Abstract
Background:
The health of caregivers can be affected during end-of-life caregiving. Previous cross-sectional studies have indicated an association between poor health status and prolonged grief disorder, but prospective studies are lacking.
Aim:
To describe physical and mental health status in caregivers of patients at the end of life, and to investigate whether caregivers’ health status during caregiving predict prolonged grief disorder.
Design:
A population-based prospective survey was conducted. Health status was measured in caregivers during caregiving (SF-36), and prolonged grief disorder was assessed 6 months after bereavement (Prolonged Grief-13). We calculated mean scores of health status and explored the association with prolonged grief disorder using logistic regression adjusted for age, gender and education.
Setting/participants:
The health in caregivers of patients granted drug reimbursement due to terminal illness in Denmark in 2012 was assessed during caregiving and 6 months after bereavement (n = 2125).
Results:
The SF-36 subscale ‘role-physical’ concerning role limitations due to physical health, the ‘mental health’ component score, and all ‘mental health’ subscales showed significantly worse health in the participants than in the general population. Both poor physical health (adjusted OR: 1.05 (95% CI: 1.04–1.07)) and poor mental health (adjusted OR: 1.09 (95% CI: 1.07–1.11)) predicted prolonged grief disorder.
Conclusion:
Caregivers scored lower on one physical subscale and all mental health measures than the general population. Prolonged grief disorder was predicted by poor physical and mental health status before bereavement. Future research is needed on the use of health status in systematic assessment to identify caregivers in need of support.
Keywords: Caregivers, palliative care, health status, mental health, bereavement, grief, surveys and questionnaires
What is already known about the topic?
End-of-life caregiving may affect the physical health in the caregivers, but the role of physical health status as a predictor of prolonged grief disorder remains unclear.
Previous studies have revealed poorer mental health in caregivers of end-of-life patients than in the general population and several aspects of poor mental health have been shown to predict prolonged grief disorder.
Cross-sectional studies have indicated a link between health status and prolonged grief disorder, but the association has not been examined prospectively.
What this paper adds?
Caregivers providing end-of-life care were limited in the daily activities due to their physical health compared to the general population.
Poor physical health during caregiving predicted prolonged grief disorder.
The mental health was worse in caregivers than in the general population, and poor mental health during caregiving predicted prolonged grief disorder.
Implications for practice, theory or policy
Both physical and mental health status of caregivers in end-of-life trajectories should be addressed in the care for caregivers.
Future research should include systematic assessments of health status to identify caregivers at risk of developing prolonged grief disorder.
Early identification of caregivers in need of support may provide new opportunities for early prevention.
Background
Losing a close relative will naturally cause grief. For most people, the grief reaction will decrease over time.1 However, some people are at risk of developing prolonged grief disorder (PGD), which is characterised by an intense emotional response that persists for an unusual long time and impairs daily functioning.1,2 Moreover, the World Health Organization (WHO) has included PGD as a diagnosis in the 11th revision of the International Classification of Diseases (ICD-11).2–4 Up to 6–10% of bereaved people suffer from the condition5–8 with severe consequences for the physical and mental health, that is, heart disease, depression and suicidal behaviour.2,9–12
To limit negative health impact of grief reactions, it is essential to identify people at risk of PGD already in the caregiving period, which will allow initiation of preventative interventions.13–16 One prior review indicated that interventions pre-death might lead to lower levels of PGD.13 Hence, studies are needed to investigate how to identify caregivers at risk of PGD. Previous studies have identified several risk factors of PGD, including female gender,15,17,18 close relationship with the deceased, specifically being a partner,5,6,15,17,19 and low income or low educational level.5,6,15 Other risk factors are level of depression or anxiety in the caregiver before bereavement,5,15,17,20 severe pre-death grief symptoms,5,6,21 lack of preparedness for death,17,18,20,21 young age of the deceased6,17 and insecure attachment style.17,19,22
Previous studies have explored the health status of caregivers in end-of-life trajectories and indicated poorer health status in caregivers than in the general population.23–26 However, only two previous studies have indicated an association between poor self-reported health in caregivers and PGD.18,27 Both studies were cross-sectional and conducted after bereavement; one assessed health status before bereavement in a retrospective study design, whereas the other only examined health status after bereavement. Hence, a prospective study investigating whether caregivers’ health status during caregiving is a predictor of PGD could increase knowledge in this area and support prevention.
We aimed to describe the physical and mental health status in caregivers of patients at the end of life and to investigate whether health status may predict PGD. Based on previous research,18,27 we hypothesised to find an association between poor physical and mental health in caregivers before bereavement and development of PGD after bereavement.
Methods
Design
The study was a population-based prospective cohort study and was based on data from caregivers to terminally ill patients in Denmark.
Setting
All residents in Denmark have free access to public healthcare, which is tax-funded. Medications are free of charge during hospital admission, whereas medications bought at pharmacies are part of a reimbursement system depending on pharmaceutical consumption per person.28 If a patient is incurably ill with a life expectancy of a few months, a physician can apply for full drug reimbursement for the patient to the Danish Medicines Agency.29 In 2012, approximately 12.000 Danish citizens received drug reimbursement due to terminal illness.30 A prior Danish study found that 27.9% of all dying patients in the period 2006–2015 received full drug reimbursement.31
Participants and sampling period
From 1 January to 31 December 2012, an invitation letter with a baseline questionnaire was systematically sent to eligible patients receiving full drug reimbursement due to terminal illness.
Approximately 9000 patients were expected to be eligible29 and to enable a sample size with the possibility of identifying meaningful clinical differences.
The patients were asked to request their closest adult caregiver to return a completed questionnaire, including written informed consent.30 Vital status of patients to participating caregivers were continuously checked in the Danish Civil Registration System and caregivers to patients who had died within 6 months was send a follow-up questionnaire. Follow-up ended in January 2014.
Data sources and variables
Questionnaire data and register-based data were merged through the Danish personal identification number (CPR).32 Data was linked at the individual level and anonymised through an authorised connection at Statistics Denmark.33
Outcome measure
The outcome measure was PGD in caregivers 6 months after bereavement measured using the five criteria (A-E) of the 13-item Prolonged Grief-13 scale (PG-13) and dichotomised according to whether or not the criteria for PGD were met (yes, no).3,6,34 To meet the criteria, the caregiver must (A) have experienced a loss, (B) experience grief-related yearning daily and (C) daily grief-related yearning must be present at least 6 months after the loss (D). Presence of at least five cognitive, emotional and behavioural symptoms on a daily basis (E) and significant impairment in social, occupational or other important areas of functioning are also mandatory criteria.3,6,34
Questionnaire data
The exposure variable was caregivers’ health status before bereavement measured by the Short Form Health Survey-36 (SF-36).35,36 The SF-36 consists of 36 items, which generate eight subscales: physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE) and mental health (MH). Furthermore, SF-36 scores can be divided into a Physical Component Summary (PCS) and a Mental Component Summary (MCS). Raw scores were reported according to the manual with a range between 0 (worst) and 100 (best) for each subscale. The physical subscale scores (PF, RP, BP, GH) are negatively weighted in calculation of MCS, and the mental subscale scores (VT, SF, RE, MH) are negatively weighted to calculate PCS.35,36 The caregiver’s relation to the patient (partner, adult child, other) was self-reported at baseline.
Register data
Caregivers’ age and gender were calculated from the CPR numbers. Age was divided into four groups (<50, 50–59, 60–69, >70 years old). Information on caregivers’ educational level was categorised into three groups according to the International Standard Classification of Education37 (<10 years, 10–15 years, >15 years of education), and their employment status (working, unemployed, outside the workforce (pensioners, cash benefiters, students)) was obtained for 2012. Information on caregivers’ number of chronic diseases (none, one or more) based on the Charlson Comorbidity Index (CCI) was retrieved through the Danish National Patient Register (NPR).32,38
Statistical methods
Descriptive analyses were performed and presented as proportions for categorical variables and as means with 95% confidence intervals (CIs) for continuous variables. Mean scores and CIs for health status were calculated and compared with SF-36 mean scores from the general population aged 55–64 years (corresponding to the mean age of the study population).39
The association between health status and PGD was estimated in a multivariable logistic regression model. Adjustments were made for caregivers’ age, gender and educational level, as these were not intermediate variables and had previously been found to predict PGD.5,6,15,17,18 The analysis was further stratified on caregivers’ relation to the patient and number of chronic diseases at baseline, as health status during caregiving was hypothesised to have different importance in these groups. Estimates were presented as odds ratios (ORs) with 95% confidence intervals (CIs). SF-36 was interpreted based on a continuous scale, which made the interpretation of ORs based on one-unit difference in the SF-36 scores. Statistical analyses were performed using Stata, version 15.1.
Ethics
The study was approved by the Danish Data Protection Agency (file no.: 2013-41-2603).5,30
The study was not subject to ethical clearance according to The Danish Act on Research Ethics Review of Health Research Projects. The study was conducted according to the International Committee of Medical Journal Editors (ICMJE) guidelines. Results are reported in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines for observational studies.40
Results
Participants
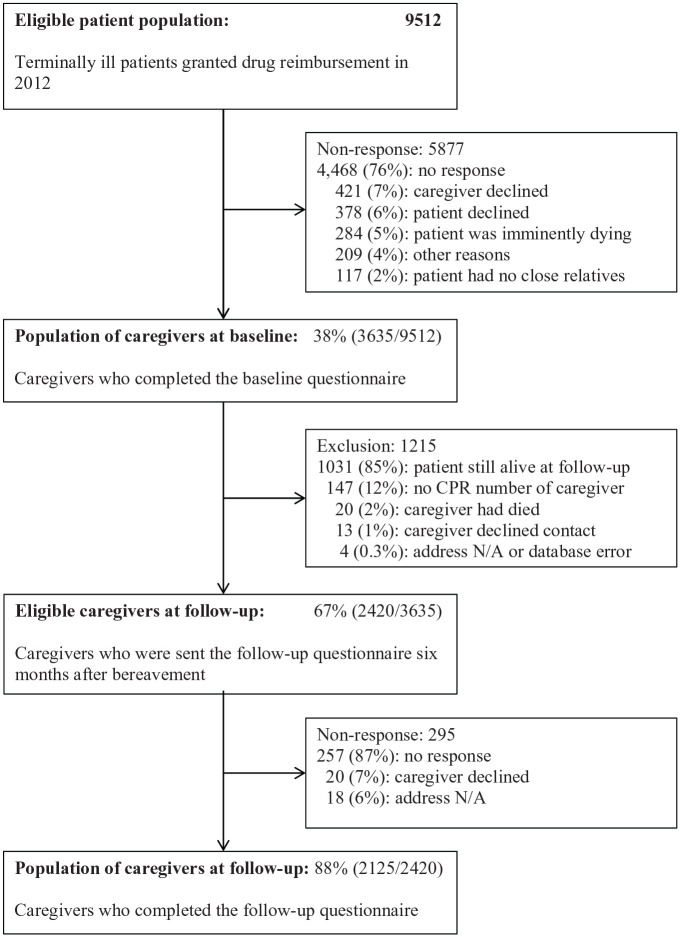
The baseline questionnaire was completed by 3635 caregivers. After 6 months, 2420 caregivers was bereaved and contacted for follow-up. A total of 2125 (88%) caregivers completed the follow-up questionnaire; this group constituted the study population (Figure 1).5
Figure 1.
Flowchart of participating caregivers.
Descriptive data
Mean age of the caregiver cohort was 62 years (95% CI: 61.5–62.6). The majority were females (70%), partners of the patients (64%), and outside the workforce (52%) (Table 1). Approximately 90% of the patients had a cancer diagnosis (lung, colorectal, breast, prostate, haematological, other), and the remaining group predominantly had heart or lung disease.30
Table 1.
Baseline characteristics in the study population of caregivers (N = 2125).
| Characteristics of the caregivers | ||
|---|---|---|
| Mean | 95% CI | |
| Age a | 62.0 | 61.5–62.6 |
| N | % | |
| Age group (years) | ||
| <50 | 354 | 17 |
| 50–59 | 510 | 24 |
| 60–69 | 692 | 32 |
| >70 | 569 | 27 |
| Gender | ||
| Male | 638 | 30 |
| Female | 1,487 | 70 |
| Personal relation to the patient | ||
| Partner | 1,360 | 64 |
| Adult child | 602 | 28 |
| Other | 163 | 8 |
| Educational level b (years of education) | ||
| <10 | 558 | 26 |
| 10–15 | 896 | 42 |
| >15 | 644 | 30 |
| Employment status b | ||
| Working | 989 | 47 |
| Unemployed | 22 | 1 |
| Outside the workforce | 1,114 | 52 |
| Number of chronic diseases c | ||
| None | 1,428 | 67 |
| One or more | 697 | 33 |
CI: confidence interval.
Age at inclusion.
Register-based data for 2012 from national health registers.
Number of chronic diseases based on the Charlson Comorbidity Index (CCI) retrieved through the Danish National Patient Registry (NPR).
Outcome data
The mean PCS score was 51.5 (95% CI: 51.1;51.9) with an absolute difference of 4.1 compared to the general population.39 (Table 2). The mean RP score, that is, role limitations due to physical health, was significantly lower in the caregivers than in the general population, whereas the mean scores in the remaining physical subscales (PF, BP, GH) were non-significantly higher than the corresponding mean scores in the general population.39
Table 2.
| Study population (n = 2125) | General population (n = 494) | |||||
|---|---|---|---|---|---|---|
| Mean | (95% CI) | SD | Mean | (95% CI) | SD | |
| Overall physical health | ||||||
| Physical Component Summary (PCS) | 51.5 | (51.1–51.9) | 10.0 | 47.4 | (43.2–51.6) | 10.4 |
| Physical subscales | ||||||
| Physical functioning (PF) | 84.7 | (83.9–85.6) | 20.7 | 80.7 | (73.6–87.8) | 23.5 |
| Role-physical (RP) | 59.8 | (58.0–61.6) | 41.4 | 75.2 | (68.6–81.8) | 36.5 |
| Bodily pain (BP) | 77.3 | (76.3–78.4) | 24.4 | 74.9 | (68.3–81.5) | 25.1 |
| General health (GH) | 70.2 | (69.3–71.1) | 21.9 | 68.2 | (62.2–74.2) | 22.3 |
| Overall mental health | ||||||
| Mental Component Summary (MCS) | 40.8 | (39.9–41.0) | 12.5 | 54.8 | (50.0–59.6) | 9.1 |
| Mental subscales | ||||||
| Vitality (VT) | 50.2 | (49.1–51.2) | 23.8 | 68.6 | (62.6–74.6) | 23.1 |
| Social functioning (SF) | 76.9 | (75.9–78.0) | 24.6 | 89.9 | (82.0–97.8) | 19.4 |
| Role-emotional (RE) | 47.9 | (46.1–49.8) | 43.1 | 85.1 | (77.6–92.6) | 29.0 |
| Mental health (MH) | 60.8 | (59.9–61.7) | 21.0 | 81.8 | (74.6–89.0) | 17.6 |
CI: confidence interval; SD: standard deviation.
Health status based on the 36-item Short-Form Health Survey (SF-36) (scores 0–100; higher score indicates better health status).
Health status of the general population-based on the SF-36 in a representative sample of the Danish population in 1994.
The mean MCS score in the caregivers was 40.8 (95% CI: 39.9;41.0) with an absolute difference of 14 compared to the mean score in the general population.39 (Table 2). All scores on the mental subscales (VT, SF, RE, MH) were significantly lower in the caregivers than in the general population.39
Health status as predictor of PGD
At follow-up, 152 (7.6%) met the criteria for PGD and had a mean PCS score of 46.3 (95% CI: 44.5;48.2) compared to 52.1 (95% CI: 51.7;52.6) in caregivers without PGD. The absolute difference between groups was 5.8.
The mean MCS score was 29.9 (95% CI: 28.2;31.6) in those with PGD compared to 41.4 (95% CI: 40.8;42.0) in caregivers without PGD corresponding to an absolute difference of 11.5. Poor pre-death physical health status (low PCS) (adjusted OR: 1.05 (95% CI: 1.04;1.07)) and poor pre-death mental health status (low MCS) (adjusted OR: 1.09 (95% CI: 1.07;1.11)) predicted PGD on a continuous SF-36 scale. For all SF-36 subscales, lower scores predicted higher risk of PGD (Table 3).
Table 3.
Multivariable regression analysis of the association between health statusa before the patient’s death and prolonged grief disorderb in a population of caregivers (N = 2125).
| Caregivers with prolonged grief disorder | Caregivers without prolonged grief disorder | Crude OR (95% CI) |
Adjustedc OR (95% CI) |
|
|---|---|---|---|---|
| (n = 152) | (n = 1973) | |||
| Mean (95% CI) |
Mean (95% CI) |
|||
| Physical health | ||||
| Physical Component Summary (PCS) |
46.3 (44.5–48.2) | 52.1 (51.7–52.6) | 1.05 (1.04–1.07) | 1.05 (1.04–1.07) |
| Physical subscales | ||||
| Physical functioning (PF) | 74.0 (70.0–78.1) | 86.1 (85.2–87.0) | 1.02 (1.02–1.03) | 1.02 (1.02–1.03)* |
| Role-physical (RP) | 31.9 (25.5–38.4) | 62.9 (61.0–64.7) | 1.02 (1.01–1.02) | 1.02 (1.01–1.02) |
| Bodily pain (BP) | 62.1 (57.9–66.4) | 78.9 (77.9–80.0) | 1.03 (1.02–1.03) | 1.03 (1.02–1.03) |
| General health (GH) | 53.1 (49.5–56.6) | 72.0 (71.1–73.0) | 1.04 (1.03–1.04) | 1.04 (1.03–1.04) |
| Mental health | ||||
| Mental Component Summary (MCS) |
29.9 (28.2–31.6) | 41.4 (40.8–42.0) | 1.08 (1.06–1.10) | 1.09 (1.07–1.11) |
| Mental subscales | ||||
| Vitality (VT) | 30.5 (27.4–33.6) | 52.1 (51.0–53.1) | 1.04 (1.04–1.05) | 1.05 (1.04–1.06) |
| Social functioning (SF) | 57.5 (53.5–61.5) | 78.7 (77.6–79.8) | 1.03 (1.02–1.04) | 1.03 (1.02–1.04) |
| Role-emotional (RE) | 20.5 (15.2–25.8) | 50.6 (48.6–52.6) | 1.02 (1.01–1.02) | 1.02 (1.01–1.03) |
| Mental health (MH) | 41.6 (38.7–44.4) | 62.5 (61.7–63.5) | 1.05 (1.04–1.06) | 1.05 (1.04–1.06) |
OR: odds ratio; CI: confidence interval.
Health status based on the 36-item Short-Form Health Survey (SF-36).
Prolonged grief disorder based on the Prolonged Grief-13 scale (PG-13).
Adjusted for age, gender and educational level of the caregivers.
On the subscale score PF, goodness of fit was p = 0.03. In all other subscale scores goodness of fit was p > 0.05.
The stratified analyses revealed that the association was statistically significant in both partners and non-partners and in caregivers with and without chronic illnesses (Supplementary Material A, Tables A1 and A2).
Discussion
Main findings
The 2125 caregivers in this nationwide prospective cohort study reported more limitations due to physical health (RP) than reported by the general population sample aged 55–64 years.39 Compared to the health status of the general population, the overall physical health status of the caregivers was non-significantly better, but the overall MCS score and all SF-36 mental subscale scores were significantly worse than in the general population.39
Poor physical and mental health status during caregiving predicted PGD, and the association was independent of the caregivers’ chronic illnesses and personal relations to the patients.
Strengths and limitations
The large study size and the population-based design were an advantage. Furthermore, the prospective study design made it possible to examine predictors of PGD. The risk of information bias of self-reported health status was low as our study used the validated SF-36 scale. Yet, the PG-13 scale has not been validated in the Danish version, but the translation followed WHO’s recommendation for translating questionnaires.41 Our use of PG-13 to measure PGD was in line with most recent grief studies, which ensure a basis for comparison with prior studies. An additional advantage was the high quality of Danish registers and the low level of missing data with 223 (10.5%) missing responses on either SF-36 or PG-13 (n = 199) or one of the adjusting factors (n = 24). Estimates of associations between health status and PGD tend to be low, which is probably due to the analyses of SF-36 scores continuously. However, significant differences were present and interpreted according to the principle of minimal clinical important difference (MCID).42
Goodness of fit for SF-36 scores indicated that our model fitted the scale, although we did find a misfit on one subscale (PF).
At baseline, the participating caregivers corresponded to 38% of the contacted patients. This is in line with other bereavement studies in national samples.23,43 However, selection bias might affect the generalisability of our study as participating caregivers may have a higher educational level than the non-responding; this is consistent with other western cohort studies, which have shown to underrepresent people of low educational level.44,45 This should be taken into account in the comparison with a standardised general population sample. Nevertheless, we believe that the study results can be generalised to other caregivers of patients in the late terminal phase in similar healthcare systems. Although data for the current analysis was collected 5 years ago, we consider the study highly relevant as it is still ongoing,46 and the setting, including the Danish healthcare system, has not changed significantly. However, the general population sample for comparison was conducted in 1994 and the interpretation must be made with caution as the health status in the general Danish population might have changed.
What this study adds
Health status of the caregivers
Our study showed that caregivers experienced limitations in their roles due to their physical health. The RP subscale score was significantly worse in caregivers than in the general population, indicating that caregivers struggle to combine their caregiver role with work-related duties and other daily activities.47 Previous studies point at high caregiver burden among caregivers, which includes a dimension of physical impairment.48 Thus, our finding of limitations in the roles and daily activities due to physical health might reflect caregiver burden that may prompt a need for healthcare interventions in caregivers.
The PCS score of the caregivers was non-significantly better than the score of the general population sample. One explanation might be that the responding caregivers comprised a selected group with a higher educational level than the non-responding caregivers, which has been associated with better health status.49 This finding is in line with previous studies that have shown similar or better overall physical health in participating caregivers than in the general population.24,25
The caregivers had worse overall MCS score than the general population sample, which is in line with previous findings that caregiving negatively affects the caregivers’ mental health.23–26 Two of the previous studies used the SF-36 to assess mental health,25,26 and our study confirmed poor mental health in caregivers in a prospective population-based study with a robust study design. Furthermore, we found that caregivers scored lower than the general population on all SF-36 mental health subscales. The findings seem to underline the exhausting and demanding situation of caregivers to severely ill patients.50
Health status as a predictor of PGD
To our knowledge, our study is the first to examine self-reported physical health status before bereavement as a predictor of PGD in caregivers. As a novel finding, PGD was predicted by poor physical health status during caregiving as measured by the validated SF-36 scale. Previous studies conducted after bereavement found similar associations.18,51 A large-scale retrospective study of 9123 bereaved persons due to cancer found that retrospectively reported poor physical health status before bereavement was associated with PGD.18 Likewise, a study of 328 bereaved persons found that poor health status 3 months after bereavement was associated with PGD 15 months after bereavement.51 Hence, poor self-rated physical health appear to be a contributory factor to the development of PGD. Allostatic load, the long-term effect of continued exposure to stress,52 may be a possible explanation for this association, as caregiving and bereavement are stressors that may cause biological dysregulation or overstimulation of the allostatic system.52 This is supported by a previous study showing an association between poor self-rated health and allostatic load operationalised as a measure of biometrics, including BMI, blood pressure and blood tests.53 Continuous allostatic load constitutes a risk of disease development, including mental illness,52 and may be a factor in the development of PGD.
Several poor mental health measures are well-documented predictors of PGD among caregivers. For instance, previous studies have identified depression, anxiety and severe grief reaction before bereavement as risk factors of PGD.5,15,17,20 Our study supports that poor mental health status predicts PGD in caregivers. Interpreting our results from a perspective of the theory of network, symptoms of psychopathology can be multi-causally connected through biological, psychological and societal stressors and complex mechanisms.54 Hence, poor health status may be a contributing factor to the pathological symptomatology and the development of PGD.
Clinical implications and future studies
Providing care for terminally ill patients affects mental health of caregivers. Prior studies suggested a MCID of 3–5 points when using SF-36.42 The caregivers in our study had a 14 points lower mean score of MCS than the general population indicating high clinical relevance. Likewise, the caregivers’ physical performance may be impaired, which is reflected by limitations in work-related or daily activities and a 15.4 points mean difference between the RP score of the caregivers and the general population.
Importantly, both poor physical and mental health before bereavement appear to increase the risk of PGD in caregivers. This calls for focus on caregivers’ health status and provision of healthcare interventions aiming to promote caregivers’ health. In addition, professional support is needed to ensure practical help, support from the network and that caregivers with a job consider the opportunity for compassionate leave.
Identification of risk factors of PGD provides an opportunity to target support at high-risk caregivers. Hence, development of risk assessment tools is necessary.55,56 In future studies measures of anxiety, depression, health status by SF-36 and associations between these factors should be included. Furthermore, future research is needed, which include caregivers’ health status after the patients’ death, as this might extend our understanding of caregivers being vulnerable to PGD and add to the understanding of allostatic load.
Conclusion
In this nationwide prospective cohort study, poor self-reported physical and mental health status in caregivers providing end-of-life caregiving was found to predict PGD, which suggests allostatic load. Furthermore, caregivers were found to be limited in their daily activities because of their physical health status; they also had significantly worse mental health than a comparable general population sample. Our findings highlight that caregivers of patients at the end of life are in a highly demanding situation, which calls for support from their surroundings, including health professionals.
Supplemental Material
Supplemental material, Supplementary_material_A_21.09.2019 for Poor physical and mental health predicts prolonged grief disorder: A prospective, population-based cohort study on caregivers of patients at the end of life by Maja Krarup Lenger, Mette Asbjoern Neergaard, Mai-Britt Guldin and Mette Kjaergaard Nielsen in Palliative Medicine
Acknowledgments
We wish to extend our profound gratitude towards patients and caregivers who participated in this study. Thanks to the staff at the Research Unit for General Practice, Aarhus, in particular IT specialist Hanne Beyer, data manager Kaare Rud Flarup and language editor Lone Niedziella.
Footnotes
Authorship: The study was predominantly conceived by MKL and MKN. Data was collected by MKN, MBG and MAN. Data was analysed by MKL and interpreted by all authors. MKL and MKN made the first draft, and all authors contributed to the critical revision and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Novo Nordisk Foundation (grant no. NNF17OC0024410) and the Danish Cancer Society (grant no. R160-A10389-16-S3).
ORCID iDs: Maja Krarup Lenger  https://orcid.org/0000-0001-5595-1610
https://orcid.org/0000-0001-5595-1610
Mette Asbjoern Neergaard  https://orcid.org/0000-0003-3309-5838
https://orcid.org/0000-0003-3309-5838
Mette Kjaergaard Nielsen  https://orcid.org/0000-0001-9940-2226
https://orcid.org/0000-0001-9940-2226
Data management and sharing: Data is stored on a secure network at Statistics Denmark and may be accessed only through an authorised connection. Data sharing is not possible according to the EU General Data Protection Regulation.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Shear MK. Complicated Grief. NEJM 2015; 372: 153–160. [DOI] [PubMed] [Google Scholar]
- 2. Shear MK, Simon N, Wall M, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety 2011; 28: 103–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med 2009; 6: e1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nakajima S. Complicated grief: recent developments in diagnostic criteria and treatment. Philos Trans R Soc Lond B Biol Sci 2018; 373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nielsen MK, Neergaard MA, Jensen AB, et al. Predictors of complicated grief and depression in bereaved caregivers: a nationwide prospective cohort study. J Pain Symptom Manage 2017; 53: 540–550. [DOI] [PubMed] [Google Scholar]
- 6. Thomas K, Hudson P, Trauer T, et al. Risk factors for developing prolonged grief during bereavement in family carers of cancer patients in palliative care: a longitudinal study. J Pain Symptom Manage 2014; 47: 531–541. [DOI] [PubMed] [Google Scholar]
- 7. Kersting A, Brahler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord 2011; 131: 339–343. [DOI] [PubMed] [Google Scholar]
- 8. Lundorff M, Holmgren H, Zachariae R, et al. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J Affect Disord 2017; 212: 138–149. [DOI] [PubMed] [Google Scholar]
- 9. Shear MK, Ghesquiere A, Glickman K. Bereavement and complicated grief. Curr Psychiatry Rep. 2013; 15: 406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prigerson HG, Bierhals AJ, Kasl SV, et al. Traumatic grief as a risk factor for mental and physical morbidity. Am J Psychiatry 1997; 154: 616–623. [DOI] [PubMed] [Google Scholar]
- 11. Mason TM, Duffy AR. Complicated grief and cortisol response: an integrative review of the literature. J Am Psychiatr Nurses Assoc 2018; 25(3): 181–188. [DOI] [PubMed] [Google Scholar]
- 12. Guldin MB, Kjaersgaard MIS, Fenger-Gron M, et al. Risk of suicide, deliberate self-harm and psychiatric illness after the loss of a close relative: a nationwide cohort study. World Psychiatry 2017; 16: 193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Waller A, Turon H, Mansfield E, et al. Assisting the bereaved: a systematic review of the evidence for grief counselling. Palliat Med. 2016; 30: 132–148. [DOI] [PubMed] [Google Scholar]
- 14. Stroebe W, Schut H, Stroebe MS. Grief work, disclosure and counseling: do they help the bereaved? Clin Psychol Rev 2005; 25: 395–414. [DOI] [PubMed] [Google Scholar]
- 15. Ghesquiere A, Haidar YM, Shear MK. Risks for complicated grief in family caregivers. J Soc Work End Life Palliat Care 2011; 7: 216–240. [DOI] [PubMed] [Google Scholar]
- 16. Guldin MB, Vedsted P, Zachariae R, et al. Complicated grief and need for professional support in family caregivers of cancer patients in palliative care: a longitudinal cohort study. Support Care Cancer 2012; 20: 1679–1685. [DOI] [PubMed] [Google Scholar]
- 17. Lobb EA, Kristjanson LJ, Aoun SM, et al. Predictors of complicated grief: a systematic review of empirical studies. Death Stud 2010; 34: 673–698. [DOI] [PubMed] [Google Scholar]
- 18. Aoyama M, Sakaguchi Y, Morita T, et al. Factors associated with possible complicated grief and major depressive disorders. Psychooncology 2018; 27: 915–921. [DOI] [PubMed] [Google Scholar]
- 19. Tofthagen CS, Kip K, Witt A, et al. Complicated grief: risk factors, interventions, and resources for oncology nurses. Clin J Oncol Nurs 2017; 21: 331–337. [DOI] [PubMed] [Google Scholar]
- 20. Tsai WI, Prigerson HG, Li CY, et al. Longitudinal changes and predictors of prolonged grief for bereaved family caregivers over the first 2 years after the terminally ill cancer patient’s death. Palliat Med 2016; 30: 495–503. [DOI] [PubMed] [Google Scholar]
- 21. Nielsen MK, Neergaard MA, Jensen AB, et al. Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin Psychol Rev 2016; 44: 75–93. [DOI] [PubMed] [Google Scholar]
- 22. Coelho AM, Delalibera MA, Barbosa A. Palliative care caregivers’ grief mediators: a prospective study. Am J Hosp Palliat Care 2016; 33: 346–353. [DOI] [PubMed] [Google Scholar]
- 23. Grande G, Rowland C, van den Berg B, et al. Psychological morbidity and general health among family caregivers during end-of-life cancer care: a retrospective census survey. Palliat Med 2018; 32: 1605–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gotze H, Brahler E, Gansera L, et al. Psychological distress and quality of life of palliative cancer patients and their caring relatives during home care. Support Care Cancer 2014; 22: 2775–2782. [DOI] [PubMed] [Google Scholar]
- 25. Kenny PM, Hall JP, Zapart S, et al. Informal care and home-based palliative care: the health-related quality of life of carers. J Pain Symptom Manage 2010; 40: 35–48. [DOI] [PubMed] [Google Scholar]
- 26. Morishita M, Kamibeppu K. Quality of life and satisfaction with care among family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care. Support Care Cancer 2014; 22: 2687–2696. [DOI] [PubMed] [Google Scholar]
- 27. Pini S, Gesi C, Abelli M, et al. Clinical correlates of complicated grief among individuals with acute coronary syndromes. Neuropsychiatr Dis Treat 2015; 11: 2583–2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. The Ministry of Health. Healthcare in Denmark - an overview 2017. Copenhagen: The Ministry of Health, Healthcare Denmark. [Google Scholar]
- 29. Danish Medicines Agency. Reimbursement for the terminally ill, https://laegemiddelstyrelsen.dk/en/reimbursement/individual-reimbursement/reimbursement-for-the-terminally-ill (2016, accessed 06/02 2019).
- 30. Nielsen MK, Neergaard MA, Jensen AB, et al. Psychological distress, health, and socio-economic factors in caregivers of terminally ill patients: a nationwide population-based cohort study. Support Care Cancer 2016; 24: 3057–3067. DOI: 10.1007/s00520-016-3120-7. [DOI] [PubMed] [Google Scholar]
- 31. Daugaard C, Neergaard MA, Vestergaard AHS, et al. Socioeconomic inequality in drug reimbursement during end-of-life care: a nationwide study. J Epidemiol Community Health 2019; 73: 435–442. [DOI] [PubMed] [Google Scholar]
- 32. Thygesen LC, Daasnes C, Thaulow I, et al. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health 2011; 39: 12–16. [DOI] [PubMed] [Google Scholar]
- 33. Statistics Denmark. Data for research, https://www.dst.dk/en/TilSalg/Forskningsservice (accessed 5 February 2019).
- 34. Prigerson HG, Maciejewski PK. Prolonged Grief Disorder (PG – 13) ©, https://endoflife.weill.cornell.edu/sites/default/files/pg-13.pdf (2011, accessed 5 February 2019). [DOI] [PubMed]
- 35. Ware JE, Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 1998; 51: 903–912. [DOI] [PubMed] [Google Scholar]
- 36. Ware JE, Jr, Snow KK, Kosinsji M, et al. SF-36 Health survey. Manual and interpretation guide. Boston: Nimrod Press, 1993. [Google Scholar]
- 37. UNESCO Institute of Statistics. International Standard Classification of Education (ISCED) 2011, http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf (2012, accessed 5 February 2019).
- 38. Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011; 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bjørner JB. Dansk manual til SF-36 : et spørgeskema om helbredsstatus (Danish Manual for SF-36: a questionnaire of health status). Lif, 1997. [Google Scholar]
- 40. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007; 4: e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Health Organization. Process of translation and adaptation of instruments, https://www.who.int/substance_abuse/research_tools/translation/en/ (accessed 8 April 2020).
- 42. Samsa G, Edelman D, Rothman ML, et al. Determining clinically important differences in health status measures. A general approach with illustration to the health utilities index Mark II. Pharmacoeconomics 1999; 15: 141–155. [DOI] [PubMed] [Google Scholar]
- 43. Pivodic L, Harding R, Calanzani N, et al. Home care by general practitioners for cancer patients in the last 3 months of life: an epidemiological study of quality and associated factors. Palliat Med 2016; 30: 64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jacobsen TN, Nohr EA, Frydenberg M. Selection by socioeconomic factors into the Danish National Birth Cohort. Eur J Epidemiol 2010; 25: 349–355. [DOI] [PubMed] [Google Scholar]
- 45. Tjonneland A, Olsen A, Boll K, et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health 2007; 35: 432–441. [DOI] [PubMed] [Google Scholar]
- 46. Nielsen MK, Carlsen AH, Neergaard MA, et al. Looking beyond the mean in grief trajectories: a prospective, population-based cohort study. Soc Sci Med 2019; 232: 460–469. [DOI] [PubMed] [Google Scholar]
- 47. Longacre ML, Valdmanis VG, Handorf EA, et al. Work impact and emotional stress among informal caregivers for older adults. J Gerontol B Psychol Sci Soc Sci 2017; 72: 522–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Adelman RD, Tmanova LL, Delgado D, et al. Caregiver burden: a clinical review. JAMA 2014; 311: 1052–1060. [DOI] [PubMed] [Google Scholar]
- 49. Sullivan M, Karlsson J. The Swedish SF-36 Health Survey III. Evaluation of criterion-based validity: results from normative population. J Clin Epidemiol 1998; 51: 1105–1113. [DOI] [PubMed] [Google Scholar]
- 50. Romito F, Goldzweig G, Cormio C, et al. Informal caregiving for cancer patients. Cancer 2013; 119(Suppl. 11): 2160–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Utz RL, Caserta M, Lund D. Grief, depressive symptoms, and physical health among recently bereaved spouses. Gerontologist 2012; 52: 460–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci 1998; 840: 33–44. [DOI] [PubMed] [Google Scholar]
- 53. Vie TL, Hufthammer KO, Holmen TL, et al. Is self-rated health a stable and predictive factor for allostatic load in early adulthood? Findings from the Nord Trondelag Health Study (HUNT). Soc Sci Med 2014; 117: 1–9. [DOI] [PubMed] [Google Scholar]
- 54. Robinaugh DJ, LeBlanc NJ, Vuletich HA, et al. Network analysis of persistent complex bereavement disorder in conjugally bereaved adults. J Abnorm Psychol 2014; 123: 510–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ewing G, Grande G. Development of a Carer Support Needs Assessment Tool (CSNAT) for end-of-life care practice at home: a qualitative study. Palliat Med 2013; 27: 244–256. [DOI] [PubMed] [Google Scholar]
- 56. Thomsen KT, Guldin MB, Nielsen MK, et al. A process evaluation of systematic risk and needs assessment for caregivers in specialised palliative care. BMC Palliat Care 2017; 16: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_material_A_21.09.2019 for Poor physical and mental health predicts prolonged grief disorder: A prospective, population-based cohort study on caregivers of patients at the end of life by Maja Krarup Lenger, Mette Asbjoern Neergaard, Mai-Britt Guldin and Mette Kjaergaard Nielsen in Palliative Medicine