Abstract
Objectives
Theories of aging posit that older adult age is associated with less negative emotions, but few studies have examined age differences at times of novel challenges. As COVID-19 spread in the United States, this study therefore aimed to examine age differences in risk perceptions, anxiety, and depression.
Method
In March 2020, a nationally representative address-based sample of 6,666 U.S. adults assessed their perceived risk of getting COVID-19, dying if getting it, getting quarantined, losing their job (if currently working), and running out of money. They completed a mental health assessment for anxiety and depression. Demographic variables and precrisis depression diagnosis had previously been reported.
Results
In regression analyses controlling for demographic variables and survey date, older adult age was associated with perceiving larger risks of dying if getting COVID-19, but with perceiving less risk of getting COVID-19, getting quarantined, or running out of money, as well as less depression and anxiety. Findings held after additionally controlling for precrisis reports of depression diagnosis.
Discussion
With the exception of perceived infection-fatality risk, U.S. adults who were relatively older appeared to have a more optimistic outlook and better mental health during the early stages of the pandemic. Interventions may be needed to help people of all ages maintain realistic perceptions of the risks, while also managing depression and anxiety during the COVID-19 crisis. Implications for risk communication and mental health interventions are discussed.
Keywords: Anxiety, Depression, Risk perception
When COVID-19 entered the United States, reports from China were already indicating that case-fatality rates increased with older adult age (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020). Generally, older adult age has been associated with reporting less negative emotions (Carstensen, Pasupathi, Mayr, & Nesselroade, 2000), perceiving stressful events as less unpleasant (Neubauer, Smyth, & Sliwinski, 2019), and scoring lower on anxiety and depression (Löwe et al., 2010). Socio-emotional Selectivity Theory posits that adults who are relatively older are more motivated to maximize their well-being in the limited time they perceive to have left (Carstensen, 2006). However, the Strength and Vulnerability model suggests that older adults may find it harder to cope with serious or prolonged stressors (Charles, 2010).
As COVID-19 spread through the United States in March 2020, this study examined whether older adult age was associated with lower risk perceptions for COVID-19 and with less depression and anxiety. The former reflect cognitive/deliberative perceptions of threat, and the latter emotional responses (Kobbeltved, Brun, Johnsen, & Eid, 2005).
Method
Sample
Between March 10–31, 2020, 6,666 of 8,489 invited members of the University of Southern California’s (USC) Understanding America Study (UAS) aged 18–100 (M = 48.56, SD = 16.62) answered the questions analyzed here (response rate = 79%). To obtain a nationally representative sample, UAS members were recruited from randomly selected U.S. addresses (Understanding America Study Recruitment Protocol, 2019), sampling probabilities were adjusted for underrepresented populations, and internet-connected tablets were provided to interested individuals if needed (Alattar, Messel, & Rogofsky, 2018). Address-recruited online panels tend to be better than opt-in online panels at achieving national representativeness (Tourangeau, Conrad, & Couper, 2013) and delivering high-quality data (Kennedy et al., 2020). Following the survey literature (Valliant, Dever, & Kreuter, 2013), poststratification weights were used to further align the present sample to the U.S. adult population regarding age, gender, race/ethnicity, education, and location (see https://uasdata.usc.edu/page/Weights).
A sample size of 1,481 would have been sufficient to discover r ≥ 0.10 with 0.90 statistical power and α = 0.01. Demographic characteristics are discussed in the Results section. There were no significant differences between invitees who completed the questions analyzed here and those who did not, regarding age, gender, education, and race/ethnicity. However, compared to invitees who did not complete the survey, those who did were slightly less likely to report below-median income (50% vs 45%), χ 2(1) = 12.23, p < .001, slightly more likely to be married (51% vs 55%), χ 2(1) = 8.26, p < .01, and slightly less likely to live in worst-hit states (26% vs 22%), χ 2(1) = 9.77, p < .01.
Procedure
The online survey was approved by USC’s Institutional Review Board, as part of the UAS. Survey and data are publicly available (https://uasdata.usc.edu/index.php; #230).
Risk perceptions
Participants were asked “On a scale from 0 to 100%, what is the chance that you will get the coronavirus in the next three months?” and “On a scale of 0 to 100 percent, what is the chance that you will be quarantined within the next three months?” with the explanation that “In a quarantine, someone who has been exposed to coronavirus but is not presently sick may have to stay away from other people for 14 days.” Perceived infection-fatality risk was assessed by asking “If you do get infected with the coronavirus, what is the chance you will die from it?” Participants who indicated being employed were asked “What is the percent chance that you will lose your job because of the coronavirus in the next three months.” All answered “What is the percent chance that you will run out of money because of the coronavirus in the next three months?” Responses were provided on a validated visual linear scale ranging from 0% to 100% (Bruine de Bruin & Carman, 2018).
Mental health
Participants completed the validated 4-item Patient Health Questionnaire (PHQ-4), which assessed depression (“feeling, down, depressed or hopeless,” and “little interest or pleasure in doing things”) and typically co-occurring anxiety (“feeling nervous, anxious, or on edge” and “not being able to stop or control worrying”) over the past 2 weeks (Kroenke, Spitzer, Williams, & Löwe, 2009; Löwe et al., 2010). Response options included not at all (0), several days (1), more than half the days (2), and nearly every day (3). Internal consistency was sufficient to warrant summation of scores for the overall scale (α = 0.89), depression subscale (α = 0.87, r = 0.77, p < .001), and anxiety subscale (α = 0.86, r = 0.77, p < .001). Scores of ≥6 on the overall scale represent warning signs of depression and anxiety disorder, with ≥3 on each subscale representing warning signs of either depression or anxiety disorder (Löwe et al., 2010).
Control variables
Experiences with COVID-10 were assessed by asking “has a doctor or another healthcare professional diagnosed you with the coronavirus (COVID-19)?” and “do you think you have been infected with the coronavirus (COVID-19)?” with response options yes, no, and unsure. Demographic variables were on record at the UAS, including gender (male = 1; female = 0), marital status (married = 1; not married = 0), non-Hispanic white race/ethnicity (yes = 1; no = 0), college education (yes = 1; no = 0), below-median income (yes = 1; no = 0), and residing in states that were worst-hit by COVID-19 at the time of the survey, including California, Massachusetts, New Jersey, New York, and Washington (yes = 1; no = 0). The date on which participants completed the survey was treated as a dichotomized variable (March 10–12, 2020 = 0; March 13–31, 2020 = 1) because half completed the survey within the first 3 days and very few completed it on later days (Bruine de Bruin & Bennett, in press). Participants were asked whether they were currently employed (yes = 1; no = 0). To incorporate precrisis depression diagnosis, the present survey data were merged with data from a survey conducted between December 2019 and January 2020, on which 5,638 (85%) of the 6,666 participants reported whether they had ever been diagnosed with depression (yes = 1; no = 0). Separate poststratification weights were used in analyses that included this variable, to align that sample to the U.S. adult population regarding age, gender, race/ethnicity, education, and location (see https://uasdata.usc.edu/page/Weights).
Results
Control Variables
Likely because the survey was conducted as the COVID-19 epidemic emerged in the United States, none of the participants reported a diagnosis with COVID-19, but 0.3% were unsure. None thought that they had been infected, with 6.9% being unsure. Older adult age, which was treated as a continuous variable in all analyses, was not associated with being unsure about a diagnosis (r = −0.02, p = .08) but it was associated with being less unsure about infection (r = −0.10, p < .001). Because the low variability of the former likely undermined the ability to discover relationships, only the latter was included as a control variable.
Overall, 48% of participants were male, 55% were married, 64% were non-Hispanic white, 34% had a college degree, and 22% lived in states that were worst-hit at the time (California, Massachusetts, New Jersey, New York, and Washington). Participants’ median income was $50,000–$59,999. By comparison, national statistics suggest that the U.S. population is 49% male, 50% married, 63% non-Hispanic white, 32% college-educated (if aged 25+), and 25% living in worst-hit states, with median income being $60,293 (Parker & Stepler, 2017; United States Census Bureau, 2018). In the present survey, 62% reported having a job. In a precrisis survey, 18% of N = 5,638 participants reported a depression diagnosis. As noted, half of participants completed the survey between March 10−12, 2020, and half between March 13−31, 2020.
Older adult age was unrelated to having a college degree (r = 0.01, p = .48), living in worst-hit states (r = −0.01, p = .47), or reporting below-median income (r = −0.01, p = .27). It was correlated to male gender (r = 0.14, p < .001), not having a job (r = −0.36, p < .001), being married (r = 0.17, p < .001), being non-Hispanic white (r = 0.19, p < .001), completing the survey before March 13, 2020 (r = −0.10, p < .001), and having no precrisis depression diagnosis (r = −0.07, p < .001).
Risk perceptions
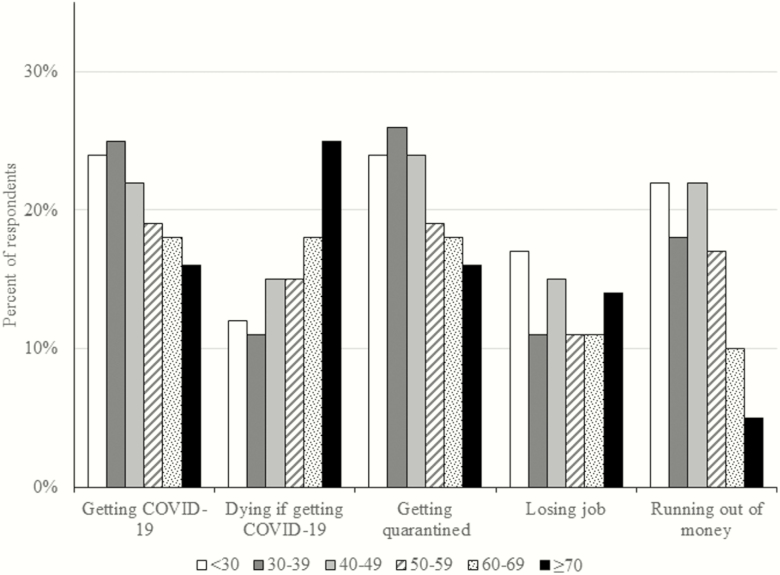
Pearson correlations indicated that older adult age was associated with perceiving greater infection-fatality risks, but smaller risks for getting COVID-19, getting quarantined, experiencing job loss (among N = 4,119 reporting current employment), and running out of money (Table 1; see also Figure 1). Except for job loss, these relationships with age held in linear regressions that controlled for being unsure about having been infected with COVID-19, gender, marital status, employment status, race/ethnicity, education, residing in the states that were worst-hit at the time, income, and survey date (Table 1, Model 1), as well as precrisis depression diagnosis (Table 1, Model 2). Full regression models with control variables appear in Supplementary Tables S1–S2.
Table 1.
Relationships of Age With Risk Perceptions and Mental Health Variables
| Predicted variable | Pearson correlation with age (r) | Relationships with age in regressions | |
|---|---|---|---|
| 1. with control variablesb | 2. with control variables and past depression diagnosis | ||
| Risk perceptions | |||
| Getting COVID-19 | −0.14*** | β = −0.11*** | β = −0.09*** |
| Dying if getting COVID-19 | 0.18*** | β = 0.17*** | β = 0.17*** |
| Getting quarantined | −0.13*** | β = −0.08*** | β = −0.08*** |
| Losing joba | −0.05** | β = −0.01 | β = −0.02 |
| Running out of money | −0.20*** | β = −0.15*** | β = −0.14*** |
| Mental health | |||
| Depression and anxiety score | −0.18*** | β = −0.19*** | β = −0.15*** |
| Depression score | −0.16*** | β = −0.18*** | β = −0.14*** |
| Anxiety score | −0.17*** | β = −0.17*** | β = −0.14*** |
| Warning signs of depression and anxiety disorder | −0.14*** | OR = 0.97*** [0.97, 0.98] | OR = 0.98*** [0.97, 0.98] |
| Warning signs of depression disorder | −0.12*** | OR = 0.97*** [0.97, 0.98] | OR = 0.98*** [0.98, 0.99] |
| Warning signs of anxiety disorder | −0.14*** | OR = 0.98*** [0.97, 0.98] | OR = 0.98*** [0.98, 0.99] |
Note. N = 6,666 for models with control variables except for N = 4,199 when predicting risk perceptions of job loss; N = 5,638 for models with control variables and past depression diagnosis except for N = 3,411 when predicting risk perceptions of job loss; β = standardized estimate in linear regression; OR = odds ratio [95% confidence interval] in logistic regression; age was treated as a continuous variable; warning signs of depression and anxiety disorder referred to scores of ≥6 on the 4-item Patient Health Questionnaire (PHQ-4) and warning signs of either depression or anxiety disorder referred to scores of ≥3 on PHQ-4 subscales (Kroenke et al., 2009; Löwe et al., 2010).
aAmong N = 4,119 who reported current employment.
bControl variables included being unsure about already having been infected (yes = 1; no = 0), gender (male = 1; female = 0), marital status (married = 1; not married = 0), non-Hispanic white race/ethnicity (yes = 1; no = 0), college education (yes = 1; no = 0), residing in worst-hit states (yes = 1; no = 0), below-median income (yes = 1; no = 0), and survey date (March 10–12, 2020 = 0; March 13–31, 2020 = 1). All regression models except ones predicting risk perceptions for job joss also included a control variable for being currently employed (yes = 1; no = 0). Pre-crisis depression diagnosis was reported in December 2019 and January 2020 (yes = 1; no = 0).
***p < .001. **p < .01.
Figure 1.
Age differences in risk perceptions. Note. Age groups were computed for presentation purposes only. The reported analyses treated age as a continuous variable. For all risks except job loss: N = 874 for age group <30, N = 1,630 for age group 30–39, N = 1,045 for age group 40–49, N = 1,102 for age group 50–59, N = 1,199 for age group 60–69, N = 816 for age group ≥70. For job loss: N = 597 for age group <30, N = 1283 for age group 30–39, N = 811 for age group 40–49, N = 788 for age group 50–59, N = 509 for age group 60–69, N = 131 for age group ≥70.
Mental health
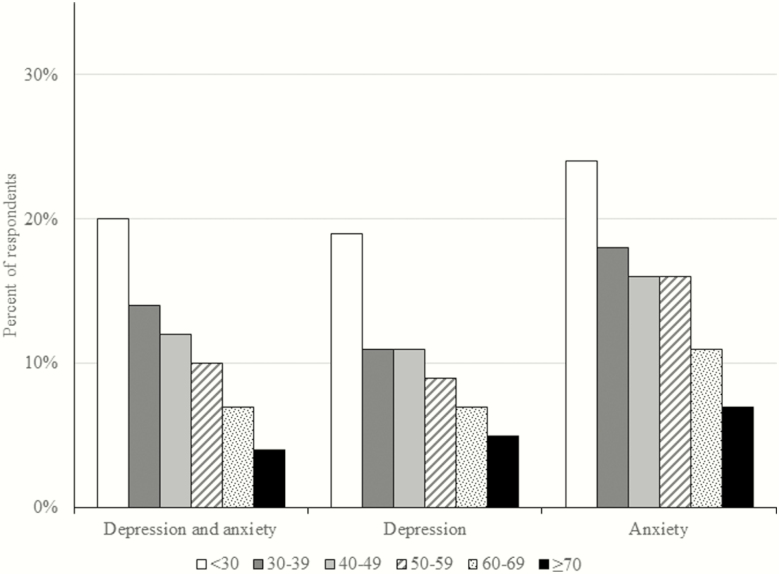
Pearson correlations indicated that relatively older adults scored lower on depression and anxiety, or their combination, with a similar pattern for exhibiting warning signs (Table 1; see also Figure 2). These results held in regressions that included the same control variables as above (Table 1, Model 1), as well as precrisis depression diagnosis (Table 1, Model 2). Full regression models with control variables appear in Supplementary Table S3–S4.
Figure 2.
Age differences in warning signs for depression and anxiety disorder. Note. Age groups were computed for presentation purposes only. The reported analyses treated age as a continuous variable. Warning signs of depression and anxiety disorder referred to scores of ≥6 on the 4-item Patient Health Questionnaire (PHQ-4) and warning signs of either depression or anxiety disorder referred to scores of ≥3 on PHQ-4 subscales (Kroenke et al., 2009; Löwe et al., 2010). N = 874 for age group <30, N = 1,630 for age group 30–39, N = 1,045 for age group 40–49, N = 1,102 for age group 50–59, N = 1,199 for age group 60–69, N = 816 for age group ≥70.
Discussion
In a national life-span sample, this study examined age differences in risk perceptions and mental health during the early stages of the COVID-19 outbreak in the United States. Older adult age was associated with perceiving greater infection-fatality risk. However, older adult age was also associated with seeing lower risks of getting COVID-19 and of experiencing negative economic consequences. Furthermore, older adult age was associated with less depression and less anxiety, for better overall mental health. Results for risk perceptions and mental health outcomes held after accounting for demographic control variables and whether or not participants had precrisis depression diagnoses, as reported between December 2019 and January 2020.
The present findings agree with studies suggesting that adults who are relatively older tend to report less negative emotions, better mental health, and less responsiveness to daily stressors (Carstensen et al., 2000; Neubauer et al., 2019), and experience less depression and anxiety (Löwe et al., 2010). Although concerns have been raised that such findings may not hold for more severe or prolonged stressors (Charles, 2010), the present findings suggest that older adult age was associated with less negative responses to the emerging COVID-19 crisis in the United States. Similarly, older adult age was associated with less distress after the 9/11 attacks, less fear of future attacks, and a steeper decline in post-traumatic stress over time (Scott, Poulin, & Silver, 2013). While the COVID-19 epidemic was outside of their control, adults who were relatively older may have regulated their emotions by focusing on the positive, or choosing activities and interactions that reduced their stress (Carstensen, 2006; Neubauer et al., 2019). Time will tell, however, whether older adults were too positive in their outlook. While unrealistic optimism can help to regulate emotions in the short run, it may sometimes leave people unprepared for negative outcomes occurring in the future (Shepperd, Waters, Weinstein, & Klein, 2015).
Like any study, the present study has potential limitations. One limitation is that it did not track individual participants over time. The survey was conducted in March 2020, at the early stages of the epidemic. As more people get sick, have loved ones fall ill and die, and suffer economic consequences, age differences in responsiveness may become less pronounced, disappear, or even reverse—especially because COVID-19 infection-mortality disproportionally affects older adults (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020). Indeed, analyses of survey data from the later stages of the COVID-19 outbreak in China suggest that there were no longer age differences in depression and anxiety (Qiu, Shen, Zhao, Xie, & Xu, 2020; Wang et al., 2020), even though the traditional finding of older adults being less depressed and anxious held in China before (Prina, Ferri, Guerra, Brayne, & Prince, 2011). Another limitation is that ill and vulnerable individuals may have been less likely to respond to the survey, potentially undermining extensive efforts toward recruiting a nationally representative sample.
Regardless, interventions may be needed to help people of all ages maintain realistic perceptions of the risks, while also managing depression and anxiety during the COVID-19 crisis. The Centers for Disease Control and Prevention’s (2014) guidelines on risk and crisis communication suggest that communications must be timely, accurate, and responsive to people’s need for information, while identifying what is known and unknown, and how the unknowns will be addressed. Additionally, the literature suggests that, moderate fear appeals may be effective when pointing to preventive behaviors that allow people to control their risks (Witte & Allen, 2000).
To manage mental health without requiring in-person meetings, psychological counseling services in China were delivered online and through voice-over-internet during their COVID-19 outbreak (Liu et al., 2020). Before COVID-19, it was already recommended that telemedicine be used when in-person care was impossible (García-Lizana & Muñoz-Mayorga, 2010). Preliminary evidence suggests the potential effectiveness of depression self-management through self-administered computer-based cognitive behavioral therapy (Grist & Cavanagh, 2013), and smartphone apps (Firth et al., 2017). Follow-up research is needed to understand age differences in risk perceptions and mental-health impacts of COVID-19 over time as well as to inform and subsequently test intervention strategies as the crisis unfolds.
Supplementary Material
Supplementary data are available at The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences online.
Funding
Data collection was supported and conducted by University of Southern California’s Center for Economic and Social Research. W. Bruine de Bruin was supported by the National Science Foundation (#2028683). University of Southern California’s Schaeffer Center for Health Policy and Economics, and the Swedish Riksbankens Jubileumsfond Program on “Science and Proven Experience.”
Acknowledgments
Marco Angrisani, Daniel Bennett, Jill Darling, Tania Gutsche, and Arie Kapteyn are gratefully acknowledged for their help with this study. Data are publicly available (https://uasdata.usc.edu/index.php; #230). The study was not preregistered.
Conflict of Interest
None declared.
References
- Alattar L., Messel M., & Rogofsky C (2018). An introduction to the understanding American study internet panel. Social Security Bulletin, 78, 13–28. Retrieved from https://www.ssa.gov/policy/docs/ssb/v78n2/v78n2p13.html. [Google Scholar]
- Bruine de Bruin W., & Bennett D. (in press). Relationships between initial COVID-19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine. doi: 10.1016/j.amepre.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin W., & Carman K. G (2018). Measuring subjective probabilities: The effect of response mode on the use of focal responses, validity, and respondents’ evaluations. Risk Analysis, 38, 2128–2143. doi: 10.1111/risa.13138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen L. L. (2006). The influence of a sense of time on human development. Science (New York, N.Y.), 312(5782), 1913–1915. doi: 10.1126/science.1127488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen L. L., Pasupathi M., Mayr U., & Nesselroade J. R (2000). Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology, 79(4), 644–655. doi: 10.1037//0022-3514.79.4.644 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2014). Crisis and emergency risk communication Retrieved May 17, 2020, from https://emergency.cdc.gov/cerc/manual/index.asp
- Charles S. T. (2010). Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychological Bulletin, 136(6), 1068–1091. doi: 10.1037/a0021232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Torous J., Nicholas J., Carney R., Pratap A., Rosenbaum S., & Sarris J (2017). The efficacy of smartphone-based mental health interventions for depressive symptoms: A meta-analysis of randomized controlled trials. World Psychiatry, 16(3), 287–298. doi: 10.1002/wps.20472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Lizana F., & Muñoz-Mayorga I (2010). Telemedicine for depression: A systematic review. Perspectives in Psychiatric Care, 46(2), 119–126. doi: 10.1111/j.1744-6163.2010.00247.x [DOI] [PubMed] [Google Scholar]
- Grist R., & Cavanagh K (2013). Computerised cognitive behavioural therapy for common mental health disorders, what works, for whom under what circumstances? A systematic review and meta-analysis. Journal of Contemporary Psychotherapy, 43, 243–251. doi: 10.1007/s10879-013-9243-y [DOI] [Google Scholar]
- Kennedy C., Hatley N., Lau A., Mercer A., Keeter S., Ferno J., & Asare-Marfo D (2020). Assessing the risks to online polls from bogus respondents Pew Research Center; Retrieved May 11, 2020, from https://www.pewresearch.org/methods/2020/02/18/assessing-the-risks-to-online-polls-from-bogus-respondents/ [Google Scholar]
- Kobbeltved T., Brun W., Johnsen B. H., & Eid J (2005). Risk as feelings or risk and feelings? A cross-lagged panel analysis. Journal of Risk Research, 8, 417–437. doi: 10.1080/1366987042000315519 [DOI] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. W., & Löwe B (2009). An ultra-brief screening scale for anxiety and depression. Psychosomatics, 50, 613–621. doi: 10.1016/S0033-3182(09)70864-3 [DOI] [PubMed] [Google Scholar]
- Liu S., Yung L., Zhang C., Xiang Y.-T, Liu Z., Hu S., & Zhang B (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet: Psychiatry, 7, PE17–PE18. doi: 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., . . . Brähler E (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122, 86–95. doi: 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- Neubauer A. B., Smyth J. M., & Sliwinski M. J (2019). Age differences in proactive coping with minor hassles in daily life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 74(1), 7–16. doi: 10.1093/geronb/gby061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (2020). The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly, 2, 113–122. doi: 10.46234/ccdcw2020.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker K., & Stepler R (2017). As U.S. marriage rate hovers at 50%, education gap in marital status widens Pew Research Center; Retrieved May 11, 2020, from https://www.pewresearch.org/fact-tank/2017/09/14/as-u-s-marriage-rate-hovers-at-50-education-gap-in-marital-status-widens/ [Google Scholar]
- Prina A. M., Ferri C. P., Guerra M., Brayne C., & Prince M (2011). Prevalence of anxiety and its correlates among older adults in Latin America, India, and China: Cross-cultural study. The British Journal of Psychiatry, 199, 485–491. doi: 10.1192/bjp.bp.110.083915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Xie B., & Xu Y (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy reminders. BMJ: General Psychiatry, 33, 1–3. doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S. B., Poulin M. J., & Silver R. C (2013). A lifespan perspective on terrorism: Age differences in trajectories of response to 9/11. Developmental Psychology, 49(5), 986–998. doi: 10.1037/a0028916 [DOI] [PubMed] [Google Scholar]
- Shepperd J. A., Waters E., Weinstein N. D., & Klein W. M (2015). A primer on unrealistic optimism. Current Directions in Psychological Science, 24(3), 232–237. doi: 10.1177/0963721414568341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourangeau R., Conrad F. G., & Couper M. P (2013). The science of web surveys. New York, NY: Oxford University Press. [Google Scholar]
- Understanding America Study Recruitment Protocol (2019). USC Dornsife Center for Economic and Social Research Retrieved May 11, 2020, from https://uasdata.usc.edu/index.php?r=eNpLtDKyqi62MrFSKkhMT1WyLrYyslwwskuTcjKT9VLyk0tzU_NKEksy8_NS8svzcvITU0BqgMrzEnPhykMdgxWCUpOLSjNLQMoVAoryS_KT83P0ClLSlKxrAZOmXCIG
- United States Census Bureau (2018). QuickFacts United States Retrieved May 11, 2020, from https://www.census.gov/quickfacts/fact/table/US/PST045218
- Valliant R., Dever J. A., & Kreuter F (2013). Practical tools for designing and weighting survey samples. New York, NY: Springer. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C. S., & Ho R. C (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Public Health Research and Public Health, 17, 1–25. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K., & Allen M (2000). A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior, 27(5), 591–615. doi: 10.1177/109019810002700506 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.