Abstract
Background:
Return to sports is an important outcome in ensuring patient satisfaction after knee-replacement surgery. However, few studies have directly compared unicompartmental knee arthroplasty (UKA), total knee arthroplasty (TKA), and patellofemoral arthroplasty (PFA).
Hypothesis:
TKA will result in lower rates of return to sports than either UKA and PFA due to increased complexity and invasiveness.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients who underwent UKA, TKA, or PFA with 1 to 2 years of follow-up were sent a questionnaire regarding return to sports, satisfaction with return to sports, pain, the University of California, Los Angeles activity scale, and the High Activity Arthroplasty Score (HAAS). The patients who underwent either TKA or UKA were matched 2:1 with regard to age and sex to patients who underwent PFA. Differences were compared using analysis of variance, t tests, and chi-square tests.
Results:
A total of 202 patients were eligible. After matching, the final cohort consisted of 23 PFA patients, 46 UKA patients, and 46 TKA patients. The majority of patients were female (87%), and the mean ± SD age was 56 ± 9.1 years. The UKA group had higher HAAS values than the TKA group pre- and postoperatively (9.9 vs 7.1 [P = .001] and 12.4 vs 9.5 [P < .001], respectively). Patients with UKA had higher rates of return to sports after surgery than those with TKA or PFA (UKA, 80.5%; TKA, 71.7%; PFA, 69.5%; P = 0.08). In addition, the UKA group had the highest satisfaction with this outcome. Improvement between pre- and postoperative scores was similar in all 3 groups.
Conclusion:
Patients who underwent UKA reported better activity scores and return-to-sports rates than patients who had TKA and PFA. No differences were found in improvement after surgery, suggesting that preoperative differences were reflected postoperatively. These findings inform shared decision making and can help to manage patient expectations after surgery.
Keywords: knee, knee replacement, aging athlete, joint replacement in the athlete
Total knee arthroplasty (TKA) is an effective method for treating osteoarthritis and patellofemoral arthritis in cases where more conservative options have failed.10,19,25,29 Unicompartmental knee arthroplasty (UKA) is less invasive and offers better postoperative outcomes such as faster recovery time, improved range of motion, greater pain relief, and earlier return to sports than TKA.11,15,18,30 Patellofemoral arthroplasty (PFA) is usually performed in younger female patients, preserves the tibiofemoral articulation, and allows for faster recovery than TKA.3,12,14,21,22 An increasingly important outcome to patients is the ability to return to their prior level of sports. With greater sports participation extending to older ages, the ability to return to prior activity levels after knee arthroplasty surgery is less well-documented, and direct comparisons among the 3 surgeries on this outcome are lacking. Because patient satisfaction is usually dependent on the expectations patients have regarding postoperative outcomes, it is important for surgeons to provide detailed information about what a patient can expect for a given surgery to ensure greater satisfaction.17,28
A number of studies have reported a high rate of return to sports after all 3 surgeries. Overall return to sports was higher after UKA than TKA and varied widely: from 36% to 89% after TKA and from 75% to 100% after UKA.1,4,6,13,27,31 In a meta-analysis, Witjes et al30 found that patients who underwent TKA returned to low- to moderate-intensity activities, whereas patients who underwent UKA could return to moderate- to high-intensity activities. A paucity of research is available regarding return to sports after PFA. Shubin Stein et al21 found that 72.2% of patients were able to return to some level of activity, and >52% returned to the same level or higher. Kamikovski et al,7 comparing patients who underwent TKA and PFA, found no difference in Tegner and University of California, Los Angeles (UCLA) scores between the 2 patient groups at 1 to 2 years of follow-up. No studies have directly compared PFA against TKA or UKA on return-to-sports outcomes in a comparable population.
The goals of this study were to compare return to sports as well as preoperative and postoperative activity levels at 1 to 2 years after UKA, TKA, and PFA. To account for the differences in patient characteristics, we matched patients on age and sex. We hypothesized that although the overall return to sports would be high, patients who underwent TKA would have a lower rate of return than patients who underwent UKA and PFA due to the invasiveness of TKA compared with UKA and PFA and changes in proprioception.
Methods
This study was approved by the institutional review board.
Patient Selection and Survey Design
A retrospective review of medical records was performed to identify patients who underwent PFA, TKA, or UKA performed by 2 of the study investigators (A.P. and S.S.). Patients were included if they were older than 18 years of age, had a minimum of 1-year and a maximum of 2-year follow-up, and understood the English language. All patients were given a standardized postoperative rehabilitation program and cleared for sporting activities.
Data Collection
A return-to-sports questionnaire was derived by the authors based on prior studies on arthroplasty patients.5,9,20,27,29 The survey consisted of questions regarding pre- and postoperative activity levels, type of sports, and patient-reported outcomes. Surveys regarding preoperative sporting activities asked patients to recall sports levels within 5 years before their procedures rather than immediately preoperatively. Based on the categorizations described by Vail et al26 and Kuster et al,9 individual sports were divided into 3 categories by impact on the knee: low (ie, swimming, walking, bicycling), medium (ie, downhill skiing, doubles tennis, hiking), and high (ie, soccer, basketball, baseball). Patients who did not indicate that they participated in sports preoperatively were not included in the final analysis. Return to sports satisfaction was graded using a 5-level Likert score. Subjective postoperative level of activity was scored as lower, similar, or higher relative to the preoperative activity level. Multiple patient-reported outcomes were collected: UCLA activity score,25,27,30 High Activity Arthroplasty Score (HAAS), and numeric rating scale (NRS) for pain.24 If a patient underwent bilateral surgery, data from the most recent surgery were used for the analysis.
Statistical Analysis
All statistical analyses were completed in RStudio. Patients who underwent TKA and UKA were matched to patients who underwent PFA on a 2:1 ratio based on age and sex. Matching on age was performed with the following age categories: ≤55, 56-60, 61-65, and >65 years. To compare the 3 patient populations on descriptive data and return to sports, chi-square tests and analysis of variance (ANOVA) were performed for categorical and continuous data, respectively. Pre- and postoperative UCLA, HAAS, NRS, and number of sports for each impact level were compared using a t test. Overall differences between the 3 surgeries on each of the outcomes were tested using 1-way ANOVA. If the ANOVA test produced a significant value P < .05, a post hoc pairwise comparison was performed using a Tukey multiple comparisons adjustment for continuous variables. All tests were 2-tailed and conducted using a significance level of P < .05.
Results
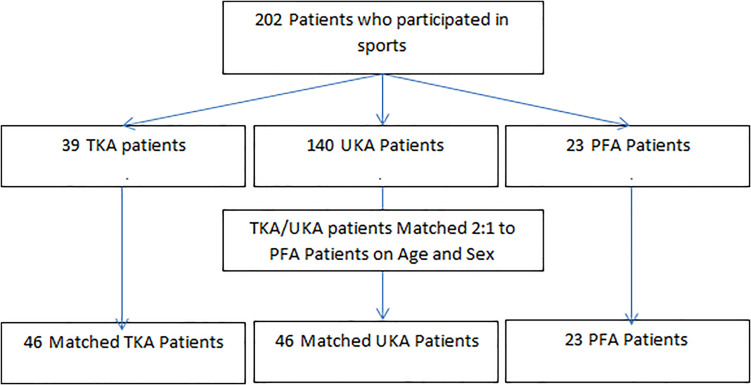
Of the 367 patients who were sent the survey, 114 (31.1%) did not complete the survey, and 51 (13.9%) indicated they did not play a sport preoperatively. Among the 202 patients included in the study, 23 (11.4%) underwent PFA, 39 (19.3%) TKA, and 140 (69.3%) UKA (Figure 1). Patients in the TKA and UKA groups were matched 2:1 to the 23 PFA patients, resulting in 46 (19 unique) TKA patients and 46 (36 unique) UKA patients. Some TKA and UKA patients were matched to >1 PFA patient, resulting in nonunique matches. Descriptive data on the matched population and other preoperative information can be found in Table 1. The matched patient population was 87% female, the mean age was 56 ± 9.1 years, and the mean body mass index was 28 ± 5.6 kg/m2. Among the UKA patients, 29 (63%) had a medial UKA and 17 (37%) had a lateral UKA. A total of 38 patients (UKA 15, TKA 14, PFA 9; P = .767) had prior surgery on the index knee. No differences were found in the UCLA score, body mass index, and surgery side at baseline. Patients in the UKA group were found to have higher preoperative HAAS values than those in the TKA group (9.9 vs 7.1; P = .001). Although the HAAS for the PFA group was 2 points less than that for the UKA group, this difference did not reach statistical significance (7.9 vs 9.9; P = .08). Patients in the PFA group were less active preoperatively, having played fewer low-impact (UKA 3.1 vs 1.7, P = .003; TKA 3.3 vs 1.7, P = .008) and medium-impact (UKA 1.5 vs 0.7, P = .008; TKA 1.4 vs 0.7, P = .02) sports than TKA and UKA groups.
Figure 1.
Flowchart for patient inclusion and matching. PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Table 1.
Preoperative Characteristics for Total Sample and UKA, TKA, and PFA Groupsa
| Characteristic | Total | UKA | TKA | PFA | P Value |
|---|---|---|---|---|---|
| Number | 115 | 46 | 46 | 23 | |
| Sex | ≥.999 | ||||
| Male | 15 (13.0) | 6 (13.0) | 6 (13.0) | 3 (13.0) | |
| Female | 100 (87) | 40 (87.0) | 40 (87.0) | 20 (87.0) | |
| Surgery side | |||||
| Right | 72 (62.6) | 25 (54.3) | 30 (65.2) | 17 (73.9) | .255 |
| Left | 43 (37.4) | 21 (45.7) | 16 (34.8) | 6 (26.1) | |
| Medial or lateral | |||||
| Medial | — | 29 (63.0) | — | — | .105 |
| Lateral | — | 17 (37.0) | — | — | |
| Age category | |||||
| ≤55 y | 55 (47.8) | 22 (47.8) | 22 (47.8) | 11 (47.8) | ≥.999 |
| 56-60 y | 25 (21.7) | 10 (21.7) | 10 (21.7) | 5 (21.7) | |
| 61-65 y | 15 (13.0) | 6 (13.0) | 6 (13.0) | 3 (13.0) | |
| >65 y | 20 (17.5) | 8 (17.5) | 8 (17.5) | 4 (17.4) | |
| Prior surgery | 38 (33.0) | 15 (32.6) | 14 (30.4) | 9 (39.1) | .767 |
| Body mass index | 27.9 ± 5.6 | 27.11 ± 4.8 | 28.1 ± 5.9 | 29.2 ± 6.3 | .392 |
| No. of impact sports | |||||
| Low impact | 2.89 ± 1.8 | 3.09 ± 2.1 | 3.26 ± 1.3 | 1.74 ± 1.5 | .002 |
| Medium impact | 1.31 ± 1.1 | 1.52 ± 1.2 | 1.41 ± 1.0 | 0.69 ± 0.8 | .007 |
| High impact | 0.58 ± 0.9 | 0.7 ± 1.1 | 0.48 ± 0.7 | 0.56 ± 0.9 | .519 |
| UCLA | |||||
| Continuous score | 5.45 ± 2.4 | 5.93 ± 2.5 | 5.26 ± 2.4 | 4.87 ± 2.1 | .177 |
| Score ≥7 | 38 (33.0) | 15 (32.6) | 18 (39.2) | 5 (21.7) | .350 |
| Score <7 | 77 (67.0) | 31 (67.4) | 28 (61.8) | 18 (78.3) | |
| HAAS total | 8.4 ± 3.8 | 9.91 ± 3.8 | 7.13 ± 3.4 | 7.9 ± 3.68 | .001 |
| NRS | 65.3 ± 19.0 | 69.4 ± 17.1 | 60.1 ± 20.4 | 66.59 ± 18.6 | .072 |
aValues are expressed as n (%) or mean ± SD. —, not applicable. HAAS, High Activity Arthroplasty Score; NRS, Numeric Rating Scale for pain; PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; UCLA, University of California, Los Angeles activity score; UKA, unicompartmental knee arthroplasty.
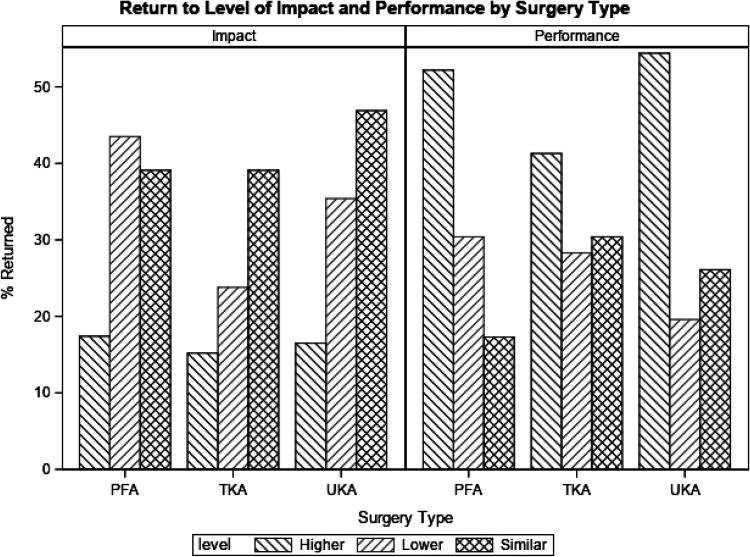
Postoperative results are reported in Table 2. The majority of patients returned to sports at the same or higher level of impact after all 3 surgeries, with 35 patients (76.2%) returning after UKA, 25 (54.3%) after TKA, and 13 (56.5%) after PFA. The proportion of patients who self-reported returning to similar or higher levels of performance was significantly higher after UKA (80.5%) than TKA (71.7%) and PFA (69.5%) (P = .008). Return to levels of impact and performance are shown in Figure 2. In general, patients in the PFA group played fewer sports after surgery than those in the UKA or TKA groups. However, this difference was significant for only medium-impact sports (UKA 1.07, TKA 1.00, and PFA 0.48; P = .04). Postoperative satisfaction with return to sports was significantly higher in the UKA group (86.9% satisfied) than in the PFA (65.2% satisfied) and TKA (67.4% satisfied) groups (P = .048). No patients received subsequent surgery in any of the 3 groups. No significant differences were seen between groups on the postoperative UCLA score or NRS pain score. Similar to the preoperative data, postoperative HAAS values were higher in the UKA group than TKA group (12.4 vs 9.5, respectively; P < .001). No significant difference was found between PFA and TKA (11.0 vs 9.5, respectively; P = .259) or PFA and UKA (11.0 vs 12.4, respectively; P = .210). The results of post hoc pairwise comparison tests can be found in Table 3.
Table 2.
Postoperative Characteristics for Total Sample and UKA, TKA, and PFA Groupsa
| Total | UKA | TKA | PFA | P Value | |
|---|---|---|---|---|---|
| Return to level of impact | |||||
| Lower | 42 (36.5) | 11 (23.8) | 21 (45.7) | 10 (43.5) | .229 |
| Similar | 54 (46.9) | 27 (58.7) | 18 (39.1) | 9 (39.1) | |
| Higher | 19 (16.5) | 8 (17.4) | 7 (15.2) | 4 (17.4) | |
| Return to level of performance | |||||
| Lower | 29 (25.2) | 9 (19.6) | 13 (28.3) | 7 (30.4) | .008 |
| Similar | 30 (26.1) | 12 (26.1) | 14 (30.4) | 4 (17.3) | |
| Higher | 56 (48.7) | 25 (54.4) | 19 (41.3) | 12 (52.2) | |
| No. of impact sports | |||||
| Low impact | 2.61 ± 1.8 | 2.82 ± 2.0 | 2.61 ± 1.6 | 1.91 ± 1.6 | .14 |
| Medium impact | 0.99 ± 0.9 | 1.07 ± 1.0 | 1.00 ± 0.9 | 0.48 ± 0.7 | .04 |
| High impact | 0.36 ± 0.7 | 0.48 ± 0.7 | 0.33 ± 0.7 | 0.17 ± 0.5 | .18 |
| Satisfaction | |||||
| (Very) dissatisfied/neutral | 29 (25.2) | 6 (13.1) | 15 (32.6) | 8 (35.8) | .048 |
| (Very) satisfied | 86 (74.8) | 40 (86.9) | 31 (67.4) | 15 (65.2) | |
| UCLA | |||||
| Continuous score | 6.71 ± 2.0 | 6.89 ± 2.0 | 6.62 ± 1.9 | 6.52 ± 2.4 | .736 |
| Score unknown | 2 (1.7) | 1 (2.2) | 1 (2.2) | 0 (0) | |
| Score ≥7 | 68 (59.1) | 25 (54.3) | 28 (60.8) | 15 (65.2) | .696 |
| Score <7 | 45 (39.1) | 20 (43.4) | 17 (37.0) | 8 (34.8) | |
| HAAS total | 10.94 ± 3.6 | 12.36 ± 3.8 | 9.54 ± 3.4 | 11.00 ± 3.7 | .001 |
| NRS | 15.15 ± 15.42 | 13.76 ± 15.3 | 13.79 ± 11.2 | 20.17 ± 21.1 | .144 |
aValues are expressed as n (%) or mean ± SD. HAAS, High Activity Arthroplasty Score; NRS, Numeric Rating Scale for pain; PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; UCLA, University of California Los Angeles activity score; UKA, unicompartmental knee arthroplasty.
Figure 2.
Return to level of impact and performance by injury type. PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Table 3.
Post Hoc Pairwise Comparison Tests With Tukey Adjustmenta
| Measure | Comparison | Difference | 95% CI | P Value |
|---|---|---|---|---|
| Preoperative | ||||
| No. of low-impact sports | UKA-TKA | –0.17 | –1.03 to 0.69 | .881 |
| TKA-PFA | 1.52 | 0.46 to 2.58 | .003 | |
| UKA-PFA | 1.34 | 0.29 to 2.41 | .008 | |
| No. of medium-impact sports | UKA-TKA | 0.11 | –0.40 to 0.62 | .869 |
| TKA-PFA | 0.72 | 0.09 to 1.35 | .021 | |
| UKA-PFA | 0.83 | 0.20 to 1.45 | .008 | |
| HAAS | UKA-TKA | 2.78 | 1.00 to 4.57 | .001 |
| TKA-PFA | –0.56 | –1.29 to 0.15 | .470 | |
| UKA-PFA | 2.00 | –0.18 to 4.18 | .080 | |
| Postoperative | ||||
| No. of medium-impact sports | UKA-TKA | 0.07 | –0.39 to 0.52 | .938 |
| TKA-PFA | 0.52 | –0.04 to 1.08 | .072 | |
| UKA-PFA | 0.59 | 0.03 to 1.14 | .036 | |
| HAAS | UKA-TKA | 2.92 | 1.14 to 4.50 | <.001 |
| TKA-PFA | –1.45 | –3.49 to 0.56 | .210 | |
| UKA-PFA | 1.36 | –0.69 to 3.41 | .259 | |
aHAAS, High Activity Arthroplasty Score; PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Improvement on the outcomes of interest between the pre- and postoperative time points is displayed in Table 4. Generally, patients played significantly fewer sports than they had within the 5 years preoperatively regardless of the procedure. However, a significant improvement was seen in activity scores (HAAS and UCLA) as well as pain scores (NRS) for all 3 groups. No difference was detected in the magnitude of improvement among the 3 groups on either number of sports played or the patient-reported outcome scores.
Table 4.
Improvement on Return to Sports and Patient-Reported Outcome Measures Between Post- and Preoperative Assessmentsa
| UKA (Post-Pre) | TKA (Post-Pre) | PFA (Post-Pre) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | Estimate | 95% CI | P Value | Between-Group P Value |
| No. of Impact Sports | ||||||||||
| Low impact | –0.26 | –0.89 to 0.37 | .41 | –0.65 | –1.10 to –0.20 | .006 | 0.17 | –0.25 to 0.60 | .4 | .164 |
| Medium impact | –0.46 | –0.78 to –0.13 | .006 | –0.41 | –0.63 to 0.20 | <.001 | –0.22 | –0.65 to 0.21 | .31 | .596 |
| High impact | –0.22 | –0.61 to 0.08 | .14 | –0.15 | –0.37 to 0.18 | .368 | –0.39 | –0.86 to 0.07 | .095 | .679 |
| UCLA | 0.96 | 0.23 to 1.68 | .01 | 1.33 | 0.25 to 2.41 | .017 | 1.65 | –0.725 to 2.58 | .001 | .626 |
| HAAS | 2.5 | 1.26 to 3.74 | <.001 | 2.41 | 1.20 to 3.63 | <.001 | 3.09 | 1.37 to 4.80 | <.001 | .81 |
| NRS | –56 | –62.67 to –49.33 | <.001 | –47.82 | –54.55 to –41.08 | <.001 | –46.14 | –56.16 to 36.11 | <.001 | .126 |
aHAAS, High Activity Arthroplasty Score; NRS, Numeric Rating Scale for pain; PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; UCLA, University of California, Los Angeles activity score; UKA, unicompartmental knee arthroplasty.
A post hoc power analysis was performed on the postoperative HAAS and UCLA scores. Using the HAAS and UCLA means and standard deviations in each group in Table 2, a power of 0.99 and 0.18 was reached to detect a difference between group HAAS and UCLA scores, respectively. This suggests that our study had power to detect a difference in HAAS values but not UCLA.
Discussion
This study entailed head-to-head comparisons of patients who had undergone UKA, TKA, and PFA and for whom we assessed return to sports, activity scores, and satisfaction while controlling for age and sex. Preoperatively, patients who underwent PFA participated in fewer low- and medium-impact sports and reported lower UCLA scores than patients who underwent UKA and TKA. Furthermore, the UKA group had higher HAAS values than the PFA and TKA groups preoperatively. These differences carry over to postoperative outcomes. The UKA group had a higher rate of return to previous levels of performance and satisfaction and reported higher HAAS values than the TKA and PFA groups. PFA patients played fewer medium-impact sports postoperatively than TKA patients. In addition, no difference was detected in the pre- and postoperative improvement among the 3 procedures, further suggesting that initial differences in patient population were reflected in postoperative outcomes.
To date, no study has directly compared the sports-related outcomes of these 3 surgeries on a matched population. In a meta-analysis, Witjes et al30 found that the UKA group had higher postoperative activity levels and returned to a greater number of sports compared with the TKA group. These results are reflected in the higher postoperative HAAS values and rates of return to sports in the UKA group of our study. Some studies have compared PFA and TKA patients, but they focused on only clinical outcomes and implant survivorship.2,3,7 A few studies, however, investigated the difference in UCLA scores between PFA and TKA. Kamikovski et al7 found no difference in UCLA scores between PFA and TKA patients. In contrast, Dahm et al2 noted a significantly higher UCLA score after PFA than TKA, although that study did not match the groups on patient characteristics. The only study on PFA and return to sports did not compare PFA against another procedure. Shubin Stein et al21 found that the majority of PFA patients returned to play at a similar level, which is also reflected in our study, but we found a higher rate of return.
A major strength of our study is that we controlled for potential confounding by matching on age and sex. In the meta-analysis performed by Witjes et al,30 15 (83%) of the 18 included studies were subject to bias due to lack of adjustment for patient-related factors and preoperative sports level. It should be noted that our preoperative activities surveys queried patients about their sporting activities within 5 years before the procedure rather than immediately preoperatively. As such, many patients presumably reported on their prearthritic activity level and compared this with their postoperative sporting level. Indeed, if we had asked about patients’ activity over a shorter preoperative timeframe (such as 6 months preoperatively), it is likely that their preoperative activity levels would have been lower, and improvement after arthroplasty would have been more impressive.30 Thus, the rates of return to sports that we have reported are not overestimates of the true return rates. Earlier studies performed on PFA patients focused on clinical and functional outcomes. In contrast, the current study concentrated on activity scores and return to sports, because these outcomes are more relevant to patients as they increasingly engage in active lifestyles at older ages. The UCLA score has been the most commonly used scale to measure physical activity. The HAAS, in contrast, is newer and was designed to replace conventional scales that were validated in older populations and that focused on activities of daily living instead of high levels of physical activity.23
One concern with returning to a high level of activity after knee arthroplasty is the potential increase in risk of revision for UKA due to implant wear and tear. This is a valid concern, but in a systematic review of studies on patients who underwent UKA and TKA, Kleeblad et al8 found that implants in younger patients (<55 years) had a low revision rate (adjusted risk ratio TKA vs UKA, 0.52), which corresponds to high 10-year survivorship (UKA 90% vs TKA 94.7%). This survivorship rate was comparable with the rate found in the general population (≥65 years).16 These patients were young and had high postoperative activity levels, suggesting that even after arthroplasty, patients can return to high levels of activity without increased risk of revision or complication.8 Moreover, increased activity can lead to other health benefits such as increased cardiovascular health and fitness. Surgeons may have to weigh the health benefits of returning to high activity against increased risk of revision when deciding which surgery to perform.
This study also has multiple limitations. The study setting is a high-volume tertiary referral hospital, so our findings may not be generalizable to institutions where UKA and PFA are not as frequently performed. The study team was not able to collect data on socioeconomic status, which may affect the outcome. In addition, only patients from 2 orthopaedic surgeons were included. Because the data collection was retrospective, there is always a concern that patients were lost to follow-up or had poor recall. This study was not randomized. Patients who had higher activity levels may have been recommended UKA more often than TKA and PFA, resulting in selection bias. The study followed patients for only 1 to 2 years postsurgically, and patient activity levels may change beyond this period. Our study may have been underpowered to detect significant differences due to the low number of PFA patients in our sample. In addition, the PFA patient population was overwhelmingly female (87%), which resulted in fewer unique TKA patients being matched. However, this sex imbalance is standard for PFA patients and resulted from matching on PFA. For example, Shubin Stein et al21 reported that in their PFA population, 84% of patients were female. As a result, our population may be less generalizable to the overall population undergoing knee-replacement procedures. It may have been beneficial to match patients on preoperative activity levels due to the possible selection bias when selecting patients for a surgery. However, due to our smaller sample size, we were concerned that matching on a third variable would result in fewer unique matches.
Conclusion
High rates of return to sports were achieved regardless of the procedure. Patients who underwent UKA and TKA had higher baseline activity scores than patients who underwent PFA, which were reflected in postoperative outcomes. We found no difference in improvements after surgery among the 3 groups. This finding suggests that preoperative patient characteristics may be more prognostic of postoperative outcomes than surgery type. Our findings may help surgeons better inform their patients on the ability to return to sports after knee replacement as well as better manage expectations.
Footnotes
Final revision submitted April 13, 2020; accepted April 27, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.S. has received research support from Fidia Pharma, consulting fees from DePuy/Medical Device Business Systems and Pfizer, honoraria from Vericel, and hospitality payments from Stryker; her spouse has received research support from Fidia Pharma, JRF Ortho, and NuTech/Organogenesis; consulting fees from Flexion, JRF Ortho, Moximed, NuTech/Organogenesis, Smith & Nephew, and Vericel; and royalties from NuTech/Organogenesis; and is a board member for Aesculap Biologics. A.P. has received educational support from Arthrex; consulting fees from Exactech, Smith & Nephew, Stryker, and Zimmer Biomet; nonconsulting fees from Arthrex and Smith & Nephew; and royalties from Zimmer Biomet; and he has ownership interests in Engage Surgical, Knee Guardian, PerfectFit, and Therma1. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital for Special Surgery (study No. 2017-0316-CR2).
References
- 1. Argenson J, Parratte S, Ashour A, Komistek RD, Scuderi GR. Patient-reported outcome correlates with knee function after a single-design mobile-bearing TKA. Clin Orthop Relat Res. 2008;466(11):2669–2676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dahm DL, Al-Rayashi W, Dajani K, Shah JP, Levy BA, Stuart MJ. Patellofemoral arthroplasty versus total knee arthroplasty in patients with isolated patellofemoral osteoarthritis. Am J Orthop. 2010;39(10):487–491. [PubMed] [Google Scholar]
- 3. Dy CJ, Franco N, Ma Y, Mazumdar M, McCarthy MM, Gonzalez Della Valle A. Complications after patello-femoral versus total knee replacement in the treatment of isolated patello-femoral osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2174–2190. [DOI] [PubMed] [Google Scholar]
- 4. Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG. Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee. 2006;13(4):296–300. [DOI] [PubMed] [Google Scholar]
- 5. Garcia GH, Taylor SA, DePalma BJ, et al. Patient activity levels after reverse total shoulder arthroplasty: what are patients doing? Am J Sports Med. 2015;43(11):2816–2821. [DOI] [PubMed] [Google Scholar]
- 6. Huch K, Müller KAC, Stürmer T, Brenner H, Puhl W, Günther K-P. Sports activities 5 years after total knee or hip arthroplasty: the Ulm osteoarthritis study. Ann Rheum Dis. 2005;64(12):1715–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kamikovski I, Dobransky J, Dervin GF. The clinical outcome of patellofemoral arthroplasty vs total knee arthroplasty in patients younger than 55 years. J Arthroplasty. 2019;34(12):2914–2917. [DOI] [PubMed] [Google Scholar]
- 8. Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD. Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1811–1822. [DOI] [PubMed] [Google Scholar]
- 9. Kuster MS, Spalinger E, Blanksby BA, Gächter A. Endurance sports after total knee replacement: a biomechanical investigation. Med Sci Sports Exerc. 2000;32(4):721–724. [DOI] [PubMed] [Google Scholar]
- 10. Laskin RS, van Steijn M. Total knee replacement for patients with patellofemoral arthritis. Clin Orthop Relat Res. 1999;367:89–95. [PubMed] [Google Scholar]
- 11. Laurencin CT, Zelicof SB, Scott RD, Ewald FC. Unicompartmental versus total knee arthroplasty in the same patient: a comparative study. Clin Orthop Relat Res. 1991;273:151–156. [PubMed] [Google Scholar]
- 12. Leadbetter WB, Seyler TM, Ragland PS, Mont MA. Indications, contraindications, and pitfalls of patellofemoral arthroplasty. J Bone Joint Surg Am. 2006;88(suppl 4):122–137. [DOI] [PubMed] [Google Scholar]
- 13. Lefevre N, Rousseau D, Bohu Y, Klouche S, Herman S. Return to judo after joint replacement. Knee Surg Sports Traumatol Arthrosc. 2013;21(12):2889–2894. [DOI] [PubMed] [Google Scholar]
- 14. Lonner JH. Patellofemoral arthroplasty: an evolving science. Instr Course Lect. 2017;66:211–221. [PubMed] [Google Scholar]
- 15. Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012;470(1):84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Niinimäki T, Eskelinen A, Mäkelä K, Ohtonen P, Puhto AP, Remes V. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res. 2014;472(5):1496–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. [DOI] [PubMed] [Google Scholar]
- 18. Noticewala MS, Geller JA, Lee JH, Macaulay W. Unicompartmental knee arthroplasty relieves pain and improves function more than total knee arthroplasty. J Arthroplasty. 2012;27(8)(suppl):99–105. [DOI] [PubMed] [Google Scholar]
- 19. Parvizi J, Stuart MJ, Pagnano MW, Hanssen AD. Total knee arthroplasty in patients with isolated patellofemoral arthritis. Clin Orthop Relat Res. 2001;392:147–152. [DOI] [PubMed] [Google Scholar]
- 20. Pietschmann MF, Wohlleb L, Weber P, et al. Sports activities after medial unicompartmental knee arthroplasty Oxford III—what can we expect? Int Orthop. 2013;37(1):31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shubin Stein BE, Brady JM, Grawe B, et al. Return to activities after patellofemoral arthroplasty. Am J Orthop. 2017;46(6):e353–e357. [PubMed] [Google Scholar]
- 22. Sisto DJ, Sarin VK. Custom patellofemoral arthroplasty of the knee: surgical technique. J Bone Joint Surg Am. 2007;89(suppl 2, pt 2):214–225. [DOI] [PubMed] [Google Scholar]
- 23. Talbot S, Hooper G, Stokes A, Zordan R. Use of a new high-activity arthroplasty score to assess function of young patients with total hip or knee arthroplasty. J Arthroplasty. 2010;25(2):268–273. [DOI] [PubMed] [Google Scholar]
- 24. Terwee CB, Bouwmeester W, van Elsland SL, de Vet HCW, Dekker J. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis Cartilage. 2011;19(6):620–633. [DOI] [PubMed] [Google Scholar]
- 25. Thompson NW, Ruiz AL, Breslin E, Beverland DE. Total knee arthroplasty without patellar resurfacing in isolated patellofemoral osteoarthritis. J Arthroplasty. 2001;16(5):607–612. [DOI] [PubMed] [Google Scholar]
- 26. Vail TP, Mallon W, Liebelt R. Athletic activities after joint arthroplasty. Sports Med Arthrosc Rev. 1996;4(3):298. [Google Scholar]
- 27. Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR. Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3281–3287. [DOI] [PubMed] [Google Scholar]
- 28. Weiss JM, Noble PC, Conditt MA, et al. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;404:172–188. [DOI] [PubMed] [Google Scholar]
- 29. Williams DH, Greidanus NV, Masri BA, Duncan CP, Garbuz DS. Predictors of participation in sports after hip and knee arthroplasty. Clin Orthop Relat Res. 2012;470(2):555–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Witjes S, Gouttebarge V, Kuijer PPFM, et al. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46(2):269–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90(7):920–923. [DOI] [PubMed] [Google Scholar]