The colloquial saying “If we fail to learn from history, we are destined to repeat it” holds true. In late 2019, a new pathogen, SARS-CoV-2, spread across the globe, killing hundreds of thousands and exposing long-standing health and social inequities. Older adults have been deemed most at risk for severe COVID-19 outcomes, resulting in less focus on younger age groups, particularly youths, defined as adolescents and young adults (AYA) aged 15 to 24 years.
We have been here before. AYA were largely ignored in the earlier stages of the HIV pandemic, but they now account for about 30% of new HIV infections worldwide.1 Similarly, in past months, it was thought that most youths were not at risk for severe complications and dying from COVID-19. However, some have become sick and died from the illness, and newer evidence has related multisystem inflammatory syndrome in children to the disease. Youths may also be asymptomatic carriers of SARS-CoV-2, placing their communities at risk. Historically, youth engagement in school and community settings has contributed to influenza outbreaks, potentially complicating COVID-19 surveillance and increasing health care use among youths’ network members.
With an estimated 1.2 billion AYA globally in 2020,2 we cannot afford to overlook this young population. Many serve as the backbone of several social networks, connecting homes, schools, and workplaces in their communities. It is through these networks that some have acquired HIV and that others may acquire and transmit COVID-19. It is also through these networks that the social impacts of COVID-19 and its mitigation efforts may affect AYA through devastating social and economic disruption. AYA are also needed in our societies and are a source of resilience and change, as recently demonstrated in the United States and other nations where they continue to confront the intersecting challenges of racial discrimination, health, and economic inequities. Furthermore, youths have distinct needs that cannot be ignored during the COVID-19 pandemic. They are undergoing a specific developmental period characterized by biological, cognitive, and social change3 and need to have the opportunity and support to grow into healthy adults. However, for some during the COVID-19 pandemic, development will continue to be challenged by the same social inequities that place them at risk for HIV, poor HIV outcomes, and other illnesses.
We call on our fellow researchers, clinicians, policymakers, and practitioners, as well as others, to dedicate increased COVID-19 attention and focus to youths now. We offer several key approaches learned during the HIV epidemic that may help improve short- and long-term COVID-19–related outcomes among this population and protect their broader communities.
APPROACH 1: DISAGGREGATE AND COLLECT DATA
Although age-disaggregated COVID-19 data are emerging, a critical lesson learned from HIV is that we need more age-specific data, and we need it sooner. Lack of age-disaggregated data resulted in limited prevention approaches and resources directed to youths until later in the HIV context, and to avoid this same type of delay with COVID-19, we need to act in this moment. As we explored sources of national-level data from several countries since the COVID-19 outbreak began, we found some examples of AYA being partially grouped with children (aged 5–17 years4; aged 19 years or younger5) or with adults more broadly (aged 18–49 years4). Publicly available age-disaggregated data are also currently lacking among some lower- and middle-income countries, including those in sub-Saharan Africa. Further disaggregation of age-specific data by gender, race, ethnicity, sexual identity, and socioeconomic status will further help us understand how youths fare in comparison with other age groups and subgroups.
Additionally, we need to actively collect data on how COVID-19 and related mitigation efforts affect AYA’s mental health, housing, food security, family relationships, and work opportunities. Learning from the HIV epidemic, it is critical that we take a multilevel approach when obtaining these data, recognizing that these levels interact and overlap, and their influence changes as youths develop and grow into adults. Our Johns Hopkins University Center for AIDS Research AYA Scientific Working Group has modified the World Health Organization determinants of adolescent health and development ecological model3 to identify potential negative multilevel impacts of COVID-19 on AYA (Figure 1). Data can be collected among these various strata, which include the individual, interpersonal, community and organizational, environmental, and macro and structural levels.
FIGURE 1—
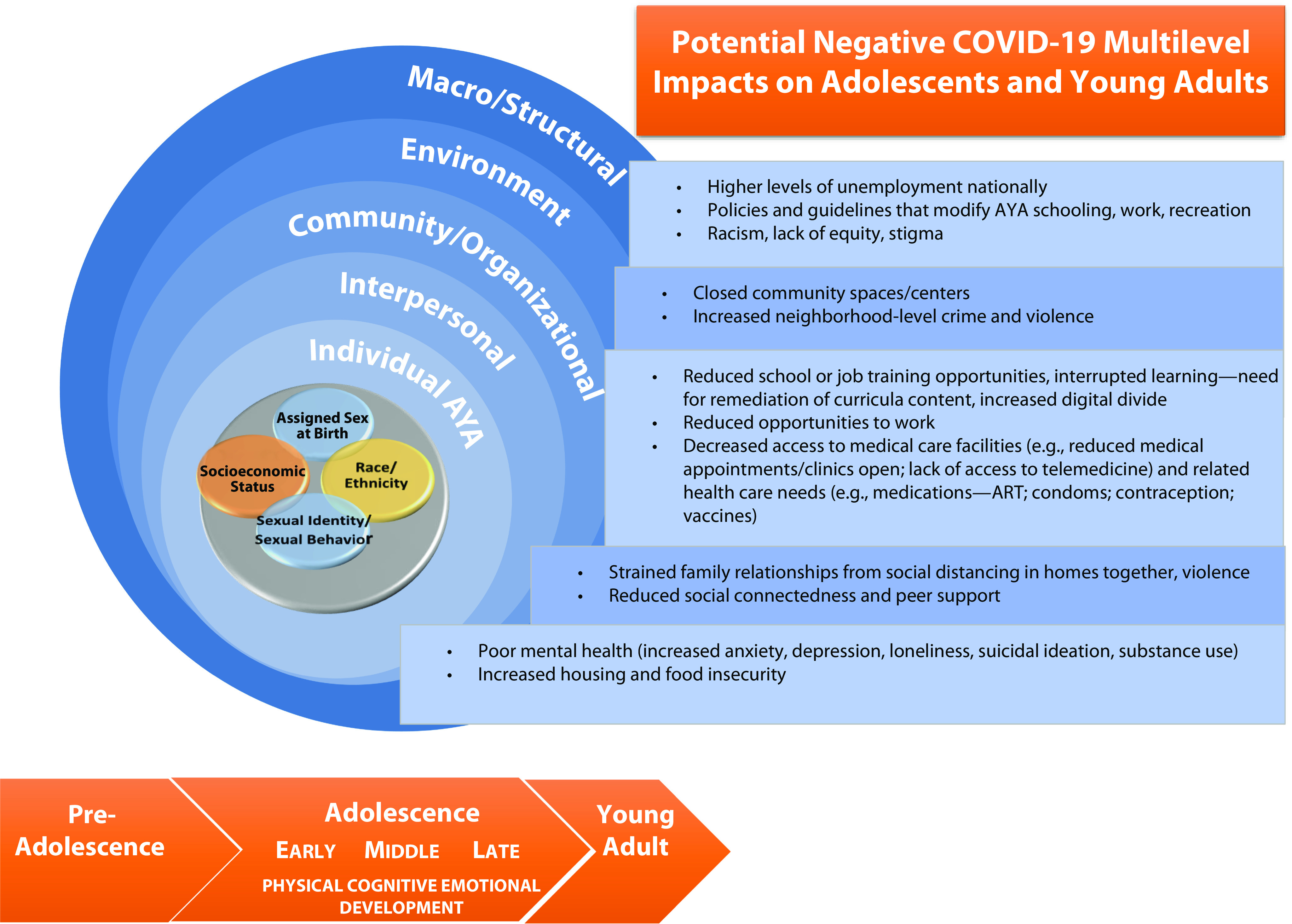
Examples of Potential Multilevel Impacts of COVID-19 on Adolescents and Young Adults: 2020
Note. AYA = adolescents and young adults. The figure is an adapted World Health Organization ecological model of the determinants of adolescent health and development.
Source. World Health Organization (https://www.who.int/about/who-we-are/publishing-policies/copyright).3
APPROACH 2: TAKE A HARM-REDUCTION APPROACH
Currently, there is limited AYA-tailored mainstream messaging related to COVID-19 prevention outside the general recommendations of not gathering in large groups, wearing masks, and keeping social distance. Although some AYA do gather virtually with friends for special events, classes, and parties, others still gather as they did before the COVID-19 pandemic. The latter may be because youths, by definition, are still developing impulse control, emotional regulation, and self-identity, and, consequently, they may not internalize general risk-reduction warnings, especially given the initial COVID-19 data suggesting that AYA were at less risk for poor outcomes. Additionally, social gathering is a critical part of socioemotional development for youths, and not all AYA have the same resources to connect with friends through alternative means and rely on in-person meetings as their main source of social support. This situation may be especially true for AYA escaping family violence exacerbated by social and economic stressors during the pandemic.
In response, COVID-19 prevention efforts among those aged 15 to 24 years need to take a harm-reduction approach, defined as reducing the risk of negative health outcomes when a risk behavior cannot be completely eliminated. Needle exchange programs, for example, were a highly successful harm-reduction strategy that decreased HIV acquisition among people who inject drugs.6 In the context of COVID-19, with the need for sustained prevention efforts, harm reduction means helping AYA figure out how to engage in risky activities such as holding parties, substance use, and having in-person sex in ways that better protect them from acquiring COVID-19. For example, a harm-reduction approach for AYA who vape might include the message “If vaping with friends, have your own equipment, and do not share it to reduce exposure to the respiratory droplets of others.” Clear messages and policies that address the varied circumstances of youths will be critical as we apply harm-reduction principles to the COVID-19 pandemic.
APPROACH 3: ENGAGE THE YOUTHS
Perhaps one of the most valuable lessons learned from the HIV pandemic is the importance of youth engagement. Engagement does not mean simply having youths participate in a research study or be beneficiaries of a program: it means fostering youth leadership and capacity building and acknowledging and addressing existing inequities. Youth engagement may include the use of participatory research methods and positive youth development resources and, within the HIV epidemic, has included youth-led research, interventions, and advisory boards. For example, Denison et al. tested a youth-led peer mentor intervention in a randomized control trial in Zambia to improve viral suppression and reduce stigma among AYA living with HIV.7 Our Johns Hopkins University Center for AIDS Research AYA Scientific Working Group also partners with a youth advisory board that informs and drives the work of some of our current group members in Baltimore, Maryland. Of particular importance, we listen and learn from our most vulnerable youths, who do not necessarily live in safety, who may not have access to ample resources, or who do not identify with binary sexual or gender identities.
We can actively support youths in championing innovative and effective solutions to COVID-19 challenges grounded in a human rights perspective and evidence showing that youth engagement is effective. Such engagement will ensure that appropriate research, programs, and developmentally tailored messages involve and reach youths in their most familiar and culturally appropriate language, mitigating the potential spread and impact of COVID-19.
SUMMARY
Reflections on the HIV pandemic offer a reminder that increased attention should be paid to youths aged 15 to 24 years. We offer successful ways identified in the HIV pandemic to help and partner with youths that are applicable during the time of COVID-19. These include understanding how COVID-19 is affecting youths through data disaggregation and collection, using harm-reduction strategies, and engaging youths throughout the pandemic. Embracing these approaches may yield optimal outcomes for youths and their communities in the short and long terms. Success hinges on the involvement of all of us to act now.
ACKNOWLEDGMENTS
This work was supported by the Johns Hopkins University Center for AIDS Research, a National Institutes of Health (NIH)–backed program (grant 1P30AI094189), which is funded by the following NIH cofunding and participating institutes and centers: National Institute of Allergy and Infectious Diseases (NIAID), National Cancer Institute, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), National Heart, Lung, and Blood Institute, National Institute on Drug Abuse (NIDA), National Institute on Aging, National Institute of General Medical Sciences, National Institute of Diabetes and Digestive and Kidney Diseases, and National Institute of Minority Health and Disparities (NIMHD). This work was also funded through NIH/NIAID (grant T32AI102623 to S. M. D.) and the NICHD Office of Women’s Health and the Johns Hopkins Building Interdisciplinary Research Careers in Women’s Health award (award K12HD085845 to K. A. A.). Furthermore, this work was funded by the National Institute of Mental Health (grants R01MH123352, R34MH116725, R21MH118945 to C. Y.) and the National Institute on Minority Health and Health Disparities (grant R01MD013495 to C. Y.). Additionally, this work was funded through the NIMHD (grant R01 MD011770 to A. A.), NIDA (grant R01DA043089 to R. A.-S.), and the National Center for Complementary and Integrative Health (5K01AT009049-02 to J. A. D.). Finally, this research was funded by an administrative supplement (to M. R. K.) to the Johns Hopkins University Center for AIDS Research, an NIH-funded program (grant P30AI094189).
Note. The contents of this editorial reflect the thoughts of the authors and not necessarily those of the NIH.
CONFLICTS OF INTEREST
None of the authors has any conflicts of interest to report.
REFERENCES
- 1.Joint United Nations Programme on HIV and AIDS. UNAIDS data 2019. Available at: https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf. Accessed June 16, 2020. [PubMed]
- 2.United Nations, Department of Economics and Social Affairs, Population Dynamics. World population prospects 2019. Population data. Subgroup: age composition. Annual population by age groups—both sexes. Available at: https://population.un.org/wpp/Download/Standard/Population. Accessed June 16, 2020.
- 3.World Health Organization. Health for the world’s adolescents: a second chance in the second decade. 2014. Available at: https://apps.who.int/iris/bitstream/handle/10665/112750/WHO_FWC_MCA_14.05_eng.pdf. Accessed June 27, 2020.
- 4.Centers for Disease Control and Prevention, COVID-NET. COVID-19 laboratory-confirmed hospitalizations. Available at: https://gis.cdc.gov/grasp/COVIDNet/COVID19_5.html. Accessed May 28, 2020.
- 5.Government of Canada. Coronavirus disease 2019 (COVID-19): epidemiology update. Available at: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html. Accessed May 28, 2020.
- 6.Dutta A, Wirtz AL, Baral S, Beyrer C, Cleghorn FR. Key harm reduction interventions and their impact on the reduction of risky behavior and HIV incidence among people who inject drugs in low-income and middle-income countries. Curr Opin HIV AIDS. 2012;7(4):362–368. doi: 10.1097/COH.0b013e328354a0b5. [DOI] [PubMed] [Google Scholar]
- 7.Denison JA, Burke VM, Miti S et al. Project YES! Youth Engaging for Success: a randomized controlled trial assessing the impact of a clinic-based peer mentoring program on viral suppression, adherence, and internalized stigma among HIV-positive youth (15–24 years) in Ndola, Zambia. PLoS One. 2020;15(4):e0230703. doi: 10.1371/journal.pone.0230703. [DOI] [PMC free article] [PubMed] [Google Scholar]


