016;23:114–8. doi: 10.1097/MEJ.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 18.Asciak R, Gouder Ciantar M, Tua J, Fenech V, Montefort S. The effect of a hospital oxygen therapy guideline on the prescription of oxygen therapy. Malta Med Sch Gaz. 2017;1:16–21. [Google Scholar]
- 19.Considine J, Botti M, Thomas S. Descriptive analysis of oxygen use in Australian emergency departments. Eur J Emerg Med. 2012;19:48–52. doi: 10.1097/MEJ.0b013e328347283c. [DOI] [PubMed] [Google Scholar]


