Abstract
This is a case report of the management of pulp canal obliteration of maxillary central incisor using guided endodontic therapy. Patient reported with discolored and proclined 11. Intraoral periapical (IOPA) Radiographs and cone-beam computed tomography (CBCT) showed periapical radiolucency. The canal was obliterated till the middle third and was patent in the apical 7 mm. Root canal treatment (RCT) was planned using guided endodontics. Information of CBCT and digital surface scan were integrated using Blue Sky Bio software. A transparent three-dimensional (3D) model of the tooth and stent, designed with a sleeve for insertion of bur, was 3D-printed using clear resin. After orientation was found satisfactory on the 3D model, access opening was initiated with the orientation of round bur through the stent. IOPAs were taken after preparation of every 3 mm. The canal was located in the apical third. Cleaning and shaping were performed, and RCT completed successfully. Guided endodontic therapy is useful in the management of calcifications in anterior teeth.
Keywords: Computer-assisted designing/computer-assisted machining, guided endodontic therapy, pulp canal obliteration, stent
INTRODUCTION
Root canal calcifications are a regular finding in dental practice, characterized by deposition of tertiary dentin. The deposition of tertiary dentin is region-specific and can be divided into reactionary and reparative dentin. The process of tertiary dentin deposition gets accelerated in teeth affected by traumatic injuries, autotransplantation, orthodontic therapy, jaw fractures, orthognathic surgery, etc., leading to rapid obliteration of the pulpal cavity.[1] Andreasen[2] hypothesized that injury to the pulpal neurovascular bundle triggers a revascularization response in the pulp. However, the loss of control of sympathetic nerve stimulation over odontoblastic secretory activity could result due to differences in the chronological patterns of neural and vascular repair. This loss of nerve control could lead to a rapid and uncontrolled deposition of dentin, thereby causing the obliteration of the pulpal lumen.
Root canal calcifications have various synonyms and etiologies elaborated in literature, some of which are reduced pulpal lumen,[3] dystrophic calcification,[4] pulp calcification,[5] calcific pulp obliteration,[6] and pulp canal sclerosis.[7] The Glossary of Endodontic Terms has defined the term Calcific Metamorphosis as A pulpal response to trauma characterized by rapid deposition of hard tissue within the canal space.[8] However, the term pulp canal obliteration (PCO) given by Andreasen et al.[9] seems a more appropriate term to describe sequelae after dental trauma, as this term more precisely reflects the nature of this response.
The prevalence of PCO after traumatic dental injuries varies widely in clinical literature, ranging from 3.7% to 40%.[1] The development of PCO depends on two main factors: The type of injury and the patient's age at the moment of trauma, with extrusions[10] and lateral luxations[11] showing the highest rates of PCO. Obliteration could be partial or complete and is not a pathology in itself. There have been some suggestions in the literature to intervene immediately on early detection of obliteration. This idea was based on a safe assumption that appearance of clinical symptoms is a definite certainty over a period of time, and therefore, root canal treatment (RCT) should be performed before complete obliteration of all anatomic landmarks. However, there is a clear consensus in the literature that endodontic intervention is to be avoided until and unless periradioular pathosis is detected or the involved tooth becomes symptomatic.[12]
The present scenario for management of obliterated canals includes a variety of instruments such as Long shank (LN) bur, Meuller bur, debriders and orifice openers, ultrasonic tips, etc., all to be used under magnification.[13] All these additions to the traditional armamentarium for endodontic access opening improve the chances of finding and negotiating obliterated canals; however, the process may involve much more time and energy compared to a routine case.
Krastl et al.[14] introduced a digital method to locate obliterated canals. A technique was successfully attempted in an ex vivo study where obliterated canals were first located virtually by obtaining cone-beam computed tomography (CBCT) images and digital impressions of the teeth. This data were then used to design and three-dimensionally (3D) print a stent with a sleeve that would guide the access opening and facilitate the location of the actual canal in the tooth. This technique highlighted the accuracy and reliability of digital data and its potential to be used clinically to obtain predictable results in less time. However, there are not many case reports in literature yet to evaluate the clinical applications of this technique. Hence, this is a case report of the management of calcified metamorphosis of the maxillary anterior tooth using guided endodontic therapy.
CASE REPORT
A 24-year-old male patient reported to the department with discolored and proclined 11 and missing 21 and 22. The patient gave a history of trauma in childhood [Figure 1a]. The electric pulp test with 11 was negative. Radiographic examination revealed complete calcification of the root canal and periapical radiolucency with 11 [Figure 1b]. Furthermore, there was evidence of a radio-opaque restoration in the palatal aspect, suggesting an attempted root canal opening. The extent of radio-opacity was further evaluated with CBCT (PLANMECA), which showed that the canal was obliterated in the cervical and middle third and was patent in the apical 7 mm [Figure 1c]. In addition, periapical radiolucency was detected on the buccal aspect of the root apex. After obtaining written informed consent from the patient, the treatment protocol finalized was RCT, with 11 followed by fixed partial denture (FPD) from 11 to 23. Since RCT with 11 was already attempted, an alternate method of guided endodontics was decided.
Figure 1.
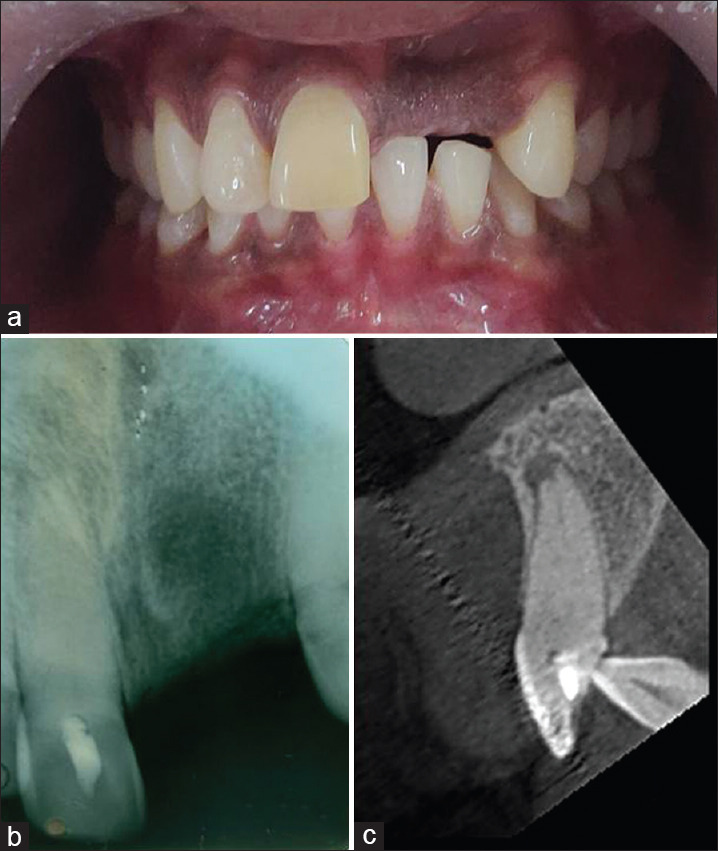
(a) Preoperative photograph. (b) Preoperative radiograph. (c) Cone beam computed tomography image of 11 (sagittal section)
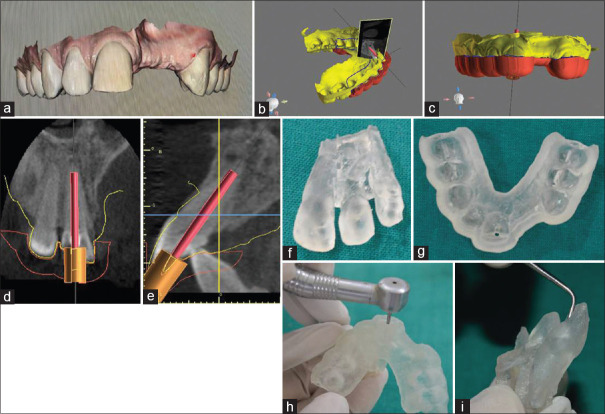
Digital surface scan of the patient was obtained using an intraoral scanner (CS3500-KODAK, CARESTREAM) [Figure 2a]. Information of CBCT and digital surface scan were integrated using Blue Sky Bio Software (BlueSkyBio, LLC, Libertyville, USA) to design a stent from 15 to 25 to guide the access opening [Figure 2b and c]. The stent was designed with a sleeve, to facilitate the insertion of bur. The direction of the sleeve was oriented by superimposing a virtual drill on the CBCT data [Figure 2d and e]. As per digital data, the dimensions of the virtual instrument were decided at 26.5 mm and diameter 2.5 mm, to accommodate the presently available cutting instruments. Keeping the natural location of the canal in mind, the bur was oriented three-dimensionally in such a way that it is centered bucco-lingually and mesio-distally in the center of the root. The stent and a transparent 3D model of the tooth were 3D-printed using clear resin (FormLabs 2) [Figure 2f and g]. The thickness of the stent was 5 mm. To confirm accuracy, preparation was first done on the model through the stent. The preparation was evaluated for its centering through the clear resin [Figure 2h and i]. Once found satisfactory on the model, the stent was checked for adaptation on the patient.
Figure 2.
(a) Digital impression. (b and c) Designing of stent on Blue Sky Bio software. (d and e) Orientation of virtual drill in the centre of the root. (f) 3D model of tooth. (g) 3D printed stent with sleeve. (h and i) Mock preparation on model
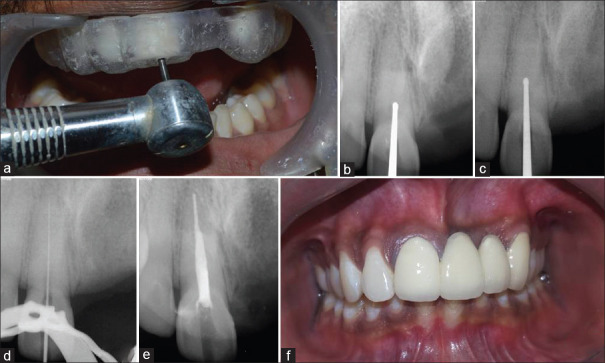
Access opening was initiated with the orientation of round bur (LN surgical round bur (Mani) length: 28 mm size: 010) through the stent [Figure 3a]. Intraoral periapical radiographs were taken after preparation of every 3 mm into the tooth, to confirm the direction of preparation [Figure 3b and c]. The canal was located and negotiated at the junction of the middle and apical third [Figure 3d]. The entire duration of canal location, including intermittent radiographs, took a mere 15 min. Subsequently, cleaning and shaping were performed, and routine RCT was completed successfully and the patient was given an FPD [Figure 3e and f].
Figure 3.
(a) Access opening through stent. (b and c) Intermittant radiographs to evaluate direction of preparation. (d) Negotiation of canal in apical third. (e) Postobturation radiograph. (f) Postoperative photograph after the placement of fixed partial denture
DISCUSSION
Evidence in the literature shows that cases of PCO may show pathological changes like yellow discoloration (8.3%–79%), pulp necrosis and apical periodontitis (1%–27.5%) over a course of time, indicating that a large percentage of cases of PCO need endodontic intervention in due course.[1] The present protocol for managing such cases involves thorough planning with the help of multiple radiographs and access opening using special burs such as LN bur, Mueller bur, and ultrasonic tips. Negotiation is advised with fine instruments (8 or 10 K file), instruments with reduced flutes (Cnal Pathfinder, D finder) or instruments with greater shaft strength (Pathfinder CS).[13] Although the newer instruments available in the market improve the possibility of locating obliterated canals, the absence of anatomical landmarks greatly amplifies the difficulties. The process is quite time consuming, entailing lengthy and sometimes multiple appointments, and generally involves trial and error of the different options of instruments available. Furthermore, the chances mishaps such as over preparation, ledges, and perforation are greater in such cases.[15]
Krastl et al.[14] first introduced the guided endodontic therapy in an ex vivo study. Later, Connert et al.[16] performed guided endodontic therapy for the management of an obliterated maxillary central incisor and concluded that the success rate of the Guided Endodontics technique is high since the deviation of angle (1.59°–1.8°) for all 3D-aspects at the tip of the bur (0.12–0.47 mm) was found to be quite low. In the present case report, RCT had already been attempted. Therefore, to minimize further errors of over preparation, guided endodontic therapy was opted. Furthermore, as experienced by previous authors, the time needed to locate the canal in this case report was very less.[15,16]
Connert et al.[15] presented a case report of mandibular central incisors where the stent was designed through the incisal edge to obtain straight-line access. Though the technique provided ease of designing a stent to provide straight-line access to the apical third of the canal, it greatly compromised the strength and esthetics of the incisal edge of the teeth. In the present case, the stent was planned with access opening on the palatal aspect to preserve the integrity of the incisal edge.
In spite of the advantages, there are a few drawbacks of guided endodontic procedures. Guided therapy is possible only in straight root canals or straight portions of curved canals. However, since dental trauma afflicts the anterior zone predominantly, Guided therapy can be a viable option for the management of PCO following trauma. Guided endodontic therapy appears to be time-consuming with various scans and designing of the stent. However, it is important to note that the chairside time is greatly reduced, compared to the conventional approach, thereby making it more comfortable and acceptable to the patient as well as the clinician. The cost involved may appear to be more, with the requirement of additional facilities. However, in retrospection, the cost may not be too much considering the iatrogenic risks avoided and chairside time saved.
CBCT is a prerequisite for this technique, and hence, increased radiation exposure might be a concern. However, CBCT has proven to be a useful tool to study the degree of calcification and canal morphology for routine cases, too, even if guided endodontic therapy is not planned. Furthermore, for a single tooth, the radiation exposure dose is well within the acceptable limit set by Atomic Energy Regulatory Board.[17]
One hurdle that was encountered was a lack of appropriate dimension cutting instruments. Previous similar case reports have fabricated a custom drill for the access opening. However, the fabrication of a custom instrument adds to the treatment cost, which is already more for guided endodontics than the conventional approach. Therefore, to make the procedure as economical as possible, the presently available instruments in the market have been used in this case.
CONCLUSION
In this case report, guided endodontic therapy was found to be a time-saving method of the management of PCO in anterior teeth. Further research is highly recommended in order for it to be a mainstream treatment option for the management of obliterated canals in anterior teeth.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bastos JV, Côrtes MS. Pulp canal obliteration after traumatic injuries in permanent teeth – scientific fact or fiction? Braz Oral Res. 2018;32(suppl):E75. doi: 10.1590/1807-3107bor-2018.vol32.0075. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen FM. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod Dent Traumatol. 1989;5:111–31. doi: 10.1111/j.1600-9657.1989.tb00348.x. [DOI] [PubMed] [Google Scholar]
- 3.Cvek M, Granath L, Lundberg M. Failures and healing in endodontically treated non-vital anterior teeth with posttraumatically reduced pulpal lumen. Acta Odontol Scand. 1982;40:223–8. doi: 10.3109/00016358209019816. [DOI] [PubMed] [Google Scholar]
- 4.Stroner WF, Van Cura JE. Pulpal dystrophic calcification. J Endod. 1984;10:202–4. doi: 10.1016/S0099-2399(84)80083-7. [DOI] [PubMed] [Google Scholar]
- 5.Birch R, Rock WP. The incidence of complications following root fracture in permanent anterior teeth. Br Dent J. 1986;160:119–22. doi: 10.1038/sj.bdj.4805786. [DOI] [PubMed] [Google Scholar]
- 6.Torneck CD. The clinical significance and management of calcific pulp obliteration. Alpha Omegan. 1990;83:50–4. [PubMed] [Google Scholar]
- 7.Yates JA. Root fractures in permanent teeth: A clinical review. Int Endod J. 1992;25:150–7. doi: 10.1111/j.1365-2591.1992.tb00778.x. [DOI] [PubMed] [Google Scholar]
- 8.Glossary of Endodontic Terms. 8th ed. Chicago: American Association of Endodontics; 2012. [Google Scholar]
- 9.Andreasen FM, Zhijie Y, Thomsen BL, Andersen PK. Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Endod Dent Traumatol. 1987;3:103–15. doi: 10.1111/j.1600-9657.1987.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 10.Lee R, Barrett EJ, Kenny DJ. Clinical outcomes for permanent incisor luxations in a pediatric population II. Extrusions Dent Traumatol. 2003;19:274–9. doi: 10.1034/j.1600-9657.2003.00208.x. [DOI] [PubMed] [Google Scholar]
- 11.Nikoui M, Kenny DJ, Barrett EJ. Clinical outcomes for permanent incisor luxations in a pediatric population III Lateral luxations. Dent Traumatol. 2003;19:280–5. doi: 10.1034/j.1600-9657.2003.00209.x. [DOI] [PubMed] [Google Scholar]
- 12.Amir FA, Gutmann JL, Witherspoon DE, et al. Calcific metamorphosis: A challenge in endodontic diagnosis and treatment. Quintessence Int. 2001;32:447–55. [PubMed] [Google Scholar]
- 13.Thomas B, Chandak M, Patidar A, Deosarkar B, Kothari H. Calcified canals: A review. IOSR J Dent Med Sci. 2014;13:38–43. [Google Scholar]
- 14.Krastl G, Zehnder MS, Connert T, Weiger R, Kuhl S. Guided endodontics: A novel treatment approach for teeth with pulp canal calcification and apical pathology. Dent Traumatol. 2016;32:240–6. doi: 10.1111/edt.12235. [DOI] [PubMed] [Google Scholar]
- 15.Connert T, Zehnder MS, Amato M, Weiger R, Kuhl S, Krastl G. Microguided endodontics: A method to achieve minimally invasive access cavity preparation and root canal location in mandibular incisors using a novel computer-guided technique. Int Endod J. 2018;51:247–55. doi: 10.1111/iej.12809. [DOI] [PubMed] [Google Scholar]
- 16.Connert T, Zehnder MS, Weiger R, Kuhl S, Krastl G. Microguided endodontics: Accuracy of a miniaturized technique for apically extended access cavity preparation in anterior teeth. J Endod. 2017;43:787–90. doi: 10.1016/j.joen.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 17. [Last accessed on 2020 Jan 12]. Available from: https://www.aerb.gov.in/images/PDF/DiagnosticRadiology/e-LORA-Diagnostic-Radiology-guidelines.pdf .