Abstract
Background: Range of motion (ROM) measurements of the fingers are frequently obtained during hand physical examinations. While traditionally measured by manual goniometry, smartphone photography introduces an alternative method of ROM measurement that also has potential telemedicine applications. The purpose of this study was to evaluate the reliability of smartphone photography measurements as an alternative to traditional goniometry, using the patient with Dupuytren disease as a model. Methods: Patients with a confirmed Dupuytren contracture were prospectively enrolled in this study. Range of motion measurements of the affected joints were obtained prior to any invasive treatments. Two sets of photographs were taken by both a clinical staff member and a nonclinical individual unaffiliated with the study. Both sets of photos were analyzed for degree of contracture via software analysis and compared against traditional goniometer measurements. Results: The study prospectively enrolled 50 consecutive patients with Dupuytren disease, comprising 123 affected joints. The mean contractures of all affected joints as measured by manual goniometry, trained photograph goniometry, and untrained photograph goniometry were 38.5, 35.3, and 35.5, respectively. The mean difference in contracture measurement was 3.2° between manual and trained photograph goniometry and 3.0° between manual and untrained photograph goniometry. There was no statistically significant difference between trained and untrained photo set measurements. Photograph measurements between separate raters demonstrated high consistency (intraclass correlation coefficient = 0.92). Conclusions: Smartphone photography provides contracture measurements equivalent to the accepted error of a finger goniometer (3.2° compared with 5°). The accuracy of smartphone photography in measuring contractures offers potential telemedicine applications for both clinical and research needs.
Keywords: Dupuytren, range of motion, smartphone photography, contracture, telemedicine
Introduction
Range of motion (ROM) measurements are a critical component of the hand surgeon’s physical examination for many diagnoses. Used to establish a quantitative marker for digit function, ROM measurements are used to establish baseline movement, assess clinical improvements, and in some pathologies guide indications for treatment. Thus, it is important that tools used to evaluate ROM be accurate and precise. Multiple methods currently exist for finger ROM measurements, including visual estimation, manual goniometry, photographic goniometry, diagrammatic recordings, goniometric gloves, and radiographic imaging.1-4 Although the accuracy of manual goniometry has been debated,2 this method is thought to have high interrater reliability5 and remains a universal technique used by hand surgeons and hand therapists.
In evaluating any new method of ROM measurement, accuracy is crucial, but the method must also remain easily accessible to patients and clinicians. Recent advances in smartphone photography have introduced a new ubiquitous platform for photo goniometry. With nearly two-thirds of Americans owning a smartphone,6 the cameras on these devices would easily allow patients to remotely send images and videos to physicians for clinical evaluation. Smartphone photography has the potential to facilitate telemedicine, increasing patient access and simplifying long-term follow-up. However, smartphone goniometry has yet to be validated for ROM measurements in the digits.
The purpose of this study was to assess the validity and reliability of smartphone photography measurements for finger ROM. Using the patient with Dupuytren disease as a model, this study compared active finger ROM measurements using smartphone photography with that of manual goniometry and assessed for interrater variability with this new technique.
Materials and Methods
Fifty consecutive patients with a Dupuytren fixed-flexion contracture (FFC) were prospectively recruited for this study. All patients had a palpable cord with an FFC greater than 20° via manual goniometry in at least one joint, and the research protocol was completed in all patients prior to any treatment. Patient age, sex, and date of recruitment were also recorded. The institutional review board of our hospital system approved this study.
ROM Measurements
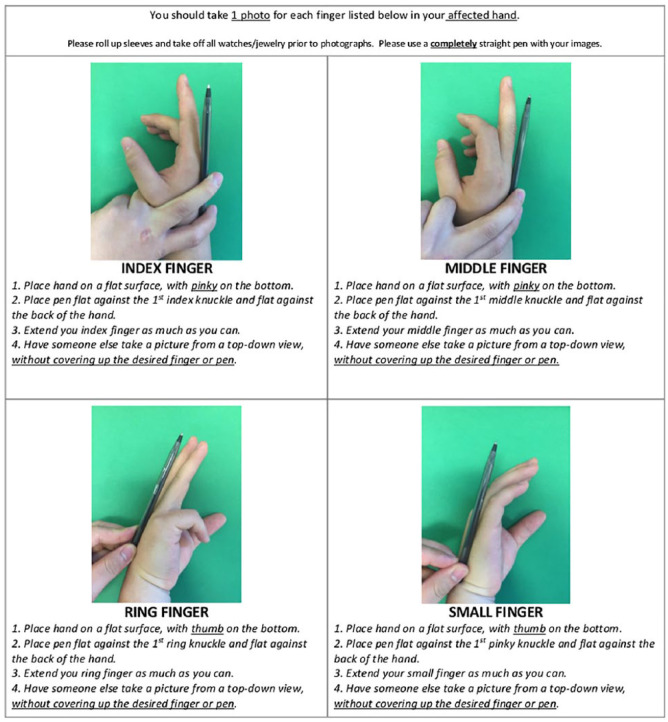
Recruited patients were first provided an instruction handout to review (Figure 1), after which any questions regarding the process were answered by the research investigators. Two series of photographs were subsequently taken: (1) “Trained photos” by research staff; and (2) “Untrained photos” by nonmedically trained individuals unfamiliar with the study, such as patients’ family members (Figure 2). This second photo set served as a proxy for photos captured by patients at home. Chronology was maintained such that patients and operators followed the instruction sheet, rather than mimicking the research staff during their photo set. Photos were obtained of each patient’s contracted digits with positioning as described in the handout. Finally, manual goniometry was performed by a fellowship-trained hand surgeon along the dorsal surface of each affected joint, and measurements were recorded for each affected joint.
Figure 1.
Instruction handout for patients.
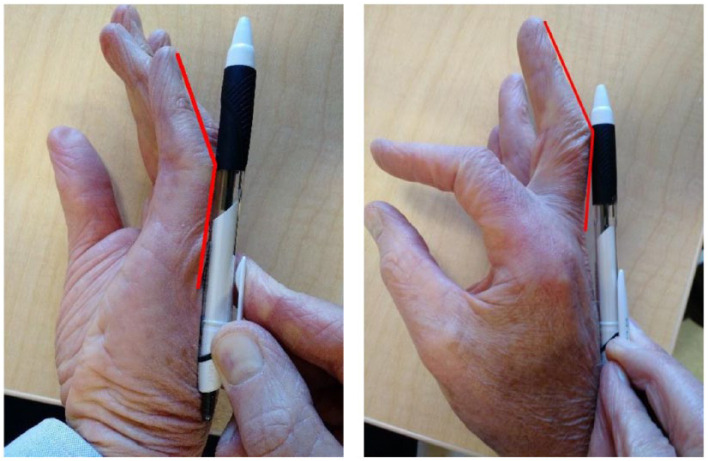
Figure 2.
Sample smartphone photographs.
Two photographs from the same patient depict contractures in the left small finger and the right middle finger.
Images were analyzed for contracture angles with GNU Image Manipulation Program software.7 The program’s measure tool allowed for direct measurement of angles within each image. Angles for each joint contracture were calculated using 3 reference points along the dorsal surface of the finger. For metacarpophalangeal (MP) joint measurements, the 3 reference points were the dorsal surface at the proximal interphalangeal (PIP) joint, the dorsal surface at the MP joint, and a distal point along the flat end of the pen used in each image. For PIP joint measurements, the 3 reference points were the dorsal surfaces at the MP joint, PIP joint, and distal interphalangeal (DIP) joint. For DIP joint measurements, the 3 reference points were the dorsal surface of the PIP joint, the DIP joint, and the distal tip of the finger. When the dorsal surface landmarks were not easily identifiable, the midpoints at each joint between the dorsal and volar surfaces were used instead. All image measurements were performed in a blinded fashion by 2 separate researchers to evaluate for interobserver reliability.
Data Analysis
Power analysis prior to the study was performed for a 2-sample t test for noninferiority, which calculated a sample size of 13 subjects based on a mean difference of 5°, a standard deviation of 10% of the expected measurement, α of 0.05, and a power of 0.80. Five degrees of difference is the accepted standard error in manual goniometry of the hand.8,9 For this study, the authors elected to include a larger sample size (n = 50).
Contracture measurements were calculated from manual goniometry, trained photos, and untrained photos. Paired differences were then calculated for the following groups: manual goniometry and trained photos, manual goniometry and untrained photos, and trained and untrained photos. The mean difference (average of the differences between each pair of contracture measurements) and the mean absolute difference (average of the absolute values of the differences) were then calculated. Comparisons between measurements from each group were done via paired-sample Student t test. Normality was tested via the χ2 test for normality.
Interobserver reliability of smartphone photograph goniometry was tested via intraclass correlation coefficients (ICCs) and Pearson correlation coefficients for both trained and untrained photograph measurements. Using the guidelines developed by Cicchetti and Sparrow,10 an ICC less than 0.40 corresponds to poor clinical reliability, an ICC between 0.4 and 0.59 corresponds to fair clinical reliability, an ICC between 0.60 and 0.74 corresponds to good clinical reliability, and an ICC between 0.75 and 1.00 corresponds to excellent clinical reliability.
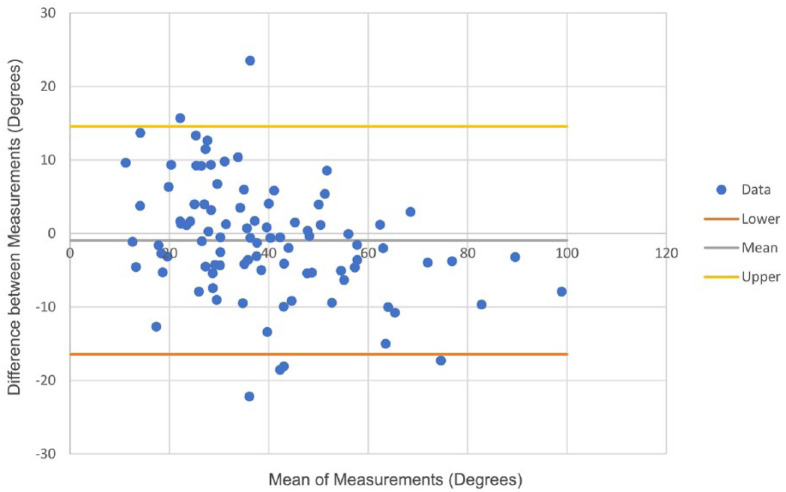
Bland-Altman analysis was also used to determine the agreement between interobserver measurements. This analysis uses the mean and standard deviation of the differences between the 2 measurements for the same joint.11 The limits of agreement were determined as limits = (mean ± 1.96 × standard deviation), conferring a 95% confidence interval.
Results
Contracture Characteristics
This study enrolled 50 consecutive patients with 94 contracted digits. Affected joints included 51 MP, 67 PIP, and 5 DIP joints. The mean patient age was 65 years, and the male to female ratio was 4:1. The mean contractures of all joints were 39°, 35°, and 36° for manual goniometry, trained photograph goniometry, and untrained photograph goniometry, respectively. Although PIP joints demonstrated higher mean contractures, this was not a statistically significant difference. The 95% confidence intervals for MP joints, PIP joints, DIP joints, and all joints combined were not statistically different across the different measurement methods (Table 1). Data for manual goniometry, trained photograph goniometry, and untrained photograph goniometry demonstrated normality (P = .13, P = .13, P = .21, where P < .05 means data are not normally distributed).
Table 1.
Contracture Measurements by Different Methods.
| Measurement method | Mean contracture | 95% confidence interval |
|---|---|---|
| Manual goniometry | 39 | 35-42 |
| MP Joints | 34 | 29-38 |
| PIP Joints | 42 | 38-47 |
| DIP Joints | 35 | 25-46 |
| Trained photograph goniometry | 35 | 32-39 |
| MP joints | 28 | 24-32 |
| PIP joints | 41 | 36-45 |
| DIP joints | 38 | 21-56 |
| Untrained photograph goniometry | 36 | 33-39 |
| MP joints | 31 | 26-35 |
| PIP joints | 40 | 35-44 |
| DIP joints | 37 | 26-48 |
Note. MP = metacarpophalangeal; PIP = proximal interphalangeal; DIP = distal interphalangeal.
Comparing Measurement Methods
There was a mean difference of 3.2° (SD: 10, min: –21, max: 37) between manual goniometry and trained photograph goniometry, and a mean difference of 3.0° (SD: 10, min: –22, max: 36) between manual goniometry and untrained photograph goniometry. The mean absolute difference was 7.9° between manual goniometry and trained photograph goniometry and 8.3° between manual goniometry and untrained photograph goniometry. The mean differences were statistically significant for both manual goniometry versus trained photograph goniometry (paired t test, P = .0005) and manual goniometry versus untrained photograph goniometry (paired t test, P = .002). However, the mean difference of 0.3° (SD: 8) between trained and untrained photograph goniometry was not statistically significant (paired t test, P = .73).
Interobserver Reliability
Both trained and untrained photograph goniometry demonstrated excellent interobserver reliability. Trained photograph goniometry resulted in an ICC of 0.94 and a Pearson correlation coefficient of 0.94. Untrained photograph goniometry resulted in an ICC of 0.89 and a Pearson correlation coefficient of 0.92. When combined, photograph goniometry resulted in an ICC of 0.92 and a Pearson correlation coefficient of 0.93 (Table 2). In terms of difference of degrees between observers, trained photograph goniometry resulted in a mean difference of 0.5° (SD: 6) between the 2 independent observers, and untrained photograph goniometry resulted in a mean difference of 3° (SD: 7). Comparisons used both positive and negative values to demonstrate whether or not one observer consistently measured larger angles compared with the other observer. The Bland-Altman analysis demonstrated that 117 of the 123 measurements were within the 95% confidence interval (Figure 3).
Table 2.
Interobserver Reliability.
| Measurement method | Intraclass correlation coefficient | Pearson correlation coefficient |
|---|---|---|
| Trained photograph goniometry | .94 | .94 |
| Untrained photograph goniometry | .89 | .92 |
| Combined | .92 | .93 |
Figure 3.
Bland-Altman plot.
Of the 123 measurements, 117 lie within the 95% confidence interval limits of agreement.
Discussion
This study demonstrates that smartphone photography provides FFC measurements within the limits of the accepted error of a manual goniometer (3.2° vs 5°).8,9 Because the mean absolute differences were greater than the mean differences, this suggests that smartphone photography does not uniformly overestimate or underestimate contracture angles compared with manual goniometry. While photograph goniometry in the hand has been studied before using dedicated clinical camera equipment with results comparable to manual goniometry,3,12,13 this study is unique in its use of smartphone photography and untrained individuals for finger ROM measurements. Smartphone photography goniometry has demonstrated accurate results in other joints, including the elbow,14,15 knee,16-18 shoulder,19 and spine,20,21 yet its use in the fingers had not been validated prior to this study.
Smith et al specifically studied the use of photograph goniometry in the patient with Dupuytren disease and similarly found a high Pearson correlation coefficient (0.88) compared with manual goniometry and a high ICC (0.92) across different observers for the photograph measurements.3 However, in that study the MP joints were excluded, all photographs were taken by physicians, and photographs were taken using a digital camera rather than a smartphone. Our study overcomes difficulty in visualizing the MP joint contractures by utilizing the straight edge of a pen in each image as a reference guide for angle measurement. In addition, this study compares photographs taken by professionals and those taken by untrained individuals such as patient family members and friends, allowing for a more realistic proxy for photographs obtained in a physically remote setting. Georgeu et al also tested photograph goniometry of the fingers and achieved a 1° difference between photograph goniometry and manual goniometry.13 However, that study utilized a custom-made jig for uniform hand placement, a procedure too cumbersome and impractical for use in a busy clinic or telemedicine setting.
There are several limitations to this study. The study was limited only to one disease process, and the positioning and photography instructions as described in the “Materials and Methods” section may be more difficult and less accurate in scenarios with posttraumatic pain, increased soft tissue swelling, and deformities of the finger along the radioulnar axis. While all of our participants were familiar with the usage of a smartphone, not all actual patients may possess or be familiar with using a smartphone, thus potentially limiting the application of this technique to all patients. Although this study attempted to simulate a home setting without professional supervision, the office environment is still more controlled than the home setting and may not account for differences in photographic backgrounds. Quality and angle from which each photo is taken may vary the measured contracture angles. Although our instruction sheet provides sample photos to mimic the angle of each desired photo, and we showed that untrained photography was not significantly different from trained photography measurements, we would expect that with a larger sample of photos from untrained individuals, the difference in contracture measurements may increase. Finally, as the usage of smartphone photography goniometry enters clinical practice, concerns for Health Insurance Portability and Accountability Act compliance and licensure for telemedicine across state lines may impede the easy adoption of this technique and may require encrypted methods of photograph transfer not typically found with traditional email or text/SMS.
The smartphone is an increasingly pervasive tool that could add value in a hand surgeon’s clinic. Because clinical treatment decisions and follow-up examinations for certain disease processes are based primarily on ROM measurements, the use of smartphone photography goniometry is an attractive method for incorporating telemedicine into a hand surgeon’s practice. Smartphone photography goniometry may also decrease economic costs and increase access to care for both patients and providers.22,23 Specifically in the case of the patient with Dupuytren disease, initial visits and subsequent long-term follow-up without the need for surgical intervention could all be conducted via the remote transfer of a smartphone photograph, thus eliminating patient travel costs, reducing clinic load, and increasing the availability of care. Long-term follow-up of patients could also be more consistent, as the barriers to follow-up are dramatically diminished.
The results of this study demonstrate that smartphone photography goniometry is a reliable and valid method to measure finger ROM. Accuracy and precision are maintained compared with manual goniometry even when photos are taken by patients’ family members or friends, allowing for use in the home setting without professional supervision. Smartphone photography goniometry is suitable for many clinical applications and could be a valuable tool for both clinicians and researchers alike.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Macionis V. Reliability of the standard goniometry and diagrammatic recording of finger joint angles: a comparative study with healthy subjects and non-professional raters. BMC Musculoskelet Disord. 2013;14:17. doi: 10.1186/1471-2474-14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McVeigh KH, Murray PM, Heckman MG, et al. Accuracy and validity of goniometer and visual assessments of angular joint positions of the hand and wrist. J Hand Surg Am. 2016;41:e21-e35. doi: 10.1016/j.jhsa.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 3. Smith RP, Dias JJ, Ullah A, et al. Visual and computer software-aided estimate of Dupuytren’s contractures: correlation with clinical goniometric measurement. Ann R Coll Surg Engl. 2009;91:296-300. doi: 10.1308/003588409X359259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Williams NW, Penrose JM, Caddy CM, et al. A goniometric glove for clinical hand assessment. Construction, calibration and validation. J Hand Surg Br. 2000;25:200-207. doi: 10.1054/jhsb.1999.0360. [DOI] [PubMed] [Google Scholar]
- 5. Ellis B, Bruton A, Goddard JR. Joint angle measurement: a comparative study of the reliability of goniometry and wire tracing for the hand. Clin Rehabil. 1997;11:314-320. doi: 10.1177/026921559701100408. [DOI] [PubMed] [Google Scholar]
- 6. Anderson M. Technology Device Ownership: 2015. Pew Research Center; 2015. http://www.pewinternet.org/2015/10/29/technology-device-ownership-2015. Accessed December 10, 2018.
- 7. GIMP-GNU. Image Manipulation Program. https://www.gimp.org/. Accessed December 10, 2018.
- 8. Boone DC, Azen SP, Lin CM, et al. Reliability of goniometric measurements. Phys Ther. 1978;58(11):1355-1360. http://www.ncbi.nlm.nih.gov/pubmed/704684. Accessed December 10, 2018. [DOI] [PubMed] [Google Scholar]
- 9. Ellis B, Bruton A. A study to compare the reliability of composite finger flexion with goniometry for measurement of range of motion in the hand. Clin Rehabil. 2002;16:562-570. doi: 10.1191/0269215502cr513oa. [DOI] [PubMed] [Google Scholar]
- 10. Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic. 1981;86(2):127-137. http://www.ncbi.nlm.nih.gov/pubmed/7315877. Accessed December 10, 2018. [PubMed] [Google Scholar]
- 11. Martin Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical agreement. Lancet. 1986;1:307-310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 12. Crasto JA, Sayari AJ, Gray RR, et al. Comparative analysis of photograph-based clinical goniometry to standard techniques. Hand. 2015;10:248-253. doi: 10.1007/s11552-014-9702-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Georgeu G, a Mayfield S, Logan a M. Lateral digital photography with computer-aided goniometry versus standard goniometry for recording finger joint angles. J Hand Surg Br. 2002;27:184-186. doi: 10.1054/jhsb.2001.0692. [DOI] [PubMed] [Google Scholar]
- 14. Ferriero G, Sartorio F, Foti C, et al. Reliability of a new application for smartphones (DrGoniometer) for elbow angle measurement. PM R. 2011;3:1153-1154. doi: 10.1016/j.pmrj.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 15. Meislin MA, Wagner ER, Shin AY. A comparison of elbow range of motion measurements: smartphone-based digital photography versus goniometric measurements. J Hand Surg Am. 2016;41:510-515e1. doi: 10.1016/j.jhsa.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 16. Ferriero G, Vercelli S, Sartorio F, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36:146-151. doi: 10.1097/MRR.0b013e32835b8269. [DOI] [PubMed] [Google Scholar]
- 17. Jones A, Sealey R, Crowe M, et al. Concurrent validity and reliability of the Simple Goniometer iPhone app compared with the Universal Goniometer. Physiother Theory Pract. 2014;30:512-516. doi: 10.3109/09593985.2014.900835. [DOI] [PubMed] [Google Scholar]
- 18. Milanese S, Gordon S, Buettner P, et al. Reliability and concurrent validity of knee angle measurement: smart phone app versus universal goniometer used by experienced and novice clinicians. Man Ther. 2014;19:569-574. doi: 10.1016/j.math.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 19. Mitchell K, Gutierrez SB, Sutton S, et al. Reliability and validity of goniometric iPhone applications for the assessment of active shoulder external rotation. Physiother Theory Pract. 2014;30:521-525. doi: 10.3109/09593985.2014.900593. [DOI] [PubMed] [Google Scholar]
- 20. Kolber MJ, Pizzini M, Robinson A, et al. The reliability and concurrent validity of measurements used to quantify lumbar spine mobility: an analysis of an iPhone® application and gravity based inclinometry. Int J Sports Phys Ther. 2013;8(2):129-137. http://www.ncbi.nlm.nih.gov/pubmed/23593551. Accessed December 10, 2018. [PMC free article] [PubMed] [Google Scholar]
- 21. Tousignant-Laflamme Y, Boutin N, Dion AM, et al. Reliability and criterion validity of two applications of the iPhoneTM to measure cervical range of motion in healthy participants. J Neuroeng Rehabil. 2013;10:69. doi: 10.1186/1743-0003-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Asch DA. The hidden economics of telemedicine. Ann Intern Med. 2015;163:801-802. doi: 10.7326/M15-1416. [DOI] [PubMed] [Google Scholar]
- 23. Daniel H, Sulmasy LS, Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: an American college of physicians position paper. Ann Intern Med. 2015;163(10):787-789. doi: 10.7326/M15-0498. [DOI] [PubMed] [Google Scholar]