Abstract
Objectives. To assess costs of video and traditional in-person directly observed therapy (DOT) for tuberculosis (TB) treatment to health departments and patients in New York City, Rhode Island, and San Francisco, California.
Methods. We collected health department costs for video DOT (VDOT; live and recorded), and in-person DOT (field- and clinic-based). Time–motion surveys estimated provider time and cost. A separate survey collected patient costs. We used a regression model to estimate cost by DOT type.
Results. Between August 2017 and June 2018, 343 DOT sessions were captured from 225 patients; 87 completed a survey. Patient costs were lowest for VDOT live ($1.01) and highest for clinic DOT ($34.53). The societal (health department + patient) costs of VDOT live and recorded ($6.65 and $12.64, respectively) were less than field and clinic DOT ($21.40 and $46.11, respectively). VDOT recorded health department cost was not statistically different from field DOT cost in Rhode Island.
Conclusions. Among the 4 different modalities, both types of VDOT were associated with lower societal costs when compared with traditional forms of DOT.
Public Health Implications. VDOT was associated with lower costs from the societal perspective and may reduce public health costs when TB incidence is high.
Tuberculosis (TB) treatment requires many months of antibiotic therapy. For persons who fall ill with drug-susceptible strains of TB, the recommended treatment duration is 6 to 9 months with a median treatment duration of 252 days (approximately 8.4 months).1,2 Drug-resistant TB treatment requires greater treatment duration and the use of additional medications, and often is associated with additional toxicity and cost.3
In the United States, TB prevention and control efforts have led to a decline in TB incidence from 14.1 cases per 100 000 in 1974 to 2.8 cases per 100 000 in 2017.4 This decline has slowed in recent years, and modeling studies forecast that TB will not be eliminated from the United States within this century.5 While TB rates have declined, public health funding has also declined, leading health departments to look for alternative approaches to provide care and maintain control of TB.6
A cornerstone of TB control is the use of directly observed therapy (DOT), in which health department staff meet with patients to monitor for medication side effects and support treatment adherence.1,7 To implement DOT, programs have traditionally sent staff to meet patients at a location outside of the clinic (e.g., the patient’s home or workplace; field DOT) or asked patients to travel to the TB clinic (clinic DOT).
Telemedicine, in which patients and providers meet virtually and interact remotely via communication technology, has the potential to reduce the cost of care.8 For this reason, a number of TB programs have adopted a type of telemedicine called video DOT (VDOT), in which patients use a video-enabled electronic device to allow TB staff to virtually observe treatment ingestion. The 2 types of VDOT are live VDOT, also known as “synchronous VDOT,” in which the patient and provider interact in real time, and recorded VDOT, also known as “asynchronous VDOT,” in which the patient records a video and the provider reviews the video later. A randomized controlled trial in the United Kingdom reported recorded VDOT to have lower health department costs and a higher observed proportion of scheduled doses as compared with traditional forms of DOT.9 Recent US evidence suggests that VDOT can also reduce time and costs associated with DOT for health departments.10–15 However, additional study is needed to delineate costs to patients and TB programs that operate within diverse localities, have alternative staffing structures, and provide care to varying numbers of patients. This evaluation estimates both patient and health department costs associated with DOT and VDOT in New York City (613 TB cases); San Francisco, California (107 TB cases); and Rhode Island (13 TB cases) in 2017.
METHODS
Data collection began in September 2017 and lasted through June 2018. We collected health department operations data, including the number of TB cases, total DOT doses delivered by DOT type, DOT staff persons, and types of video DOT provided. In addition, health department staff were interviewed to collect start-up and fixed costs of training, VDOT software and hardware costs, and number of DOT-dedicated vehicles. Costs associated with field DOT included vehicle maintenance, depreciation, insurance, parking, and the cost of public transportation. Because health departments often offer incentives (e.g., meal vouchers) or enablers (e.g., public transit vouchers) to patients, we included incentive and enabler costs when provided.
Prospective Directly Observed Therapy Logs
Health department staff completed time–motion logs for 3 to 5 days of DOT sessions for all types of DOT (clinic DOT, field DOT, VDOT live, or VDOT recorded). Days of the week were not repeated within site, and data collection was spaced over a period of 16 weeks. All DOT staff members completed DOT logs. If staff members were absent on a day of observation, those staff members conducted their time–motion log the following week. New York City was sampled on randomly chosen weekdays without replacement such that each borough and DOT type was represented, and every DOT staff member was sampled once over the sampling period.
For each DOT session, staff recorded patient characteristics including number of weeks of treatment, the type of DOT session, and whether the patient was being treated for latent TB infection, drug-susceptible TB disease, or drug-resistant TB disease. Staff also collected the start and finish times for DOT sessions, whether sessions were “missed” or “rescheduled,” whether the patient reported medication side effects, the travel time and distance, and if the patient needed translation services. Generic nonidentifying patient and staff numeric codes were used to identify DOT sessions.
DOT start time was defined as when staff arrived at a patient’s DOT location (or the patient entered the DOT room), and finish time was defined as when staff left the patient’s home (or the patient left the DOT room). For VDOT, start time was defined as when staff started a session by logging on to observe a dose, and finish time was when staff logged off after viewing a dose. Travel time for field DOT was measured as the time from previous location to the next patient’s location (including parking). We used corresponding Bureau of Labor Statistics (BLS) metropolitan statistical area (MSA) hourly wages by occupational category to estimate wage costs and added 30% for fringe benefits.16
Health Department Directly Observed Therapy Costs
Health departments incurred start-up training costs for clinic staff when initiating VDOT implementation. We estimated training costs by multiplying the time spent in training by the corresponding BLS wage for each attendee. VDOT vendors did not charge for their in-person training sessions.
Fixed costs for VDOT included software, phones, webcams, headsets, computers, and tablets purchased to conduct VDOT (depreciated over an estimated 3 years of life, with no scrap value). As the cost of smartphones was not available, we valued each smartphone at $460 (2017 average price of a smartphone sold in North America).17 We did not include computers repurposed for VDOT or computers that had multiple uses in the cost analysis. Sites reported their annual cost of VDOT software contracts with providers.17 We calculated the per-session fixed cost by dividing fixed costs by total annual sessions for each DOT type. In this way, per-session DOT cost is reflective of the health department practices and dosing schedules in 2017 (Table 1). Because of limited data on vehicle purchase, maintenance, and insurance costs, we assumed that all vehicles were small, compact cars. We calculated insurance, depreciation, and maintenance via the American Automobile Association formulas for cost of ownership (see the “Additional Details on Cost Calculations” in the Appendix, available as a supplement to the online version of this article at http://www.ajph.org).18 Finally, because TB programs operate TB clinics regardless of the type of DOT, we did not include overhead costs associated with maintaining a clinic.18
TABLE 1—
Site Directly Observed Therapy (DOT) Descriptive Data: New York City; San Francisco, CA; and Rhode Island; 2017–2018
| New York City | Rhode Island | San Francisco, CAa | |
| 2017 TB | |||
| Cases, no. | 613 | 13 | 107 |
| Rate per 100 000 | 7.1 | 1.2 | 7.6 |
| DOT workers, no. | 10 | 1 | 4 |
| Annual DOT sessions, no. | 40 546 | 2 372 | 19 735 |
| VDOT recorded | |||
| Annual patients, no. | 186 | 9 | 62 |
| Annual sessions, no. | 7 964 | 708 | 7 488 |
| DOT schedule | |||
| Initial in-person DOT required | No | Yes | Yes |
| Intensive phase | 5× per wkb | 7× per wkc | 7× per wkc |
| Continuation phase | 3× wk offeredb | 7× per wkc | 7× per wkc |
| Software cost, $ | 19 440 | 14 310 | 12 060 |
| VDOT live | |||
| Annual patients, no. | 399 | NA | NA |
| Annual sessions, no. | 14 045 | NA | NA |
| DOT schedule | |||
| Initial in-person DOT required | No | NA | NA |
| Intensive phase | 5× per wkb | NA | NA |
| Continuation phase | 3× week offeredb | NA | NA |
| Software cost,d $ | 1 152 | NA | NA |
| Clinic DOT | |||
| Annual patients, no. | 597 | NA | 143 |
| Annual sessions, no. | 9 273 | NA | 4 435 |
| DOT schedule | |||
| Intensive phase | 5× per wkb | NA | 5× per wk |
| Continuation phase | 3× wk offeredb | NA | 5× per wk |
| Clinics, no. | 4 | NA | 1 |
| Field DOT | |||
| Annual patients, no. | 280 | 20 | 152 |
| Annual sessions, no. | 9 264 | 1 664 | 7 812 |
| DOT schedule | |||
| Intensive phase | 5× per wkb | 5× per wk | 5× per wk |
| Continuation phase | 3× wk offeredb | 5× per wk | 5× per wk |
| DOT dedicated vehicles | 10 | 1 | 2 |
| DOT miles travelede | 41 198 | 18 054 | 16 351 |
Note. NA = site does not offer DOT; VDOT = video DOT.
Estimated annual doses and patients.
Self-administered weekend doses and intermittent dosing based on physician discretion.
Rhode Island and San Francisco weekend doses are observed via recorded video.
New York City VDOT live costs were based on Microsoft Office Suite 365 2017 government contract costs.
DOT miles based on miles per session plus a return trip for each day of observation.
Variable costs included cost of DOT and VDOT staff time, which was estimated by multiplying the staff member’s estimated hourly wage plus benefits by staff time. Variable costs also included training patients for VDOT, and provided incentives and enablers. We did not include costs associated with masks, gloves, or water cups as their use varied by patient and locality.19 We estimated the cost of gasoline for DOT-dedicated staff vehicles based on the distance traveled, divided by the fuel economy and multiplied by the annual average cost of gasoline in the site’s MSA in 2017.20 We estimated daily available capacity for field DOT as staff daily work hours, minus 1 hour for breaks and 25 minutes needed for a return trip from the field.
Patient Costs
In each site, we surveyed a convenience sample of patients aged at least 18 years, with written surveys at the clinic or by phone after their most recent clinic session. Surveys were available in Chinese, English, Spanish, and Vietnamese; interpreters were used when needed. We collected information on age, race/ethnicity, health status, country of birth, education, occupation, job title, monthly income, distance traveled to the TB clinic, time spent traveling, cost of travel, and time spent waiting at the clinic. For patients on field or clinic DOT, we estimated time spent in the clinic or during field DOT by using the DOT time reported by health department staff.
Survey questions included VDOT-specific information such as time spent learning software, type of hardware (e.g., phones or tablets), and technical problems associated with their most recent session. We also collected information on patient needs for childcare when traveling to the TB clinic and the number of times patients contacted staff via phone, text, or e-mail regarding a DOT visit.
To estimate the value of patient time spent on DOT and travel, we used patients’ self-reported income. If a patient’s income was not reported, we matched their self-reported occupation and job title to MSA wage data.16 Among patients who were unemployed or students, we valued their time by using an annual value of household productivity matched by age and gender.21 We estimated the value of dependent care by using BLS wages for care providers by MSA.16 We prorated the cost of patients’ personal phones used for VDOT by the time the patient spent on VDOT. We assumed patient phones had the same purchase price and useful life as the national average cost of a smartphone ($460).
Data Analysis
We used RStudio 1.1.453 with R version 3.6.1 to import, clean, and analyze our data.22 Because our dependent variable (DOT time) was nonnegative and highly right-skewed (Appendix Figure A), and contained repeated observations on staff and patients, we used the lme4 package for generalized linear mixed-effects models (“Regression Analyses” in the Appendix).23 The model controlled for the type of DOT, whether side-effects were reported, whether the session was missed or rescheduled, the phase of treatment (intensive phase: ≤ 8 weeks of treatment; continuation phase: > 8 weeks and ≤ 36 weeks of treatment; and long duration: > 36 weeks of treatment), whether the patient had drug-resistant TB or latent TB infection, and if the patient needed interpretation. The reference case was field DOT time in minutes for a patient with drug-susceptible TB. To examine the significance of differences between DOT modalities, we calculated confidence intervals (CIs) of the difference that accounted for the covariance between estimates.
Health department costs and patient costs are reported separately per DOT dose and per patient completing treatment. Similarly, we estimated overall patient costs via patient survey sample means, medians, and the 2.5 and 97.5 percentiles.
Societal Costs
To estimate societal costs, we added health department and patient costs by type of DOT. Before averaging health department and patient costs by site, we adjusted individual site costs for purchasing power parity using the Bureau of Economic Analysis implicit regional price deflator by MSA (index = 100).
RESULTS
Sites varied in their provision of DOT: New York City provided all 4 types of DOT; San Francisco provided field DOT, clinic DOT, and recorded VDOT; and Rhode Island provided field DOT and recorded VDOT (Table 1). All 3 sites offered daily dosing and New York City also offered intermittent (3× per week) dosing. We observed 353 staff sessions (drug-resistant TB: 7 sessions representing 6 patients; latent TB infection: 11 sessions representing 5 patients). We excluded sessions that were non–DOT related or included non-DOT activities (n = 7) and sessions that did not record a start or finish time (n = 3). The final sample represented 343 DOT sessions from 225 patients; 105 (70 patients) were field DOT, 65 (52 patients) were clinic DOT, 57 (50 patients) were live VDOT, and 116 (63 patients) were recorded VDOT. Five patients were observed in 2 types of DOT. Our regression analysis of DOT times estimated an average DOT time of 4.86 minutes (95% CI = 3.77, 6.26) for live VDOT, 5.62 (95% CI = 4.06, 7.77) for recorded VDOT, 10.27 (95% CI = 7.51, 14.04) for clinic DOT, and 10.13 (95% CI = 7.89, 3.01) for field DOT. Regression adjusted average travel time for field DOT was 16.67 minutes (95% CI = 12.08, 22.99).
Health Department Directly Observed Therapy Costs
Cost associated with start-up training varied from $0.06 to $1.66 per session (Table 2). Our sample included 2 recorded VDOT software platforms (emocha and SureAdhere) and 1 live VDOT platform (Skype for Business).24–26 Annual software costs ranged from $1152 to $19 440 in 2017 (Table 1). Per-session software costs ranged from $0.14 to $20.21 per session. One site provided 122 phones to patients for VDOT at a monthly service cost of $34.99. Both sites that provided clinic DOT provided incentives and enablers for patients to attend clinic sessions (Table 2). For example, New York City provided transportation cards for patients ($5.50) and San Francisco offered lunch gift certificates ($5 all clinic DOT patients) as well as 2 bus tokens ($3 for 25% of clinic DOT patients) or a monthly bus pass ($40 per month for 56% of clinic DOT patients).
TABLE 2—
Health Department Directly Observed Therapy (DOT) Costs per Session by DOT Type and Site: New York City; San Francisco, CA; and Rhode Island; 2017–2018
| VDOT Recorded, US$ 2017 | VDOT Live, US$ 2017, | Field DOT, US$ 2017 | Clinic DOT, US$ 2017 | ||||||
| NYC | RI | SF | NYC | NYC | RI | SF | NYC | SF | |
| Start-up costsa: initial staff training | 0.11 | 1.66 | 0.50 | 0.06 | |||||
| Fixed costsb | |||||||||
| Vehicles | 7.12 | 3.61 | 1.44 | ||||||
| Hardware | 2.16 | 0 | 0 | 2.51 | 1.01 | ||||
| Software | 2.44 | 20.21 | 1.61 | 0.14 | |||||
| Variable costs | |||||||||
| DOT time, $ per session (95% CI)c | 2.96 (2.23, 3.92) | 2.28 (1.03, 5.02) | 5.86(3.57, 9.63) | 2.90 (2.25, 3.75) | 7.54 (5.78, 9.83) | 3.55 (1.91, 6.60) | 9.37 (6.78, 12.94) | 3.37 (2.51, 4.54) | 27.55 (13.82, 54.91) |
| Gasoline | 0.39 | 0.91 | 0.45 | ||||||
| Patient enablerd | 0.43 | 0 | 1.58 | 0.43 | 5.50 | 7.20 | |||
| Patient trainingd | 0.40 | 0.17 | 0.33 | 0.49 | |||||
| Travel time, $ per session (95% CI)c | 10.52 (6.90, 16.04) | 11.86 (4.14, 33.94) | 8.17 (4.45, 14.99) | ||||||
| Return trip | 1.10 | 1.10 | 1.00 | ||||||
| Subtotal cost per session | 8.39 | 22.66 | 9.38 | 6.47 | 27.68 | 21.03 | 20.43 | 8.87 | 34.75 |
| Cost of missed sessione | 0.57 | 1.54 | 0.64 | 0.79 | 0.52 | 0.40 | 0.39 | 0 | 0 |
| Total cost per session (95% CI)c | 8.96 (8.84, 10.04) | 24.20 (23.57, 25.26) | 10.02 (7.75, 10.64) | 7.26 (6.88, 8.45) | 28.20 (23.40, 33.43) | 21.43 (8.86, 34.23) | 20.82 (15.56, 27.61) | 8.87 (8.88, 10.69) | 34.75 (29.90, 38.88) |
| Total cost per session, PPP adjusted $ (95% CI)f | 6.51 (5.95, 7.26) | 21.59 (20.39, 24.19) | 6.96 (5.26, 9.75) | 5.64 (5.13, 6.29) | 22.06 (18.17, 25.95) | 20.52 (8.44, 32.60) | 16.01 (11.54, 20.48) | 6.89 (6.21, 7.79) | 25.77 (15.59, 46.08) |
Note. CI = confidence interval; NYC = New York City; PPP = purchasing power parity; RI = Rhode Island; SF = San Francisco, CA; VDOT = video DOT.
Start-up costs are 1-time costs when first setting up VDOT and are not included in total cost per dose.
Vehicle fixed costs include annual vehicle costs (depreciation, insurance, and maintenance). Hardware includes the cost of phones, webcams, and tablets.
95% CI generated from generalized linear mixed model regression with random effects on patients and staff (“Regression Analysis” in the Appendix, available as a supplement to the online version of this article at http://www.ajph.org).
Cost per dose of patient enablers and training cost based on 124 total dose treatment regimen.
Missed sessions were observed 6.8%, 12.3%, 1.9%, and 0% of the time for VDOT recorded, VDOT live, field DOT, and clinic DOT, respectively.
Adjusted for PPP using Bureau of Economic Analysis 2017 implicit regional price deflator by metropolitan statistical area.
Field DOT and recorded VDOT were offered by every site (Table 2). Compared with field or clinic DOT options, VDOT was associated with lower costs to health department in all 3 sites. However, for the smallest health department, Rhode Island, the mean recorded VDOT cost was greater than field DOT ($24.20 vs $21.43, respectively); this difference was not statistically significant at the 5% level.
Patient Costs
A total of 87 patients responded to our survey—55 in New York City, 25 in San Francisco, and 7 in Rhode Island. Our sample of patients was similar to the national population of TB patients in terms of percentage male (63% vs 62%), the group aged 45 to 64 years (30% vs 33%), and positive HIV status (5% vs 6%); however, the sample differed with a lower proportion of patients in the group aged 65 years or older (10% vs 26%), and greater proportions of patients in the group aged 18 to 44 years (59% vs 41%), in the Asian racial/ethnic group (60% vs 36%), who were non–US-born (95% vs 73%), and who were unemployed (43% vs 34%; Appendix Table A).4 The greatest patient cost was the value of time associated with clinic DOT: $17.99 (range = $2.57–$80.99). The next largest cost was out-of-pocket expenses associated with travel to the clinic: $6.63 (range = $0.00–$30.97). After adjusting for purchasing power parity and subtracting the value of site incentives and enablers, the average patient cost for a clinic DOT visit was $33.98 (Table 3).
TABLE 3—
Patient Cost Summary Data by Directly Observed Therapy (DOT) Type: New York City; San Francisco, CA; and Rhode Island; 2017–2018
| US$ 2017, Mean (Median; 95% Range) | |
| VDOT recorded (n = 50) | |
| Traininga | |
| Health department (n = 50) | 0.06 (0.05; 0.01, 0.14) |
| Self-learn time (n = 45) | 0.03 (0.02; 0.00, 0.09) |
| DOT time cost (n = 48) | 1.12 (0.58; 0.11, 4.36) |
| Phoneb (n = 38) | 0.01 (0.01; 0.00, 0.05) |
| Total cost per session (n = 34) | 1.10 (0.56; 0.12, 5.97) |
| VDOT live (n = 37) | |
| Traininga | |
| Health department (n = 37) | 0.04 (0.04; 0.01, 0.07) |
| Self-learn time (n = 24) | 0.03 (0.01; 0.00, 0.18) |
| DOT time cost (n = 35) | 0.95 (0.71; 0.17, 2.63) |
| Phoneb (n = 31) | 0.02 (0.01; 0.00, 0.09) |
| Total cost per session (n = 18) | 1.01 (0.73; 0.15, 2.60) |
| Clinic DOT (n = 87) | |
| Travel time, round trip (n = 84) | 17.99 (11.12; 2.57, 80.99) |
| Travel out-of-pocket cost (n = 73) | 6.63 (4.27; 0.00, 30.97) |
| Coordination timec (n = 87) | 0.09 (0.00; 0.00, 0.76) |
| DOT time costd (n = 87) | 2.52 (2.48; 0.64, 5.78) |
| Dependent caree (n = 87) | 1.65 (0.00; 1.63, 13.50) |
| Total cost per session (n = 71) | 37.18 (21.71; 5.28, 196.20) |
| Net enablerf (n = 71) | 33.98 (18.50; 2.07, 193.00) |
| Field DOT (n = 87) | |
| DOT time costd (n = 87) | 2.43 (2.39; 0.61, 5.57) |
| Coordination timec (n = 87) | 0.09 (0.00; 0.00, 0.76) |
| Total cost per session (n = 87) | 2.52 (2.39; 0.61, 6.49) |
Note. VDOT = video DOT. Costs adjusted for purchase power parity (PPP).
Total cost divided by 114 doses on VDOT. Individual costs may not sum to total cost due to skewedness of data and number of responses (see “Calculation of Total Cost per Dose in Table 3” in the Appendix, available as a supplement to the online version of this article at http://www.ajph.org).
In our sample, 89.5% of patients used their own phone.
Coordination time is the amount of time spent before a DOT session contacting a health department worker. Forty-nine percent of patients reported coordination time greater than zero.
Clinic and field DOT time estimated from health department staff DOT times.
Fifteen percent of patients reported needing dependent care for family members at home during their clinic visit. Dependent care valued at $15 per hour.
New York City and San Francisco offered enabler and incentives for coming into the clinic of $5.50 and $7.20, respectively. We adjusted this subsidy for PPP, then averaged across 3 sites, and subtracted from total patient cost.
The largest patient cost associated with VDOT was patient DOT time, at $1.12 (range = $0.11–$4.36) and $0.95 (range = $0.17–$2.63) for VDOT recorded and VDOT live, respectively.
Before a patient’s session, 48% (39/82) of patients stated that they contacted health department staff by phone and 7% (6/83) by text message. Eighteen percent (15/85) of patients reported needing dependent care when traveling to the clinic. Patients reported a median of 3 hours of dependent care per clinic session (range = 1.5–13.5 hours). Furthermore, 10 of 86 patients (12%) reported a technical issue with their most recent VDOT dose. Five patients reported that the problem was immediately resolved, and the remaining 5 patients reported between 12 hours and 3 days to resolve a technical issue. Sites reported that the greatest proportion of technical issues were related to Internet connectivity.
Total patient costs for live VDOT, recorded VDOT, field DOT, and clinic DOT were $1.01 (2.5 and 97.5 percentile = $0.15, $2.60), $1.10 (2.5 and 97.5 percentile = $0.12, $5.97), $2.52 (2.5 and 97.5 percentile = $0.61, $6.49), and $33.98 (2.5 and 97.5 percentile = $2.07, $193.00), respectively.
Societal Costs
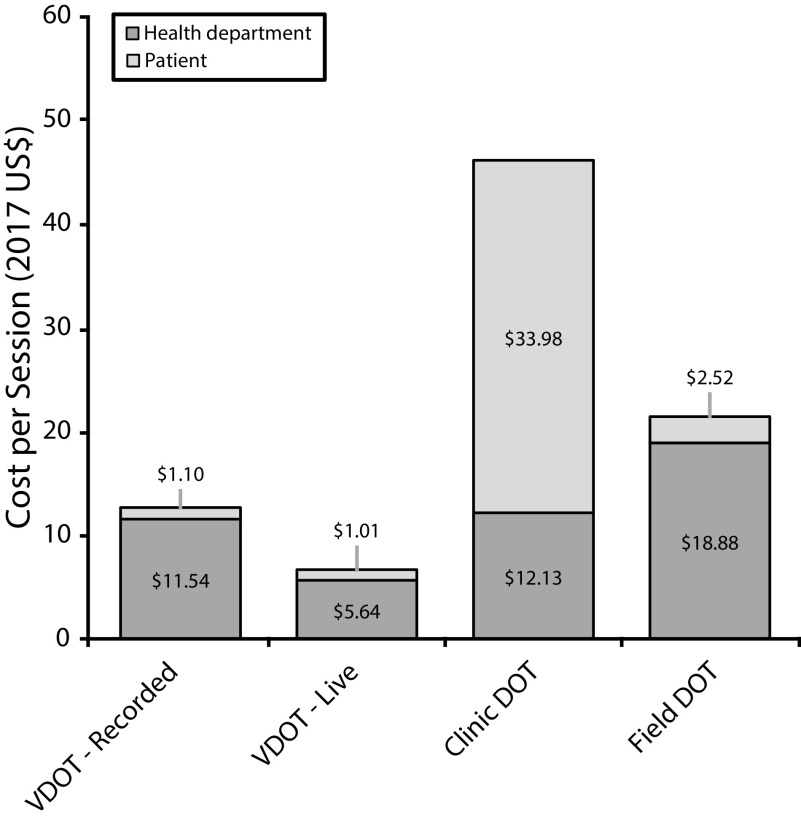
Societal per-session costs (health department + patient costs) were lower for both types of VDOT (live: $6.65 per session and recorded: $12.64) when compared with traditional DOT (clinic DOT: $46.11 and field DOT: $21.40; Figure 1).
FIGURE 1—
Average Total Cost per Session by Directly Observed Therapy (DOT) Type: New York City; San Francisco, CA; and Rhode Island; 2017–2018
Note. VDOT = video DOT. Site costs adjusted using Bureau of Economic Analysis, Regional Purchase Price Deflator (Index = 100).
In this sample, 56% of recorded VDOT sessions were recorded outside of traditional work hours (9 am to 5 pm), as opposed to live VDOT, in which only 5% of sessions were conducted outside work hours (Appendix Figure B).
DISCUSSION
This analysis provides estimates of both health department and patient costs for 4 DOT methods using data from programmatic settings, in which program implementation was not altered. We found that both live and recorded video DOT had lower total societal costs when compared with in-person DOT. Patient costs were highest for clinic DOT and lowest for live VDOT. When we compared our cost estimates with published reports, our estimates included a diverse set of sites (varying TB case counts), more costs associated with field DOT (e.g., vehicle insurance, depreciation, maintenance, and parking), and patient costs. From the health department perspective, these results align with previous reports that, on average, VDOT is less costly, although, in our analysis, Rhode Island’s VDOT cost was not statistically different from field DOT.14,27
Our analysis of data from Rhode Island illustrated that VDOT costs may not always be lower than traditional forms of DOT for health departments. New York City and San Francisco, with more TB patients, reduced VDOT fixed costs by spreading cost over a greater number of patients, and because of their size have greater ability to negotiate costs with vendors. In Rhode Island, the amount of staff time saved by using VDOT recorded as compared with field DOT amounted to 22 minutes per session, or 42 hours over the entire course of treatment. Thus, for low-TB-incidence settings, integrating VDOT fixed costs (e.g., equipment and software purchasing) across multiple localities could enable state health departments to take advantage of economies of scale, reducing cost per session.
This evaluation drew attention to some differences between recorded and live VDOT. First, recorded VDOT allows both the patient and health department staff to schedule recorded VDOT at their own convenience, lowering scheduling costs. Recorded VDOT software also offered administrative and tracking features (e.g., integration of patient data with electronic medical record and surveillance systems) not available with live VDOT; however, the benefits of these features were not included in our calculations. Finally, recorded VDOT allows for daily dosing with observed doses on weekends, an option that is not feasible without health department staff being available on weekends for live VDOT, clinic DOT, or field DOT.
Future evaluations could explore these differences further and assess for variations from the perspective of patients. While VDOT was associated with the lowest patient cost, there may be differences in patients’ satisfaction when compared with traditional DOT.28–30 Within our sample, 12% reported a technical problem with their most recent VDOT dose. Of those who experienced an issue, half had their problem resolved immediately. Most technical issues were associated with difficulty in uploading videos. As health departments and patients become more acquainted with VDOT software and the software is improved, technical issues will likely decrease.
Limitations
Because our sample data are reflective of the 3 sites and differ from national data, the results should be interpreted with care. We note that in San Francisco, clinic DOT was conducted by higher-paid staff than those conducting field DOT. Also, although the prorated cost of patients’ phones was minimal, access to a smartphone could be a barrier for some patients with TB. In our sample, New York City was able to loan phones to patients; however, some health departments may not be able to absorb this additional cost.
Our evaluation was also limited because we were not able to quantify costs associated with time spent gaining approval to initiate a VDOT program (e.g., approval from contracts, information technology, and legal departments), nor were we able to quantify the efficiency of being able to view multiple videos sequentially (recorded VDOT). In our sample, 69% of employed patients reported their income; while we were able to approximate the remaining patient incomes from reported job title and industry, this approximation may differ from actual income. In addition, we may have underestimated the value of time for patients who were unemployed or in school, biasing our patient cost estimates downward.
Furthermore, our analysis did not include patient adherence; previously published studies in New York City found that adherence to scheduled VDOT was better than that with traditional forms of DOT (95% vs 91%) and that treatment completion between the 2 groups was not statistically different (96% vs 97%).15 In California, another study found that VDOT adherence to scheduled doses was better than that with traditional DOT (93% vs 66.4%).14
Conclusions
Applications of telemedicine are evolving and expanding quickly.14,27–30 Currently, recorded VDOT has been implemented by providers for hepatitis C treatment and methadone treatment for drug overdose prevention.31 While live VDOT is currently reimbursable by many insurance plans, the use of recorded videos in treatment of patients is a relatively new health management strategy, and, with few exceptions, has not been reimbursable. Moving forward, the Centers for Medicare and Medicaid Services’ 2019 physician’s fee schedule includes 2 newly defined physicians’ services that use communication technology.32 These codes allow Medicare billing by physicians and federally qualified health centers for live and recorded VDOT. According to the physician fee schedule, the code G2010 allows billing for review of “remote image by patient” and an average $12.91 reimbursement per session.33 Patients may need to pay a copay depending on their health insurance and provider, and these costs are not reimbursed. Given our 3-site average cost of $11.54 per recorded VDOT session, it appears that the Medicare reimbursement is slightly greater than the health department cost of providing the service. Regardless of the actual reimbursement rate, VDOT has the potential to reduce health department and patient costs.
ACKNOWLEDGMENTS
This evaluation was funded by the Centers for Disease Control and Prevention (CDC) through the Combatting Antibiotic Resistant Bacteria mechanism, Cooperative Agreement PS-151501.
We acknowledge Andrew Vernon and Richard Garfein for guidance and technical support during the evaluation.
Note. References in this article to any specific commercial products, process, service, manufacturer, or company does not constitute its endorsement or recommendation by the US government or CDC. The findings and conclusions are those of the authors and do not necessarily represent the official views of the CDC.
CONFLICTS OF INTEREST
The authors report no conflicts of interest relevant to this article.
HUMAN PARTICIPANT PROTECTION
The institutional review boards at the CDC, the New York City Department of Health and Mental Hygiene, the San Francisco Department of Health, and the Rhode Island Department of Health determined this evaluation to be nonresearch.
REFERENCES
- 1.Winston CA, Mitruka K. Treatment duration for patients with drug-resistant tuberculosis, United States. Emerg Infect Dis. 2012;18(7):1201–1202. doi: 10.3201/eid1807.120261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nahid P, Dorman SE, Alipanah N et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis. 2016;63(7):e147–e195. doi: 10.1093/cid/ciw376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nahid P, Mase SR, Migliori GB Treatment of drug-resistant tuberculosis. An official ATS/CDC/ERS/IDSA clinical practice guideline [erratum in Am J Respir Crit Care Med . 2020;201(4):500–501]. Am J Respir Crit Care Med . 2019;200(10):e93–e142. [DOI] [PMC free article] [PubMed]
- 4.Centers for Disease Control and Prevention. TB incidence in the United States, 1953–2017. 2018. Available at: https://www.cdc.gov/tb/statistics/tbcases.htm. Accessed November 27, 2018.
- 5.Menzies NA, Cohen T, Hill AN et al. Prospects for tuberculosis elimination in the United States: results of a transmission dynamic model. Am J Epidemiol. 2018;187(9):2011–2020. doi: 10.1093/aje/kwy094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Himmelstein DU, Woolhandler S. Public health’s falling share of US health spending. Am J Public Health. 2016;106(1):56–57. doi: 10.2105/AJPH.2015.302908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dela Cruz CS, Lyons PG, Pasnick S et al. Treatment of drug-susceptible tuberculosis. Ann Am Thorac Soc. 2016;13(11):2060–2063. doi: 10.1513/AnnalsATS.201607-567CME. [DOI] [PubMed] [Google Scholar]
- 8.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Story A, Aldridge RW, Smith CM et al. Smartphone-enabled video-observed versus directly observed treatment for tuberculosis: a multicentre, analyst-blinded, randomised, controlled superiority trial. Lancet. 2019;393(10177):1216–1224. doi: 10.1016/S0140-6736(18)32993-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeMaio J, Schwartz L, Cooley P, Tice A. The application of telemedicine technology to a directly observed therapy program for tuberculosis: a pilot project. Clin Infect Dis. 2001;33(12):2082–2084. doi: 10.1086/324506. [DOI] [PubMed] [Google Scholar]
- 11.Krueger K, Ruby D, Cooley P et al. Videophone utilization as an alternative to directly observed therapy for tuberculosis. Int J Tuberc Lung Dis. 2010;14(6):779–781. [PubMed] [Google Scholar]
- 12.Mirsaeidi M, Farshidpour M, Banks-Tripp D, Hashmi S, Kujoth C, Schraufnagel D. Video directly observed therapy for treatment of tuberculosis is patient-oriented and cost-effective. Eur Respir J. 2015;46(3):871–874. doi: 10.1183/09031936.00011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holzman SB, Zenilman A, Shah M. Advancing patient-centered care in tuberculosis management: a mixed-methods appraisal of video directly observed therapy. Open Forum Infect Dis. 2018;5(4):ofy046. doi: 10.1093/ofid/ofy046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garfein RS, Liu L, Cuevas-Mota J et al. Tuberculosis treatment monitoring by video directly observed therapy in 5 health districts, California, USA. Emerg Infect Dis. 2018;24(10):1806–1815. doi: 10.3201/eid2410.180459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chuck C, Robinson E, Macaraig M, Alexander M, Burzynski J. Enhancing management of tuberculosis treatment with video directly observed therapy in New York City. Int J Tuberc Lung Dis. 2016;20(5):588–593. doi: 10.5588/ijtld.15.0738. [DOI] [PubMed] [Google Scholar]
- 16. May 2017 national occupational employment and wage estimates. Washington, DC: US Bureau of Labor Statistics; 2018.
- 17. Global smartphone average sales price sees record year-on-year growth in 4Q17. Nuremberg, Germany: GfK; 2018.
- 18. Your driving costs: how much are you really paying to drive? Heathrow, FL: American Automobile Association; 2017.
- 19. Centers for Disease Control and Prevention. Self-study module 6: managing tuberculosis patients and improving adherence. Atlanta, GA: Division of Tuberculosis Elimination; 2014.
- 20. Annual retail gasoline and diesel prices by locality. Washington, DC: US Energy Information Administration; 2019.
- 21.Grosse SD, Krueger KV, Pike J. Estimated annual and lifetime labor productivity in the United States, 2016: implications for economic evaluations [erratum in J Med Econ. J Med Econ. 2019;22(6):612. doi: 10.1080/13696998.2018.1542520. 2019;22(6):501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2019.
- 23.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 24. emocha. Baltimore, MD: emocha Mobile Health; 2019.
- 25. SureAdhere. San Diego, CA: SureAdhere Mobile Technology; 2019.
- 26. Skype for Business. Redmond, WA: Microsoft; 2019.
- 27.Lam CK, Fluegge K, Macaraig M, Burzynski J. Cost savings associated with video directly observed therapy for treatment of tuberculosis. Int J Tuberc Lung Dis. 2019;23(11):1149–1154. doi: 10.5588/ijtld.18.0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garfein RS, Collins K, Munoz F et al. Feasibility of tuberculosis treatment monitoring by video directly observed therapy: a binational pilot study. Int J Tuberc Lung Dis. 2015;19(9):1057–1064. doi: 10.5588/ijtld.14.0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gassanov MA, Feldman LJ, Sebastian A, Kraguljac MJ, Rea E, Yaffe B. The use of videophone for directly observed therapy for the treatment of tuberculosis. Can J Public Health. 2013;104(3):e272. doi: 10.17269/cjph.104.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salerno M, Reaves M, Dias M Comparing electronic directly observed therapy with in-person DOT: patients’ perspectives. Presented at: The 49th Union World Conference on Lung Health; October 2018; The Hague, The Netherlands.
- 31.Johnson CK. Selfie medicine: phone apps push people to take their pills. Associated Press. March 28, 2018. Available at: https://apnews.com/189668d9268243b2921a6a0764ddd511/Selfie-medicine:-Phone-apps-push-people-to-take-their-pills. Accessed August 19, 2020.
- 32. Final policy, payment, and quality provisions changes to the Medicare physician fee schedule for calendar year 2019. Baltimore, MD: Centers for Medicare and Medicaid Services; 2019.
- 33. Physician fee schedule. Baltimore, MD: Centers for Medicare and Medicaid Services; 2019.