Abstract
Repair of transposition of the great arteries usually involves an atrial switch or arterial switch operation, which can complicate physiological adaptation to the demands of pregnancy and adversely affect the fetus. We retrospectively compared outcomes of 48 completed pregnancies in 23 women with surgically corrected transposition of the great arteries (38 atrial switch/10 arterial switch operation) under joint cardiac-obstetric care in our tertiary referral clinic between 1997 and 2017. Most women delivered vaginally (85%). The pre-term delivery rate was high (atrial switch 39%; arterial switch operation 40%). Small for gestational age occurred in 56% of babies, significantly more in the atrial switch group (66%) than arterial switch operation (20%), p = 0.013. Women with surgically corrected transposition of the great arteries wishing to become pregnant are at high risk of obstetric complications, primarily pre-term delivery and small for gestational age baby. They require more careful ultrasound surveillance beyond 36 weeks’ gestation and/or may benefit from early induction of labour.
Trial registration: Text/Not applicable.
Keywords: Transposition of the great arteries, dextro-transposition of the great arteries, atrial switch procedure, Mustard, Senning, arterial switch operation, obstetric outcomes, small for gestational age
Introduction
Congenital heart disease (CHD) affects 8 in 1000 live births.1 More affected women are surviving into adulthood, having undergone complex cardiac surgery in childhood and are undertaking pregnancy.
Complete transposition of the great arteries (TGA) or dextro-transposition of the great arteries (d-TGA) accounts for approximately 5%–7% of CHD.2 In d-TGA, there is ventricular–arterial discordance with the aorta arising from the morphological right ventricle (RV) and the pulmonary artery from the morphological left ventricle (LV). The atrial switch procedure, developed by Mustard3 and Senning,4 was the first operation to enable survival beyond infancy. It involves redirection of venous blood flow within the atrial compartment, leaving the morphological right ventricle supporting the systemic circulation.
Pregnancy outcomes in women with an atrial switch have been described in the literature.5–9 Cardiac risks include deterioration of ventricular function, heart failure and arrhythmias.10 Obstetric risks include pre-term delivery and small for gestational age babies (SGA, defined as birthweight below the 10th centile).
The atrial switch procedure was superseded by the arterial switch operation (ASO). First successfully performed in 1975 by Jatene et al.,11 it involves transection and ‘re-plumbing’ of the great arteries to restore near normal anatomy and physiology. The pulmonary arteries come to lie anterior to the aorta and the coronary arteries are re-implanted into the neo-aorta. Survival has increased with refinement of surgical techniques and 20-year survival now approaches 90%.12 Long-term complications include (supra) pulmonary stenosis, neo-aortic valve regurgitation, neo-aortic dilatation and coronary artery complications.
Adult survivors of the ASO are now undertaking pregnancy. The first reported outcome was in 2006 in a woman who had an ASO in 1978 and subsequent replacement of the pulmonary valve without further complications nor significant haemodynamic sequelae. An SGA baby was successfully delivered at term by emergency caesarean section for fetal distress.13
With limited data, it was assumed that that preservation of the left ventricle as the systemic ‘pump’ would mean fewer cardiac events and obstetric complications in pregnant women. The only published series to date by Tobler et al.14 states a 15% (2/13) rate of adverse cardiac events and incomplete obstetric outcome data.
As an adult congenital heart disease (ACHD) centre and tertiary level maternal medicine service, our unit has over 20 years’ experience in the multi-disciplinary team (MDT) management of women with surgically corrected TGA in pregnancy.
We report and compare obstetric outcomes in women with congenital TGA, corrected by either an atrial switch procedure or an ASO. We have previously published our cardiac complications experienced during pregnancy after atrial switch.15 Therefore, here, we aim to compare the obstetric and neonatal outcomes between the two surgical repair groups, and provide advice for the safe obstetric management for such women.
Methods
This was a retrospective cohort study. Women with TGA that had been surgically corrected with either an atrial switch procedure or an ASO and had undertaken pregnancy were identified from the database at our tertiary cardiac/maternal medicine antenatal clinic at St Michael’s Hospital, Bristol. Patient records were reviewed for those who delivered beyond 24 weeks’ gestation between 1997 and 2017. Cases prior to 1997 were not included as databases were not well established and data were incomplete.
Data collection involved multiple sources: hard copies and electronic patient records from different systems: Evolve, PODS viewer, Medway, Medway Maternity, the cardiac/maternal medicine clinic and Viewpoint databases.
Baseline data were recorded for both groups, including age, parity, smoking status, body mass index (BMI), type of primary repair, age at primary surgery and pre-pregnancy medications.
Obstetric outcome data were recorded, including gestation at delivery, birthweight and birthweight centile. SGA (those with birthweight under the 10th centile) neonates were sub-divided into those predicted by antenatal ultrasound assessment and those not predicted, induction of labour (IOL) and reasoning, mode of delivery and analgesia. Birthweight centiles were taken from WHO growth charts and adjusted for gender.16
Neonatal outcome data included: live births, pre-term delivery (under 37 weeks), presence of pre-labour, pre-term rupture of membranes (PPROM) or pre-labour rupture of membranes (PROM), APGAR scores, admission to neonatal intensive care unit (NICU) and neonatal morbidity.
Obstetric complications included: post-partum haemorrhage (PPH), antepartum haemorrhage (APH), PPROM, PROM, pre-term delivery, spontaneous pre-term labour, obstetric cholestasis, intrapartum sepsis, thromboembolic events, pre-eclampsia (also known as pre-eclamptic toxaemia or PET), defined by NICE as new onset hypertension of over 140/90 mmHg after 20 weeks of gestation with significant proteinuria (urinary protein: creatinine ratio greater than 30 mg/mmol])17 and gestational hypertension, defined as new hypertension >140/90 mmHg after 20 weeks of gestation, without significant proteinuria.17
Miscarriages were not included as it was not possible to ensure inclusion of all cases retrospectively.
Statistical methods
Median values and ranges were calculated for continuous variables where appropriate. Descriptive statistics for nominal data were expressed in absolute numbers and percentages. Comparison of the occurrence of complications between the two groups was performed using Fisher’s exact test and the Mann–Whitney U test. A p-value <0.05 was considered statistically significant. Data were presented as mean ± standard deviation for parametric data and median and range for non-parametric data.
Results
There were 48 completed pregnancies in 23 women. Nineteen women who had undergone an atrial switch procedure delivered 38 babies and 4 women who had undergone an ASO had 10 babies. Baseline characteristics of both groups are shown in Table 1, and there were no statistically significant differences between the two groups.
Table 1.
Baseline characteristics of women undergoing pregnancy after atrial switch or ASO.
| Type of cardiac repair | Atrial switch, n | ASO, n | p Value |
|---|---|---|---|
| Women | 19 | 4 | |
| Pregnancies >24 weeks | 38 | 10 | |
| Smoker | 4 (20%) | 2 (50%) | 0.27 |
| Age (years; median + range) | 24.5 (16–36) | 25.5 (21–30) | 0.40 |
| BMI (kg/m2; median + range)) | 22.6 (17.9–40) | 24.5 (15.5–28) | 0.40 |
| Parity | 19 primagravidae (50%) | 4 primagravidae (40%) | 0.73 |
| Cardiac medication during pregnancy | 8 (21%) | 2 (20%) | 1.00 |
Obstetric outcomes
Obstetric outcomes are shown in Table 2. Most women delivered vaginally (85%), significantly more in the atrial switch group than the ASO group (92% vs. 60%, p = 0.027).
Table 2.
Obstetric outcomes.
| Atrial switch, n = 38 (%) | ASO, n = 10 (%) | p Value | |
|---|---|---|---|
| Induction of labour | 30 (79) | 6 (60) | 0.24 |
| Geography | 6 | 4 | |
| Fetal concerns | 13 | 3 | |
| Maternal cardiac condition | 10 | 0 | |
| Maternal obstetric reasons | 8 | 2 | |
| Maternal and fetal indications | 7 | 3 | |
| Vaginal delivery | 35 (92) | 6 (60) | 0.03 |
| Normal vaginal delivery | 25 (71) | 5 (50) | |
| Instrumental delivery | 10 (29) | 1 (10) | |
| Forceps delivery | 8 (23) | 1 (10) | |
| Ventouse delivery | 2 (6) | 0 (0) | |
| Caesarean section | 3 (8) | 4 (40) | 0.03 |
| Elective | 3 | 1 | |
| Emergency | 0 | 3 | |
| Total post-partum haemorrhage (PPH) | 9 (24) | 2 (20) | 1.00 |
| PPH 500–1000 ml | 6 (16) | 0 | 0.32 |
| PPH > 1000 ml | 3 (8) | 2 (20) | 0.28 |
| Antepartum haemorrhage | 5 (13) | 0 | 0.57 |
| Pulmonary embolus | 2 (5) | 0 | 1.00 |
| Malpresentation (breech) | 1 (3) | 0 | 1.00 |
| Idiopathic thrombocytopenic purpura | 1 (3) | 0 | 1.00 |
| Manual removal of placenta | 0 | 2 (20) | 0.04 |
| Pre-eclampsia | 1 (3) | 0 | 1.00 |
| Pregnancy-induced hypertension | 1 (3) | 0 | 1.00 |
Of the women who had an atrial switch and a vaginal delivery 25/35 (71%) delivered normally and 10/35 (29%) had an instrumental delivery, 9 of which were following a reduced second stage or planned, elective instrumental delivery. A reduced second stage consisted of 30 min of active pushing, whilst a passive second stage consisted of an early epidural, 2 h of passive descent (once fully dilated) and an elective forceps delivery without maternal effort. The decision for a reduced or passive second stage was based on maternal antenatal cardiac status. In the ASO group, only one woman had instrumentation, again this was performed electively, for cardiac reasons. Regarding epidural use, 19/35 (54%) of women who delivered vaginally in the atrial switch group had an epidural, as did 4/6 (67%) of the ASO group. All caesarean sections were performed for obstetric reasons (previous caesarean section, breech presentation).
Most women were induced (79% atrial switch vs. 60% ASO, p = 0.24), there was no significant difference between the two groups. The most common reason for induction in both groups was fetal concern (suspected IUGR consisting of reduced growth velocity, and/or oligohydramnios, and/or abnormal Dopplers suggesting arterial or venous dysfunction) (43% atrial switch vs. 50% ASO, p = 1.00). Maternal concern (largely deterioration in cardiac status) was more often the cause for IOL in the atrial switch group than in the ASO group (33% vs. 0%, p = 0.16) and some women were induced for multiple reasons.
Overall the rate of post-partum haemorrhage was higher than background rate of 12.7%,18 the reason for this is unclear but it seems similar to published rates of PPH in women with cardiac disease.5 There was no difference between the two groups (atrial switch 9/38 (24%) vs. ASO 2/10 (20%), p = 1.00). Antepartum haemorrhage was more common in the atrial switch group (atrial switch 5/38 (13%) vs. ASO 0/10 (0%), p = 0.57) but not significantly so. Other obstetric complications were rare in both groups.
Neonatal outcomes
Neonatal outcomes are reported on Table 3. All pregnancies resulted in live births and there were no neonatal deaths. There was no difference in mean gestation at delivery (atrial switch 37 + 1 vs. ASO 36 + 2 weeks, p = 0.218) or mean birthweight (atrial switch 2515 g vs. ASO 2630 g, p = 0.939).
Table 3.
Neonatal outcomes.
| Atrial switch, n = 38 | ASO, n = 10 | p value | |
|---|---|---|---|
| Birth weight (g; mean + range) | 2515 (1460–3530) | 2630 (1700–3310) | 0.94 |
| Gestation at delivery (weeks; mean + range) | 37 + 1 (32 + 2 to 40) | 36 + 2 (32 + 0 to 38 + 3) | 0.22 |
| SGA (birthweight <10th centile) | 25 (66%) | 2 (20%) | 0.01 |
| US detected SGA | 9 (24%) | 1 (10%) | 0.66 |
| PPROM | 4 (11%) | 0 | 0.57 |
| PROM | 0 | 1 (10%) | 0.21 |
| Pre-term delivery | 15 (39%) | 4 (40%) | 1.00 |
| Induction of labour | 11 | 2 | |
| Spontaneous | 4 | 2 | |
| APGAR scores ≤7 at 1 min | 5 (13%) | 1 (10%) | 1.00 |
| Admission to NICU | 8 (21%) | 1 (10%) | 0.66 |
| 5/8 under 37 weeks | 1/1 under 37 weeks | ||
| Transitional care admission | 12 (32%) | 3 (30%) | 1.00 |
| >34 weeks ± <2.5 kg | 10/12 under 37 weeks | 3/3 under 37 weeks |
NICU: neonatal intensive care unit; PPROM: pre-term, pre-labour rupture of membranes; PROM: pre-labour rupture of membranes; SGA: small for gestational age; US: ultrasound.
The number of SGA babies was high overall, 27/48 (56%) but significantly higher in the atrial switch group (atrial switch – 25/38 (66%) vs. ASO 2/10 (20%), p = 0.013). Only 10/27 (37%) were diagnosed at <10th centile by ultrasound prior to delivery.
The number of pre-term deliveries was similar in each group (atrial switch 15/38 (39%) vs. ASO 4/10 (40%), p = 1.00) and there was no difference in the finding of an APGAR scores of less than 7 at 1 min (atrial switch 5/38 (13%) vs. ASO 1/10 (10%), p = 1.00) or the number of admissions to NICU (atrial switch 8/38 (21%) vs. ASO 1/10 (10%), p = 0.66) or transitional care (atrial switch 12/38 (32%) vs. ASO 3/10 (30%), p = 1.00).
Additional neonatal morbidity included two cases of cerebral palsy (both in the atrial switch group). The first was born at 36 weeks’ gestation, following PPROM at 30 weeks; the fetus was SGA and delivery was out of area. The second was born at 34 weeks’ gestation, following IOL for deteriorating maternal cardiac condition. No CHD was diagnosed in the neonates.
Discussion
With improvement in survival following surgical correction of TGA, more women are choosing to undertake the challenge of pregnancy. It is therefore increasingly important to understand the associated risks and offer such women the safest care possible.
Vaginal delivery is preferred following corrected TGA. We were encouraged to see that 85% women overall delivered vaginally and that all caesarean sections were performed for obstetric indications. Instrumental delivery was more commonly used in the atrial switch group to permit a cardio-protective second stage.
IOL was common for fetal reasons in both groups but a quarter of women in the atrial switch group were induced for maternal cardiac reasons compared to none in the ASO group, reflecting the different cardiac anatomy.
The rate of PPH was higher than the background rate18 in both groups, the reason for this is not clear but it did not appear to be associated with mode of delivery.
The 39%–40% rate of preterm delivery was high in both groups and significantly higher than the background risk.19 As shown in Table 4, this has previously been reported as between 25% and 50% post-atrial switch.5,6,8,9 Women in our series typically delivered their babies at 36–37 weeks, which earlier than reported in other studies.6,7
Table 4.
A comparison of reported obstetric outcomes.
|
ASO |
Atrial switch |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tobler et al.14 | Current study | Drenthen et al.5 | Trigas et al.6 | Guedes et al.7 | Canobbio et al.8 | Metz et al.9 | Current study | ||
| n = (women/pregnancies) | 9/13 | 4/10 | 28/49a | 34/44 | 16/28 | 54/40 | 10/14 | 19/38 | |
| Age at delivery (years) | 22 | 26 | 25.8 | 25 | – | – | 23.4 | 25 | |
| Gestation at delivery (weeks) | – | 36 + 2 | 36 + 5 | 39 + 0 | 38 + 1 | – | 35 + 6 | 37 + 1 | |
| Pre-term delivery | 0 | 4 (40%) | 16(31%) | 11(25%) | – | 19(39%) | 7 (50%) | 15 (39%) | |
| Spontaneous pre-term labour | – | 2 (20%) | 12(24%) | – | – | – | 2 (14%) | 4 (11%) | |
| SGA <10th centile | 1 (8%)b | 2 (20%) | 11(22%) | 5(8.3%) | – | – | – | 25 (66%) | |
| US detected SGA | – | 1 (10%) | – | – | – | – | – | 9 (24%) | |
| PPROM | – | 0 (0%) | 7(14%) | 10(16.7%) | – | – | 2 (14%) | 4 (11%) | |
| Postpartum haemorrhage | – | 2 (20%) | 7(14%) | – | – | – | – | 9 (24%) | |
| Pregnancy-induced hypertension | – | 0 (0%) | 4(8.2%) | – | – | – | – | 1 (3%) | |
| Pre-eclampsia | – | 0 (0%) | 5(10.2%) | 1(1.7%) | – | – | 1 (7%) | 1 (3%) | |
| Thromboembolic events | – | 0 (0%) | 2(4.1%) | – | – | – | – | 2 (5%) | |
| NICU admission | – | 1 (10%) | – | – | – | – | – | 8 (21%) | |
| APGARS <7 at 1 minute | – | 1 (10%) | – | – | – | – | – | 5 (13%) | |
| Neonatal morbidity | – | 0 (0%) | – | – | – | – | – | 0 (0%) | |
| Perinatal mortality | 0 | 0 (0%) | 2(4%) | – | – | – | 0 (0%) | 0 (0%) | |
| CHD recurrence | 0 | 0 | 0(0%) | 0(0%) | 0(0%) | 0(0%) | 0 (0%) | 0 | |
CS: Caesarean section; SGA: small for gestational age; US: ultrasound; PPROM: pre-term, pre-labour rupture of membranes; NICU: neonatal intensive care unit; CHD: congenital heart disease.
aObstetric outcomes only available for 48 pregnancies.
bBirthweight data only available for 7/13 births.
Table 5.
Maternal cardiac status and outcomes.
| Patient no./pregnancies | Cardiac status | Systemic ventricular function | NYHA classPreg/class | O2 Sats.>96% | Maternal complications | Cardiac medication | IUGR |
|---|---|---|---|---|---|---|---|
| ASO | |||||||
| 1/4 | RVOT and PA patchmod. TR mod. PR(between 2nd and 3rdpregnancy – TVT and PVR) | Good | 1-12-13-24-2 | No | 1-No2-No3-No4-No | 1-No2-No3-No4-Yesfurosemide | 1-No2-No3-No4-No |
| 2/2 | RVOT patchmod PRmod TR | Good | 1-22-2 | No | No | No | 1-No1-Yes |
| 3/1 | PA patch repairCABG | Good | 1 | No | No | 1-Yesbisoprolol | 1-Yes |
| 4/2 | 1-severe PRbetween 1 and 2 – PVRTVR | Good | 1 | No | 1-post-natal BV failure2-No | No | 1-No2-No |
| Atrial switch | |||||||
| 1/2 | Normal | Good | 1 | No | No | No | 1-No2-Yes |
| 2/3 | Normal | Good | 1 | No | No | No | 1-Yes2-No3-No |
| 3/2 | Intermittent nodal rhythm | Mild impairment | 2 | No | No | 1-digoxin2-digoxin | 1-No2-No |
| 4/3 | Atrial tachycardiamild TR | Good | 1 | No | No | 1-digoxin2-digoxin3-digoxin | 1-Yes2-Yes3-No |
| 5/3 | Mild TR | Moderate impairment | 1 | No | 1-2-No3 angina | No | 1-Yes2-No3-Yes |
| 6/1 | Intermittent nodal rhythm | Mild impairment | 1 | No | No | No | 1-Yes |
| 7/3 | Baffle leak, pulmonary venous baffle dilatation | Good | 1 | No | No | No | 1-Yes2-Yes3-Yes4-Yes |
| 8/2 | Mild SVC baffle obstruction | Good | 1 | No | No | No | 1-Yes |
| 9/1 | SVT – ablated | Good | 1 | No | SVTbaffle thrombus | 1-Yesdigoxin and labetalol | 1 |
| 10/4 | Small baffle leak | Good | 1 | No | No | No | 1-Yes2-No3-Yes4-Yes |
| 11/2 | Mild TR | Mild impairment | 1 | No | No | No | 1-No2-Yes |
| 12/4 | Normal | 1-good2-mild 3-moderate4-severe impairment | 1-Yes2-Yes3-24-3 | 1-2No3-4Yes | 1-4 escalating RV impairment 4 – angina and nodal rhythm | 1-No2-No3-No4-Yesdigoxin/ISMN | 1-Yes2-No3-No4-Yes |
| 13/1 | Mild TR | Mild impairment | 1 | No | No | No | 1-Yes |
| 14/1 | Mild TR | Mild impairment | 1 | No | Frequent ectopy | 1-Yesbisoprolol | 1-Yes |
| 15/1 | Normal | Good | 1 | Nodal rhythm | No | 1-Yes | |
| 16/2 | Moderate TRNSVT, AT | Moderate impairment | 1 | No | No | 1-Yes 2-Yesbisoprolol | 1-No2-No |
| 17/1 | Mild TR | Mild-moderate impairment | 1 | No | No | No | 1-Yes |
| 18/1 | Baffle obstruction | Good | 1 | No | No | 1-Yeslabetalol | 1-Yes |
| 19/1 | Normal | Mild impairment | 1 | No | Reduced VF | 1-Yesbisoprolol | 1-Yes |
NYHA: New York Heart Association; RVOT: right ventricular outflow tract; PA: pulmonary artery; TR: tricuspid regurgitation; PR: pulmonary regurgitation; TVR: tricuspid valve replacement; PVR: pulmonary valve replacement; CABG: coronary artery bypass graft; SVC: superior vena cava; SVT: supra-ventricular tachycardia; NSVT: non-sustained ventricular tachycardia; AT: atrial tachycardia; BV: bi-ventricular; RV: right ventricle; VF: ventricular function; ISMN: isosorbide mononitrate.
A striking finding was the number of SGA babies born in this cohort. In the only other published series of pregnancies in women with ASO, Tobler et al.14 reported 8% SGA, compared to our 20%, however birthweight was only reported for 7/13 births in that series.
Although SGA is widely reported in the infants of women post-atrial switch, rates have ranged from 8% to 22%,4,5 and 26% in our previously reported data10 whereas in this cohort 66% babies of our post-atrial switch mothers were SGA.
The high rate of SGA could be explained in part by other risk factors for SGA, such as smoking and age.17 However, the number of smokers was similar in both groups and only two mothers in our cohort (both in the atrial switch group) were aged 35 years or older.
We hypothesise that the sub-optimal maternal physiological adaptation to pregnancy, following surgical correction of TGA, results in fetuses being unable to meet their growth potential.
Disappointingly only 37% SGA babies in the atrial switch group were diagnosed antenatally. This is concerning as these women had regular fetal growth surveillance (usually every month from 28 weeks’ gestation). It is likely that the SGA in these women is secondary to placental insufficiency, occurring late in the third trimester and therefore not always recognised by routine clinical assessment and ultrasound.
The risks associated with SGA and prematurity have been well described.20 Structurally normal, SGA fetuses are at increased risk of perinatal mortality and morbidity, hence the preoccupation with their identification and early delivery.
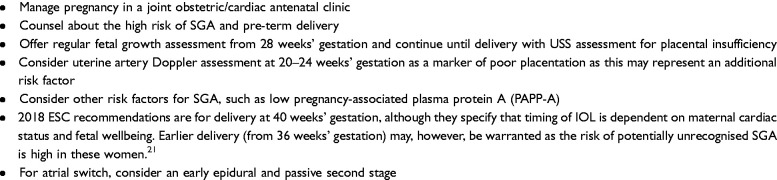
Therefore, we recommend that these women have more intensive obstetric and fetal surveillance and the obstetric management outlined below (see Box 1).
Strengths and limitations
This study represents the largest single centre experience of women with TGA corrected by ASO with detailed obstetric outcomes and the only study comparing outcomes by type of TGA repair. The findings are limited by the retrospective nature of the study and by small numbers, as the condition is rare. Due to the low statistical power and small numbers conclusions must be drawn with caution. However, this paper may be useful in the clinical management of such patients.
Conclusion
Women with surgically corrected TGA who wish to become pregnant are at high risk of obstetric complications, primarily pre-term delivery and delivering an SGA baby. The risk of SGA is greatest after atrial switch, but is still prevalent after the ASO. Mothers with surgically corrected TGA therefore require more careful ultrasound surveillance beyond 36 weeks’ gestation and/or may benefit from early induction of labour. Our data suggests that a high rate of vaginal delivery can be achieved, even in this high-risk group.
These women need specialised pre-pregnancy counselling, antenatal and intrapartum care in a combined cardiac/obstetric antenatal clinic. Recommendations for care of these women are described in Figure 1.
Figure 1.
Recommendations for obstetric care for women with surgically corrected TGA.
Acknowledgements
The patients and staff at the specialist cardiac antenatal clinic.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
This retrospective review was undertaken as part of clinical service evaluation and adhered to local audit protocols and ethical approval. Written, informed consent from patients was therefore not sought.
Informed consent
Not applicable.
Guarantor
JT is the guarantor of the work.
Contributorship
All authors are involved in the preparation of this manuscript.
References
- 1.Warnes CA. Adult congenital heart disease: the challenges of a lifetime. Eur Heart J 2017; 38: 2041–2047. [DOI] [PubMed] [Google Scholar]
- 2.Gelson E, Curry R, Gatzoulis MA, et al. Pregnancy in women with a systemic right ventricle after surgically and congenitally corrected transposition of the great arteries. Eur J Obstet Gynecol Reprod Biol 2011; 155: 146–149. [DOI] [PubMed] [Google Scholar]
- 3.Mustard WT. Successful two-stage correction of transposition of the great vessels. Surgery 1964; 55: 469–472. [PubMed] [Google Scholar]
- 4.Senning A. Surgical correction of transposition of the great vessels. Surgery 1959; 45: 966–980. [PubMed] [Google Scholar]
- 5.Drenthen W, Pieper PG, Ploeg M, et al. Risk of complications during pregnancy after Senning or Mustard (atrial) repair of complete transposition of the great arteries. Eur Heart J 2005; 26: 2588–2595. [DOI] [PubMed] [Google Scholar]
- 6.Trigas V, Nagdyman N, Pildner von Steinburg S, et al. Pregnancy-related obstetric and cardiologic problems in women after atrial switch operation for transposition of the great arteries. Circ J 2014; 78: 443–449. [DOI] [PubMed] [Google Scholar]
- 7.Guedes A, Mercier LA, Leduc L, et al. Impact of pregnancy on the systemic right ventricle after a Mustard operation for transposition of the great arteries. J Am Coll Cardiol 2004; 44: 433–437. [DOI] [PubMed] [Google Scholar]
- 8.Canobbio MM, Morris CD, Graham TP, et al. Pregnancy outcomes after atrial repair for transposition of the great arteries. Am J Cardiol 2006; 98: 668–672. [DOI] [PubMed] [Google Scholar]
- 9.Metz TD, Jackson GM, Yetman AT. Pregnancy outcomes in women who have undergone an atrial switch repair for congenital d-transposition of the great arteries. Am J Obstet Gynecol 2011; 205: 273.e1–273.e5. [DOI] [PubMed] [Google Scholar]
- 10.European Society of Gynecology, Association For European Paediatric Cardiology, German Society For Gender Medicine et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011; 32: 3147–3197. [DOI] [PubMed] [Google Scholar]
- 11.Jatene AD, Fontes VF, Paulista PP, et al. Anatomic correction of transposition of the great vessels. J Thorac Cardiovasc Surg 1976; 72: 364–370. [PubMed] [Google Scholar]
- 12.Villafane J, Lantin-Hermoso MR, Bhatt AB, et al. D-transposition of the great arteries: the current era of the arterial switch operation. J Am Coll Cardiol 2014; 64: 498–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ploeg M, Drenthen W, van Dijk A, et al. Successful pregnancy after an arterial switch procedure for complete transposition of the great arteries. Bjog: Int J O&G 2006; 113: 243–244. [DOI] [PubMed] [Google Scholar]
- 14.Tobler D, Fernandes SM, Wald RM, et al. Pregnancy outcomes in women with transposition of the great arteries and arterial switch operation. Am J Cardiol 2010; 106: 417–420. [DOI] [PubMed] [Google Scholar]
- 15.Cataldo S, Doohan M, Rice K, et al. Pregnancy following Mustard or Senning correction of transposition of the great arteries: a retrospective study. BJOG 2016; 123: 807–813. [DOI] [PubMed] [Google Scholar]
- 16.Kiserud T, Piaggio G, Carroli G, et al. The World Health Organization fetal growth charts: a multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. PLoS Med 2017; 14: e1002220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NICE. Hypertension in pregnancy: the management of hypertensive disorders in pregnancy CG107. 2010. [PubMed]
- 18.Calvert C, Thomas SL, Ronsmans C, et al. Identifying regional variation in the prevalence of postpartum haemorrhage: a systematic review and meta-analysis. PLoS One 2012; 7: e41114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez Bernal A. Overview. Preterm labour: mechanisms and management. BMC Pregnancy Childbirth 2007; 7: S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alberry M, Soothill P. Management of fetal growth restriction. Arch Dis Child Fetal Neonatal Ed 2007; 92: F62–F67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J 2018; 39: 3165–3241. [DOI] [PubMed] [Google Scholar]