Abstract
Early intensive intervention has been shown to significantly affect the development of children with autism spectrum disorder. However, the costly implementation of such interventions limits their wide dissemination in the community. This study examined an integration of the Early Start Denver Model into community preschool programs for children with autism spectrum disorder in Israel. Four community preschools implemented the preschool-based Early Start Denver Model and four implemented a multidisciplinary developmental intervention which is widely applied in Israeli community autism spectrum disorder preschools. Fifty-one children (aged 33–57 months) participated in the study. Twenty-six attended the preschool-based Early Start Denver Model preschools and twenty-five attended the multidisciplinary developmental intervention settings. Groups were comparable on age, developmental functioning, and socio-economic status. Compared to the multidisciplinary developmental intervention group, children in the preschool-based Early Start Denver Model treatment made greater gains on blinded measures of overall cognitive development, receptive and expressive language skills, as well as on parent- and teacher-reported adaptive communication and socialization abilities. In the preschool-based Early Start Denver Model group, children with lower symptom severity, higher adaptive functioning, and receptive language abilities at pre-treatment showed greater improvement. This study documents the successful integration of an Early Start Denver Model intervention into pre-existing community preschools, underlining the importance of disseminating evidence-based early intervention in community settings.
Lay Abstract
Early intensive intervention has been shown to significantly affect the development of children with Autism. However, the costly implementation of such interventions limits their wide dissemination in the community. This study examined an integration of a research-supported early intensive intervention model called the Early Start Denver Model into community preschool programs for children with Autism in Israel. Four community preschools implemented the preschool-based Early Start Denver Model and four implemented the existing multidisciplinary developmental intervention which is widely applied in Israeli community preschools for children with autism. Fifty-one children (aged 33–57 months) participated in the study. Twenty-six attended the preschool-based Early Start Denver Model preschools and twenty-five attended the multidisciplinary developmental intervention preschools. Before the intervention began, groups were comparable on children’s age and developmental functioning and on families’ socio-economic status. Results showed that, compared to the multidisciplinary developmental intervention group, children in the preschool-based Early Start Denver Model treatment group made greater gains on measures of overall cognitive development, language skills, as well as on parent- and teacher-reported adaptive communication and socialization abilities. Children who had lower autism symptom severity, higher adaptive functioning and better language understanding abilities before taking part in the preschool-based Early Start Denver Model program showed greater improvements following it. This study documents the successful implementation of an intensive early intervention program in pre-existing community preschools, underlining the importance of the integration of research-supported intervention programs into community settings.
Keywords: autism, clinical trial, early intervention, ESDM, preschool
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental condition, characterized by social communication deficits and restrictive repetitive behaviors (American Psychiatric Association (APA), 2013). In the last decades, the prevalence of ASD has seen a substantial escalation and is currently reported at around 1.68% of children diagnosed by the age of eight (Baio et al., 2018).
The age at which ASD is identified has gradually declined (Nygren et al., 2012; Raz et al., 2015), widening options for intervention during early sensitive periods of brain development (Anagnostou et al., 2014).
The educational system is currently the main provider for ASD-specific interventions in various countries, including the United States (Suhrheinrich et al., 2014). It implements various treatment practices which target social, communicational, and other developmental objectives in one-on-one and in group settings (Freeman & Kasari, 2013; Stahmer, 2007). Aside from the fact that these services are subsidized and easier to attain than private home-based interventions, preschool settings provide children with invaluable opportunities to generalize learned material, to interact with peers, and to practice social skills such as reciprocity, engagement, and cooperation via direct experience (Vivanti, Duncan, et al., 2017). Research in community intervention for children with ASD shows that evidence-based early intervention models can be effectively implemented in community settings. These models include, for example, the joint attention, symbolic play, engagement and regulation intervention (JASPER; Chang et al., 2016), and pivotal response training (PRT; Mohammadzaheri et al., 2015).
In Israel, children with an ASD diagnosis are eligible for a therapeutic package of 14 hours delivered in community ASD preschool settings by clinical and educational professionals. Most Israeli ASD preschools do not adhere to a specific comprehensive treatment model (CTM), that is, a manualized set of treatment practices targeting core ASD features, based on a comprehensive theoretical framework, and delivered in an intensive fashion (Odom et al., 2010). Rather, they build on various treatment approaches, aiming to integrate their practices when constructing each child’s treatment program.
The ESDM is a manualized CTM informed by behavioral, developmental, and relationship-based approaches (Rogers & Dawson, 2010), designed for toddlers and young children between 12 and 60 months. It involves the use of behavioral teaching techniques embedded in joint activity routines (Ratner & Bruner, 1978) characterized by high positive affect and adult sensitivity and responsiveness to the child’s communicative cues. Teaching episodes take place in routine day-to-day activities, so as to maximize naturalistic learning opportunities for the child. Learning objectives are based on a developmental curriculum which addresses a variety of developmental domains. In addition, the ESDM promotes active parental involvement, including parent coaching aimed to empower parents to implement the model’s principles and strategies in their daily routines. As a manualized model, the ESDM also adheres to fidelity criteria which therapists are required to meet as part of their training and throughout treatment delivery (Rogers & Dawson, 2010).
The ESDM was formerly shown to be efficacious in enhancing child outcomes in an intensive 1:1 setting (Dawson et al., 2010), with preliminary research suggesting positive outcomes also in response to a low-intensity 1:1 program (Colombi et al., 2018), in parent-delivered programs (Rogers et al., 2019), and in daycares that were created with the a priori intent to deliver the group-based ESDM model (G-ESDM; Vivanti, Duncan, et al., 2017) to attending children with ASD (Vivanti et al., 2014). Until now, however, there is limited research on the effectiveness of the ESDM when introduced and integrated into pre-existing preschool community settings (Vivanti et al., 2018). Furthermore, in a recent study, attempting to replicate the results of the first randomized controlled trial which examined the intensive one-on-one delivery of the ESDM as compared to treatment-as-usual, intervention-related gains were limited to expressive language (EL) and receptive language (RL) (Rogers et al., 2019). This set of results indicates that the ESDM should be further studied in various delivery settings. Furthermore, the effect of child pre-intervention characteristics on treatment outcome requires further examination.
In the past decade, early intervention research has started focusing on the examination of “what works for whom,” aiming to identify child factors associated with change occurring during intervention. Some of the pre-treatment child-related predictors associated with better response to early intervention include pre-treatment higher cognitive abilities (Hudry et al., 2018; Smith et al., 2015; Tiura et al., 2017), expression of positive affect (Fossum et al., 2017), decreased social avoidance (Fossum et al., 2017), lower ASD symptom severity (Ben-Itzchak & Zachor, 2011), younger age (Smith et al., 2015; Vivanti et al., 2016, 2018), higher adaptive skills (Flanagan et al., 2012), imitation, functional use of objects and goal understanding (Vivanti et al., 2013), play skills (Ingersoll, 2010), and joint attention (Kasari et al., 2008). The exploration of factors associated with intervention response is essential in community-based treatment programming, where resources are usually limited, the profiles of treated children are heterogeneous, and different intervention options might exist. In this context, the examination of specific response profiles to different interventions has the potential to inform proactive child-intervention assignment based on pre-intervention profiles. For example, two studies examined response profiles to PRT and discrete trial training (DTT) and identified object manipulation, approach, and avoidance behaviors and self-stimulatory behaviors as predictive of treatment response to PRT but not DTT (Schreibman et al., 2009; Sherer & Schreibman, 2005). This approach enables treatment providers to make more informed and cost-effective choices for children with ASD. However, the research regarding treatment response profiles is relatively scarce.
This study
This study documents the integration of the ESDM framework into pre-existing community ASD preschools in Israel. We examined the implementation and the effectiveness of a preschool-based ESDM (PB-ESDM) program, which combined individual, group, and parent ESDM intervention components. The effectiveness of the PB-ESDM was compared with the commonly provided multidisciplinary developmental intervention (MDI). Developmental and adaptive gains made by participating children in response to the two models were compared. In addition, we explored the developmental profiles of children who were defined as either high or low responders to the PB-ESDM treatment. To the best of our knowledge, no previous research has addressed these research questions.
The following hypotheses were examined: (1) children from both groups will show significant gains after intervention in measures of cognitive development and adaptive skills; (2) the PB-ESDM group will show significantly higher gains in measures of receptive and expressive language and in adaptive communication and socialization skills, compared to the MDI group; and (3) based on prior research, we hypothesized that high-treatment responders would have lower pre-treatment ASD symptom severity and higher cognitive and adaptive abilities compared to low responders.
Methods
Design
The study employed a 2 × 2 repeated measures factorial design, with intervention (PB-ESDM, MDI) as the between-group factor and time (pre-intervention and post-intervention) as the within-subject factor. Out of 48 preschools located in a central district in Israel, jointly operated by the Ministry of Education and the Autism Treatment and Research Center, the Association for Children at Risk, a non-governmental organization that provides Ministry of Health (MOH) mandated treatment packages to ASD preschools, seven community preschools showed interest in implementing the PB-ESDM model. Four of these preschools, which were attended by the youngest children, were chosen to participate in the study. Then, four comparison preschools from the same district delivering the MDI were approached based on children’s age. The eight selected preschools had full educational and therapeutic staffing, in order to assure optimal treatment conditions. The study was ethically approval by the Beer-Yaacov - Ness-Ziona mental health center’s Helsinki committee.
Participants
Out of the sixty-six children who attended the eight community ASD preschools, fifty-two parents gave consent to participate in the study. Twenty-six children were from the PB-ESDM group and 26 from the MDI group. Class sizes were of 8–9 children overall. Children whose parents did not consent to take part in the study received the intervention throughout the year but were not assessed. All children were pre-diagnosed with ASD by either a neurodevelopmental pediatrician, a pediatric neurologist, or a child and adolescent psychiatrist, as well as a psychologist, in community or private settings, according to Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5) criteria (APA, 2013). The autism diagnostic observation schedule, second edition (ADOS-2; Lord et al., 2012) was administered to all participating children by a research-reliable team in order to verify their diagnosis. All of the participants scored above cutoff for ASD. Preschools of both groups were located in an urban, central district in Israel. Groups were comparable on family socio-economic status (SES), children’s age, gender, developmental and adaptive functioning levels, and on symptom severity, as detailed in Table 1. After the pre-intervention assessment, one family from the MDI group left the study. In addition, parents of four participants did not complete the VABS-II interview due to scheduling difficulties (two families at baseline and post-treatment and two families at post-treatment only).
Table 1.
Participants’ pre-intervention measures.
| Measure | PB-ESDM (n = 26) | MDI (n = 25) | p | Cohen’s d |
|---|---|---|---|---|
| Age (months) | 43.65 (7.37) | 45.12 (4.8) | 0.41 | 0.24 |
| Gender (m:f) | 20:6 | 22:3 | ||
| SES | 2.92 (0.76) | 3.23 (0.99) | 0.22 | 0.35 |
| ADOS calibrated severity score | 7.11 (1.66) | 7.13 (1.78) | 0.98 | 0.01 |
| External treatment (h\week) | 0.73 (0.92) | 0.76 (1.09) | 0.92 | 0.03 |
| Prior exposure to MDI (%) | 36% | 40% | 0.77 | |
| MSEL DQ scores | ||||
| Total | 53.95 (18.74) | 46.86 (17.36) | 0.17 | 0.39 |
| Visual reception | 57.30 (19.3) | 51.39 (19.24) | 0.28 | 0.31 |
| Fine motor | 56.25 (15.21) | 51.32 (14.27) | 0.24 | 0.33 |
| Receptive language | 52.84 (24.77) | 43.01 (22.31) | 0.14 | 0.41 |
| Expressive language | 48.38 (23.33) | 41.16 (21.53) | 0.26 | 0.32 |
| VABS-II parent report | ||||
| Adaptive behavior composite | 70.12 (8.41) | 66.09 (7.74) | 0.09 | 0.49 |
| Communication domain | 74.8 (15.06) | 67.70 (13.31) | 0.09 | 0.50 |
| Daily living skills domain | 71.32 (10.55) | 67.65 (10.22) | 0.23 | 0.35 |
| Social skills domain | 71.04 (8.70) | 68.17 (10.16) | 0.30 | 0.31 |
| Motor skills domain | 76.40 (10.54) | 73.00 (7.42) | 0.21 | 0.37 |
| VABS-II teacher report | ||||
| Adaptive behavior composite | 68.67 (10.82) | 65.21 (9.74) | 0.59 | 0.34 |
| Communication domain | 69.04 (16.49) | 64.75 (15.88) | 0.34 | 0.27 |
| Daily living skills domain | 70.15 (14.57) | 66.71 (13.09) | 0.38 | 0.25 |
| Social skills domain | 65.08 (9.84) | 63.83 (7.99) | 0.62 | 0.14 |
| Motor skills domain | 74.89 (11.21) | 77.38 (13.27) | 0.48 | 0.20 |
All group comparisons were non-significant.
PB-ESDM: preschool-based Early Start Denver Model; MDI: multidisciplinary developmental intervention; MSEL DQ: Mullen scales of early learning developmental quotient, VABS-II: Vineland adaptive behavior scales, second edition; SES: socio-economic status (rated on a 1–5 scale, 1 being the lowest); ADOS: autism diagnostic observation schedule.
Intervention
Children in both groups received one of the following intervention programs during their 44 weekly hours preschool time, over an 8-month period:
MDI
This intervention program consisted of a combination of methods from several approaches and CTMs—applied behavioral analysis (ABA), the developmental, individual difference, relationship-based (DIR) model (Greenspan & Wieder, 2005), treatment and education of autistic and related communication handicapped children (TEACCH; Lord & Schopler, 1989), and dynamic psychotherapy. The intervention was delivered by a multidisciplinary team, which included a speech-language pathologist, an occupational therapist, a psychologist or a social worker, a behavioral analyst, a creative-arts therapist (art/dance/music), and a physical therapist, who worked alongside the special education teacher and her paraprofessional aides (Laor et al., 2017). While this model included no structured intervention protocol, individualized educational plans (IEPs) were determined by the multidisciplinary staff based on its assessments and were reviewed three times a year. Parents attended fortnightly counseling sessions with a psychologist or a psychotherapist in order to receive input regarding their child’s condition and progress and raised various issues concerning their child’s functioning. Parents met with the other therapeutic and educational staff members at least three times a year. Staff members received individual and group supervision regularly, which was not guided by formal fidelity criteria.
The PB-ESDM
Integrating the ESDM into the community ASD preschools involved an authorization process of the ESDM by the Israeli MOH as a service included in the intervention package provided to children with ASD in terms of intensity and supervision. Next, a group of therapists (at least one from each preschool) underwent the basic and advanced ESDM workshops and met fidelity criteria (fidelity ⩾ 80%) by the first 3 months following training. Fidelity scoring was based on the ESDM fidelity checklist, which was previously shown to have an inter-rater agreement of 97% (Vismara et al., 2012). Scoring was completed by MIND Institute certified ESDM trainers who were not part of the research team. The formal training did not include the parent-coaching module. However, team members who engaged in parent coaching were supervised by a senior clinical psychologist, who was also a certified ESDM therapist, formally trained on the parent module of the ESDM. The model’s principles were explained and demonstrated by trained therapists to the preschools’ educational and therapeutic teams, intervention materials were provided, and members of those teams were encouraged to participate in the team’s learning process. Each team had at least one ESDM therapist receiving formal training, who conducted the initial assessment process, wrote children’s objectives, and coordinated their monitoring. In addition, para-professional staff received ESDM-oriented supervision and implemented the model’s principles in their daily interactions with children. Finally, parents participated in weekly joint sessions with their children, in which they have acquired different principles to promote language, communication, and social engagement.
The PB-ESDM group differed from the MDI group in three main aspects: (1) Individual Educational Plans were guided by the ESDM curriculum. Children were observed by the multidisciplinary staff and curriculum items were coded according to the child’s performance in each domain. Developmental skills that were not fully mastered by the child were translated into learning objectives which were targeted by the intervention team. Child progress against the predefined objectives as well as fidelity of implementation were systematically monitored. Objectives were updated when the child met criteria for full mastery; (2) Interventions were conducted according to ESDM principles and included, in addition to individual and group interventions, weekly parent–child sessions which were based on the ESDM guidebook for parents (Rogers et al., 2012). In these sessions, parents observed the therapist interact with the child while applying various teaching techniques, implemented these techniques during their interaction with the child, received feedback from the therapist, and discussed various ways to enhance child communication. In addition, parents were encouraged to familiarize themselves with the daily objective sheet and to practice its items at home. No fidelity data were taken on parents’ delivery of the ESDM at home; (3) Supervision was provided according to the ESDM fidelity rating system. Fidelity was measured every few weeks for every team member implementing the PB-ESDM, targeting a fidelity rate of at least 80%. Sessions that did not reach fidelity were reviewed and therapists were requested to demonstrate corrective action with regards to fidelity items that received low scores.
Measures
Demographic data
The data collected included child gender and age, previous schooling history, and information on the types and intensity of additional therapies received outside of the preschool (as reported by parents). Family SES was rated by preschool case managers, based on parent contribution to the cost of schooling which depends on parental income.
Mullen scales of early learning (MSEL)
A standardized measure of early development which is administered to children from birth to 68 months of age (Mullen, 1995). The MSEL includes five subscales: receptive language (RL), expressive language (EL), visual reception (VR) and fine motor (FM) skills, for which standard T scores and age equivalents (AEs) are computed, together with a total composite of intellectual ability. As many children in this study did not reach sufficient scores for standard scores to be computed, an estimated developmental quotient (DQ) was obtained using the following formula: (MSEL AE/chronological age) × 100 (see Vivanti et al., 2014).
Vineland adaptive behavior scales, second edition
A structured interview measuring adaptive behavior from birth to adulthood (Sparrow et al., 2005). This measure is divided into 11 subscales, clustered into four domains: communication, daily living skills, socialization, and motors skills. Standard scores and AEs can be obtained from this measure, together with an adaptive behavior composite (ABC). In this study, parents were administered the interview version of the Vineland adaptive behavior scales, second edition (VABS-II) by trained examiners, while teachers filled out the instrument’s survey form. Since a group of children in the current sample did not reach baseline levels in some of the subdomains of the teacher form, the parent version, for which norms include infancy, was given to the teachers as well.
Procedure
At the beginning of the school year, parents of participants in both groups were informed that an evaluation of their children’s preschool intervention will be conducted at the beginning and the end of the school year.
After receiving informed consent, pre-treatment child and parent measures were collected during the first 2 months of the school year by qualified clinicians. During the 8 months of intervention, children attended the preschool for 44 h per week, in which group and individual educational activities and treatments were delivered, together with free play and mealtimes. Treatment fidelity in the PB-ESDM group and continuation of treatments in the MDI group were monitored throughout the year. Post-treatment data were obtained on the last 2 months of the school year. Child evaluation took place at the child’s preschool setting. It lasted approximately 1.5 h and was distributed over two consecutive sessions to avoid fatigue. Assessors were blind to treatment allocation and study hypotheses. Data from parents were collected either at home or at the preschool, per their choice.
Results
First, in order to make sure all outcome measures met the requirements for parametric analysis, the data were checked for outliers and Kolmogorov–Smirnov tests were conducted to confirm all measures were normally distributed.
In order to test the study hypotheses, analyses of variance (ANOVAs) with repeated measures were conducted for the primary and secondary outcome measures with time (pre–post-intervention) as the within-subject factor and group (PB-ESDM, MDI) as the between-subject factor.
Mullen scales of early learning
Overall score
The ANOVA yielded an overall main effect for time (F(1, 49) = 9.50, p < 0.01, d = 0.87), group (F)1, 49) = 4.90, p < 0.05, d = 0.63), and a significant time × group interaction effect (F(1, 49) = 8.52, p < 0.01, d = 0.84). Post hoc analyses with Bonferroni correction showed a significant increase in participants’ overall estimated DQ for the PB-ESDM group (mean diff. i − j = 12.36, standard error (SE) = 2.88, p < 0.001) but not for the MDI group (mean difference I − j = 0.34, SE = 2.94, non-significant (ns)).
Subscales
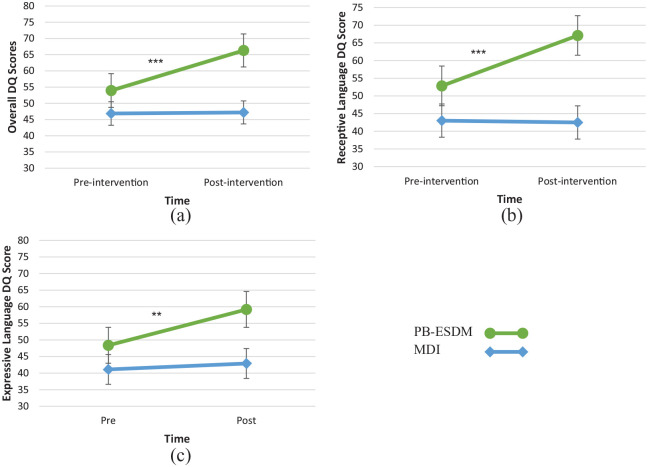
The analyses, detailed in Table 2, showed significant main effects for time in all four subscale scores, with an overall increase in these scores beyond group. A significant main effect for group was found for the RL measure only, with the PB-ESDM group showing higher overall RL scores than the MDI group. Significant time × group interaction effects for the RL and EL scales were also found. Simple main effects post hoc analyses with Bonferroni correction showed significant gains in the PB-ESDM group for EL (mean difference i − j = 10.81, SE = 2.98, p < 0.01) and RL (mean difference i − j = 14.26, SE = 3.32, p < 0.001), which were not found in the MDI group (EL—mean difference i − j = 1.74, SE = 3.03, ns; RL—mean difference i − j = 5.08, SE = 3.39, ns). The interaction effects are illustrated in Figure 1.
Table 2.
Means (SDs) of pre- and post-intervention MSEL subscale scores.
| PB-ESDM | MDI | Time | Time × group | |||||
|---|---|---|---|---|---|---|---|---|
| Measure | Pre | Post | Pre | Post | F(1, 45) | d | F(1, 45) | d |
| Total DQ | 53.95 (8.74) |
66.31 (27.22) |
46.86 (17.36) |
47.19 (24.62) |
9.50** | 0.87 | 7.52** | 0.84 |
| RL | 52.84 (24.77) |
67.10 (29.75) |
43.01 (22.31) |
42.50 (29.75) |
8.39** | 0.81 | 9.68** | 0.91 |
| EL | 48.38 (23.33) |
59.19 (30.52) |
41.12 (21.53) |
42.90 (22.60) |
8.73** | 0.84 | 4.55* | 0.63 |
| VR | 57.30 (19.30) |
70.69 (29.41) |
51.39 (19.24) |
58.42 (30.20) |
14.22*** | 1.06 | 1.38 | 0.35 |
| FM | 56.25 (15.21) |
68.28 (26.57) |
51.32 (14.27) |
55.33 (19.01) |
14.80*** | 1.09 | 3.69 | 0.55 |
SD: Standard deviation; PB-ESDM: preschool-based Early Start Denver Model; MDI: multidisciplinary developmental intervention; DQ: developmental quotient; RL: receptive language; EL: expressive language; VR: visual reception; FM: fine motor.
p < 0.05, **p < 0.01, ***p < 0.001.
Figure 1.
Mean pre- and post-intervention standard scores of (a) MSEL overall DQ, (b) receptive language DQ, and (c) expressive language DQ.
**p < 0.01; ***p < 0.001.
VABS-II parent report
Adaptive behavior composite
The ANOVA yielded an overall main effect for time (F(1, 45) = 7.59, p < 0.01, d = 0.81), with both groups showing a significant increase in the parent-reported overall adaptive score. The main effect for group (F(1, 45) = 3.23, p = ns) as well as the time × group interaction effect (F(1, 45) = 0.87, ns) did not reach significance.
Domain scores
The domain score analyses, detailed in Table 3, yielded significant main effects of time for the communication, daily living skills, and socialization domains, but not for the motor skills domain. A significant time × group interaction effect was found for the VABS-II socialization domain. Post hoc analyses with Bonferroni correction have shown an increase in parent-reported socialization skills in the PB-ESDM group (mean difference i − j = 8.25, SE = 1.91, p < 0.001), while the increase in those skills in the MDI groups was not significant (mean difference i − j = 1.74, SE = 1.95, ns). This effect is illustrated in Figure 2.
Table 3.
Means (SDs) of pre- and post-intervention parent-reported VABS-II domain scores.
| PB-ESDM | MDI | Time | Time × group | |||||
|---|---|---|---|---|---|---|---|---|
| Measure | Pre | Post | Pre | Post | F(1, 45) | d | F(1, 45) | d |
| Adaptive behavior composite | 70.33 (8.52) |
75.25 (14.00) |
66.09 (7.74) |
68.52 (13.90) |
7.59** | 0.81 | 0.87 | 0.29 |
| Communication | 75.21 (15.24) |
79.58 (20.56) |
67.70 (13.31) |
71.70 (19.52) |
6.42* | 0.77 | 0.01 | 0 |
| Daily living skills | 71.17 (10.74) |
77.54 (16.60) |
67.65 (10.22) |
70.13 (14.32) |
8.32** | 0.87 | 1.61 | 0.41 |
| Socialization | 70.71 (8.73) |
78.96 (13.88) |
68.17 (10.16) |
69.91 (14.99) |
13.46** | 1.09 | 5.72* | 0.70 |
| Motor skills | 77.33 (9.65) |
76.13 (11.60) |
73.00 (7.42) |
73.70 (10.21) |
003. | 0.06 | 038. | 0.20 |
SD: standard deviation; PB-ESDM: preschool-based Early Start Denver Model; MDI: multidisciplinary developmental intervention.
p < 0.05; **p < 0.01
Figure 2.
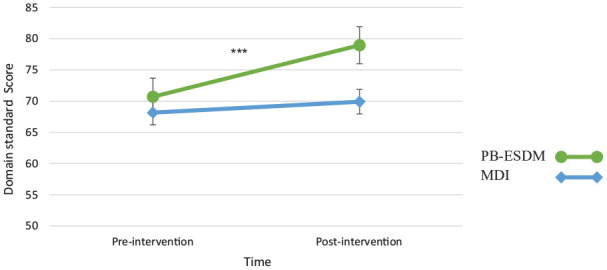
Mean pre- and post-intervention standard scores on the parent-reported VABS-II socialization domain.
***p < 0.001.
VABS-II teacher report
Adaptive behavior composite
The ANOVA yielded an overall main effect for time (F(1, 49) = 17.29, p < 0.001, d = 1.22), with both groups showing a significant increase in the teacher-reported overall adaptive score. The main effect for group (F(1, 49) = 0.89, p = ns), and the time × group interaction effect (F(1, 49) = 1.67, p = ns) did not reach significance.
Domain scores
The analyses, presented in Table 4, revealed a significant main effect for time for the communication, daily living skills, and socialization domains. No main effects for group were found significant. In addition, as illustrated in Figure 3, a significant time × group interaction was found for the communication domain.
Table 4.
Means (SDs) of pre- and post-intervention teacher-reported VABS-II domain scores.
| PB-ESDM | MDI | Time | Time × group | |||||
|---|---|---|---|---|---|---|---|---|
| Measure | Pre | Post | Pre | Post | F(1, 46) | d | F(1, 46) | d |
| Adaptive behavior composite | 66.81 (11.21) |
72.88 (13.80) |
65.21 (9.54) |
67.96 (13.18) |
17.09*** | 1.19 | 2.42 | 0.46 |
| Communication | 69.04 (16.50) |
77.68 (20.30) |
64.04 (15.84) |
67.87 (17.59) |
19.99*** | 1.40 | 5.47* | 0.67 |
| Daily living skills | 70.15 (14.57) |
77.08 (15.44) |
66.61 (13.37) |
68.78 (14.77) |
8.35** | 0.87 | 3.05 | 0.50 |
| Socialization | 65.08 (9.84) |
71.48 (15.61) |
63.65 (8.12) |
68.13 (13.80) |
16.31*** | 1.15 | 0.73 | 0.29 |
| Motor skills | 74.88 (12.00) |
75.72 (13.04) |
77.48 (13.56) |
78.83 (14.18) |
0.42 | 0.20 | 0.01 | 0 |
PB-ESDM: preschool-based Early Start Denver Model; MDI: multidisciplinary developmental intervention.
p < 0.05; **p < 0.01; ***p < 0.001.
Figure 3.
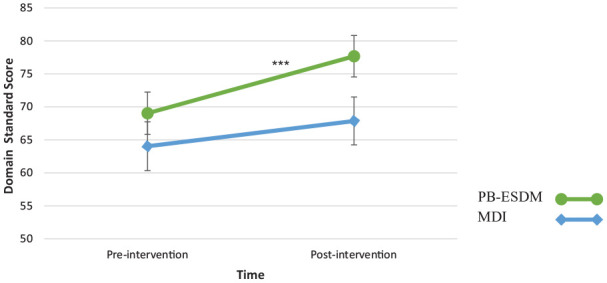
Mean pre- and post-intervention standard scores on the preschool-reported VABS-II communication domain.
***p < 0.001.
Post hoc analyses with Bonferroni correction have shown a statistically significant improvement in the communication domain for the PB-ESDM group (mean difference i − j = 9.04, SE = 1.86, p < 0.001) but not for the MDI group (mean difference i − j = 2.83, SE = 1.90, p = ns).
Treatment response profile analysis
In order to identify outcome predictors, we examined the profiles of children who made substantial developmental progress with treatment (high responders) and children whose progress was comparatively modest or those who did not make progress with treatment (low responders). We used the “slope-discrepancy” approach (Fuchs & Deshler, 2007; Jimerson et al., 2016), which focuses on the discrepancy between the developmental rate during the treatment period and the developmental rate that would be expected in the absence of treatment. This method has been employed with different populations, including autism (Klintwall et al., 2015). Treatment response was calculated for each child as follows
First, the child’s observed developmental treatment-related gain was calculated by subtracting pre- from post-intervention overall MSEL AE. Then, the child’s expected developmental rate (in months) without treatment was calculated based on her pre-treatment overall MSEL DQ score, divided by a 100 (to create a percentage score) and multiplied by the 8 months of intervention. Children whose observed intervention-related developmental gain superseded their expected developmental rate were classified as high responders, whereas children whose observed developmental intervention-related gain fell below their expected developmental gain were classified as low responders. For example, the expected developmental rate (following 8 months of intervention) of a child whose initial DQ was 75 would be 6 months (75/100 × 8 = 6). If this child’s overall AE increased by more than 6 months, she was classified as a high-treatment responder.
Based on this classification, 20 participants (80%) from the PB-ESDM group and 14 participants from the MDI group (56%) were classified as HR. This group difference did not reach significance (χ2 (1) 1.98, ns).
Next, in order to examine the profiles of high responders and low responders in the PB-ESDM group, independent-sample t-tests were conducted with response group as the independent variable. The dependent variables were selected based on prior literature regarding early intervention outcome predictors, including age at entry, ADOS comparison score, total MSEL and subscales DQ, and parent and teacher reports in the VABS-II (Fossum et al., 2017; Reichow et al., 2012; Smith et al., 2015; Vivanti et al., 2016). In addition, chi-square tests were conducted to check gender differences between the two groups and differences in prior exposure to MDI and external treatment received during the intervention. As shown in Table 5, before the intervention, treatment high responders had lower ADOS scores and higher MSEL and VABS-II scores, compared to treatment low responders.
Table 5.
Baseline differences between high and low responders on the PB-ESDM group.
| Measure | High responders (n = 20) | Low responders (n = 6) | t(25) |
|---|---|---|---|
| Gender (girls:boys) | 5:15 | 1:5 | χ2 = 0.67, ns |
| Age (months) | 41.67 (7.81) | 44.25 (7.32) | 0.75 |
| External treatment (h) | 0.70 (0.98) | 0.83 (0.75) | 0.31 |
| Previous exposure to MDI (%) | 41.2% | 37.5% | χ2 = 0.90, ns |
| ADOS CSS | 6.50 (1.28) | 9.17 (1.28) | 4.69*** |
| MSEL total DQ | 59.69 (16.20) | 34.82 (13.71) | 3.4** |
| MSEL VR DQ | 62.85 (16.04) | 38.72 (18.62) | 3.12* |
| MSEL FM DQ | 60.12 (13.69) | 43.33 (13.57) | 2.64* |
| MSEL RL DQ | 60.01 (28.94) | 28.94 (16.90) | 3.14** |
| MSEL EL DQ | 54.40 (21.80) | 28.29 (16.91) | 2.68* |
| VABS-II-P composite | 72.94 (6.881) | 61.17 (6.55) | 3.70** |
| VABS-II-T composite | 72.95 (15.15) | 56.00 (14.95) | 2.31* |
MDI: multidisciplinary developmental intervention; ADOS-CSS: autism diagnostic observation schedule calibrated severity score; MSEL: Mullen’s scales of early learning; DQ: developmental quotient; VR: visual reception; FM: fine motor; RL: receptive language; EL: expressive language; VABS-II-P: Vineland adaptive behavior scales, second edition, parent report; VABS-II-T: Vineland adaptive behavior scales, second edition, teacher report.
p < .05; **p < .01; ***p < .001
Discussion
This study examined the effectiveness of the PB-ESDM, a preschool-based adaptation of the ESDM, and its integration into Israeli community ASD preschool settings. The effects of the PB-ESDM were compared to the effects of existing ASD preschools, which employ a MDI. In addition, this study examined high and low treatment response profiles to the PB-ESDM.
Compared to children in the MDI group, children who received the PB-ESDM made significantly higher gains in overall cognitive functioning and in the MSEL receptive and expressive scales. Parent-reported VABS-II socialization domain scores significantly increased with treatment among children from the PB-ESDM preschools but not in the MDI group. Finally, we found that children from the PB-ESDM group showed a significant intervention-related increase in teacher-reported VABS-II communication domain scores which were not found in the MDI group.
These results stand in line with prior research regarding the effectiveness of ESDM-based programs in community or low-intensity settings (Colombi et al., 2018; Holzinger et al., 2019; Vivanti et al., 2014). This study also adds to the growing body of knowledge supporting the successful implementation of the ESDM in non-English speaking countries.
The effects reported in this study highlight the effectiveness of the ESDM in addressing the core difficulties of social communication that characterize ASD. Specifically, improvements found on expressive and receptive communication, as assessed by the MSEL, and on socialization and communication skills, as assessed by the VABS-II, exceeded those of the MDI group. Notably, no differential effects were found in other domains the ESDM aims to target, such as motor skills. A similar pattern was found by Vivanti et al. (2014), where higher increases were shown in the ESDM group for the overall MSEL score and the RL subscale after 12 months of group-delivered ESDM intervention. Dawson et al. (2010) reported differential effects for the total DQ and the VR subscale, with a near-significant effect for the receptive language scale, and differential effects in other measures (i.e. RL and EL, ABC, communication, daily living, and motor skills) manifested after 24 months of intensive 1:1 intervention. A follow-up examination of our participants after 2 years of PB-ESDM may indicate if similar results can be found in this format.
A recent multisite randomized controlled trial by Rogers et al. (2019) compared the outcomes of children receiving a 1:1 high-intensity ESDM treatment and those of children receiving community interventions for a period of 24 months. The ESDM group showed significantly higher gains in language skills than the community intervention group. However, no differences were found between the two groups in gains on DQ, adaptive skills or ASD symptom severity. Although the authors did not describe in detail the nature of the community intervention, they proposed that the limited superiority of the ESDM on intervention gains may be due to improved services delivered by community settings in the studied sites in the United States, as compared to the Dawson et al. (2010) study. Notably, in this study, the treatment-as-usual group was less heterogeneous than in Rogers et al. (2019), since it was operated by the same organization. This is possibly the reason the differences between the groups reported here were more pronounced.
This study also looked into specific response profiles of children receiving the PB-ESDM. Most of the children who received the PB-ESDM responded to it well. However, a small but still substantial subgroup of children made slower progress in the time they have received the PB-ESDM. These children, the low-response group, had lower initial developmental levels, in both verbal and nonverbal scales. The severity of their autism symptoms was significantly higher than that of the high-response group, and their adaptive functioning was lower. Interestingly, the two groups did not differ on age or gender, though all but one of the female participants belonged to the high responders’ group.
Our results suggested that intervention for children who have higher ADOS calibrated severity scores, lower adaptive behavior scores, and poorer developmental skills may need to be further facilitated in order for these children to demonstrate significant progress. Several such amendments were suggested for children who do not make sufficient progress with treatment. These include increasing treatment dose or intensity (Lovaas, 1993), augmenting treatment using alternative and augmentative communication technology (Kasari et al., 2014), and delivering interventions through multiple agents (e.g. therapists, parents, teachers, etc.) at different settings (Kasari et al., 2018).
The ESDM manual (Rogers & Dawson, 2010) guides for an increase in teaching structure and changes in the rewarding method (from naturalistic to object based) when a child does not acquire a learning objective in a set time period (usually 12 weeks). The option for more structured intervention methods with higher degrees of support for children who do not make sufficient progress was also raised by other researchers exploring treatment individualization (e.g. Stahmer et al., 2011).
As mentioned above, a potential adaptation to consider is that of treatment dosage and duration. Children from the low-response group may have needed more hours per week and/or a longer duration of the intervention they were already receiving. Studies exploring the effects of behavioral interventions supported the notion that higher intensity and longer term interventions are related to better treatment outcomes (Linstead et al., 2016; Virués-Ortega et al., 2013). Since children in Israeli ASD community preschools attend these settings for a significant amount of time (about 44 h a week), “higher intensity” might translate to a greater dosage of 1:1 pull-out treatment during the school day. Additional treatment time could be provided after school. However, ecologically—this may prove detrimental for the familial climate and routine (Pellecchia et al., 2019).
While this study defined treatment response as gains made in a global measure of cognitive abilities, a question arises regarding the sensitivity of such measures to the different aspects of change occurring with treatment. The MSEL is a distal outcome measure, that is, a tool designed to measure overall generalized skills that are not necessarily taught during treatment (Fletcher-Watson & McConachie, 2017). Arguably, children from the low-response group may have improved in various skills, which were not spotted by the assessment methods chosen in this study. It is possible that other, more proximal, or sensitive fine-grained measures could have detected significant changes in various skills with treatment (e.g. microanalytic observation of behaviors at different time points; Berman et al., 2018). Future research should combine proximal and distal measures in its outcome assessment. In addition, the exploration of low response to intervention should also question what counts as a good treatment outcome or as a treatment success, while also considering child characteristics, parental priorities, and clinicians’ professional input.
One limitation of this work is its quasi-experimental design. While every measure was taken to match both groups at their pre-intervention characteristics, randomized studies enable researchers to draw stronger conclusions regarding intervention effectiveness. However, full randomization is difficult to attain in community intervention research. Future studies might employ cluster randomization at the setting level, which can be more feasible in this sort of research (Dingfelder & Mandell, 2011). Furthermore, since different preschool teams implemented the two interventions in each setting, a multi-level modeling approach would have been preferable for the analysis of the combined effects of setting and intervention type. However, following guidelines on multilevel modeling (Maas & Hox, 2005), a multilevel modeling approach could not be applied to our data given the relatively small cluster sizes (4–9 children assessed within each preschool setting). Also, an examination of the effects of different covariates on treatment effects was not conducted so not to lose statistical power, given the limited sample size. Future research using larger samples should address these limitations.
This study still leaves the issue of the “active ingredients” (Vivanti, Kasari, et al., 2017) in the ESDM, unclear. As in previous studies, the MDI group in this work differed from the PB-ESDM group on several elements: model manualization, the existence of criteria for treatment fidelity, the active involvement of parents in treatment, and methods of progress assessment in the learning curriculum. Theoretically, any one of these factors may have a beneficial impact on children’s developmental trajectories. Future research should attempt to examine the role of various elements of the ESDM, such as parental involvement effects, on changes in developmental rates. For example, the intervention described by Vivanti et al. (2014) did not include routine parent involvement and still showed significant increases in developmental rates among treated children. The active ingredient question is of great importance in community implementation of intervention, where resources are limited and the provision of full CTMs may not be easily attained. Pinpointing specific mechanisms through which the ESDM works can allow community settings to prioritize critical treatment elements and more readily incorporate them in daily practice.
This study adds to the accumulating research showing that children with greater developmental, adaptive, and communicative abilities also make greater gains with intervention. Notably, while this study mainly focused on non-modifiable response predictors, future research should focus on those factors which are modifiable and can augment treatment effects for low responders, such as treatment intensity, duration, or the use of additional intervention components. Such an examination can be made, using a sequential multiple assignment randomized trial (SMART) research design, in which treatment adaptations are made based on ongoing analysis of children’s progress and needs (Kasari et al., 2018). Future studies may utilize the SMART model to examine a more flexible implementation of the PB-ESDM, in accordance with children’s individual needs.
Another possible approach to the isolation of active treatment ingredients is the prospective examination of high and low response to the PB-ESDM, based on the factors identified in this study. In this sort of research, children are allocated to interventions according to their initial developmental profile (Fossum et al., 2017). This sort of approach was implemented in prior research, for example, by Sherer and Schreibman (2005) and Schreibman et al. (2009), with promising results.
It is, however, important to note that the incorporation of evidence-based intervention into community settings in Israel is still in the early stages of implementation and dissemination. Hence, the effectiveness of the PB-ESDM as an evidence-based CTM was the main focus of our study. Future studies may methodically explore outcome predictors of the Israeli PB-ESDM and its adaptations according to pre-treatment profiles.
Finally, this study did not address the question of implementation feasibility and the social validity of the PB-ESDM. This sort of exploration is significant in community implementation of evidence-based practice, as it has implications on treatment adherence, sustainability, and the overall success of the dissemination process. Future research exploring the PB-ESDM should address these important issues.
To conclude, a significant contribution of this study lies in its integration of an evidence-based treatment model into existing community ASD preschools. Our encouraging findings may have important implications for policy makers to facilitate further research and to integrate research-based practices into existing community settings.
Acknowledgments
We would like to thank the Autism and Research Center, Association for Children at Risk, and the Harry and Jeanette Weinberg Foundation for supporting the implementation of ESDM in Israeli preschools. Thanks to Dr. Michal Rapoport for her cooperation in this project. We would also like to thank Omer Yaacov, Danit Turgeman, Adi Dangoor, and Mattan Ben-Yosef for their invaluable contribution to this study. We thank all staff members of the participating preschools for their cooperation and hospitality. Finally, we would like to thank the children participating in the study, and their families, for generously giving their time and patience to this study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The first author was supported by Bar-Ilan University president’s scholarship.
ORCID iD: Ofer Golan  https://orcid.org/0000-0001-8760-5691
https://orcid.org/0000-0001-8760-5691
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Anagnostou E., Zwaigenbaum L., Szatmari P., Fombonne E., Fernandez B. A., Woodbury-Smith M., . . . Scherer S. W. (2014). Autism spectrum disorder: Advances in evidence-based practice. Canadian Medical Association Journal, 186(7), 509–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baio J., Wiggins L., Christensen D. L., Maenner M. J., Daniels J., Warren Z., . . . Durkin M. S. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Itzchak E., Zachor D. A. (2011). Who benefits from early intervention in autism spectrum disorders? Research in Autism Spectrum Disorders, 51(1), 345–350. [Google Scholar]
- Berman S., Ventola P., Gordon I. (2018). Improvements in micro level indices of social communication following pivotal response treatment (PRT). Research in Autism Spectrum Disorders, 51, 56–65. [Google Scholar]
- Chang Y., Shire S., Shih W., Gelfand C., Kasari C. (2016). Preschool deployment of evidence-based social communication intervention: JASPER in the classroom. Journal of Autism and Developmental Disorders, 46(6), 2211–2233. [DOI] [PubMed] [Google Scholar]
- Colombi C., Narzisi A., Ruta L., Cigala V., Gagliano A., Pioggia G., & . . . Prima Pietra Team. (2018). Implementation of the Early Start Denver Model in an Italian community. Autism, 22(2), 126–133. [DOI] [PubMed] [Google Scholar]
- Dawson G., Rogers S. J., Munson J., Smith M., Winter J., Greenson J., . . . Varley J. (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125(1), e17–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingfelder H. E., Mandell D. S. (2011). Bridging the research-to-practice gap in autism intervention: An application of diffusion of innovation theory. Journal of Autism and Developmental Disorders, 41, 597–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan H. E., Perry A., Freeman N. L. (2012). Effectiveness of large-scale community-based intensive Behavioral Intervention: A waitlist comparison study exploring outcomes and predictors. Research in Autism Spectrum Disorders, 6(2), 673–682. [Google Scholar]
- Fletcher-Watson S., McConachie H. (2017). The search for an early intervention outcome measurement tool in autism. Focus on Autism and Other Developmental Disabilities, 32(1), 71–80. [Google Scholar]
- Fossum K., Williams L., Garon N., Smith I. M. (2017). Pivotal response treatment for preschoolers with autism spectrum disorder: Defining a predictor profile. Autism Research, 11(1), 153–165. [DOI] [PubMed] [Google Scholar]
- Freeman S., Kasari C. (2013). Parent–child interactions in autism: Characteristics of play. Autism, 17(2), 147–161. [DOI] [PubMed] [Google Scholar]
- Fuchs D., Deshler D. D. (2007). What we need to know about responsiveness to intervention (and shouldn’t be afraid to ask). Learning Disabilities Research & Practice, 22(2), 129–136. [Google Scholar]
- Greenspan S. I., Wieder S. (2005). Engaging autism: The Floortime approach to helping children relate, communicate and think. Perseus Books. [Google Scholar]
- Holzinger D., Laister D., Fellinger J., Vivanti G., Barbaresi W. (2019). Feasibility and outcomes of the Early Start Denver Model implemented with low intensity in a community setting in Austria. Journal of Developmental and Behavioral Pediatrics, 40(5), 354–363. [DOI] [PubMed] [Google Scholar]
- Hudry K., McConachie H., Le Couteure A., Howlin P., Barret B., Slonims V.,& The PACT Consortium. (2018). Predictors of reliable symptom change: Secondary analysis of the Preschool Autism Communication Trial. Autism and Developmental Language Impairments, 3, 1–12. [Google Scholar]
- Ingersoll B. (2010). Pilot randomized controlled trial of reciprocal imitation training for teaching elicited and spontaneous imitation to children with autism. Journal of Autism and Developmental Disorders, 40(9), 1154–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimerson S. R., Burns M. K., VanDerHeyden A. M. (2016). From response to intervention to multi-tiered systems of support: Advances in the science and practice of assessment and intervention. In Jimerson S. R., Burns M. K., VanDerHeyden A. M. (Eds.), Handbook of response to intervention (pp. 1–6). Springer. [Google Scholar]
- Kasari C., Kaiser A., Goods K., Nietfeld J., Mathy P., Landa R., . . . Almirall D. (2014). Communication interventions for minimally verbal children with autism: A sequential multiple assignment randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(6), 635–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C., Paparella T., Freeman S., Jahromi L. B. (2008). Language outcome in autism: Randomized comparison of joint attention and play interventions. Journal of Consulting and Clinical Psychology, 76(1), 125–137. [DOI] [PubMed] [Google Scholar]
- Kasari C., Sturm A., Shih W. (2018). SMARTer approach to personalizing intervention for children with autism spectrum disorder. Journal of Speech, Language and Hearing Research, 61(11), 2629–2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klintwall L., Eldevik S., Eikeseth S. (2015). Narrowing the gap: Effects of intervention on developmental trajectories in autism. Autism, 19(1), 53–63. [DOI] [PubMed] [Google Scholar]
- Laor N., Nagel-Edelstein T., Barzilay R., Golan O. (2017). Israel and autism. In Volkmar F. R. (Ed.), Encyclopedia of autism spectrum disorders (pp. 1–9). Springer; 10.1007/978-1-4614-6435-8_102030-1 [DOI] [Google Scholar]
- Linstead E., Dixon D. R., French R., Granpeesheh D., Adams H., German R., . . . Kornack J. (2016). An evaluation of the relationship between intensity and learning outcomes in the treatment of autism spectrum disorder. Behavior Modification, 41, 229–252. [DOI] [PubMed] [Google Scholar]
- Lord C., Rutter M., DiLavore P., Risi S., Gotham K., Bishop S. L. (2012). Autism Diagnostic Observation Schedule, Second edition (ADOS-2) manual. Western Psychological Services. [Google Scholar]
- Lord C., Schopler E. (1989). The role of the age at assessment, developmental level, and test in the stability of intelligence scores in young autistic from preschool years through early school age. Journal of Autism and Developmental Disorders, 18, 234–253. [DOI] [PubMed] [Google Scholar]
- Lovaas O. I. (1993). The development of a treatment-research project for developmentally disabled and autistic children. Journal of Applied Behavior Analysis, 26(4), 617–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas C. J., Hox J. J. (2005). Sufficient sample sizes for multilevel modeling. Methodology, 1(3), 86–92. [Google Scholar]
- Mohammadzaheri F., Koegel L. K., Rezaei M., Bakhshi E. (2015). A randomized clinical trial comparison between pivotal response treatment (PRT) and adult-driven applied behavior analysis (ABA) intervention on disruptive behaviors in public school children with autism. Journal of Autism and Developmental Disorders, 45(9), 2899–2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen E. M. (1995). Mullen Scales of Early Learning (AGS ed.). American Guidance Service. [Google Scholar]
- Nygren G., Cederlund M., Sandberg E., Gillstedt F., Arvidsson T., Gillberg I. C., . . . Gillberg C. (2012). The prevalence of Autism Spectrum Disorders in toddlers: A population study of 2-year-old Swedish children. Journal of Autism and Developmental Disorders, 42(7), 1491–1497. [DOI] [PubMed] [Google Scholar]
- Odom S. L., Boyd B., Hall L. J., Hume K. (2010). Evaluation of comprehensive treatment models for individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 40, 425–436. [DOI] [PubMed] [Google Scholar]
- Pellecchia M., Iadarola S., Stahmer A. C. (2019). How meaningful is more? Considerations regarding intensity in early intensive behavioral intervention. Autism, 23, 1075–1078. [DOI] [PubMed] [Google Scholar]
- Ratner N., Bruner J. (1978). Games, social exchange, and the acquisition of language. Journal of Child Language, 5, 391–402. [DOI] [PubMed] [Google Scholar]
- Raz R., Weisskopf M. G., Davidovitch M., Pinto O., Levine H. (2015). Differences in autism spectrum disorders incidence by sub-populations in Israel 1992–2009: A total population study. Journal of Autism and Developmental Disorders, 45(4), 1062–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichow B., Barton E. E., Boyd B. A., Hume K. (2012). Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). The Cochrane Database of Systematic Reviews, 10,CD009260. [DOI] [PubMed] [Google Scholar]
- Rogers S. J., Dawson G. (2010). Early Start Denver Model for Young Children with Autism. Promoting language, learning and engagement. Guilford Press. [Google Scholar]
- Rogers S. J., Estes A., Lord C., Munson J., Rocha M., Winter J., . . . Talbott M. (2019). A Multisite randomized controlled two-phase trial of the Early Start Denver Model compared to treatment as usual. Journal of the American Academy of Child & Adolescent Psychiatry, 58(9), 853–865. [DOI] [PubMed] [Google Scholar]
- Rogers S. J., Estes A., Lord C., Vismara L., Winter J., Fitzpatrick A., . . . Dawson G. (2012). Effects of a brief Early Start Denver model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 51(10), 1052–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibman L., Stahmer A. C., Barlett V. C., Dufek S. (2009). Brief report: Toward refinement of a predictive behavioral profile for treatment outcome in children with autism. Research in Autism Spectrum Disorders, 3(1), 163–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherer M. R., Schreibman L. (2005). Individual behavioral profiles and predictors of treatment effectiveness for children with autism. Journal of Consulting and Clinical Psychology, 73(3), 528–538. [DOI] [PubMed] [Google Scholar]
- Smith T., Klorman R., Mruzek D. W. (2015). Predicting outcome of community-based early intensive behavioral intervention for children with autism. Journal of Abnormal Child Psychology, 43(7), 1271–1282. [DOI] [PubMed] [Google Scholar]
- Sparrow S. S., Cicchetti D. V., Balla D. A. (2005). Vineland-II Adaptive Behavior Scales: Survey forms manual. AGS Publishing. [Google Scholar]
- Stahmer A. C. (2007). The basic structure of community early intervention programs for children with autism: Provider descriptions. Journal of Autism and Developmental Disorders, 37, 1344–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer A. C., Schreibman L., Cunningham A. B. (2011). Toward a technology of treatment individualization for young children with autism spectrum disorders. Brain Research, 1380, 229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suhrheinrich J., Hall L. J., Reed S. R., Stahmer A. C., Schreibman L. (2014). Evidenced based interventions in the classroom. American Psychological Association. [Google Scholar]
- Tiura M., Kim J., Detmers D., Baldi H. (2017). Predictors of longitudinal ABA treatment outcomes for children with autism: A growth curve analysis. Research in Developmental Disabilities, 70, 185–197. [DOI] [PubMed] [Google Scholar]
- Virués-Ortega J., Rodríguez V., Yu C. T. (2013). Prediction of treatment outcomes and longitudinal analysis in children with autism undergoing intensive behavioral intervention. International Journal of Clinical Health Psychology, 13, 91–100. [Google Scholar]
- Vismara L. A., Young G. S., Rogers S. J. (2012). Telehealth for expanding the reach of early autism training to parents. Autism Research and Treatment, 2012, 121878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vivanti G., Dissanayake C., Duncan E., Feary J., Upson S., Bent C. A., . . . Hudry K. (2018). Outcomes of children receiving Group-Early Start Denver Model in an inclusive versus autism-specific setting: A pilot randomized controlled trial. Autism, 23(5), 1165–1175. [DOI] [PubMed] [Google Scholar]
- Vivanti G., Dissanayake C. The Victorian ASELCC Team, M. V. A. (2016). Outcome for children receiving the Early Start Denver Model before and after 48 months. Journal of Autism and Developmental Disorders, 46(7), 2441–2449. [DOI] [PubMed] [Google Scholar]
- Vivanti G., Dissanayake C., Zierhut C., Rogers S. J. Victorian ASELCC Team. (2013). Brief Report: Predictors of outcomes in the Early Start Denver Model delivered in a group setting. Journal of Autism and Developmental Disorders, 43, 1717–1724. [DOI] [PubMed] [Google Scholar]
- Vivanti G., Duncan E., Dawson G., Rogers S. J. (2017). Implementing the group-based Early Start Denver Model for preschoolers with autism. Springer. [Google Scholar]
- Vivanti G., Kasari C., Green J., Maye M., Hudry K. (2017). Implementing and evaluating early intervention for children with autism: Where are the gaps and what should we do? Autism Research, 11(1), 16–23. [DOI] [PubMed] [Google Scholar]
- Vivanti G., Paynter J. M., Duncan E., Fothergill H., Dissanayake C., Rogers S. J.,&. the Victorian ASELCC Team. (2014). Effectiveness and feasibility of the Early Start Denver Model implemented in a group-based community childcare setting. Journal of Autism and Developmental Disorders, 44, 3140–3153. [DOI] [PubMed] [Google Scholar]