Abstract
Background: The goal of this study is to biomechanically compare Fowler central slip tenotomy with spiral oblique retinacular ligament (SORL) reconstruction in correcting a chronic mallet deformity as part of a swan-neck deformity. Methods: We used 24 human cadaver fingers from 6 hands. Mallet finger and swan-neck deformities were created; then, Fowler tenotomy was done on one group including 3 hands with 12 fingers, and SORL reconstruction was done on the others. Results: During simulated finger extension, there was no significant difference between the 2 techniques in correcting the distal interphalangeal joint droop; however, Fowler tenotomy resulted in hyperflexion of the proximal interphalangeal (PIP) joint, whereas it remained straight after SORL reconstruction. Conclusions: This study supports the SORL reconstruction in correcting a chronic mallet deformity, especially when there is a concomitant PIP hyperextension deformity, which lowers the risk of reversing the deformity after a Fowler procedure.
Keywords: cadaveric biomechanical study, Fowler central slip tenotomy, spiral oblique retinacular ligament reconstruction, swan-neck deformity
Introduction
Chronic mallet finger deformity does not inherently impair the function, but a swan-neck deformity may be problematic.1 Many different procedures have been described for correcting a chronic mallet deformity (untreated or failed surgery) including tenodermodesis,2 scar placation,3 the excision of the scar and direct attachment to the distal phalanx,4 spiral oblique retinacular ligament (SORL) reconstruction,5 Fowler central slip tenotomy,6 and arthrodesis of the distal interphalangeal (DIP) joint.7
Both central slip tenotomy and SORL reconstruction are described for correcting a chronic mallet deformity with or without a supple swan-neck deformity.5,8,9 Central slip tenotomy creates tension on the distal phalanx via the lateral bands. This procedure is mainly criticized because of a residual extension lag in the proximal interphalangeal (PIP) joint or even reversing the deformity creating PIP extension lag resulting in a boutonnière deformity.9,10 This may occur especially if the triangular ligament between the lateral bands is injured during tenotomy.11
The SORL is theorized to link the DIP and PIP joints. Reconstruction of the SORL can be done with the use of either a tendon graft or harvesting half of a lateral band.5,12
The biomechanical basis of these reconstructions is unclear, and the use of these procedures relies on clinical experience.1,8 The goal of this study is to biomechanically compare Fowler central slip tenotomy with SORL reconstruction using a lateral band in correcting a chronic mallet deformity as part of a swan-neck deformity.
Material and Methods
Specimens
We used 24 fresh frozen human cadaver fingers (6 index, 6 middle, 6 ring, and 6 little fingers) from 6 hands. There were three male and three female cadaver arms with a mean age of 76 (range = 57-94) years. The specimens have been individually thawed a minimum of 24 hours prior to the procedure and testing. No injuries or limitation in range of motion was known or found after inspection of the specimen. After removing the skin, we separated each ray by detaching from the carpometacarpal joint while the extensor and flexor tendons and the intrinsic musculature with tendons were preserved. Becker sutures were placed into each tendon separately.13 This included flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) together, extensor digitorum communis, radial interosseous ligament and lumbrical together, and ulnar interosseous ligament. Saline was used during testing to keep the digits moist. Twelve fingers from 3 hands were used for the Fowler procedure testing, whereas the other 12 fingers from 3 hands were used for the SORL reconstruction testing.
Preparation of Fowler tenotomy specimens
To create a chronic mallet finger deformity in the Fowler group, the terminal band of the extensor mechanism was detached from its insertion at the distal phalanx. To maintain an extension deficit of 45° at the DIP joint, we sutured the detached terminal band to the distal phalanx using transosseous sutures while DIP was held in 45° of flexion to simulate the slack tendon.14
Preparation of SORL reconstruction specimens
In the SORL reconstruction group, we first harvested the medial portion of the radial lateral band. We made 2 longitudinal parallel incisions to separate the radial lateral band at the insertion site on the distal phalanx, and then continued the parallel incisions proximally to the base of the proximal phalanx along the path of the radial lateral band to include half of the lateral band in the graft. The proximal end of the graft was then separated while the distal end was left attached to the distal phalanx insertion.8 After harvesting the graft, the remaining extensor mechanism was detached from the DIP to create a mallet deformity.
Creation of swan-neck deformity
To create a swan-neck deformity in all of the specimens, we cut the oblique retinacular ligament and the transverse retinacular ligament on both sides of the PIP joint without injuring the lateral bands. The palmar capsule and the volar plate of the PIP joint was detached proximally as well as the palmar portion of the collateral ligaments. Releasing all of these structures could consistently create a swan-neck deformity with a mean persistent hyperextension of 26.6° (minimum-maximum = 15°-35°) in the PIP joint.
Fingers were then positioned in a custom jig (Figure 1).15 The jig was built using 2 plastic radiolucent boards mounted on an aluminum profile. At the rear end, we attached 4 pulleys for loading the flexors (FDP and FDS), extensor, and radial and ulnar intrinsic tendons. Fingers were secured with two 1.6-mm Kirschner wires in the metacarpal base and middle area of the shaft through predrilled 2-mm holes in the jig to provide a free motion of the DIP, PIP, and MCP joints. To simulate a controlled physiological extension of the fingers, the extrinsic extensor tendon was loaded with a 500 g weight, each of the intrinsic tendons were loaded with 100 g, and the flexor tendons were loaded with 50 g according to previous articles.14,15 We conducted a complete motion of extension in all of the fingers before and after the operative procedures out of a maximally flexed finger position. We measured DIP, PIP, and MCP joint angles (loss of extension in the DIP joint, the hyperextension of the PIP joint, and extension of the MCP joint) with the goniometer on the fluoroscopic lateral view of the fingers before and after the surgical procedure.
Figure 1.

Customized testing jig with loading of the 4 tendons and the image intensifier for measurements.
Surgical Procedures
1. Fowler central slip tenotomy.
We elevated the entire extensor hood including central slip and the lateral bands proximal to the PIP joint off of the bone. The central slip insertion was exposed inserting at the dorsal-proximal part of the middle phalanx. Taking care not to injure the distal extensor mechanism and the triangle between the lateral bands, we detached the central slip from its insertion while detachment of the extensor mechanism was continued over the middle phalanx up to two-third of the phalangeal length as described by Hiwatari et al.15
2. SORL reconstruction.
The harvested tendon graft was transferred in between the PIP joint and the volar plate from distal ulnar to proximal radial (Figure 2a). It is notable that the original method suggests passing palmar to the flexor tendon sheaths.1,5 This route of the tendon graft passage is supposed to maintain the palmar stability of the PIP joint in a more direct way. In other words, we used a nonstandard route because we thought that this pathway can create a better momentum on the PIP joint, as well as avoiding impingement, adhesion, or hindering the motion of the flexor tendons (Figure 2b). Graft tension is adjusted with both the PIP and the DIP joints in neutral position. The proximal end of the graft was secured to the extensor tendon over the proximal phalanx.
Figure 2.
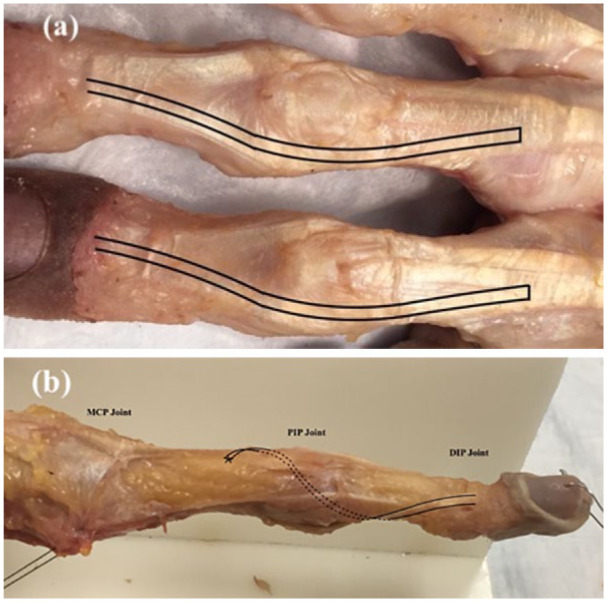
(a) Spiral oblique retinacular ligament (SORL) technique: distally based graft harvesting and (b) SORL technique: graft passage.
Note. MCP = metacarpophalangeal; PIP = proximal interphalangeal; DIP = distal interphalangeal.
Statistical Analysis
A paired Student t test was used to compare the mean angles between the 2 operation groups. Continuous data are presented as mean with SD or 95% confidence interval. Categorical data are presented as frequencies and percentages, and P values were provided. A P value of less than .05 was considered statistically significant.
Results
There was no significant difference between the 2 techniques in correcting the DIP joint droop with both bringing the DIP close to full extension. The SORL reconstruction resulted in an average residual flexion of 2.4° in the DIP joint (95% confidence interval = 6.8° flexion-2.1° extension; minimum-maximum = 20° flexion-5° extension) while an average of 2.1° toward extension of the DIP (95% confidence interval = 5.2° flexion-9.5° extension; minimum-maximum = 15° flexion-26° extension) was achieved after central slip tenotomy (Table 1). Although the difference in correction was significant for the PIP and MCP, the difference was not significant for the DIP. In addition, we performed a post hoc power analysis to detect the achieved power for the DIP. This yielded 50% power using a 2-tailed Wilcoxon-Mann-Whitney test for 12 fingers in each group. Therefore, we could not reject or accept the null hypothesis regarding DIP correction.
Table 1.
The Effect of 2 Techniques on the Finger Joints After Correcting a Chronic Mallet Finger.
| Joint | SORL reconstruction |
Fowler tenotomy |
P value | ||
|---|---|---|---|---|---|
| Final joint position | Degrees, mean, SD | Final joint position | Degrees, mean, SD | ||
| Metacarpophalangeal | Extension | 8.0 (4.9) | Extension | 15 (7.8) | .016 |
| Proximal interphalangeal | Flexion | 8.3 (9.0) | Flexion | 24 (27) | .069 |
| Distal interphalangeal | Flexion | 2.4 (7.0) | Extension | 2.1 (12) | .263 |
Note. SORL = spiral oblique retinacular ligament.
The extension was closer to the anatomic range for both MCP and PIP joints after the SORL reconstruction (Figure 3a-c) (P = .016 for the MCP and P = .069 for the PIP) compared with the fingers treated with Fowler procedure. Although the difference between the mean PIP angles was statistically near significant, the residual deformity was clinically significant (8.3° flexion after SORL reconstruction vs 24° flexion after central slip tenotomy).
Figure 3.
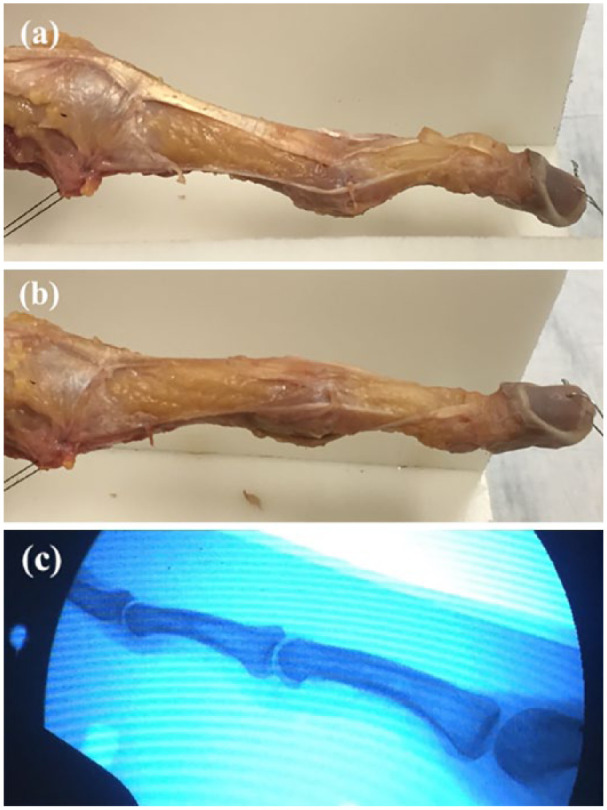
(a) Deformity created before spiral oblique retinacular ligament (SORL) reconstruction, (b) deformity after SORL reconstruction, and (c) deformity after SORL reconstruction under the fluoroscope.
Flexion of the PIP joint was noted after Fowler central slip tenotomy in 7 fingers (range = 25°-77°). Also, central slip tenotomy resulted in hyperextension of the DIP in 2 fingers (15° and 26°), whereas no severe PIP hyperextension occurred after SORL reconstruction. With Fowler central slip tenotomy, severe PIP flexion was correlated with DIP hyperextension (index finger = DIP 15° hyperextension and PIP 58° flexion; ring finger = DIP 26° hyperextension and PIP 77° flexion).
We did not observe any tendon rupture, or other complications rather than hyperflexion of the PIP joint after central slip tenotomy (Figure 4).
Figure 4.
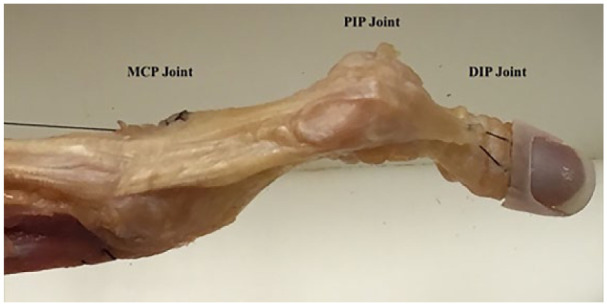
Failed Fowler tenotomy after applying traction.
Note. MCP = metacarpophalangeal; PIP = proximal interphalangeal; DIP = distal interphalangeal.
Discussion
This study compared the techniques of SORL reconstruction with Fowler central slip tenotomy for the correction of chronic mallet deformity with resultant swan-neck deformity. The results suggest that SORL reconstruction may provide more favorable correction of swan-neck deformity compared with Fowler tenotomy.
Limitations should be considered when interpreting the results: (1) There were a limited number of specimens available in this study; (2) we did not have matched pairs in the 2 groups; and (3) the exact forces on each tendon are unknown and variation in these forces can influence the outcome. Moreover, we were not able to assess the deformity with dynamic forces. Accordingly, before choosing the proper weights, we tested various forces and did not find any clinical difference in the form of the joints, and these forces were adapted from prior biomechanical studies.14 Nevertheless, the pathologic changes occurred in the PIP and MCP joints can be attributed to both the “force” and the “force transmission pathway.” The amount of force can vary depending on the type of activity; however, we believe that the transmission pathway is playing a more important role in creating any type of deformity. In addition, the routing of the SORL reconstruction was not standard and does not reflect standard clinical practice.
Both techniques showed comparable results in correcting the DIP joint position. However, our study showed that the central slip tenotomy may result in a reverse deformity after surgery. The reason why hyperextension of the PIP joint occurs only in some patients following a mallet deformity is unknown; however, it is plausible that the triangular ligament and volar plate of the PIP joint have been injured at the time of index trauma. Other possibility in chronic cases is overstretching of the structures over the time resulting in insufficiency of the ligaments and the volar plate. In our cadaver study, we tried to create a swan-neck deformity by making the volar plate insufficient.
A surgery is considered successful when the DIP extension lag is less than 10° while allowing enough flexion of the DIP joint.16 To correct hyperextension of the PIP joint as well as flexion deformity of the DIP joint, there are reports on the spiral oblique ligament reconstruction in that they achieved excellent extension of the DIP joint plus correction of the PIP joint hyperextension.2,17 Nevertheless, there are reports that a mallet deformity can turn to a boutonnière deformity after Fowler central slip tenotomy.18 Grundberg and Reagan9 reported a PIP extensor lag up to 10° in 4 of the 20 patients after Fowler procedure, which improved gradually over an 1-year follow-up.
The clinical relevance and implication of this study is to support the SORL reconstruction in correcting a chronic mallet deformity, especially when there is a concomitant PIP hyperextension deformity, which lowers the risk of reversing the deformity after a Fowler procedure.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the Office of Biological Safety, Harvard Medical School Research. All the cadavers were handled according to the institutional laboratory safety policy and standard operating procedures. This article does not contain any studies with live human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Each author certifies that he or she, or a member of their immediate family, has no commercial associations (ie, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Aslan Baradaran  https://orcid.org/0000-0002-5291-4141
https://orcid.org/0000-0002-5291-4141
References
- 1. Kleinman WB, Petersen DP. Oblique retinacular ligament reconstruction for chronic mallet finger deformity. J Hand Surg. 1984;9(3):399-404. [DOI] [PubMed] [Google Scholar]
- 2. De Boeck H, Jaeken R. Treatment of chronic mallet finger deformity in children by tenodermodesis. J Ped Orthop. 1992;12(3):351-354. [DOI] [PubMed] [Google Scholar]
- 3. Elliott RA., Jr. Injuries to the extensor mechanism of the hand. Orthop Clin North Am. 1970;1(2):335-354. [PubMed] [Google Scholar]
- 4. Ulkur E, Acikel C, Ergun O, et al. Repair of chronic mallet finger deformity using Mitek micro arc bone anchor. Ann Plast Surg. 2005;54(4):393-396. [DOI] [PubMed] [Google Scholar]
- 5. Thompson JS, Littler JW, Upton J. The spiral oblique retinacular ligament (SORL). J Hand Surg. 1978;3(5):482-487. [DOI] [PubMed] [Google Scholar]
- 6. Asghar M, Helm RH. Central slip tenotomy for chronic mallet finger. Surgeon. 2013;11(5):264-266. [DOI] [PubMed] [Google Scholar]
- 7. Pechlaner S, Hussl H, Kerschbaumer F, et al. Operationsatlas Handchirurgie. Stuttgart, Germany: Georg Thieme Verlag; 1997. [Google Scholar]
- 8. Oh JY, Kim JS, Lee DC, et al. Comparative study of spiral oblique retinacular ligament reconstruction techniques using either a lateral band or a tendon graft. Arch Plast Surg. 2013;40(6):773-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Grundberg AB, Reagan DS. Central slip tenotomy for chronic mallet finger deformity. J Hand Surg. 1987;12(4):545-547. [DOI] [PubMed] [Google Scholar]
- 10. Houpt P, Dijkstra R, Storm van Leeuwen JB. Fowler’s tenotomy for mallet deformity. J Hand Surg Br. 1993;18(4):499-500. [DOI] [PubMed] [Google Scholar]
- 11. Jones FE. Fowler’s tenotomy for mallet deformity. J Hand Surg Br. 1994;19(3):405-406. [DOI] [PubMed] [Google Scholar]
- 12. Littler JW. The finger extensor mechanism. Surg Clin North Am. 1967;47(2):415-432. [DOI] [PubMed] [Google Scholar]
- 13. Arora R, Lutz M, Gabl M, et al. [Primary treatment of acute extensor tendon injuries of the hand]. Oper Orthop Traumatol. 2008;20(1):13-24. [DOI] [PubMed] [Google Scholar]
- 14. Chao JD, Sarwahi V, Da Silva YS, et al. Central slip tenotomy for the treatment of chronic mallet finger: an anatomic study. J Hand Surg. 2004;29(2):216-219. [DOI] [PubMed] [Google Scholar]
- 15. Hiwatari R, Kuniyoshi K, Aoki M, et al. Fractional Fowler tenotomy for chronic mallet finger: a cadaveric biomechanical study. J Hand Surg. 2012;37(11):2263-2268. [DOI] [PubMed] [Google Scholar]
- 16. Makhlouf VM, Deek NA. Surgical treatment of chronic mallet finger. Ann Plast Surg. 2011;66(6):670-672. [DOI] [PubMed] [Google Scholar]
- 17. Kardestuncer T, Bae DS, Waters PM. The results of tenodermodesis for severe chronic mallet finger deformity in children. J Ped Orthop. 2008;28(1):81-85. [DOI] [PubMed] [Google Scholar]
- 18. Bowers WH, Hurst LC. Chronic mallet finger: the use of Fowler’s central slip release. J Hand Surg. 1978;3(4):373-376. [DOI] [PubMed] [Google Scholar]


