Abstract
Background:
Synoptic operative reports (SOR) are more accurate than dictated operative reports (DOR) in a few single institution experiences. We sought to examine the completeness of SOR for laparoscopic cholecystectomy (LC) and pancreaticoduodenectomy (PD) in a multi institutional pilot study.
Methods:
Six institutions participated in SOR submission via a web-based survey. One institution collected DOR and case matched historical dictated operative reports (HOR) for subset analysis. A checklist evaluated completeness of all reports. A post-survey assessed participant opinions.
Results:
40 PD SORs were 98.5% complete and 35 LC SORs were 99.7% complete. Single institution subset analysis respective percent complete were: 11 PD SORs 99%, DORs 70% and HORs 74% and 14 LC SORs 99.7%, DORs 76%, and HORs 75%. Post-survey results yielded 10 PD and 24 LC responses. An overwhelming majority agreed that SOR were easy to use and would prefer to use SOR compared to DOR.
Conclusion:
SOR are more complete than both study associated DOR and HOR. The majority of surgeons indicated their preference for SOR and their willingness to use them.
Introduction
Traditionally, surgeons or their delegates document the details of an operation using dictation, templates, or, increasingly rare, hand written notes. These reports are essential to documentation in the patient’s medical record and contribute valuable information to healthcare professional communication, billing, quality assurance, and research (1-4). Review of the literature demonstrates that significant aspects of the operation are commonly missed and clinically relevant details are often omitted in traditional operative reports (5-10). In addition, there is a dramatic improvement in time to appearance in the medical record with concordant decrease in transcription costs associated with electronic templated reports (5). Because of this, synoptic operative reporting has been proposed for use as an alternative to dictated reports.
There are three primary formats for documentation of the operative report that have been used, each with their own unique challenges. Templated operative reports are a “one size fits all” approach to documentation that relies on a pre-written template of the standard operation which can then be actively edited by the surgeon to modify any components within the text or template for that operation. Dictated operated reports are a direct result of the surgeon orally documenting the components of the operation for a transcriptionist to then transcribe into an operative report in the medical record. Finally, synoptic operative reports are computer-based forms that are used to describe the findings and details of an operation using predefined components that gather the appropriate information for individual procedures and guide the surgeon to complete each component which is modifiable to each individual operation and requires active entry. A recent publication presented strong evidence that a synoptic operative report for laparoscopic cholecystectomy produced a more accurate document compared to the dictated report (6). This same methodology held true in a publication for a more complex procedure with highly variable data elements, a pancreaticoduodenectomy, at Memorial Sloan Kettering Cancer Center (7).
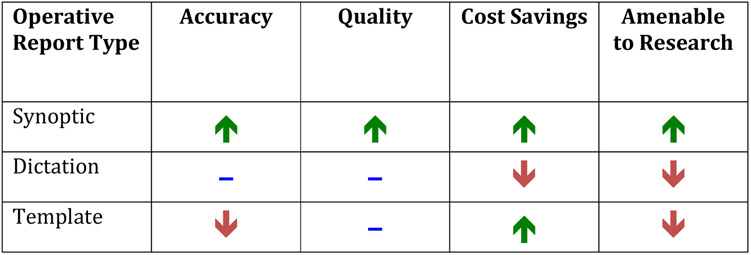
Research supports that synoptic operative reporting increases accuracy, quality, research quality, and efficiency compared to operative reports generated by dictation or templates (Figure 1). Many surgeons and researchers postulate that use of SOR may drive users toward the standard of care and potentially reduce cost (7,8). Most previously conducted studies are single institution and lack heterogeneity as well as reproducibility. No multi-institutional studies have been conducted to test the feasibility of reporting at multiple sites using the same forms. In addition, assessment of surgeon perceptions regarding the adoption of this methodology has not been explored. Additional evidence is needed to support the widespread adoption of synoptic operative reporting. We aimed to assess the completeness of synoptic operative reports compared to dictated operative reports while gaging surgeon feedback on the use of synoptic operative reports.
Figure 1.
Comparison of accuracy, quality, cost savings and ability to aid research and/or quality improvement projects by operative report type.
Materials and methods
This project was reviewed and met criteria as a quality improvement project not requiring human subjects review. A formal determination was provided by the Virginia Mason Medical Center Benaroya Research Institute Institutional Review Board. Synoptic operative report forms were modified and revised from those previously published with good reliability data for both pancreaticoduodenectomy (11) and laparoscopic cholecystectomy (7). The institution that previously developed the pancreaticoduodenectomy SOR participated and assisted with the modifications to the SOR developed for this study design. We recruited six participating institutions for pancreaticoduodenectomy including: Virginia Mason Medical Center, Memorial Sloan Kettering Cancer Center, Methodist Dallas Medical Center, Carolinas Medical Center, Providence Portland and Washington University St. Louis. We recruited six participating institutions for laparoscopic cholecystectomy including: Virginia Mason Medical Center, Barnes Jewish Hospital, Washington University St. Louis, Thomas Jefferson University Hospital, Northshore University Health System, Guthrie Clinic and Winchester Hospital. Lead surgeons at each site served as content experts to review the two report forms and achieve consensus on form components via rounds of editing. Input and support was provided by the Americas Hepatopancreaticobiliary Association (AHPBA) for the PD SOR form and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Safe Laparoscopic Cholecystectomy Task Force for the LC SOR form. The electronic synoptic operative reports for pancreaticoduodenectomy (Appendix 1) and laparoscopic cholecystectomy (Appendix 2) are available for review. It is important to note that SOR ideally should be generated in a way that is interactive. Specifically, as selections are made from multiple choice or drop down menu options, the form automatically adds additional components that are relevant based on that selection. Both developed SOR had these capabilities improve ease of use so that components not applicable to the operation would not be seen by the user. In addition, to address case complexity and/or incorporate additions to the SOR, free text response options titled “brief narrative of the case” and “additional comments” are optional components of every SOR.
Study data were collected and managed using REDCap electronic data capture tools hosted at Virginia Mason Medical Center’s Benaroya Research Institute. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies. A web-based link was provided to the synoptic operative reporting form for pancreaticoduodenectomy and laparoscopic cholecystectomy to all participating institutions. Any surgeon at a participating institution, or their delegate (resident or fellow) performing a pancreaticoduodenectomy or laparoscopic cholecystectomy was asked to complete the form via the link. Surgeons were instructed to complete the form the day of the operation and to still complete their usual form of documentation. Synoptic operative reporting forms were independent from all electronic medical records at participating sites. We chose this approach because integration into the electronic medical record at each participating site would be prohibitive due to time, information technology variation, and medico-legal barriers.
Cases were entered between November 2016 and May 2017. The sponsoring institution, Virginia Mason Medical Center, collected associated dictated operative reports (DOR) for all procedures entered during the SOR collection period with approval from the Institutional Review Board to conduct retrospective chart review. In addition, case matched historical dictated operative reports (HOR) were identified using retrospective chart review for subset analysis. Cases were matched by surgeon, patient age within 10 years, patient gender, indication for surgery, and exact procedure match.
Accuracy was assessed with a checklist assigning 1 point for each component using the developed interactive SOR form as the gold standard. If the component was present, 1 point was given and if missing, no points were given. This process was used to assign point totals for every SOR, DOR and HOR included in the study. Because every procedure included a unique total number of components based on what was done in the procedure, the total points possible was unique to each operation to improve accuracy of the data. For example, if DVT prophylaxis was done, a point would then be possible for documenting the type of DVT prophylaxis given. Study results were, therefore, assessed for percent of data points included, documented as percent complete.
The primary aim of our study was to assess for completeness using the checklist and feasibility. Secondary aims compared percent complete across a subset of SOR, DOR and HOR to determine differences in completeness between the two methods of operative documentation. To determine feasibility, a post-participation survey was designed to gauge ease of use, perception of accuracy, and gather feedback and opinions of participating surgeons. The survey was sent to all participants and results were analyzed using descriptive statistics and thematic analysis.
Results
Pancreaticoduodenectomy
A total of forty pancreaticoduodenectomy synoptic operative reports were entered electronically during the study period. Using our completeness checklist, 98.5% were complete. Single institution subset analysis of percent complete of 11 pancreaticoduodenectomies using the checklist were: SORs 99%, DORs 70% and HORs 74%. Percent complete for all collected operative reports are summarized in Table 1. We found that percent complete for components within the DOR and HOR subset analysis were variable and can be viewed in further detail in Table 2. Within this subset analysis, the percent of frequently missed components for PD were: pre operative stent type (DOR 45%, HOR 71%), resection R0/R1 (DOR 91%, HOR 80%), and pancreatic duct stent placement or not (DOR 73%, HOR 55%) (Figure 2). Brief case narratives were entered for 45% of SORs.
Table 1.
Overall percent complete for synoptic operative reports, dictated operative reports and case matched historical operative reports in both pancreaticoduodenectomies and laparoscopic cholecystectomies.
| SOR n= 40 |
VM SOR n= 11 |
VM DOR n= 11 |
VM HOR n= 11 |
|
|---|---|---|---|---|
| Pancreaticoduodenectomy | 98.5% | 99% | 70% | 74% |
| SOR n= 35 |
VM SOR n= 14 |
VM DOR n= 14 |
VM HOR n= 14 |
|
| Laparoscopic Cholecystectomy | 99.7% | 99.7% | 76% | 75% |
SOR = synoptic operative report, VM = Virginia Mason, DOR = dictated operative report, HOR = historical dictated operative report
Table 2.
Percent complete for pancreaticoduodenectomies for subset analysis of dictated operative reports (DOR) and historical case matched operative reports (HOR).
| DOR | HOR | |
|---|---|---|
| Patient Age | 100% | 91% |
| Gender | 100% | 100% |
| BMI | 0% | 27% |
| Attending | 100% | 100% |
| Assistants | 100% | 100% |
| Procedure | 100% | 100% |
| Indications | 100% | 100% |
| Clinical Stage | 9% | 22% |
| DVT Prophylaxis | 45% | 73% |
| Antibiotics | 45% | 55% |
| ASA | 0% | 0% |
| Risk Factors | 36% | 45% |
| Findings | 91% | 91% |
| History of pancreatitis | 45% | 56% |
| History of cholangitis | 18% | 33% |
| Stent | 73% | 78% |
| Stent location | 55% | 71% |
| Stent type | 55% | 29% |
| Neoadjuvant treatment | 100% | 89% |
| Neoadjuvant type | 100% | 67% |
| Previous cholecystectomy | 82% | 82% |
| Incision location | 100% | 100% |
| Portal vein resection and reconstruction | 100% | 100% |
| Resection (R0/R1) | 9% | 20% |
| Pancreas consistency | 64% | 91% |
| Pancreas duct size | 100% | 82% |
| Biliary duct size | 82% | 55% |
| Pancreatic duct anastomosis type | 100% | 91% |
| Pancreatic duct anastomosis technique | 100% | 100% |
| Pancreatic duct stent placed | 27% | 45% |
| Gastrojejunostomy type | 100% | 100% |
| Drain placed | 91% | 91% |
| Number of drains | 86% | 100% |
| Drain locations | 89% | 80% |
| EBL | 100% | 91% |
| Blood transfusion | 9% | 100% |
| Skin closure | 82% | 100% |
| Sponge/Instrument counts correct | 55% | 82% |
| Complications | 100% | 27% |
Figure 2. Percentage of frequently missed components in pancreaticoduodenectomies.
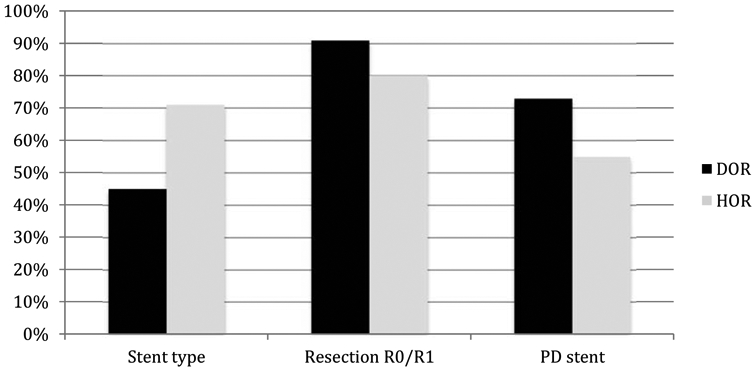
PD = pancreaticoduodenectomy
Laparoscopic Cholecystectomy
A total of 35 laparoscopic cholecystectomy synoptic operative reports were entered electronically during the study period. Using the completeness checklist, 99.7% were complete. Single institution subset analysis of percent complete of 14 LC using the checklist were: SORs 99.7%, DORs 76%, and HORs 75%. Percent complete for all collected operative reports are summarized in Table 1. We found that percent complete for components within the DOR and HOR subset analysis were variable and can be viewed in further detail in Table 3. Within the single institution subset analysis, the percent of frequently missed components for LC were: incomplete critical view of safety description (DOR 39%, HOR 41%), antibiotics given or not (DOR 29%, HOR 50%), documentation of whether counts were correct (DOR 64%, HOR 79%), and the indication for performing an intraoperative cholangiogram if it was done (DOR 50%, HOR 60%) (Figure 3). Brief case narratives were entered for 48.5% of SORs.
Table 3.
Percent complete for laparoscopic cholecystectomies for subset analysis of dictated operative reports (DOR) and historical case matched operative reports (HOR).
| DOR | HOR | |
|---|---|---|
| Patient Age | 86% | 86% |
| Gender | 86% | 86% |
| BMI | 0% | 7% |
| Attending | 100% | 100% |
| Assistants | 100% | 93% |
| Procedure | 93% | 100% |
| Indications | 100% | 100% |
| Operative urgency | 100% | 100% |
| Inpatient or Outpatient | 100% | 100% |
| ASA | 0% | 0% |
| Risk Factors | 0% | 7% |
| DVT prophylaxis | 71% | 50% |
| Antibiotics | 71% | 50% |
| Findings | 100% | 93% |
| Abdominal entry | 100% | 100% |
| Adhesiolysis | 79% | 64% |
| Where was adhesiolysis performed | 88% | 86% |
| Gallbladder (GB) appearance | 100% | 93% |
| Energy devices used | 93% | 86% |
| Conversion to open | 93% | 100% |
| Reason for conversion | 100% | 100% |
| Hepatocystic triangle cleared | 73% | 77% |
| Lower 1/3 of GB separated from cystic plate | 45% | 23% |
| 2 only 2 structures | 64% | 77% |
| Cystic artery clips | 33% | 92% |
| Cystic duct ligation type | 100% | 100% |
| Number of clips | 73% | 86% |
| Bile spillage | 50% | 43% |
| Stone spillage | 43% | 21% |
| Intraoperative cholangiogram (IOC) performed | 100% | 100% |
| Indication for IOC | 50% | 40% |
| IOC findings | 100% | 100% |
| Bag used to remove specimen | 73% | 85% |
| Which port site used to remove specimen | 91% | 100% |
| Drain placed | 100% | 100% |
| Number of drains | 100% | 100% |
| Drain location | 100% | 100% |
| EBL | 57% | 71% |
| Fascial closure | 93% | 100% |
| Skin closure | 100% | 100% |
| Sponge/Instrument counts correct | 36% | 21% |
| Complications | 79% | 79% |
Figure 3. Percentage of frequently missed components for laparoscopic cholecystectomy.
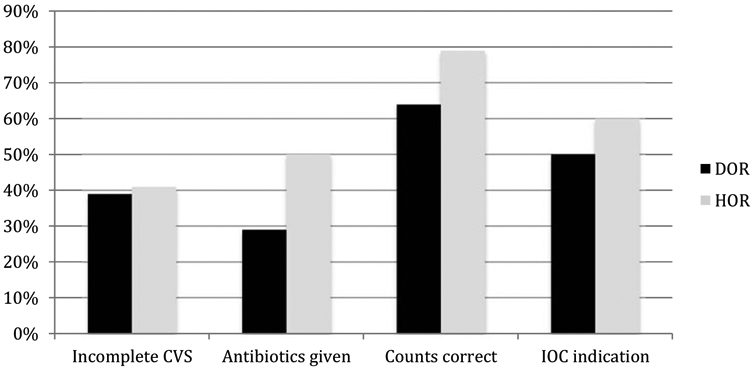
CVS = critical view of safety; IOC = intraoperative cholangiogram
Post-Participation Survey Results
Survey results yielded 10 PD and 24 LC responses. The percent responding agree or strongly agree to the following statements are shown in Figure 4 and were:
Figure 4. Percent of participant survey respondents that agree or strongly agree with statements.
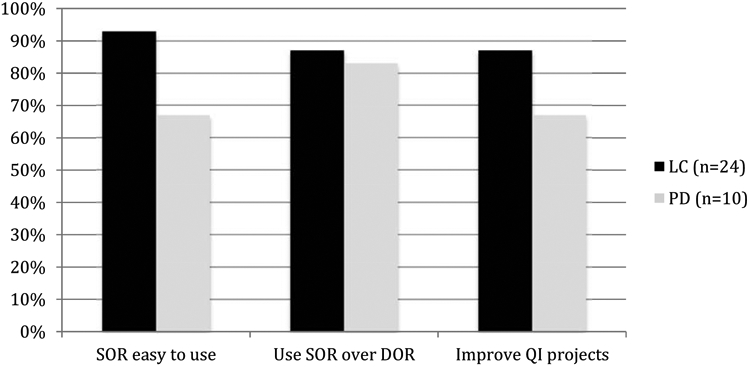
QI = quality improvement
The synoptic operatic report was easy to use (PD 67%, LC 93%)
I would use the synoptic operative report over a dictated operative report (PD 83%, LC 87%)
The synoptic operative report would improve my ability to conduct QI projects (PD 67%, LC 87%).
Benefits of using synoptic operative reports included:
The perceived value of standardized reporting
The ability to conduct quality research
Reducing dictation costs
Barriers to using synoptic operative reports included:
Creating a user-friendly electronic medical record integrated synoptic operative report using various platforms
Access to information technology (IT) support
Overcoming surgeon preference to dictate
Concern over template abuse (similar to standardized note templates)
Discussion
Our results demonstrate that synoptic operative reports are completed at a percent approaching almost 100% in both pancreaticoduodenectomy and laparoscopic cholecystectomy. This goal was achieved at multiple participating sites and demonstrates feasibility of integration into daily provider documentation practice. At a single institution, synoptic operative reports were more complete than associated dictated operative reports and historical case matched dictated operative reports. Assessment of completeness is subject to interpretation. If components that are easily identified in the electronic medical record elsewhere are missing (such as patient age, BMI, or gender), then the impact is significantly less on high quality documentation. However, if the missing components are essential such as documentation of the critical view of safety, stent placement and location or indication for an intraoperative cholangiogram, the effect on high quality, consistent documentation is much different. We found that the more frequently missed components in dictated operative reports were typically essential items or those that would only be found in an operative report. This supports that synoptic operative reporting may confer a benefit by “cueing” providers to enter critical portions of the procedure and help improve reporting consistency between providers and institutions. This is further enhanced by the ability to incorporate “hard stops” into the synoptic report by requiring the provider to enter information or make a selection in order to complete the submission.
The benefit of incorporating required elements both improves consistency and also assists with billing. Those with administrative duties can rely on these elements being present within the operative note and thus potentially improve workflow and accuracy. For billing purposes and to address case complexity, the optional components of a “brief narrative of the case” and “additional comments” were present in both SORs. This allowed surgeons to tailor the SOR to the case if unique components, complexity or missing elements required documentation. These optional components were used in both SORs almost 50% of the time, indicating their utility for documentation purposes. Surgeons may find these components helpful, especially for operative components that need to be communicated to covering surgeons in their absence, radiologic evaluation, oncologic surveillance, future treatment or surgical intervention, and/or justification of billing.
This study also highlights that surgeons are generally satisfied with the use of this operative reporting format. Ease of use could certainly be augmented by incorporating electronic medical record features that would auto-populate components in synoptic operative reports. We acknowledge that this was not part of our study and may increase surgeon preference to use SOR further by eliminating the need to enter redundant information and the amount of “clicking” necessary to progress through the automated form. Having the option to provide a brief narrative and additional comments was deemed useful by participants in the event that a component was not part of the SOR or a unique situation needed to be included in the SOR.
This study demonstrates the ability to reach a consensus on SOR using expert groups for two different procedures, implementing them in a multi-institutional fashion, and achieving a high degree of surgeon satisfaction. Notably, determining what should and should not be included in a synoptic operative report is subject to surgeon opinion. However, we were able to achieve consensus regarding the content of synoptic operative reporting forms among participating institutions for each operation. After completing the data collection, participating surgeons suggested removing a few components. For PD, removing clinical stage was recommended as it is not pertinent in most cases. In addition, finding a way to incorporate automated data would be ideal for a number of entered components including patient demographics (age, gender, BMI, risk factors, ASA class), surgeon, assistants, and other elements that are documented before the operation or during the surgical procedure. Future work to delineate components that may be auto-populated into the operative report would be favorable to reduce data entry but also unique to each EMR platform and thus was not possible in this study.
The College of American Pathologists (CAP) has done a commendable job of standardizing pathologic reporting for cancer using SOR. The CAP has reached consensus on reporting for a number of complicated pathology reports including autopsy(9), thyroid cytopathology(10), hematologic and lymphoid neoplasms(11), and cancer biomarkers(12) to name a few. The CAP rectal cancer synoptic report is one of the important standards of the new Commission on Cancer (CoC) National Accreditation Program for Rectal Cancer (NAPRC) Because of this work, published cancer synoptic reports are accepted and utilized nationally(12-14). The American College of Surgeons has the opportunity to utilize similar methodology in developing a core of nationally accepted operative synoptic reports. One of the standards of the new ACS CoC NAPRC requires the use of a synoptic operative report which is currently under development by a work group from the American Society of Colon and Rectal Surgeons (15).
There is also an educational benefit to synoptic operative reporting. Residents learn what is important to include in the report. They must know what was and was not done in the procedure by engaging in the documentation process. Residents have been shown to gain educational benefits and that resident data entry for synoptic operative reports is superior to dictation (8). Unfortunately, the presence of synoptic operative reporting is currently quite uncommon in most surgical subspecialty residencies (16). Enhancing the quality of operative documentation while improving resident education and engagement is another potential benefit of SOR.
There are several limitations in this study. The synoptic operative report forms were developed based on previously published forms with revisions based on expert content analysis and rounds of editing. A more robust way of developing a form, should it be used regionally or nationally, would be to conduct a Delphi consensus approach to determining included components. This has been done successfully for a lung cancer synoptic reporting form and emulating this process may improve the included components further (17). We did not assess the reliability of reported data. This has been done previously with good inter-rater reliability between attending physician reporters and fellows (7).
In addition, we did not specifically address whether the dictated report was completed by the same individual that entered the synoptic operative report for our single institution subset analysis. Because of this, there may be a tendency toward increased or decreased completeness depending on whether the individual completing the dictated report had just completed the synoptic report. Recent SOR entry could predispose the dictating surgeon to include more components. To improve methodology in future studies we should standardize that the dictated operative report should be done first and then followed by the synoptic operative report to ensure that dictations are not falsely improved by cues from the synoptic operative report. Despite this, we still saw a difference in completeness between SOR and DOR even though participants were well aware of the synoptic operative report components that would be included.
Conclusions
Synoptic operative reporting is a high quality, consistent, and feasible reporting method for documenting operative reports. When surveyed, the majority of participating surgeons indicated their preference for using synoptic operative reports and expressed their willingness to use them. Future implementation of synoptic operative reporting may require overcoming barriers of electronic medical record integration, ensuring meaningful use, and providing adequate information technology support.
Supplementary Material
Highlights.
Synoptic operative reports are more complete than dictated operative reports
The majority of surgeons indicated their preference for SOR and their willingness to use them
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation
Western Surgical Association Annual Meeting, Scottsdale, AZ November 2017
References
- 1.Novitsky YW, Sing RF, Kercher KW, Griffo ML, Matthews BD, Heniford BT. Prospective, blinded evaluation of accuracy of operative reports dictated by surgical residents. Am Surg. 2005;71(8):627–31; discussion 31-2. [PubMed] [Google Scholar]
- 2.Flynn MB, Allen DA. The operative note as billing documentation: a preliminary report. Am Surg. 2004;70(7):570–4; discussion 4-5. [PubMed] [Google Scholar]
- 3.Mack LA, Bathe OF, Hebert MA, Tamano E, Buie WD, Fields T, et al. Opening the black box of cancer surgery quality: WebSMR and the Alberta experience. J Surg Oncol. 2009;99(8):525–30. [DOI] [PubMed] [Google Scholar]
- 4.Weymuller EA Jr., Ahmad K, Casiano RR, Schuller D, Scott CB, Laramore G, et al. Surgical reporting instrument designed to improve outcome data in head and neck cancer trials. Ann Otol Rhinol Laryngol. 1994;103(7):499–509. [DOI] [PubMed] [Google Scholar]
- 5.Laflamme MR, Dexter PR, Graham MF, Hui SL, McDonald CJ. Efficiency, comprehensiveness and cost-effectiveness when comparing dictation and electronic templates for operative reports. AMIA Annu Symp Proc. 2005:425–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Harvey A, Zhang H, Nixon J, Brown CJ. Comparison of data extraction from standardized versus traditional narrative operative reports for database-related research and quality control. Surgery. 2007;141(6):708–14. [DOI] [PubMed] [Google Scholar]
- 7.Park J, Pillarisetty VG, Brennan MF, Jarnagin WR, D'Angelica MI, Dematteo RP, et al. Electronic synoptic operative reporting: assessing the reliability and completeness of synoptic reports for pancreatic resection. J Am Coll Surg. 2010;211(3):308–15. [DOI] [PubMed] [Google Scholar]
- 8.Gur I, Gur D, Recabaren JA. The computerized synoptic operative report: a novel tool in surgical residency education. Arch Surg. 2012;147(1):71–4. [DOI] [PubMed] [Google Scholar]
- 9.Hutchins GM, Berman JJ, Moore GW, Hanzlick R. Practice guidelines for autopsy pathology: autopsy reporting. Autopsy Committee of the College of American Pathologists. Arch Pathol Lab Med. 1999;123(11):1085–92. [DOI] [PubMed] [Google Scholar]
- 10.Auger M, Nayar R, Khalbuss WE, Barkan GA, Benedict CC, Tambouret R, et al. Implementation of the Bethesda System for Reporting Thyroid Cytopathology: observations from the 2011 thyroid supplemental questionnaire of the College of American Pathologists. Arch Pathol Lab Med. 2013;137(11):1555–9. [DOI] [PubMed] [Google Scholar]
- 11.Mohanty SK, Piccoli AL, Devine LJ, Patel AA, William GC, Winters SB, et al. Synoptic tool for reporting of hematological and lymphoid neoplasms based on World Health Organization classification and College of American Pathologists checklist. BMC Cancer. 2007;7:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzgibbons PL, Lazar AJ, Spencer S. Introducing new College of American Pathologists reporting templates for cancer biomarkers. Arch Pathol Lab Med. 2014;138(2):157–8. [DOI] [PubMed] [Google Scholar]
- 13.Pathologists CoA. Cancer Protocol Templates [Available from: www.cap.org/cancerprotocols.
- 14.Cancer Co. National Accreditation Program for Rectal Cancer [Available from: https://www.facs.org/quality-programs/cancer/naprc.
- 15.Wexner SD, Berho ME. The Rationale for and Reality of the New National Accreditation Program for Rectal Cancer. Dis Colon Rectum. 2017;60(6):595–602. [DOI] [PubMed] [Google Scholar]
- 16.Melton GB, Burkart NE, Frey NG, Chipman JG, Rothenberger DA, Vickers SM. Operative report teaching and synoptic operative reports: a national survey of surgical program directors. J Am Coll Surg. 2014;218(1):113–8. [DOI] [PubMed] [Google Scholar]
- 17.Schneider L, Shargall Y, Schieman C, Seely AJ, Srinathan S, Malthaner RA, et al. Design of a consensus-derived synoptic operative report for lung cancer surgery. Ann Thorac Surg. 2014;97(4):1163–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.