Abstract
Addressing parental smoking in the child healthcare setting improves the health of all family members. Innovative approaches, such as mobilizing technology-based platforms, may streamline screening and motivate acceptance of behavioral health services to treat tobacco use and dependence. The obective of this study was to describe innovations added to the CEASE intervention and to track 2 year post-intervention implementation data on families who were screened for tobacco use. Child healthcare practices in five states (IN, NC, OH, TN, and VA) used an electronic tablet screener to identify tobacco use within families and deliver tobacco cessation assistance to smokers. Motivational/educational videos on cessation were displayed via the screener to enhance its utility. Five CEASE intervention practices screened 50,111 family members for tobacco use and identified 6,885 families with children exposed to tobacco smoke. The mean number of screeners per practice per month was 417; the mean number of households with smokers identified per month was 57. Of 2,764 smokers who were at visits and consented, 57% indicated that they wanted a prescription to reduce or quit smoking; 94% of these were given preprinted prescriptions. Of 41% who requested connection to the quitline, 93% were given enrollment forms. Electronic screening was used to routinely identify tobacco users, leading to increased potential for offering cessation assistance to all household members who smoke. Improved delivery of smoking cessation services to families may be achieved by integrating technological innovations into routine pediatric practice.
CLINICAL TRIALS REGISTRATION: Trial Number NCT01882348
Keywords: Smoking cessation, Tobacco smoke exposure, Technological innovations, Public health, Tobacco control interventions
Implications.
Practice: The addition of a mobile technology-based platform to an existing family-centered tobacco control program improves efficiency in screening and increases motivation to accept tobacco treatment services.
Policy: Policymakers and accountable care organizations can improve the health of families by implementing systems aided by technology that routinely screen for household tobacco use, deliver meaningful cessation assistance, and bill for services in the pediatric setting.
Research: Future research should focus on developing better integration of technology for tobacco control programs used in pediatric office settings that will result in routine screening and delivery of smoking cessation assistance for families.
BACKGROUND
Tobacco use is a well-known preventable cause of morbidity and mortality in the USA, accounting for 480,000 deaths annually [1]. The 2006 U.S. Surgeon General’s Report concluded that there is no safe level of exposure to tobacco smoke [2]. Exposure to tobacco smoke causes depression and anxiety [3–5], decreases in attention span [6–8], decreases in working memory, decreases in alveolar lung growth [9–11], and impairment in weight gain [12]. Exposure to tobacco smoke in utero increases the risk of premature birth and low birth weight [2,13,14] and also increases the risk for Sudden Infant Death Syndrome (SIDS) [1]. Children’s exposure to toxins in tobacco smoke is a known cause of asthma, bronchitis, pneumonia, and middle ear infection [1,2,15,16]. When parents and legal guardians (henceforth parents) quit smoking [17], their life expectancy is increased [18] and their children have lower odds of becoming smokers [19–21]. Overall, parental smoking cessation may lead to reduced tobacco smoke exposure (TSE) of children, which can reduce diseases caused by TSE and yield fewer missed school days [2]. Parents who smoke usually visit their child’s healthcare provider more often than their own [22,23], creating an opportunity for staff at child healthcare settings to identify smoking parents and deliver effective tobacco cessation intervention [24,25]. However, fewer than 3% of parents get any tobacco dependence treatment in this context of the child healthcare setting [24].
Although there is a clear need for programs and services to help families become tobacco-free, few programs in the child healthcare setting address this gap. The Clinical Effort Against Secondhand Smoke Exposure (CEASE) program was developed to address parental tobacco use and the tobacco smoke exposure of children [26,27]; the program was developed in 2004, based on earlier work in hospital-based efforts at parental smoking cessation [28]. From 2004 until 2014, CEASE was primarily a paper-based intervention that used paper forms to screen for tobacco use and exposure; although this method was successfully implemented in study practices [24,29], it was not shown to result in sustainable practice change [30]. Informal feedback from clinicians and staff who were part of the paper-based CEASE study indicated that problems with sustaining the intervention may have been due to the limited time to address parental tobacco use during a 15 min visit, lack of follow-up with smoking parents due to documentation of smoking status on paper forms rather than in electronic health record systems, and lack of time-efficient methods to facilitate connection to cessation resources. The paper-based version of CEASE was updated in 2015 by using an electronic screening tool to screen families for tobacco use and deliver tobacco cessation treatment in pediatric practices.
This paper describes the methods and innovations of the CEASE intervention used to deliver tobacco cessation treatment to families in the child healthcare delivery setting. This paper explores these innovations while presenting post-intervention implementation data on the number of families screened for household tobacco use over 2 years, the number of smokers identified at the visits, and the number of smokers requesting tobacco cessation assistance in the form of a nicotine replacement therapy (NRT) prescription and referral to the tobacco quitline. We hypothesized that the addition of technological advances to an existing family-centered tobacco control program would improve delivery of tobacco cessation assistance in a sustainable manner.
METHODS
Intervention design and updates
The development and improvement of the CEASE intervention was shaped by research findings and guidelines for the treatment of tobacco use and dependence [1,2,31,32], as well as by conceptual frameworks for implementing and sustaining practice change [26,27]. The design and improvement of CEASE was influenced by the Chronic Care Model [33–35], the RE-AIM model [36,37], and the literature on sustainability of healthcare programs [38–40]. Table 1 shows how these models were used to improve the delivery of CEASE within pediatric practices to help every family become tobacco-free.
Table 1.
Conceptual model constructs that influenced innovations
| Conceptual Model | |
|---|---|
| Component and Rationale | Innovative CEASE aspect influenced by the model |
| Chronic Care Model [33,34] (Clinical Information Systems) recommends that practices: • Identify relevant subpopulations for proactive care • Facilitate care planning • Share information to coordinate care (information about smoking and tobacco smoke exposure; information about services requested) |
Electronic screening for tobacco use and tobacco smoke exposure to screen for: • Tobacco use and exposure • Interest in using smoking cessation medications • Interest in community smoking cessation support services (such as the free state quitline or SmokefreeTXT) Practices are instructed to document household tobacco use status and assistance provided (if any) information in the electronic medical record of the child for care coordination. |
| Chronic Care Model (the Community) encourages programs to: • Connect patients to effective community programs • Form partnerships with community organizations to support and develop interventions that fill gaps in needed services |
CEASE trains pediatric offices to refer tobacco users to free community-based cessation resources such as the state tobacco quitline and SmokefreeTXT |
| Chronic Care Model (Self-management Support) recommends: • Emphasizing patient’s central role in managing their health • Using effective self-management support strategies that include goal-setting, action planning, problem-solving, and follow-up |
CEASE promotes self-management support through training clinicians to help all tobacco users: • Set a quit date • Develop a quit plan, including strategies to overcome barriers to smoking cessation • Use over-the-counter smoking cessation medications to manage cravings while quitting smoking • Establish smoke-free home and car rules |
| RE-AIM [36,37] (Reach): • Tailor interventions to reach more people |
CEASE intervention is tailored based on the needs of individual pediatric practices and families that these practices treat: • Spanish materials are offered in a practice with high Spanish speaking population • The CEASE Action Sheet is individually designed for each practice and resources in each state The flow of screening using the electronic tablet is adapted to the needs and unique situation of the practice |
| RE-AIM (Implementation): Consistently deliver the main components of the intervention |
CEASE staff worked with practices to ensure consistency of key elements of the CEASE intervention, including: • Screening for tobacco use and exposure; • Referral to free cessation services; • Offer and/or prescription of cessation medication) |
| Sustainability [38–41] Focus on support and education at the health system level practice |
CEASE staff supports and educates practices to make changes to their healthcare delivery system to routinely and effectively address family tobacco use and tobacco smoke exposure over time The design of CEASE focuses on maintaining core elements of the intervention while tailoring some aspects to adapt to the needs of the practice over time CEASE advocates for and supports maintaining a local tobacco control champion at the practice CEASE accounts for staff turnover by training new clinicians and staff members as they are hired into the practice CEASE provides support and education on how to acquire resources for tobacco control activities through billing for services |
To help all office staff members understand family tobacco use and treatment, multiple forms of training were offered at various time points, including telephone training calls, training videos, manuals, educational materials, and online courses [42]. We strove to create simple and accessible training materials, such as the CEASE Implementation Comic (Fig. 1).
Fig. 1.
CEASE implementation comic (artwork done by Nathan Yuen).
As demonstrated in the healthcare implementation and sustainability literature [38,40,43,44], sustainable change requires the buy-in of the whole office staff, clear knowledge of the problem at hand, and motivation to implement the change. Additional support to practices included opportunities to brainstorm on how to overcome potential barriers to implementing CEASE, address workflow concerns, tailor CEASE to work in their clinical setting, and motivate staff through motivational messaging.
INTERVENTION OVERVIEW
The CEASE intervention has been designed to work within the current practices of pediatric primary care healthcare settings to routinely and effectively address parental smoking and tobacco smoke exposure of all family members. The CEASE materials support the Ask, Assist, Refer (AAR) [45] approach to deliver the intervention:
ASK: (1) Identification of smoking household members using a screener via an electronic tablet (henceforth mentioned as tablet) before the parents see their child’s clinician at the visit;
-
ASSIST: (2) Smoking cessation and smokefree homes/cars counseling (brief motivational messaging elements include collaborative goal setting, establishing a quit date, etc) during the visit;
(3) Smoking cessation medication (NRT prescription for cessation and for those cutting down as recommended in latest guidelines);
-
REFER: (4) Referral and enrollment of smoking family members in the free state telephone quitline via a faxed enrollment form;
(5) A mHealth (mobile health) initiative to refer and enroll smoking family members into a free mobile phone-based smoking cessation support texting service (SmokefreeTXT).
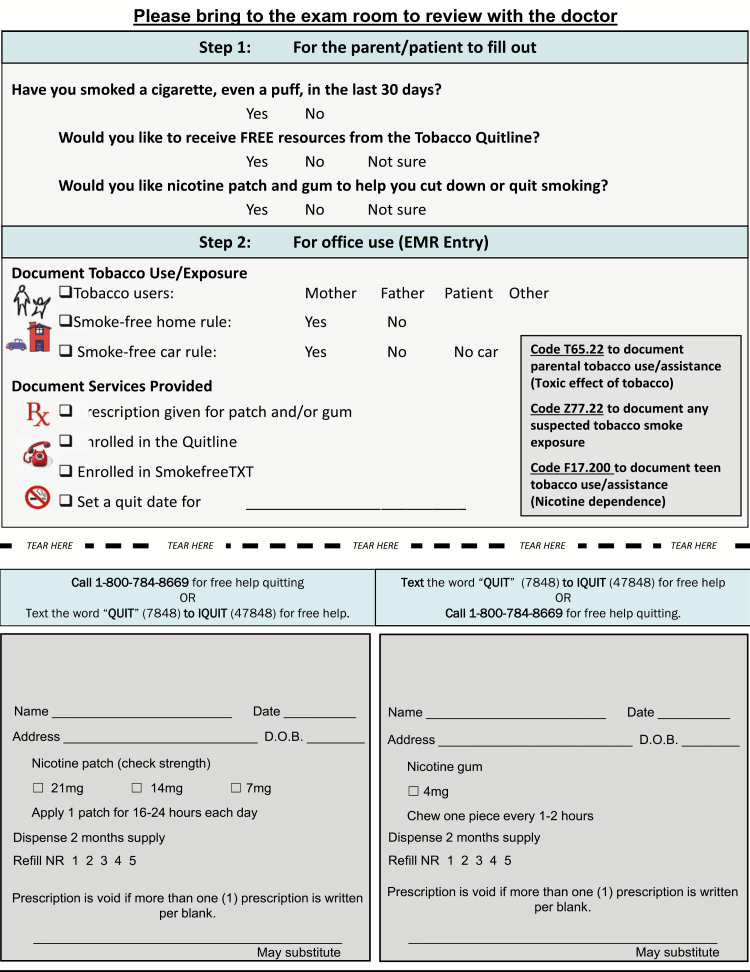
One of the core features of the CEASE intervention is the CEASE Action Sheet (Fig. 2), which was given to the parent if they reported having a household tobacco user on the screener. The CEASE Action Sheet serves as a guide for the clinician to document tobacco cessation services provided and contains cues to ensure tobacco use/smoke-free home and car rules are documented in the child’s medical record. The customizable CEASE Action Sheet included preprinted prescriptions for NRT and information about SmokefreeTXT. All practices requested and were given electronically signed preprinted prescriptions to save time.
Fig. 2.
CEASE action sheet (also found on https://www.massgeneral.org/ceasetobacco/assets/PDF/blank-CEASE-action-sheet.pdf).
INNOVATIONS
Electronic screening for household tobacco use using tablets
To systematically screen families for household tobacco use and exposure and treat tobacco dependence, the CEASE intervention was improved by the addition of a previsit, tablet-based electronic screener at all visits. The screener was managed using REDCap [46], which is a secure, web-based application designed to support data capture for research studies. The CEASE screener identified families with exposure to tobacco smoke and offered cessation assistance to smoking adults who were present at the child’s visit. For one practice with a large Spanish speaking population, Spanish and English texts were both presented on the screener.
The first page of the screener for each practice was customized with pictures of the clinicians at the practice and a brief message from the staff asking parents to complete the screener. Parents completed the screener during the check-in process or before the visit with the child’s healthcare provider. The first question on the screener was: “Does any member of your household use any form of tobacco?” The parent could choose one of the following answer options: “Yes,” “No,” or “Decline; I prefer not to answer at this time.” The screener ended for parents who answer “No” to this question and they were prompted to hand the tablet back to the office staff. Parents who reported having a household tobacco user were consented electronically on the screener to complete additional questions. These questions included information about their child’s name, relationship to the child, clinician seen at that visit, and their tobacco use status. If they were current smokers, then the screener was programmed to ask them about their interest in NRT and connection to the free state quitline and SmokefreeTXT program. After the parent completed all questions, the administrative staff handed them a CEASE Action Sheet and documented the distribution of the sheet on the screener. If the parent indicated on the screener that he or she would like to be connected with the state tobacco quitline on the screener, the office staff were prompted to hand the parent a tobacco quitline enrollment form and document the distribution of the enrollment form on the screener. When available from the state’s tobacco quitline, the tablet included information for parents who receive a tobacco quitline form about when to expect a call from the quitline and/or how the phone number would likely appear on their caller ID.
Real-time data collection and transmission
Data from the screener were electronically housed in a REDCap database accessible only by CEASE staff at MGH. The data were transmitted in real-time to the MGH staff; they monitored the data about how often the tablet was handed out daily for the first few weeks after intervention implementation. This monitoring continued on a weekly basis. These data were shared with practices regularly to provide feedback on their iPad handout numbers. Real-time data monitoring helped identify any problems with intervention implementation at an early stage and share the progress of the practice with their staff. Quick identification of problems with screening parents for household tobacco use led to discussions with practices on how to improve their screening processes.
Creation of family tobacco use registry of children exposed to household tobacco use
As part of the disease management approach of the CEASE intervention, CEASE included a registry of children exposed to tobacco smoke [47–49]. Each month, CEASE staff created a practice-specific registry report based on the electronic screener, organized by clinician name. This report provided a list of the children seen who live with a household tobacco user and whether the user requested any tobacco cessation assistance. Many practices did not have a system to document family tobacco users in the child’s health record so this automated report served as a tool to track all children in the practice who had a household tobacco user. For those practices that already documented family tobacco use, the report streamlined the process by listing all families who have requested specialized tobacco services and resources. This report was sent weekly in the first month and then once a month via a password protected file, which was to be distributed to each of the clinicians in the practice. The CEASE team recommended ways to use the report and practices chose what worked for them. One recommendation was to send letters with the quitline number and signed NRT prescriptions to smoking parents who requested assistance on the screener. All five practices implemented this strategy. One practice used this report to follow-up with the parents by phone to assess their cessation progress and whether they received the requested services. Studies have suggested that if chronic disease registries are utilized in one or more ways, they can improve clinical processes and outcomes for patients with the chronic disease or exposure [50–52].
Use of media (short videos) to help motivate parents to quit smoking
Health promotion programs are recognizing the power of advertising/media to discourage harmful behaviors and to improve overall health outcomes [53]. By showing short videos to smoking parents to increase their knowledge about the harms of tobacco use and of smoking cessation methods, healthcare providers can help motivate these smokers to set a quit date, accept prescriptions for NRT, and connect to free smoking cessation counseling resources outside of the practice. Research has also shown that antitobacco industry advertising, which focuses on the deceitful marketing practices of the industry, reduces smoking among adolescents [54–57].
To increase awareness about harms of tobacco use on smokers and family members exposed to tobacco smoke, the CEASE program used the electronic screener to show short motivational and educational videos from national sources like Center for Disease and Control, tobacco-free nonprofit organizations and state sources like the state health department and quitline. All parents who reported having a household tobacco smoker were given the opportunity to view the video. A short description of the video was added on the top of the video page and parents were encouraged to watch the video. Watching the video was not required to complete the screener in order to respect parent’s preferences and help save time for those parents who had limited time with the iPad.
The videos were added to the screener in April of 2016. They were uploaded on YouTube; the CEASE team tracked viewing trends via Google analytics. To help evaluate which videos were most liked by parents, we added a rating question in October 2016 asking parents to provide a score between 1 and 4 stars, where higher stars indicated a higher rating. The parents were also given the option “I did not watch the video.” The videos were changed monthly to keep them fresh for repeat parents and to change the message. State-specific quitline videos were used in some months, where available to increase the awareness of free state quitline among parents. The study team invited ideas from the practice staff regarding video preferences tailored to their parent population and changed the screener video based on these suggestions. Practices were informed when a new video was deployed on the tablets in each location and the practice staff was encouraged to watch the video and provide feedback. This strategy was intended to help engage the practice staff in the implementation of the program at their practice.
Table 2 outlines how the CEASE intervention was evaluated, monitored, supported, and improved, as guided by the RE-AIM framework [36]. A continuous quality improvement strategy was used to evaluate and improve both the CEASE intervention and the implementation of CEASE. This was done through monitoring each practice’s RedCap screener data, iPad video views collected with Google analytics, and contacts (phone and email) with practice staff. These process data were enhanced by situational information about the practices gathered during recruitment, peer-to-peer training calls, and the whole-office training calls, creating a deeper understanding of the factors in the practice that could influence the implementation of CEASE. Situational information and monitoring data were shared between all relevant members of the CEASE team to develop concrete steps for adapting CEASE to each practices’ needs and to improve the implementation of practice-based family tobacco control in a consistent and timely manner.
Table 2.
Monitoring and evaluation of the CEASE intervention using the RE-AIM framework
| RE-AIM Component | Process Evaluation (Level of assessment) | Monitoring to identify problems and actions to solve them | Lessons Learned |
|---|---|---|---|
| Reach | Parent level and practice level assessment • Monitor number of people screened (RedCap screener data) • Monitor the number of people watching the video embedded in the screener (Google analytics data on you tube) |
• Some practices had busy front-desk or did not have families wait in waiting area so they had a drop in iPad handout numbers; those practices decided to hand out the iPads to parents to screen for household tobacco use in the examination rooms • When iPad screener numbers dropped, a video was added to the screener • When fewer views were observed, a “rate the video” question was added to screener to engage the families |
• Be flexible according to the needs of the practice and parents • Keep the intervention fresh for repeat users. For example, change videos every month |
| Effectiveness | Parent level and practice level assessment • Parents requesting prescription for NRT and those who received it (RedCap screener data) • Parents requesting connection to the quitline and those who received the quitline enrollment form (RedCap screener data) • Monthly phone conversation with the practice leader or office manager to discuss any issues related to screener handout, medication or quitline connection (Documented on a spreadsheet) |
• When a low percentage of parents receiving prescriptions was observed, CEASE staff called and/or emailed the practice to encourage clinicians to write prescriptions for all parents who requested for medication • Clinicians did not have time to sign NRT prescriptions: All practices chose to have electronic signatures on NRT patch and gum prescriptions so that nurses and medical assistants could also hand out the prescriptions • When a low percentage of parents receiving qutiline enrollment form was observed, CEASE staff called and/or emailed the practice to encourage staff to hand out the enrollment form, help parents complete the form as needed, and fax the form to the quitline using the same process as faxing referrals to other practices • Practices reported that parents were hesitant to answers calls from an unknown number. To address this concern, information was added to the screener for parents who request for a tobacco quitline form about when to expect a call from the quitline and/or how the phone number would likely appear on their caller ID (when available) • Some practices requested additional materials about the quitline to raise awareness of the services offered; additional materials were created by the CEASE team or ordered for free from the state’s tobacco control services |
• Connect practices with free, existing health education materials, when possible • Use a multi-disciplinary approach to deliver care to reduce the time and effort burden on doctors |
| Adoption | Practice level and individual staff member level assessment • Practice-level agreement to adopt the CEASE intervention was an inclusion requirement for the study; as a result, at the practice level, 100% of the five practices adopted the intervention. • Monitor practices for new staff in need of training at the individual staff member level through routine phone calls and emails with the practice leader or office manager, documented on a spreadsheet |
• When new staff members joined a practice, training in the CEASE intervention was offered; this offered training was tailored to the needs of the staff member and included telephone training calls, paid access to an online UMASS Medical school course (Basic Skills for Working with Smokers), an online American Academy of Pediatrics course (EQIPP: Eliminating Tobacco Use and Exposure to Secondhand Smoke), a training video, and a training manual | • Offer a mixture of training and education options about the intervention to suit the needs of the practice and of the individual. • Provide free or low cost training to reduce barriers to access • Provide asynchronous training options so that staff members can engage in training at a time that works best for them. • Provide access to courses that have CMEs as incentives |
| Implementation | Practice level assessment • Monitor staff handing out the CEASE Action Sheets to the eligible families (RedCap screener data) • Monitor staff handing out the quitline forms to the parents requesting them (RedCap screener data) • Monitor number of smokers requesting for NRT prescriptions and referral to the quitline (RedCap screener data) • Monthly phone conversation with the practice leader or office manager to discuss the intervention implementation in their office (documented on a spreadsheet) • Yearly phone meeting with the whole office staff to discuss sustainability of the intervention (documented on a spreadsheet) |
• One practice had a very high Spanish speaking population and parents had trouble completing the screener: Spanish translation was added to the screener. • One practice had a high percentage of smokers who did not want to talk about harms of using tobacco; this practice chose to display a presentation about harms of tobacco smoke on the body on their television screen in the waiting rooms • Parents in a practice did not know about the quitline so did not request it: Videos were sometimes tailored based on requests from the practice staff or clinicians or based on a new quitline video available from that state’s quitline |
• Seek feedback from the implementing partners like clinicians and office staff at regular intervals to improve or tailor the intervention • Use already available free media messages or resources to encourage families to quit smoking |
| Maintenance | Practice level assessment • Monitor staff handing out CEASE Action Sheet to repeat parents (RedCap screener data) • Monitor staff handing out quitline enrollment forms to repeat parents who requested quitline connection (RedCap screener data) |
• When monitoring data revealed that practices were not handing out the CEASE Action Sheet to repeat parents, the CEASE team encouraged practice staff to hand out the CEASE Action Sheet to them • When monitoring data revealed that practices were not handing out the CEASE Action Sheet to repeat parents, the CEASE team encouraged practice staff to connect parents to the quitline • When a quitline offered free nicotine replacement therapy, this information was shared with practice staff through phone calls and emails to motivate referral to the quitline. The information was also shared in real-time with the parents through the RedCap screener. • The CEASE staff sent data about quitline connection to four practices in order to show practice staff the outcome of their quitline referral activities |
• To promote the sustained adoption of an intervention, encourage each practice to have a trained local tobacco control champion • Motivate practice staff to refer repeat parents to the quitline by informing them of relevant external health promotion programs, such as free NRT from a quitline |
Setting
The CEASE intervention was implemented in five pediatric practices in five different states (IN, NC, OH, TN, and VA). Practices were eligible if they had parent smoking prevalence ≥15%, average patient flow ≥50 families per day, at least four full-time clinicians, and used an electronic health record (EHR). The study protocol was approved by Institutional Review Boards at the AAP, Massachusetts General Hospital, and individual practice IRBs when required.
RESULTS
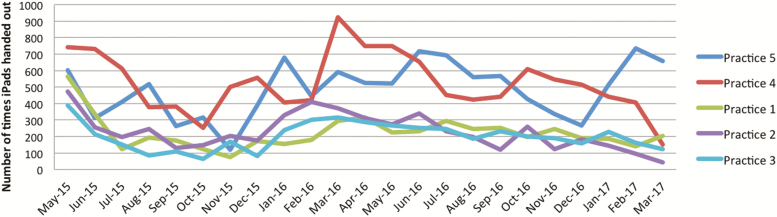
Five CEASE intervention practices screened 50,111 family members for tobacco use in the 2 year post-intervention implementation using the electronic screener (Fig. 3 shows the iPad screening data by month for each practice). Table 3 shows the intake data by practice. The screener identified 6,885 new families with children who were exposed to tobacco smoke. Of these, 4,194 families with a smoker were seen on repeat visits. In the 2 year study period, the mean number of screeners completed in a month per practice was 417; the mean number of households with smokers identified in a month per practice was 57. Of the 2,764 smokers who were at the visit and consented to be a part of the intervention, 57% indicated that they wanted a prescription to reduce/quit smoking and 94% of these were given a preprinted prescription. Of the 41% who requested connection to the quitline, 93% were given the enrollment form. Thirty-three per cent of smoking parents who completed the screener for the first time and at that visit, 31% of repeat parents reported connecting with SmokefreeTXT. Of the 4,194 repeat parents, 22% reported already being connected to the quitline and14% requested connection to the quitline.
Fig. 3.
iPad screeners completed per month by Practice.
Table 3.
Intake screener data on households with tobacco users using the RE-AIM framework
| Practice 1 | Practice 2 | Practice 3 | Practice 4 | Practice 5 | Total | |
|---|---|---|---|---|---|---|
| Reach | ||||||
| Identify households with tobacco users for parents completing the screener for the first time (new parents) | 1,382 (57.8%) | 1,348 (55.2%) | 1,150 (62.5%) | 1,642 (62.5%) | 1,363 (42.8%) | 6,885 (50.8% of new parents) |
| Consented to be part of the program | 1,013 (73.4%) | 949 (70.5%) | 723 (62.9%) | 1,033 (63.0%) | 771 (56.8%) | 4,489 (65.3% of new parents with a household tobacco user) |
| Identify tobacco users at visit | 674 | 569 | 407 | 616 | 498 | 2,764 |
| Households with tobacco users completing the screener again within the past 6 months (Repeats) | 1,677 (64.6%) | 604 (51.2%) | 876 (53.1%) | 632 (20.6%) | 405 (58.2%) | 4,194 (45.7% of repeat parents completing the screener) |
| Effectiveness | ||||||
| Smokers at the visit requesting a prescription for nicotine replacement therapy (NRT) | 500 (74.3%) | 210 (36.8%) | 177 (43.3%) | 374 (60.55) | 301 (59.8%) | 1,562 (56.3% of smokers at visit) |
| Percent of smokers who requested prescription for NRT, who received the prescription at that visit n (%) | 95.6% | 99.5% | 91.1% | 89.7% | 91.7% | 93.6% |
| Total households with smokers requesting enrollment in the quitline | 837 | 176 | 175 | 281 | 224 | 1,693 |
| Percent of smokers who requested quitline connection, who received the quitline enrollment form at that visit n (%) | 97.2% | 100% | 86.9% | 85.5% | 88.8% | 93.4% |
| Implementation | ||||||
| Staff handing out iPads (total number of times in 2 years) | 8,380 | 6,764 | 6,755 | 15,426 | 12,786 | 50,111 |
| Staff handing out CEASE Action Sheets to new households with tobacco users | 1,214 (90.5%) | 1,314 (98.3%) | 778 (69.2%) | 968 (59.7%) | 716 (83.6%) | 4,990 (79.4% of new households with tobacco users) |
| Maintenance | ||||||
| Staff handing out CEASE Action Sheet to repeat parents | 1,466 (91.6%) | 586 (97.5%) | 311 (37.2%) | 156 (24.9%) | 161 (68.8%) | 2,680 (68.7% of repeat households with tobacco user) |
| Staff handing out quitline enrollment forms to repeat parents who requested quitline connection | 364 (96.8%) | 35 (100%) | 45 (78.9%) | 26 (76.5%) | 38 (97.45) | 508 (93.9% of repeat parents requesting quitline enrollment) |
The adoption rate is 100% because by definition, all practices agreed to hand out the iPad as part of the study. Some percentages may not add up due to missing values.
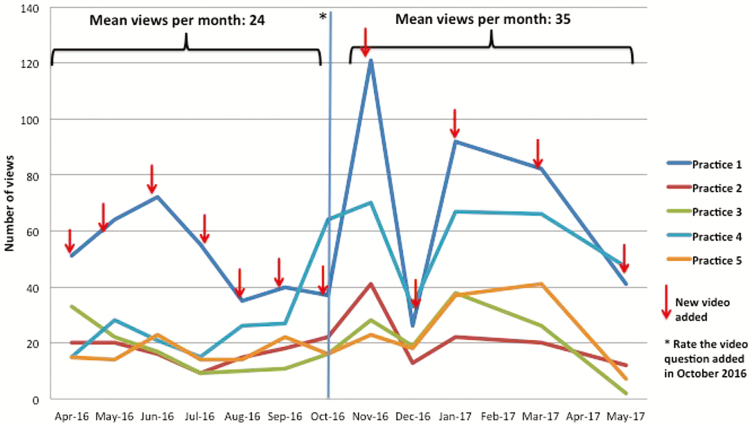
The number of video views by practice by month is shown in Fig. 4. Video ratings were added to the screener on October 14, 2016. Nicotine replacement therapy requests increased from 59% in the 3 months before adding the rating question to 64% in the 3 months after adding the rating question. Similarly, request for quitline enrollment increased from 34% in the 3 months before adding the rating question to 43% after adding the rating question. In our study, we found that smoking parents watched and rated highly videos that were meant to be funny but had an important message like the CATMageddon video by Truth initiative (https://www.youtube.com/watch?v=tLtschJxRy8&feature=youtu.be), that highlighted new concepts related to smoking like the third-hand smoke video by KidsHealth.org (https://www.youtube.com/watch?v=eAXpYhGeRFE), or that had a quit message from former smokers like CDC’s Cessation Tips Ad (https://www.youtube.com/watch?v=d6iS44aHy4s).
Fig. 4.
Video views by practice.
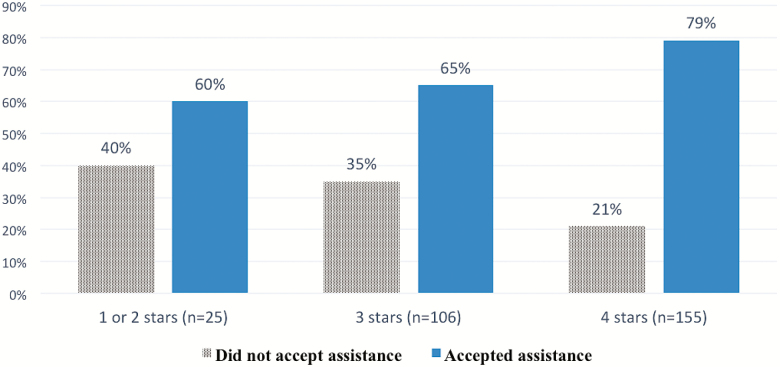
More parents who provided a rating of the video (87%) requested tobacco cessation assistance (prescription for NRT or referral to quitline) than those who declined to watch (13%) the video (p = .05). Parents who rated the video 4 stars out of 4 (59%) were more likely to request assistance compared with those who rated the video less than 4 stars (40%; p = .02). Figure 5 shows the association between the video ratings and acceptance of assistance. Of the parents who declined to answer the question about household tobacco use, 218 watched the video. Of those, 6% requested tobacco cessation assistance services.
Fig. 5.
Acceptance of assistance on the iPad by video rating (N = 286). p = .021.
DISCUSSION
The incorporation of an electronic screener showed high and sustained rates of screening families for household tobacco use, and subsequent request and delivery of tobacco control assistance to smokers. A high number of smokers present at the visit requested cessation services (NRT prescription [57%] and quitline connection [41%]) and over 90% of them were given either a prescription or quitline enrollment form. Of the 41% who requested connection to the quitline, 93% were given the enrollment form. Furthermore, 14% of parents asked to be connected to the quitline on repeat visits, emphasizing the need to consistently and routinely offer tobacco cessation assistance over time.
In addition to the logistical advantage of using an electronic previsit screening tool, there may be additional reasons why this screener led to high rates of documentation and request for tobacco cessation assistance services by smoking parents. By using photos of practice staff, the familiar faces on the tablet added a personal touch to the screener. Nonsmoking families were quickly identified by the screener; for nonsmokers, the screener ended after one question to minimize the burden on the practice and parents. Families with a smoking parent who had completed the screener in the prior 6 months were given a shortened version of the screener to reduce their time burden. These strategies were intended to streamline the screening process for the practices and enhance the potential for sustainable practice change.
Table 3 maps the major steps of the CEASE intervention to aspects of the RE-AIM framework to explore how and to what extent practices engaged with the CEASE intervention. Table 3 and Fig. 3 show the variability in screening households for tobacco use in the five practices. These data also prompted further investigation to understand potential reasons behind differences between practices. Based on feedback from the practices during their discussions with study staff, the variability in handing out the iPads was due to the following factors: (a) Migration to a new electronic health record (EHR) system in one practice, which led to the increased work load of the front desk staff till all parents were manually entered by them at check-in; (b) Staff turnover at the front desk in four practices; (c) Shortage of staff at front desk when the regular front desk person was on sick or maternity leave. The screener data presented in Table 3 and Fig. 3 and the feedback from practices provided real-time, actionable, and specific quality improvement data for practices and for future versions of CEASE.
As seen in Fig. 4, there was variability in the number of video views per practice. One practice had consistently high number of families watching the videos incorporated in the screener. Based on feedback from the staff at this practice, the CEASE team found out that they handed out the iPads in the examination rooms and encouraged all parents to watch the videos while handing out the iPad. Parents may have had more time in the examination room to watch the video or the secluded environment of the examination room may have given parents a sense of privacy to watch the videos, which may have led to increased video views but the exact reason is unclear.
Videos were incorporated into the screener, giving parents the option of watching motivational content on smoking cessation and the harms of tobacco use and exposure to motivate acceptance of NRT and quitline services. Six per cent of those who did not want to answer the question about household tobacco use but did watch the video ended up requesting tobacco cessation assistance services. It appears that the videos embedded in the electronic screener prompted additional parents to request services that they might otherwise not have received because they did not identify their households as having a smoker.
Another benefit of integrating the videos into the screener is its ability to repeatedly disseminate messages over time at low cost. Although we were concerned that people might not watch the videos, many people did and the addition of the “rate the video” question increased the overall video views and helped us to determine which kind of videos people preferred. The rate the video question was preceded by the following text: “Let your voice be heard. Please watch this short video and rate it.” It is not clear why adding the rating question increased video views but it is possible that providing viewers the opportunity to “rate” the video, a practice common on social media, increased their sense of personal involvement with the platform.
Showing informational videos on the screener in the child healthcare setting communicates important information to parents who may not otherwise be reached by these messages. A review of the literature on the use of mass media for smoking cessation concluded that socioeconomically disadvantaged populations may have lower rates of exposure to the media [58]. In the USA, those living in poverty and those with lower educational attainment have barriers to accessing tobacco dependence treatment [59,60]. The CEASE study shows that the pediatric setting can provide an opportunity to deliver motivational videos about the harms of tobacco use and to promote and increase access for smoking cessation services. Advertisements that evoke strong emotional responses through negative visceral imagery or personal stories about the health effects of smoking can increase attention, generate greater recall and appeal, and influence smoking beliefs and intentions [61,62]. However, these videos may not be suited for child healthcare settings where children may also be looking at the screen. Studies are needed to better understand which kind of videos are watched by parent and adolescent tobacco users and the effectiveness of these videos on motivating behavioral change.
STRENGTHS
Use of the electronic tablet screener to identify tobacco use within families made the screening process quick and efficient by ending the screener after just one question for those parents who did not have a household smoker. The electronic screener could be changed easily to promote any new messages or promotions from the state quitline. Real-time data monitoring helped identify any intervention implementation problems at an early stage. Use of videos helped engage and educate parents about the dangers of tobacco smoke and motivated them to quit smoking.
LIMITATIONS
Even though the intervention was designed to integrate into existing office workflows, it increased the workload on pediatric office staff, particularly the front desk staff what had been tasked with handing out the tablet and distributing the CEASE Action Sheet and quitline forms to parents identified by the screener. During busy times, office staff members noted that they were not always able to hand out the tablet. The total number of families seen at the pediatric practices during these 2 years is unknown. Hence, it is difficult to assess how many families were not screened for household tobacco use. We encouraged the staff to hand out of the iPads routinely at all visits so that the few families that are missed at some visits are screened at subsequent visits.
Secondly, although identification of families with tobacco use was performed electronically, assistance delivery (quitline and NRT) was not fully automated. Delivery of assistance still relied on staff or clinician action, and not all parents who indicated they needed smoking cessation assistance on the screener received it during that visit. In addition, some elements of the intervention such as watching videos were optional, so there was an element of self-selection in intervention delivery. Lastly, because the screener did not auto-populate the child’s record, clinical decision support and billing were not fully automated.
CONCLUSION
The technological innovations used in this study were successfully deployed and sustained in the outpatient pediatric office in five states. These innovations dramatically improved delivery of tobacco control services to parents compared with paper-based intervention. If successfully deployed in child healthcare settings nationally, these innovations could lead to significant reductions in morbidity and mortality across the USA.
Acknowledgments
The authors especially appreciate the efforts of the AAP practices and practitioners who participated in the study.
Funding:
This study was supported by the National Institutes of Health, National Cancer Institute grant 2R01-CA127127 (to J. P. Winickoff).
Compliance with Ethical Standards
Conflict of Interest: The authors have no financial relationships or conflicts of interest relevant to this article to disclose.
Authors’ Contributions: All authors are responsible for the reported research and have participated in the concept and design, analysis and interpretation of data, drafting or revising the manuscript, and have approved it as submitted.
Ethical Approval: I confirm that all procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. The study protocol was approved by the Institutional Review Boards (IRB) of AAP, Massachusetts General Hospital, and by individual practices’ IRB, when required.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [PubMed]
- 2. U.S. Department of Health and Human Services. The Health Consequences of Involuntary Tobacco Smoke: A Report of the Surgeon General. Altanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 3. Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19(1):3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moylan S, Jacka FN, Pasco JA, Berk M. How cigarette smoking may increase the risk of anxiety symptoms and anxiety disorders: a critical review of biological pathways. Brain Behav. 2013;3(3):302–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DiFranza JR, Savageau JA, Rigotti NA, et al. Trait anxiety and nicotine dependence in adolescents: a report from the DANDY study. Addict Behav. 2004;29(5):911–919. [DOI] [PubMed] [Google Scholar]
- 6. Goriounova NA, Mansvelder HD. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb Perspect Med. 2012;2(12):a012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Counotte DS, Spijker S, Van de Burgwal LH, et al. Long-lasting cognitive deficits resulting from adolescent nicotine exposure in rats. Neuropsychopharmacology. 2009;34(2):299–306. [DOI] [PubMed] [Google Scholar]
- 8. Counotte DS, Goriounova NA, Li KW, et al. Lasting synaptic changes underlie attention deficits caused by nicotine exposure during adolescence. Nat Neurosci. 2011;14(4):417–419. [DOI] [PubMed] [Google Scholar]
- 9. Stocks J, Hislop A, Sonnappa S. Early lung development: lifelong effect on respiratory health and disease. Lancet Respir Med. 2013;1(9):728–742. [DOI] [PubMed] [Google Scholar]
- 10. Hayatbakhsh MR, Sadasivam S, Mamun AA, Najman JM, Williams GM, O’Callaghan MJ. Maternal smoking during and after pregnancy and lung function in early adulthood: a prospective study. Thorax. 2009;64(9):810–814. [DOI] [PubMed] [Google Scholar]
- 11. Bek K, Tomaç N, Delibas A, Tuna F, Teziç HT, Sungur M. The effect of passive smoking on pulmonary function during childhood. Postgrad Med J. 1999;75(884):339–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGrath-Morrow SA, Hayashi M, Aherrera A, et al. The effects of electronic cigarette emissions on systemic cotinine levels, weight and postnatal lung growth in neonatal mice. Plos One. 2015;10(2):e0118344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dejmek J, Solansk y I, Podrazilová K, Srám RJ. The exposure of nonsmoking and smoking mothers to environmental tobacco smoke during different gestational phases and fetal growth. Environ Health Perspect. 2002;110(6):601–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leonardi-Bee J, Smyth A, Britton J, Coleman T. Environmental tobacco smoke and fetal health: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2008;93(5). doi:10.1136/adc.2007.133553. [DOI] [PubMed] [Google Scholar]
- 15. Prescott SL. Effects of early cigarette smoke exposure on early immune development and respiratory disease. Paediatr Respir Rev. 2008;9(1):3–10. doi:10.1016/j.prrv.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 16. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in schoolchildren. Am J Epidemiol. 2003;157(10):861–869. [DOI] [PubMed] [Google Scholar]
- 17. Taylor SM, Ross NA, Cummings KM, et al. Community Intervention Trial for Smoking Cessation (COMMIT): changes in community attitudes toward cigarette smoking. Health Educ Res. 1998;13(1):109–122. [DOI] [PubMed] [Google Scholar]
- 18. Winickoff JP, Healey EA, Regan S, et al. Using the postpartum hospital stay to address mothers’ and fathers’ smoking: the NEWS study. Pediatrics. 2010;125(3):518–525. [DOI] [PubMed] [Google Scholar]
- 19. den Exter Blokland EA, Engels RC, Hale WW 3rd, Meeus W, Willemsen MC. Lifetime parental smoking history and cessation and early adolescent smoking behavior. Prev Med. 2004;38(3):359–368. [DOI] [PubMed] [Google Scholar]
- 20. Farkas AJ, Distefan JM, Choi WS, Gilpin EA, Pierce JP. Does parental smoking cessation discourage adolescent smoking? Prev Med. 1999;28(3):213–218. [DOI] [PubMed] [Google Scholar]
- 21. Bricker JB, Leroux BG, Peterson AV Jr, et al. Nine-year prospective relationship between parental smoking cessation and children’s daily smoking. Addiction. 2003;98(5):585–593. [DOI] [PubMed] [Google Scholar]
- 22. Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338(8):513–519. [DOI] [PubMed] [Google Scholar]
- 23. Hall N, Hipple B, Friebely J, Ossip DJ, Winickoff JP. Addressing family smoking in child health care settings. J Clin Outcomes Manag. 2009;16(8):367–373. [PMC free article] [PubMed] [Google Scholar]
- 24. Winickoff JP, Nabi-Burza E, Chang Y, et al. Implementation of a parental tobacco control intervention in pediatric practice. Pediatrics. 2013;132(1):109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nabi-Burza E, Winickoff JP, Finch S, Regan S. Triple tobacco screen: opportunity to help families become smokefree. Am J Prev Med. 2013;45(6):728–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Winickoff JP, Hipple B, Drehmer J, et al. The Clinical Effort Against Secondhand Smoke Exposure (CEASE) intervention: a decade of lessons learned. J Clin Outcomes Manag. 2012;19(9):414–419. [PMC free article] [PubMed] [Google Scholar]
- 27. Winickoff JP, Park ER, Hipple BJ, et al. Clinical effort against secondhand smoke exposure: development of framework and intervention. Pediatrics. 2008;122(2):e363–e375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Winickoff JP, Hillis VJ, Palfrey JS, Perrin JM, Rigotti NA. A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003;111(1):140–145. [DOI] [PubMed] [Google Scholar]
- 29. Winickoff JP, Berkowitz AB, Brooks K, et al. State-of-the-art interventions for office-based parental tobacco control. Pediatrics. 2005;115(3):750–760. doi:10.1542/peds.2004-1055 [DOI] [PubMed] [Google Scholar]
- 30. Winickoff JP, Nabi-Burza E, Chang Y, et al. Sustainability of a parental tobacco control intervention in pediatric practice. Pediatrics. 2014;134(5):933–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Service Department of Health, Human Services. Public Health, eds. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; May 2008. [Google Scholar]
- 32. Tanski SE, Klein JD, Winickoff JP, Auinger P, Weitzman M. Tobacco counseling at well-child and tobacco-influenced illness visits: opportunities for improvement. Pediatrics. 2003;111(2):E162–7. [DOI] [PubMed] [Google Scholar]
- 33. Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 34. Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care. 2005;43(5):436–444. [DOI] [PubMed] [Google Scholar]
- 35. Si D, Bailie R, Weeramanthri T. Effectiveness of chronic care model-oriented interventions to improve quality of diabetes care: a systematic review. Prim Health Care Res Dev. 2008;9(01):25–40. doi:10.1017/S1463423607000473 [Google Scholar]
- 36.RE-AIM. Re-Aim Planning Tool. Re-AimOrg. 2010;10:1-5. Available at: http://www.re-aim.org/resources-and-tools/self-rating-quiz/. Accessed May 1, 2019.
- 37. Glasgow RE. RE-AIMing research for application: ways to improve evidence for family medicine. J Am Board Fam Med. 2006;19(1):11–19. [DOI] [PubMed] [Google Scholar]
- 38. Shediac-Rizkallah MC, Bone LR. Planning for the sustainability of community-based health programs: conceptual frameworks and future directions for research, practice and policy. Health Educ Res. 1998;13(1):87–108. [DOI] [PubMed] [Google Scholar]
- 39. Proctor E, Luke D, Calhoun A, et al. Sustainability of evidence-based healthcare: research agenda, methodological advances, and infrastructure support. Implement Sci. 2015;10:88. doi:10.1186/s13012-015-0274-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Johnson K, Hays C, Center H, Daley C. Building capacity and sustainable prevention innovations: a sustainability planning model. Eval Program Plann. 2004;27(2):135–149. doi:10.1016/j.evalprogplan.2004.01.002 [Google Scholar]
- 41. Scheirer MA, Hartling G, Hagerman D. Defining sustainability outcomes of health programs: Illustrations from an on-line survey. Eval Program Plann. 2008;31(4):335–346. [DOI] [PubMed] [Google Scholar]
- 42. Walters BH, Ossip DJ, Drehmer JE, et al. Clinician telephone training to reduce family tobacco use: analysis of transcribed recordings. J Clin Outcomes Manag. 2016;23(2):79–86. [PMC free article] [PubMed] [Google Scholar]
- 43. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wiltsey Stirman S, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012;7:17. doi:10.1186/1748-5908-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Burnett KF, Young PC. Ask, advise, assist: pediatricians and passive smoke exposure. Clin Pediatr. 1999;38(6):339–345. [DOI] [PubMed] [Google Scholar]
- 46. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ortiz DD. Using a simple patient registry to improve your chronic disease care. Fam Pract Manag. 2006;13(4):47–8, 51. [PubMed] [Google Scholar]
- 48. Schmittdiel J, Bodenheimer T, Solomon NA, Gillies RR, Shortell SM. Brief report: the prevalence and use of chronic disease registries in physician organizations. A national survey. J Gen Intern Med. 2005;20(9):855–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Metzger J. Using Computerized Registries in Chronic Disease Care. Oakland, Calif: California Healthcare Foundation; 2004. [Google Scholar]
- 50. Stroebel RJ, Scheitel SM, Fitz JS, et al. A randomized trial of three diabetes registry implementation strategies in a community internal medicine practice. Jt Comm J Qual Improv. 2002. doi:10.1016/S1070-3241(02)28044-X [DOI] [PubMed] [Google Scholar]
- 51. Renders CM, Valk GD, Griffin SJ, Wagner E, van Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2000. doi:10.1002/14651858.CD001481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Harris MF, Priddin D, Ruscoe W, Infante FA, O’Toole BI. Quality of care provided by general practitioners using or not using Division-based diabetes registers. Med J Aust. 2002;177(5):250–252. [DOI] [PubMed] [Google Scholar]
- 53. Golechha M. Health promotion methods for smoking prevention and cessation: a comprehensive review of effectiveness and the way forward. Int J Prev Med. 2016;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sly DF, Hopkins RS, Trapido E, Ray S. Influence of a counteradvertising media campaign on initiation of smoking: the Florida “truth” campaign. Am J Public Health. 2001;91(2):233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sly DF, Trapido E, Ray S. Evidence of the dose effects of an antitobacco counteradvertising campaign. Prev Med. 2002;35(5):511–518. [DOI] [PubMed] [Google Scholar]
- 56. Evans WD, Price S, Blahut S, Hersey J, Niederdeppe J, Ray S. Social imagery, tobacco independence, and the truthsm campaign. J Health Commun. 2004;9(5):425–441. [DOI] [PubMed] [Google Scholar]
- 57. Farrelly MC, Healton CG, Davis KC, Messeri P, Hersey JC, Haviland ML. Getting to the truth: evaluating national tobacco countermarketing campaigns. Am J Public Health. 2002;92(6):901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Niederdeppe J, Kuang X, Crock B, Skelton A. Media campaigns to promote smoking cessation among socioeconomically disadvantaged populations: What do we know, what do we need to learn, and what should we do now? Soc Sci Med. 2008;67(9):1343–1355. doi:10.1016/j.socscimed.2008.06.037 [DOI] [PubMed] [Google Scholar]
- 59. Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults—United States 2005–2014. Morbidity and Mortality Weekly Report 2015;64(44):1233–40. No Title. [DOI] [PubMed] [Google Scholar]
- 60. Moritsugu KP. The 2006 report of the surgeon general: the health consequences of involuntary exposure to tobacco smoke. Am J Prev Med. 2007;32(6):542–543. [DOI] [PubMed] [Google Scholar]
- 61. Biener L, Reimer RL, Wakefield M, Szczypka G, Rigotti NA, Connolly G. Impact of smoking cessation aids and mass media among recent quitters. Am J Prev Med. 2006;30(3):217–224. [DOI] [PubMed] [Google Scholar]
- 62. Farrelly MC, Niederdeppe J, Yarsevich J. Youth tobacco prevention mass media campaigns: past, present, and future directions. Tob Control. 2003;12(Suppl 1):i35–47. doi:10.1136/tc.12.suppl_1.i35 [DOI] [PMC free article] [PubMed] [Google Scholar]