Abstract
Objectives. To identify body mass index (BMI) trajectories in Chinese children and to compare the risk of incident high blood pressure (HBP) across trajectory groups.
Methods. A total of 9286 children were included. The mean age at baseline was 8.9 years; age at endpoint ranged between 16 and 18 years. At least 8 measurements were obtained from each involved child. We used group-based trajectory modeling to identify BMI trajectory groups in each sex. We used blood pressure from each measurement to define HBP.
Results. We identified 4 BMI trajectories for each sex. Compared with the low trajectory group, the hazard ratios of HBP in the higher trajectory groups ranged from 1.17 (95% confidence interval [CI] = 1.11, 1.23) to 2.00 (95% CI = 1.78, 2.27) during follow-up, and HBP risk at late adolescence ranged from 1.36 (95% CI = 1.22, 1.52) to 3.63 (95% CI = 3.12, 4.21). All trend P values across trajectories were less than .001. In terms of population level, overweight started 3 years earlier than HBP.
Conclusions. Children of higher BMI trajectories had a higher risk of HBP during adolescence. The transition period from overweight to HBP onset could be critical for HBP prevention.
High blood pressure (HBP) and hypertension have brought a heavy burden to global public health in recent decades,1,2 and the situation is increasingly severe in Southeast Asia.3–5 Childhood obesity is a well-documented risk factor for adulthood hypertension.6–8 In China, prevalence of overweight and obesity among children aged 7 to 17 years has increased from 4.8% in 1995 to 18.4% in 2014,9 and has become an alarming issue in public health.10 Although body mass index (BMI) is widely acceptable to evaluate children’s weight status and related disease risk, a simple classification of overweight and obesity by BMI in 1 visit may not be sufficient to explain HBP risk in later life.
To better understand the effect of childhood BMI on disease risk in later life, the BMI trajectory during childhood has been drawing researchers’ attention. Different from the BMI in a single or limited number of measurements, BMI trajectories help to capture the dynamic change of BMI within a certain time period.11 Because of the rapid change of BMI during adolescence, study of BMI trajectories may provide more information on the association between BMI and risk of HBP.
Buscot et al.12 found that compared with children with a normal, stable BMI trajectory, children of worsening or persisting obesity were generally associated with an increased risk of cerebrovascular disease in their early adulthood. A study in young adults aged 20 to 35 years also found that a higher-than-normal level of BMI trajectory was associated with increased hypertension risk.13 However, as a considerable number of studies have proven that the roots of hypertension in adulthood could extend back into childhood,14 understanding the relationship between adolescent BMI trajectories and hypertension in late adolescence is necessary for the early stage of disease control and for early primary and secondary prevention of hypertension.
By using annually repeated BMI measurements from the age of 7 to 18 years among children and adolescents in Guangdong, China, this study aimed to identify various modes of BMI trajectories during adolescence, to compare incidence rates of HBP between different BMI trajectories during the follow-up period, and to estimate the interval between overweight onset and HBP onset.
METHODS
The data in this study came from the Zhongshan school physical examination database between 2006 and 2016. All of the measurements were conducted by qualified medical physicians from medical establishments. In the present study, 78 428 measurements from 9286 participants with normal blood pressure at baseline, when they had their physical examination at primary school (mainly in 2006–2008) for the first time, were included. The endpoint was defined as the time of the last physical examination for each participant, which mainly happened during high school. At least 8 measurements were obtained from each participant; therefore, the quality of model fit on BMI trajectories was relatively good.
Measurements
Participants’ sex and date of birth were collected at their first physical examination in primary school and were recorded in the school register system along with the date of the examination. The age at each follow-up examination was calculated as (date of examination – date of birth)/365.25.
Height was measured using the portable stadiometer (model TZG, Jiangyin No. 2 Medical Equipment Factory, Jiangsu Province, China) to the nearest 0.1 centimeter, with students standing straight and barefoot. Weight was measured with a lever type weight scale (model RGT-140, Shanghai Dachuan Electronic Weighing Apparatus Co Ltd, Shanghai, China) to the nearest 0.1 kilogram while children were wearing undergarments. BMI was calculated as weight in kilograms divided by the square of height in meters. Overweight and thinness were defined as age- and sex-specific BMI z scores of greater than or equal to 1 or less than −2, while stunting was defined as height-for-age z scores less than −2, according to the World Health Organization (WHO) growth reference.15
Blood pressure was measured consistent with the recommendation of 2017 Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children (2017 Guideline).16 Mercury sphygmomanometers (model XJ11D, Shanghai Medical Instruments Co Ltd, Shanghai, China), stethoscopes (model TZ-1, Shanghai Medical Instruments Co Ltd, Shanghai, China), and appropriate cuffs were used for the measurement. Participants were asked to sit quietly for at least 5 minutes before the first reading. Systolic blood pressure (SBP) was determined by onset of the first Korotkoff sound and diastolic blood pressure (DBP) was determined by the fifth Korotkoff sound. Blood pressure was measured twice with a 5-minute gap between the 2 measurements from the right arm. If the difference between 2 measurements was 10 millimeters of mercury or higher (mm Hg; either SBP or DBP), an extra measurement would be conducted until the difference between the last 2 measurements was less than 10 mm Hg.
The average of SBP and DBP values were calculated, respectively. HBP is defined as blood pressure greater than or equal to the 95th percentile for children younger than 13 years, and blood pressure greater than or equal to 130/80 mm Hg for children aged 13 years or older, according to the 2017 Guideline.16 Blood pressure outcome at late adolescence indicates the last blood pressure measurement of each involved child, which occurred between the ages of 16 and 18 years. Follow-up time was defined as the time period between the first and the last physical examination.
Students’ residential area was recorded as urban or rural based on their household register card (Hukou booklet) and collected from their guardians. The division of urban and rural residential records was based on the statistical division and code of urban and rural division from the National Bureau of Statistics.
All measurements had been logically checked before being recorded into the system and the examination results were returned to the parents. After careful recheck of the database, no biologically implausible values were identified and excluded in the present analysis.
Statistical Analysis
We used a Stata plugin for group-based trajectory modeling (GBTM) developed by Bobby Jones to identify different trajectory groups of BMI over the ages from 7 to 18 years.17 We modeled trajectories with a censored normal distribution by sex with following steps.18 First, we conducted a 1-trajectory model to determine whether shapes of BMI trajectories were linear, quadratic, or cubic according to the Bayesian information criteria (BIC). Second, we increased the number of trajectory groups in the model by 1 and the repeated steps until we found the best-fit model. We based model selection mainly on the absolute value of BIC. However, we modified it by (1) BIC decreased by at least 20, (2) high mean posterior probability greater than 0.7, and (3) the odds of correct classification based on the posterior probabilities of group membership greater than 5 for each group.11,19 To maintain an adequate sample size of each group, we performed models with 2 to 5 classes in the current study.13 As we were aware that the BMI trajectory could have sex disparities, we conducted GBTM separately for both sexes. We compared parameters for both sexes, and we based the final decision on the optimal number of trajectory groups on the solution that contained the trajectories common to both sexes, which was cubic trajectories of 4 groups for both sexes. The model came with the minimum BIC absolute value, as well with adequate sample size for each trajectory group and the highest mean posterior probabilities. The results of model fitting process are displayed in Tables A and B (available as supplements to the online version of this article at http://www.ajph.org).
We used Cox parametric survival regression models to estimate the differences on HBP risks among 4 different BMI trajectory groups during follow-up, with the follow-up time set as time variable, and the HBP incidence during follow-up as the outcome. We used log binomial regression models reporting risk ratios, as well as a linear trend test, to analyze the association between BMI trajectory groups and HBP risk in late adolescence, with participants’ last blood pressure measurement set as the outcome. We also estimated the association between the age of overweight onset and HBP risk in late adolescence with a log-binomial regression model. We recruited children’s baseline SBP, baseline age, and urban or rural residence in all adjusted models for the analysis described previously. We calculated age- and sex-specific incident rates and 95% confidence intervals (CIs) of HBP and overweight for each BMI trajectory group.
We performed all analyses with Stata version 14.0 (StataCorp LP, College Station, TX), and we considered the associations to be significant when P was less than .05.
RESULTS
The results of the 4 distinct BMI trajectory groups for each sex are displayed in Figure 1 and are labeled as low (42.7% in boys vs 37.5% in girls), middle (38.2% in boys vs 42.7% in girls), high (14.9% in boys vs 17.0% in girls), and very high (4.2% in boys vs 2.8% in girls). We compared the BMI levels of these trajectories with growth references recommended by WHO. In boys, BMI of the “very high” and “high” trajectories were each higher than WHO cutoffs of obesity and overweight, while that of “middle” trajectory was close to the normal cutoff. In girls, the “very high,” “high,” and “middle” trajectories each coincided with WHO cutoffs of obesity, overweight, and normal. The “low” trajectories in both sexes were between WHO cutoffs of normal and thinness, close to the curve of the BMI z score of −1.
FIGURE 1—
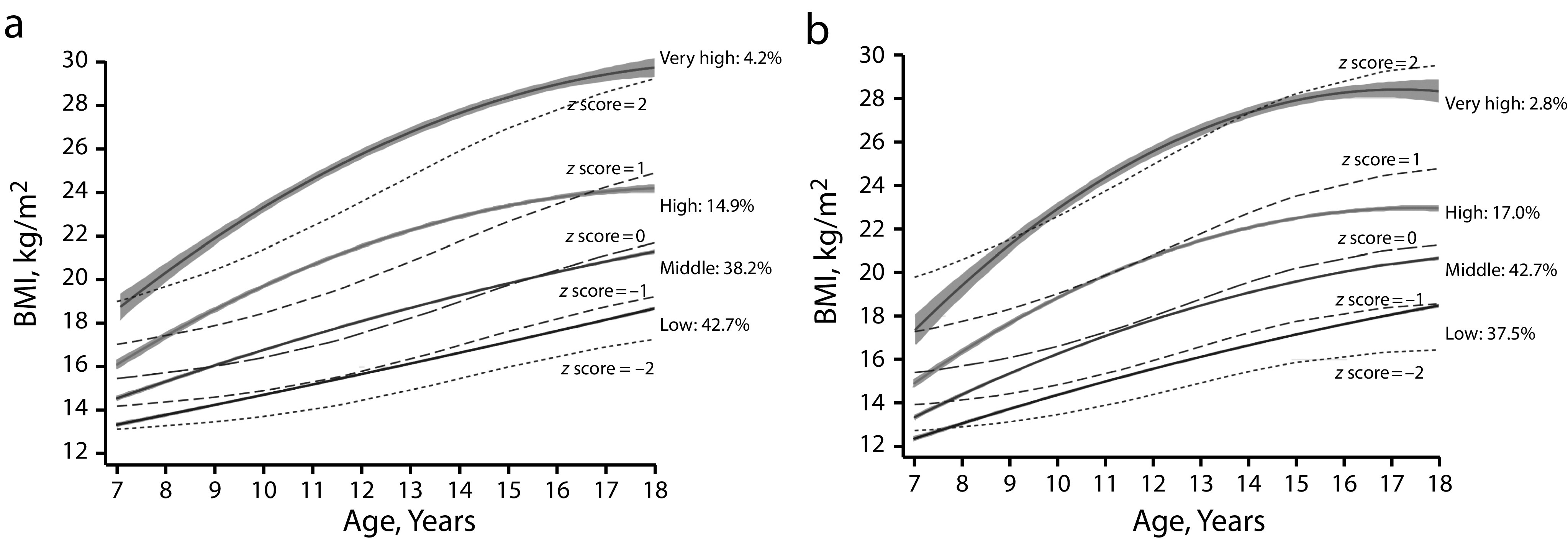
Trajectories of Body Mass Index During Adolescence Compared With the World Health Organization 2007 Growth Reference in Children and Adolescents for (a) Boys and (b) Girls: Guangdong, China, 2006–2016
Note. BMI = body mass index. Solid lines indicate the trajectory groups, while gray shades indicate 95% confidence intervals of each trajectory group. Gray dash lines from bottom to top represent World Health Organization cutoffs for thinness, slim, normal, overweight, and obesity (z score of −2 SD, −1 SD, median, 1 SD, and 2 SD, respectively).15
Table 1 shows the baseline characteristics by trajectory groups. A total of 9286 children were recruited in the present study (50.1% were boys), with an average baseline age of 8.9 (SD = 1.2) years and average follow-up time of 9.0 (SD = 1.0) years. During follow-up, the overall incidence rate of HBP was 6.51 (95% CI = 6.36, 6.65) per 100 person-years. A total of 1569 (16.9%) participants were identified as having HBP at endpoint in their late adolescence. The percentage of participants enrolled at each age is presented in Table C (available as a supplement to the online version of this article at http://www.ajph.org) by BMI trajectory groups.
TABLE 1—
Characteristics of Participants at Baseline and During Follow-Up, by Body Mass Index Trajectory Groups: Guangdong, China, 2006–2016
| Trajectory Group |
|||||
| Variables | Overall | Low | Middlea | High | Very High |
| Number of participants, no. (%) | 9286 | 3 725 (40.1) | 3 754 (40.4) | 1 480 (15.9) | 327 (3.5) |
| Male, no. (%) | 4 650 (50.1) | 1 985 (53.3)** | 1 776 (47.3) | 694 (46.9)** | 195 (59.6)* |
| Urban living, no. (%) | 4 612 (49.7) | 1 698 (45.6)** | 1 894 (50.5) | 846 (57.2)** | 174 (53.2)** |
| Baseline | |||||
| Age, y, mean ±SD | 8.2 ±0.9 | 8.2 ±0.9 | 8.2 ±0.9 | 8.2 ±0.9 | 8.2 ±0.9 |
| BMI, kg/m2, mean ±SD | 15.3 ±2.0 | 14.1 ±0.9** | 15.4 ±1.2 | 17.2 ±1.8** | 20.3 ±2.7** |
| SBP, mm Hg, mean ±SD | 104.6 ±5.5 | 103.9 ±5.5** | 104.7 ±5.4 | 105.6 ±5.4** | 106.5 ±5.4** |
| DBP, mm Hg, mean ±SD | 66.6 ±4.7 | 66.3 ±4.7 | 66.6 ±4.7 | 67.0 ±4.7** | 67.1 ±5.0 |
| Thinness,b no. (%) | 673 (7.2) | 650 (17.5)** | 23 (0.6) | . . . | . . . |
| Stunting,b no. (%) | 539 (5.8) | 318 (8.5)** | 164 (4.4) | 45 (3.0)** | 12 (3.7)* |
| Overweight,b no. (%) | 994 (10.7) | 6 (0.2)** | 126 (3.4) | 570 (38.5)** | 292 (89.3)** |
| Follow-up | |||||
| Years, mean ±SD | 9.0 ±1.0 | 9.1 ±1.0 | 9.0 ±1.0 | 9.0 ±1.0 | 9.1 ±1.1 |
| Average incident HBP/100 person-y (95% CI) | 6.51 (6.36, 6.65) | 5.92 (5.70, 6.14)** | 6.51 (6.28, 6.75) | 7.66 (7.25, 8.08)** | 8.67 (7.76, 9.68)** |
| Total measurement with detected HBP, no. (%) | 18 440 (23.5) | 6 017 (19.3)** | 7 348 (23.1) | 3 840 (30.4)** | 1 235 (44.5)** |
| HBP prevalence at endpoint, no. (%) | 1 569 (16.9) | 452 (12.1)** | 620 (16.5) | 353 (23.9)** | 144 (44.0)** |
| Overweight at endpoint, no. (%) | 770 (8.3) | . . . | 37 (1.0) | 429 (29.0)** | 304 (93.0)** |
Note. BMI = body mass index; CI = confidence interval; DBP = diastolic blood pressure; HBP = high blood pressure; kg/m2 = weight in kilograms divided by the square of height in meters; mm Hg = millimeters of mercury; SBP = systolic blood pressure.
The middle trajectory group was set as the reference.
According to the World Health Organization 2007 growth reference.15
P < .05 compared with the reference group; **P < .01 compared with the reference group.
Table 2 presents the differences of HBP risk among 4 trajectory groups during follow-up and at late adolescence. Compared with middle trajectory group, the hazard ratio of HBP incidence was 0.71 (95% CI = 0.68, 0.74) in low trajectory group, and ranged from 1.44 (95% CI = 1.38, 1.51) to 2.50 (95% CI = 2.35, 2.66) during follow-up; the trend P from lower to higher trajectory groups was less than .001. The HBP risk for participants in higher trajectory groups was also higher at the end of follow-up, with the risk ratios ranging from 1.58 (95% CI = 1.37, 1.83) to 3.98 (95% CI = 3.15, 5.03), and trend P level was less than .001. These results did not differ by sex, and remained consistent after adjustment of participants’ baseline BMI, baseline SBP, and urban or rural living condition. Among those in higher trajectory groups, the earlier they became overweight, the more likely they got HBP at late adolescence (results displayed in Table D, available as a supplement to the online version of this article at http://www.ajph.org). This trend was especially significant in boys.
TABLE 2—
Odds Ratios and 95% Confidence Intervals of High Blood Pressure Risks Among Different Body Mass Index Trajectory Groups: Guangdong, China, 2006–2016
| HBP During Follow-Up, HR (95% CI) |
HBP at Late Adolescence, RR (95% CI) |
|||||
| Trajectory Group | Total | Boys | Girls | Total | Boys | Girls |
| Crude model | ||||||
| Low | 0.71 (0.68, 0.74) | 0.66 (0.63, 0.69) | 0.74 (0.68, 0.81) | 0.70 (0.61, 0.80) | 0.59 (0.51, 0.69) | 0.74 (0.57, 0.98) |
| Middle (Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| High | 1.44 (1.38, 1.51) | 1.49 (1.41, 1.57) | 1.45 (1.32, 1.60) | 1.58 (1.37, 1.83) | 1.71 (1.42, 2.06) | 1.57 (1.18, 2.09) |
| Very high | 2.50 (2.35, 2.66) | 1.96 (1.82, 2.10) | 3.53 (3.10, 4.02) | 3.98 (3.15, 5.03) | 3.55 (2.62, 4.80) | 4.44 (2.89, 6.83) |
| P for trend | < .001 | < .001 | < .001 | < .001 | < .001 | < .001 |
| Adjusted model | ||||||
| Low | 0.83 (0.78, 0.89) | 0.75 (0.70, 0.81) | 0.73 (0.63, 0.85) | 0.73 (0.64, 0.83) | 0.63 (0.54, 0.74) | 0.74 (0.56, 0.98) |
| Middle (Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| High | 1.46 (1.36, 1.56) | 1.71 (1.58, 1.86) | 1.24 (1.07, 1.43) | 1.51 (1.30, 1.75) | 1.66 (1.38, 2.01) | 1.47 (1.10, 1.96) |
| Very high | 2.70 (2.46, 2.97) | 2.33 (2.10, 2.59) | 3.09 (2.53, 3.77) | 3.73 (2.94, 4.73) | 3.32 (2.44, 4.51) | 4.20 (2.71, 6.51) |
| P for trend | < .001 | .001 | < .001 | < .001 | .001 | < .001 |
Note. CI = confidence interval; HBP = high blood pressure; HR = hazard ratio; RR = risk ratio. Baseline systolic blood pressure, baseline age, and living condition (urban or rural) were adjusted in the adjusted model.
Figure 2 presents age-specific incidence rates of HBP by sex and trajectory groups, and the corresponding values and CIs are displayed in Table E (available as a supplement to the online version of this article at http://www.ajph.org). Age-specific incidence rates of overweight are also presented (Table F, available as a supplement to the online version of this article at http://www.ajph.org). The peak age of overweight incidence was 9 years for both sexes, and was around 3 years earlier than the peak age of HBP incidence. The change in HBP incidence rate with age was parabolic in each trajectory group, while higher incidence rates were found in higher BMI trajectory groups.
FIGURE 2—
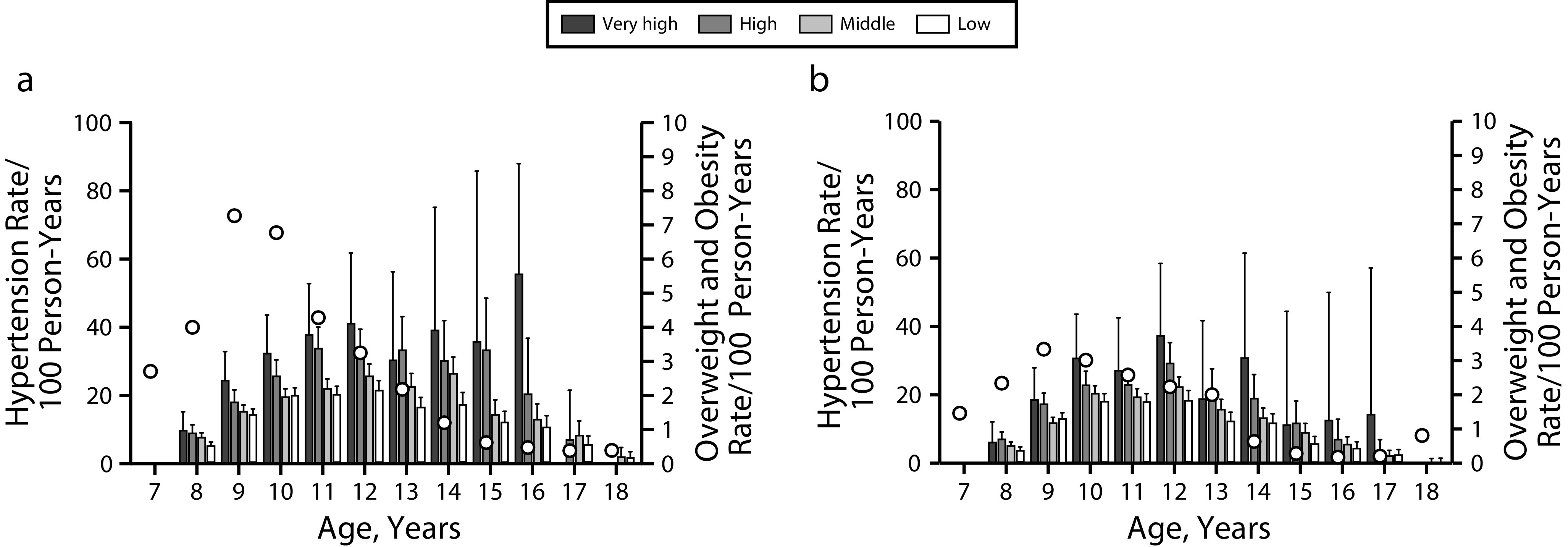
Incident Rates and 95% Confidence Intervals of Hypertension and Incident Rates of Overweight at Each Age, by Trajectory Groups for (a) Boys and (b) Girls: Guangdong, China, 2006–2016
Note. Overweight was defined as age- and sex-specific body mass index z score ≥ 1 according to the World Health Organization 2007 growth reference.15 Bars and error bars stand for incident high blood pressure and 95% confidence intervals for each trajectory group at each age, while circles stand for the incident overweight at each age. The values of bars and error bars are displayed in Table E (available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
In this longitudinal study, with 78 428 measurements from 9286 Chinese children and adolescents, we identified 4 distinct BMI trajectories from ages 7 to 18 years. We estimated the incidence rates of hypertension in participants of different BMI trajectory groups, as well as their association with onset of overweight. We found the group of higher BMI trajectories had higher HBP risk, and the change of HBP incidence rate with age was parabolic in each trajectory group, while we found higher incidence rates in higher BMI trajectory groups. Moreover, the earlier overweight and obesity began, the higher the HBP risk was in late adolescence. The pathway from excessive fat to HBP could be caused by the accumulation of dysfunctional adipose tissue and would take time.20 We found a possible 3-year transition period from overweight onset to HBP onset, which could be a critical window period for intervention. The participants of the present study were from Guangdong, China, which is one of the southernmost provinces. Although people from this part of China have lower BMI than those from northern parts, a previous study found that there was no significant difference in BMI categories and related mortality from cardiovascular diseases between geographical areas.21 Thus, the findings of this study may apply to the general Chinese population.
Various BMI trajectories were detected by different studies11,22–26 when using GBTM to derive sets of growth patterns by grouping children with similar growth patterns.27 The specific number of groups may be related to the age range, follow-up time, and number of participants.13 The present study was one of the first studies to assess the BMI trajectory–related HBP risk in school-aged children, and we identified 4 distinct trajectories of BMI for school-aged children for both sexes. Despite the fact that the overall BMI level in our participants was relatively lower, the trajectories identified in our study were similar to those found in the US National Longitudinal Survey of Youth23 and in the Early Bird cohort in the United Kingdom.25
Previous studies described BMI trajectories from late adolescence to middle age and their related hypertension risk,28–30 which underscored the importance of higher weight and weight gain in increasing the risk of hypertension from young adulthood into later life. From the present study, we have reached a consistent conclusion in school-age children, and additionally detected an early warning period at the age of 9 years, when the overweight incidence reached its peak. These findings illustrated that BMI polarization could start at an early age, and the window period of population-based hypertension prevention could be brought forward to the time before the explosion of overweight. With the premise that earlier start of overweight leads to higher blood pressure in late adolescence, it might be more cost-effective to take prompt actions to control the growth of overweight. Although we found that children with lower BMI trajectories were associated with lower HBP risk, we still recommend that children should keep a moderate, rather than low growth pattern during adolescence, for their comprehensive and healthy development.
Instead of prevalence, we used incidence rates to assess HBP across BMI trajectory groups, which is appropriate for analyzing the rapid change of new cases in a specific population.31 Research focusing on the incidence of HBP in children and adolescents is quite rare. This study may provide new and dynamic insight to the change of HBP in this population by displaying the speed at which new cases of HBP occurred in the population.32 In the present study, we found that there were only a few new HBP cases between the ages of 16 and 18 years in children of higher BMI trajectories; it caused exceptionally large CIs of the estimation, but also warranted that interventions should start before the peak incidence age.
Limitations
There were several limitations about the present study. The major limitation was that the data came from routine school health examinations, and some important risk factors for HBP, such as participants’ race/ethnicity, socioeconomic status, quality of dietary intake, and time of physical activity, were unavailable. As these factors also matter in the development of BMI, we hope to include this relevant information in further studies. In addition, because of the lack of school information, we were unable to perform the analysis accounting for school-level clustering. Although its influence on statistical efficiency could be limited,33 it should be noticed in the generalization of the present study.
Moreover, because of the site conditions of school health examination, blood pressure was defined with the average of 2 measurements from a single time, which makes the reported percentage of children with HBP risk higher than that from other studies with a similar setting. Studies found that only 22% to 56% of the children would remain the same hypertension stage on 3 different occasions.16 According to this percentage, estimated prevalence of hypertension in the participants at endpoint could be 3.7% to 9.5%. This was essentially close to what Song et al. had reported in their study, in which the pooled prevalence in children younger than 19 years was 4.59% (95% CI = 3.24%, 6.15%)34 and was close to domestic data with prevalence of 8.9% to 11.8% (data not published in English). White-coat hypertension could also have contributed to the high proportion of HBP, because children would get nervous during physical examinations. However, because of the limitations of the data, we could not further explore the specific reason for the high HBP prevalence in the present study and how each reason affected the results.
Second, when assessing the influence of overweight onset on HBP risk, we were unable to differentiate the participants who returned to a normal BMI level from those who were consistently overweight. Meanwhile, as children’s blood pressure fluctuates during adolescence, the hypertensive children may become normotensive later. With the possibility of misclassification bias from these conditions, the effect of BMI trajectories and overweight onset age would be underestimated,35 and the actual influence may be more significant than what we observed. Further studies with the continuous change of BMI and blood pressure could provide stronger evidence for the association found in the present study. Further approaches with more precise evaluation on fat mass and distributions can also be useful.
Third, GBTM is a device for approximating the unknown population distribution of trajectories. From this perspective, the present trajectory groups should not be taken as literally distinct groups but rather as clusters of individuals following approximately the same trajectory. More personalized growth trajectories may need further development for more individualized disease prevention programs.
Public Health Implications
By using longitudinal physical examination data from 9286 Chinese children and adolescents between 2006 and 2016, with a medium follow-up of 9.0 years, we fitted 4 distinct BMI trajectory groups for each sex. Participants with higher BMI trajectories showed an elevated HBP risk, and the earlier start of overweight could be related to increased HBP risk in late adolescence. We additionally detected a key transition period of 3 years from overweight onset to HBP onset, indicating a crucial time for hypertension prevention.
ACKNOWLEDGMENTS
The present research was supported by funding from the National Natural Science Foundation of China (81903344 and 81673192), the Excellent Talents Fund Program of Peking University Health Science Center (BMU2017YJ002), and the Young Researcher Personal Project of Beijing.
The authors would like to acknowledge the hard work by all of the team members and the support from recruited students, teachers, parents, and all of the medical staff who worked on annual physical examinations in Zhongshan, Guangdong.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest in the present study.
HUMAN PARTICIPANT PROTECTION
The use of the present data set has been authorized by Zhongshan Health Care Centers for Primary and Secondary School. All of personal information that could be related to identify the specific child was removed from the data before use. The present analysis has been approved for exemption of ethical application by the institutional review board of Peking University (IRB00001052-20011-免).
Footnotes
See also D’Agostino and Skinner, p. 1599.
REFERENCES
- 1.Wildman RP, Mackey RH, Bostom A, Thompson T, Sutton-Tyrrell K. Measures of obesity are associated with vascular stiffness in young and older adults. Hypertension. 2003;42(4):468–473. doi: 10.1161/01.HYP.0000090360.78539.CD. [DOI] [PubMed] [Google Scholar]
- 2.Samuels J, Bell C, Samuel J, Swinford R. Management of hypertension in children and adolescents. Curr Cardiol Rep. 2015;17(12):107. doi: 10.1007/s11886-015-0661-1. [DOI] [PubMed] [Google Scholar]
- 3.Theodore RF, Broadbent J, Nagin D et al. Childhood to early-midlife dystolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66(6):1108–1115. doi: 10.1161/HYPERTENSIONAHA.115.05831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Noncommunicable diseases in the South-East Asia region: situation and response—2011. New Delhi, India: World Health Organization Regional Office for South East Asia; 2012. [Google Scholar]
- 5.Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S. The burden of blood pressure-related disease: a neglected priority for global health. Hypertension. 2007;50(6):991–997. doi: 10.1161/HYPERTENSIONAHA.107.095497. [DOI] [PubMed] [Google Scholar]
- 6.Lawes CM, Rodgers A, Bennett DA et al. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003;21(4):707–716. doi: 10.1097/00004872-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Woodward M, Barzi F, Martiniuk A et al. Cohort profile: the Asia Pacific Cohort Studies Collaboration. Int J Epidemiol. 2006;35(6):1412–1416. doi: 10.1093/ije/dyl222. [DOI] [PubMed] [Google Scholar]
- 8.Suglia SF, Clark CJ, Gary-Webb TL. Adolescent obesity, change in weight status, and hypertension: racial/ethnic variations. Hypertension. 2013;61(2):290–295. doi: 10.1161/HYPERTENSIONAHA.111.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong Y, Ma J, Song Y et al. Secular trends in blood pressure and overweight and obesity in Chinese boys and girls aged 7 to 17 years from 1995 to 2014. Hypertension. 2018;72(2):298–305. doi: 10.1161/HYPERTENSIONAHA.118.11291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y, Mi J, Shan XY, Wang QJ, Ge KY. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond). 2007;31(1):177–188. doi: 10.1038/sj.ijo.0803354. [DOI] [PubMed] [Google Scholar]
- 11.Tu AW, Mâsse LC, Lear SA, Gotay CC, Richardson CG. Body mass index trajectories from ages 1 to 20: results from two nationally representative Canadian longitudinal cohorts. Obesity (Silver Spring) 2015;23(8):1703–1711. doi: 10.1002/oby.21158. [DOI] [PubMed] [Google Scholar]
- 12.Buscot MJ, Thomson RJ, Juonala M et al. Distinct child-to-adult body mass index trajectories are associated with different levels of adult cardiometabolic risk. Eur Heart J. 2018;39(24):2263–2270. doi: 10.1093/eurheartj/ehy161. [DOI] [PubMed] [Google Scholar]
- 13.Fan B, Yang Y, Dayimu A et al. Body mass index trajectories during young adulthood and incident hypertension: a longitudinal cohort in Chinese population. J Am Heart Assoc. 2019;8(8):e011937. doi: 10.1161/JAHA.119.011937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Urbina EM, Khoury PR, Bazzano L et al. Relation of blood pressure in childhood to self-reported hypertension in adulthood. Hypertension. 2019;73(6):1224–1230. doi: 10.1161/HYPERTENSIONAHA.118.12334. doi: 10.1161/HYPERTENSIONAHA.118.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Onis M. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flynn JT, Kaelber DC, Baker-Smith CM et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 17.Jones BL, Nagin D. A Stata plugin for estimating group-based trajectory models. Pittsburgh, PA: Carnegie Mellon University; 2018. [DOI] [Google Scholar]
- 18.De Onis M. WHO child growth standards based on length/height, weight and age. Acta Paediatr. 2010;95(suppl 450):76–85. doi: 10.1080/08035320500495548. [DOI] [PubMed] [Google Scholar]
- 19.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6(1):109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 20.Pausova Z. From big fat cells to high blood pressure: a pathway to obesity-associated hypertension. Curr Opin Nephrol Hypertens. 2006;15(2):173–178. doi: 10.1097/01.mnh.0000214775.42103.a5. [DOI] [PubMed] [Google Scholar]
- 21.Gu D, He J, Duan X et al. Body weight and mortality among men and women in China. JAMA. 2006;295(7):776–783. doi: 10.1001/jama.295.7.776. [DOI] [PubMed] [Google Scholar]
- 22.Hsu AS. Consequences of Different BMI Trajectories During Childhood and the Protective and Risk Effects of Parental Factors. Dissertation. University of California Irvine; 2017. Available at: https://escholarship.org/uc/item/3m90x0bv. Accessed August 20, 2019. https://doi.org/10.1016/j.mser.2008.09.002.
- 23.Nonnemaker JM, Morgan-Lopez AA, Pais JM, Finkelstein EA. Youth BMI trajectories: evidence from the NLSY97. Obesity (Silver Spring) 2009;17(6):1274–1280. doi: 10.1038/oby.2009.5. [DOI] [PubMed] [Google Scholar]
- 24.Huang DYC, Lanza HI, Wright-Volel K, Anglin MD. Developmental trajectories of childhood obesity and risk behaviors in adolescence. J Adolesc. 2013;36(1):139–148. doi: 10.1016/j.adolescence.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mostazir M, Jeffery A, Voss L, Wilkin T. Childhood obesity: evidence for distinct early and late environmental determinants a 12-year longitudinal cohort study (EarlyBird 62) Int J Obes (Lond) 2015;39(7):1057–1062. doi: 10.1038/ijo.2015.248. doi: 10.1038/ijo.2015.248. [erratum in Int J Obes (Lond). 2016;40(2):380. ] [DOI] [PubMed] [Google Scholar]
- 26.Chen TA, Baranowski T, Moreno JP et al. Obesity status trajectory groups among elementary school children. BMC Public Health. 2016;16(1):526. doi: 10.1186/s12889-016-3159-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2(1):302–317. doi: 10.1111/j.1751-9004.2007.00054.x. [DOI] [Google Scholar]
- 28.Shihab HM, Meoni LA, Chu AY et al. Body mass index and risk of incident hypertension over the life course: the Johns Hopkins Precursors Study. Circulation. 2012;126(25):2983–2989. doi: 10.1161/CIRCULATIONAHA.112.117333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Attard SM, Herring AH, Howard AG, Gordon-Larsen P. Longitudinal trajectories of BMI and cardiovascular disease risk: the National Longitudinal Study of Adolescent Health. Obesity (Silver Spring) 2013;21(11):2180–2188. doi: 10.1002/oby.20569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang M, Zhao Y, Sun H et al. Effect of dynamic change in body mass index on the risk of hypertension: results from the Rural Chinese Cohort Study. Int J Cardiol. 2017;1(238):117–122. doi: 10.1016/j.ijcard.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 31.Alexander LK, Lopes B, Ricchetti-Masterson K, Yeatts KB. ERIC Notebook. 2nd ed. University of North Carolina at Chapel Hill Gillings School of Global Public Health, Department of Epidemiology; 2015. Incident vs. prevalent cases and measures of occurrence. Available at: https://sph.unc.edu/files/2015/07/nciph_ERIC1.pdf. Accessed September 17, 2019. [Google Scholar]
- 32.Principles of Epidemiology in Public Health Practice. An Introduction to Applied Epidemiology and Biostatistics. Vol. 11. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [DOI] [Google Scholar]
- 33.Daniels MJ, Dominici F, Zeger S. Underestimation of standard errors in multi-site time series studies. Epidemiology. 2004;15(1):57–62. doi: 10.1097/01.ede.0000092721.00997.f7. [DOI] [PubMed] [Google Scholar]
- 34.Song P, Zhang Y, Yu J et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. 2019;173(12):1–10. doi: 10.1001/jamapediatrics.2019.3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Copeland KT, Checkoway H, McMichael AJ, Holbrook RH. Bias due to misclassification in the estimation of relative risk. Am J Epidemiol. 1977;105(5):488–495. doi: 10.1093/oxfordjournals.aje.a112408. [DOI] [PubMed] [Google Scholar]


