Abstract
Objective
The Inter Organizational Practice Committee (IOPC) convened a workgroup to develop guidance on models to provide neuropsychological (NP) care during the COVID-19 pandemic while minimizing risks of novel coronavirus transmission as lockdown orders are lifted and ambulatory clinical services resume.
Method
A collaborative panel of experts from major professional organizations developed provisional guidance for models of neuropsychological practice during the pandemic. The stakeholders included the American Academy of Clinical Neuropsychology/American Board of Clinical Neuropsychology, the National Academy of Neuropsychology, Society of Clinical neuropsychology (Division 40) of the American Psychological Association, the American Board of Professional Neuropsychology, and the American Psychological Association Services, Inc.
Results
This guidance reviews the risks and benefits of conducting NP exams in several ways, including standard in-person, mitigated in-person, in-clinic teleneuropsychology (TeleNP), and in-home TeleNP. Strategies are provided for selecting the most appropriate model for a given patient, taking into account four levels of patient risk stratification, level of community risk, and the concept of stepped models of care. Links are provided to governmental agency and professional organization resources as well as an outline and discussion of essential infection mitigation processes based on commonalities across recommendations from diverse federal, state, local, and professional organization recommendations.
Conclusion
This document provides recommendations and guidance with analysis of the risks relative to the benefits of various models of NP care during the COVID-19 pandemic. These recommendations may be revised as circumstances evolve, with updates posted continuously on the IOPC website (https://iopc.online/).
Keywords: Neuropsychological assessment, Teleneuropsychology, Coronavirus, COVID-19, Recommendations, Models of care, In-clinic
Goals of the Models of Care Recommendation and Guidance
Clinical neuropsychologists globally are trying to determine how to provide neuropsychological (NP) services while minimizing risks of the COVID-19 illness and novel coronavirus transmission as lockdown orders are lifted and ambulatory clinical services resume in many settings. To do so rationally requires analysis of the risks relative to the benefits of various models of NP care. An advocacy team was established by the Inter Organizational Practice Committee (IOPC)1 to develop guidance and resources for neuropsychologists navigating practice during the pandemic. Readers are referred to the IOPC Recommendations/Guidance for Teleneuropsychology (TeleNP) in Response to the COVID-19 Pandemic (Bilder et al., 2020), which was developed to provide guidance for TeleNP in the context of the disruption in the usual face-to-face interpersonal contact that characterizes NP assessments. This additional guidance first outlines the benefits of NP assessment, then surveys the risks of conducting NP assessments in the context of the novel coronavirus pandemic, and finally reviews the options for conducting NP exams in several ways, including standard in-person NP exams and several modified NP exam formats including mitigated in-person, in-clinic TeleNP, and in-home TeleNP. Models for informed consent procedures and suggestions for documentation are included.
This material is provided to help readers consider options and risk–benefit ratios of different strategies for NP care during the COVID-19 pandemic. Given wide regional variation in risks of coronavirus infection or transmission, and wide variation in individual patient risk characteristics and practice settings, no uniform guidance or set of recommendations is likely to be appropriate across clinical settings, and “hybrid” or “blended” models may best balance risks and benefits. The guidance is not meant to supplant typical practices and guidelines under normal circumstances. That is, when safe and feasible to resume typical in-person services, the recommendations should not override existing practice standards. No recommendation should be followed if it contradicts federal, state, or local laws overseeing the practice of psychologists. It is assumed that all psychologists will adhere to respective federal and state rules and regulations, the American Psychological Association’s Ethical Standards (APA, 2017), and the Standards for Educational and Psychological Testing (American Educational Research Association et al., 2014).
Benefits of NP Assessment
Emerging literature supports the incremental validity of NP assessment above and beyond other demographic, medical, and diagnostic variables; NP assessment enhances diagnostic decision-making and prediction of outcomes and reduces costs (Braun et al., 2011; Donders, 2020; Watt & Crowe, 2018). These benefits have almost always exceeded risks because the typical risks of NP assessment are so low. Now that the novel coronavirus pandemic has made in-person clinical encounters subject to non-negligible risks (enumerated below), it is valuable to specify the benefits of NP exams so that these can be weighed against potential risks.
Many benefits of NP assessment can be understood as assisting in differential diagnosis or characterization of brain function that affects treatment or other interventions (Braun et al., 2011). A nonexhaustive list of interventions that are often guided by NP exams is as follows:
Surgical (neurosurgical [e.g., epilepsy, tumor, deep brain stimulator]; transplant)
Medical (medication, physical rehabilitation)
Educational, psychoeducational
Psychiatric, psychopharmacological
Cognitive remedial, psychological rehabilitation
Psychotherapeutic, behavioral, coaching
Family-focused therapies
Vocational
Lifestyle
Social
Ecological (housing, independent living)
Decisional (individual: assessment of capacity; disability; driving)
Forensic (political/justice: immigration; asylum seeking; civil litigation; criminal litigation/capital crime)
In addition to direct impacts on interventions, NP exams may provide differential diagnoses and/or characterization of patient functioning that affects patient and/or caregiver understanding. This could be seen as an intervention itself, insofar as increased understanding may change behavior, but it deserves separate consideration in this context. For example, it may be of high importance to a patient and family members to know how likely it is that their loved one has dementia or that their symptoms are better understood as a response to stressors or isolation during the pandemic. By identifying appropriate treatments and increasing understanding, NP assessments also reduce costs, including direct financial costs (through reduction in suboptimal treatment utilization) and other human costs (through productivity loss, treatment of ancillary disorders, caregiver burden, and other indirect impacts).
The benefits of NP assessment need to be determined with respect to time. This weighs particularly on decisions to delay exams considering the benefits of earlier intervention and understanding versus the risks of delayed interventions and understanding. The distinctions between “emergency,” “urgent,” and “elective” procedures are often unclear,2 and it is more accurate to consider “urgency” as a dimension or continuum rather than classify the potential scenarios that can arise for patients given specific syndromes, ages, and other contextual factors.
A patient who has epilepsy surgery delayed because NP information is not available may have adverse consequences of ongoing recurrent seizures during that waiting period.
A patient who has a cardiac or other major organ transplant (e.g., kidney, liver) delayed because NP information is not available may experience severe medical consequences or even death.
A patient with Parkinson’s disease who has a deep brain stimulation surgery delayed because NP information is not available may experience adverse consequences such as a fall and poor adaptive functioning during that waiting period, hindering his/her ability to live independently.
A patient with suspected dementia who is living alone, driving, and/or working may experience adverse consequences of continuing these activities without intervention, potentially endangering self and others.
An immigrant could be denied asylum because NP information is not available, and this could result in deportation and possible lethal consequences on return to their country of origin.
A child with a learning disorder may not receive appropriate instruction, and their educational progress and potential placements may be affected adversely. The risks for adverse impacts of not receiving appropriate educational support and intervention may be magnified in the context of homeschool or hybrid homeschool models prior to full return to school conditions (which may not occur in some areas until a vaccine is widely available).
A child with autism spectrum disorder or attention-deficit/hyperactivity disorder with significant behavioral dysregulation may not receive appropriate interventions such as applied behavior analysis or psychiatric management. As a result, the child’s condition may worsen and require more intensive and costly interventions. The child may no longer be appropriate for school placement, and this could have negative downstream effects for both the child and the family system (e.g., parental stress; job loss).
A patient with a major comorbid mood disorder may not receive an appropriate diagnosis and treatment plan, increasing the risk for suicide.
Risks of In-Person NP Assessment
Health Risks
The primary risks of conducting in-person or in-clinic assessments during the pandemic are health risks, including:
Patient risk of contracting COVID-19
Examiner(s) risk of contracting COVID-19
Risk of transmission of coronavirus to patient, examiner(s), and/or community
Risks of exam validity being undermined by illness anxiety, which may be manifested by both examinees and examiners.
With regard to health risks, it should be noted that for Phase I and Phase II reopening as defined by White House/CDC criteria, “vulnerable persons” (i.e., individuals with serious underlying health conditions, including high blood pressure, chronic lung disease, diabetes, obesity, asthma, and those whose immune system is compromised, such as by chemotherapy for cancer and other conditions requiring such therapy) are instructed to continue to follow “safer-at-home” orders. For more details: https://www. whitehouse.gov/openingamerica/#criteria.
Legal Risks
It should be recognized that the risks are not limited to health risks as noted earlier but also entail legal risks, including (a) exposure to litigation that may arise if an examinee’s or employee’s health is compromised, (b) exposure to litigation if the conclusions of the examination are questioned or considered invalid, and (c) possibility that the clinician’s or practice’s insurance coverage may not include practice under these circumstances (which may interact with other state, county, or city regulations imposed at the time; e.g., if the practice is not considered appropriate under “reopening” guidelines in effect within that jurisdiction). Clinicians are encouraged to discuss their practice reopening plans with their malpractice insurance carrier. Most carriers offer individual consultations for this purpose.
The Trust has developed a statement https://bit.ly/TrustGuidelines(https://bit.ly/TrustGuidelines; Parma Trust Insurance, 2020) on in-person psychological services during the COVID-19 crisis, which is a useful reference and highlights the importance of each psychologist considering, among other factors, all relevant institutional, regional, state, and federal regulations in effect within their jurisdiction in considering risk management strategies.
Models for Conducting NP Assessments
The following models are summarized to help provide options that may be considered by those planning reopening. It is assumed that no single model is best and that each practitioner needs to select elements from different models to maximize benefits and minimize risks.
In-Person Assessments
Standard in-person administration
In-person or “in-clinic” assessment without mitigation procedures is the pre-COVID-19 “gold standard” against which other procedures are compared. These are also generally the conditions under which normative and standardization studies were conducted, so deviation from this may be considered nonstandard administration.
Modified in-person administration (using mitigation procedures to minimize the risk of coronavirus infection and/or transmission)
The risks of in-person assessment are reduced by mitigation strategies (e.g., use of PPE, physical distancing), but some of these strategies may also potentially increase patient anxiety and represent an alteration in standard administration practices and therefore may affect the validity and increase the risk of inaccurate diagnoses. Note that significant deviation from standard assessment procedures affects scores in unknown ways and therefore reduces the reliability of score interpretation (American Educational Research Association et al., 2014). We do not currently have a clear understanding of the point at which a virus mitigation measure becomes a significant departure from standardized administration. There are currently no studies of potential threats to validity in the context of in-person viral mitigation strategies.
See below for a discussion of mitigation procedures. The following is a nonexhaustive list of procedures that are designed to reduce the risk of exposure but differ from standard practice and may affect test performance or interpretation:
Screening procedures to determine that the patient (and the examiner) do not have symptoms or recent exposure, discussion of potential risk as part of an informed consent process, and visible signs of mitigation (e.g., masks, gloves, plexiglass barriers, warning signs) may increase patient anxiety to a degree that interferes with test performance. Lack of physical contact between the patient and office staff or examiners may also have a general anxiety-provoking effect and reduce the level of support patients experience from interpersonal contact. Even if examiner behavior and office practices do not raise anxiety, there is a risk that the examinee may have increased anxiety or other symptoms secondary to health, social, and/or financial concerns related to COVID-19. A standardized assessment (e.g., Coronavirus Anxiety Scale; National Institute of Health Office of Behavioral & Social Sciences Research, 2020) may help assess the severity of COVID-specific concerns and supplement the usual clinical interview and standard instruments customarily used to assess the current emotional state effects on NP exam results.
Use of masks, gloves, or other personal protective equipment (PPE) by examiners and/or examinees may have additional adverse impacts on validity. Masks may be distracting to examinees and therefore affect performance on tests. Masked verbalizations may be harder to understand for both examinee and examiner. This may be particularly problematic for tests where standard administration procedures do not allow repetition of items (e.g., Digit Span) and tests measuring the ability to distinguish sounds (e.g., items from a measure of phonological processing that are read aloud by the examiner). Masks may also interfere with nonverbal communications including facial expressions and articulatory movements.
Increased distance between patient and examiner may make it more difficult for instructions to be delivered effectively and for examiners to record responses accurately. Although some recommendations focus on a distance of “six feet” between examiner and examinee, considerations include the configuration of the space, ventilation, and how long the exposure lasts. In some settings, novel physical barriers may be put in place between patients and office staff and/or examiners (e.g., plexiglass shields at reception desks or within exam rooms) when closer seating arrangements are unavoidable, but in those situations airflow and filtration must be considered carefully, and their impact on test performance has not been evaluated.
Restricted use of manipulatives and other articles that are “high contact” during testing. Procedures that involve the patient and the examiner touching the same materials (e.g., blocks, pegs, tapping devices, pencils) may be minimized and alternatives identified.
In-clinic TeleNP
In this model, both the clinician and the patient are in a clinic but in separate rooms using videoconferencing methods to conduct the NP assessment. In some circumstances, the rooms are in different clinic locations (e.g., a patient in a satellite clinic in a rural area and a neuropsychologist in a main clinic in a city center), and in other models, the rooms are in the same building. Having patients in a separate room further reduces the risk of patient and clinician exposure to coronavirus as compared to direct in-person mitigated assessment. Clinicians control the quality of the TeleNP platform and equipment, are available to troubleshoot, can control the testing environment, and typically have greater ability to monitor patients.
Most TeleNP research has been conducted in the context of in-clinic TeleNP, and because of the larger research base, the in-clinic method is generally better validated than in-home TeleNP assessments. The existing literature for in-clinic TeleNP suggests that at least for some measures the actual difference between in-person and in-clinic TeleNP modalities is small (e.g., Hedges g = 0.033 or 1/33 SD; Bilder et al., 2020). However, validation and equivalence studies are lacking for many measures and a wide array of patient populations. The “Computerized Neuropsychological Assessment Devices: Joint Position Paper of the American Academy of Clinical Neuropsychology and the National Academy of Neuropsychology” (Bauer et al., 2012) clarifies that “a computerized test adapted from an examiner administered test is a new test. As a result, it is essential that new normative data with adjustments for the pertinent demographic variables be established for computerized tests. Utilizing an in-clinic TeleNP model with tests that have not yet been validated in this context will reduce the validity of diagnostic conclusions.
In-home TeleNP assessments (patient at home)
The NP evaluation is conducted with the patient in their own home or other remote location via audio or videoconferencing technology (Bilder et al., 2020). Most of the TeleNP research has not been conducted in this context, where examiners do not have control over the availability or quality of the telehealth platforms, cannot guarantee the availability of a distraction free testing environment, cannot help troubleshoot technical problems, and have limited ability to monitor patients. Note that the testing portion of the NP assessment may or may not be included in the episodes of neuropsychological care conducted via in-home TeleNP. Interviews of patients and collaterals combined with a record review may provide sufficient information in some cases, and the clinician may decide there is not sufficient incremental validity of additional NP testing to justify risks to validity of nonstandard administration.
Several factors may limit the benefits of in-home TeleNP assessment in specific patient populations. Reduced patient access to technology due to economic disparities and potentially widening health disparities is a significant problem. For example, a Pew Research study in 2015 found that 15% of Hispanic and 12% of Black Americans (vs. 4% of Whites) rely on smartphones and do not have internet access (Pew Research, 2015). Disabled Americans are less likely to have computers, smartphones, or any internet access at all (Pew Research, 2017). Sixteen percent of persons in the USA aged 16–65 are not digitally literate, and adults who are not digitally literate are, on average, less educated, older, and more likely to be Black, Hispanic, or foreign born, compared to digitally literate adults (Pew Research, 2019).
Socioeconomic disparities may further result in patients having limited access to a quiet, distraction-free place to engage in home TeleNP assessment. Finally, few validation studies for TeleNP have been conducted for multilingual, non-European American patients.
Combined, hybrid, or staged models (combining elements of TeleNP with elements of in-person face-to-face)
Clinicians might blend elements of TeleNP (either in clinic or at home) with mitigated in-person assessment to maximize the benefits and minimize the risks of the overall assessment strategy. By conducting some procedures via home or in-clinic TeleNP, it may be possible to narrow the scope of questions that must be addressed in person, thereby minimizing exam time and exposure to risks associated with the coronavirus.
For example, initial interviews, select testing measures, and feedback sessions might be conducted using telehealth platforms to reduce the number of hours an examinee needs to spend in a clinic. There may be instruments that have been validated via in-clinic or in-home TeleNP with a particular patient population and those might be administered with confidence via in-clinic or in-home TeleNP. Other instruments lacking TeleNP validation might be administered in person.
Stepped care
The primary care model of making medical treatment decisions based on a “stepped-care” approach can be applied to NP episodes of care (Lanca, 2018; Sobell & Sobell, 1999, 2000). With the stepped-care model, care proceeds in a stepwise fashion from least intensive to most intensive. These steps can also be recursive. That is, a patient who may have had a full NP evaluation in the past may only require a briefer evaluation for continued monitoring or consultation in the future. This stepped model of care becomes even more relevant in the current COVID era since the benefit of stepped care increases the flexibility for modality of treatment and decreases the length of NP assessment, which decreases exposure time.
Delaying the assessment until it is possible to see the patient in person without modifications
The timeframe for the conditions under which this would again be safe (development and wide availability of vaccine) is currently unknown. The risks of delaying neuropsychological care are described earlier.
Decision-Making: Patient Risk Stratification, Assessing Community Risk, and Selecting the Most Appropriate Strategy for NP Assessment During the Pandemic
Patient Risk Stratification
Considering the benefits of NP assessment in the context of the risks of in-person practice during the pandemic, as mitigated by the various models for assessment noted earlier, is a complex process and involves at least four different factors (see Fig. 1).
Fig. 1.

Patient risk stratification.
Urgency of care
Practitioners should consider the urgency of the clinical condition/situation and the potential adverse consequences if NP assessment is delayed. Does the NP assessment have to occur prior to a surgical procedure? Does the referral question involve the possibility that the patient may require increased levels of supervision or other treatments, without which there would be adverse consequences?
Symptom acuity and impact
Practitioners should consider the severity of the presenting symptoms and the likelihood that the condition may cause harm if NP assessment information is lacking. Is the patient experiencing high levels of depression or actively hallucinating? Is the patient, per family report, engaging in dangerous activities (such as driving while cognitively compromised)?
Incremental validity
Practitioners should consider the incremental validity of different NP procedures to competently answer the primary referral question and make appropriate diagnoses and treatment recommendations for the patient. A NP interview, collateral interview(s), and records review may be conducted using telehealth methods at very low risk of viral transmission, and higher risk in-person NP testing may only be well justified—in the context of risk of viral transmission—by determining the elements of the assessment that will provide incremental validity for the most pressing aspect of the referral question. As an example, in the case of an 11-year-old child diagnosed with dyslexia the year prior via cognitive and academic achievement testing, where the primary referral question is whether continued reading intervention is necessary, a clinician might conclude that repeating a reading assessment adds considerable incremental validity to the most pressing aspect of the referral question but that repeating the rest of the battery might be delayed until extended face-to-face assessment is safer.
Assessment of incremental validity should also consider the validity data supporting the chosen model of assessment. For example, a visual memory test lacking validation evidence for in-home TeleNP may not have clear incremental validity. The same test may have been validated using in-clinic TeleNP, so the incremental validity of administering the test via in-clinic TeleNP may be judged as higher. The use of that same procedure in home TeleNP may also vary in validity depending on the technology, bandwidth, home setting, and comfort levels of both patient and clinician with the use of this technology. These considerations highlight the complexity and context specificity of these decisions.
Individual health risk for COVID-19
Practitioners should consider whether the patient or a close family member of the patient has underlying health conditions that may increase the risk of serious complications from contracting the virus. As noted earlier, for Phase I and Phase II reopening as defined by White House/CDC criteria, “vulnerable persons” (i.e., individuals with serious underlying health conditions, including high blood pressure, chronic lung disease, diabetes, obesity, asthma, and those whose immune system is compromised, such as by chemotherapy for cancer and other conditions requiring such therapy) are instructed to continue to follow “safer-at-home” orders. Practitioners also should consider these guidelines for their own personal health and safety. For more details: https://www.whitehouse.gov/openingamerica/#criteria.
Community risk
In addition to the above individual risk stratification, providers should consider larger issues of population risk. How many cases are in the community? What is the likelihood that the individual, if seen in person, might increase risks to the community or family from which they are coming and to which they will return?
As clinicians engage in a decision-making process, it may be helpful to consider a balance between competing threats (Fig. 2). Traditional nonmitigated NP practice may result in the fewest threats to validity, but greater risks to safety, depending on the health status of a particular patient and the community threat level. In-home TeleNP may result in the fewest threats to safety but pose substantial risks to validity.
Fig. 2.
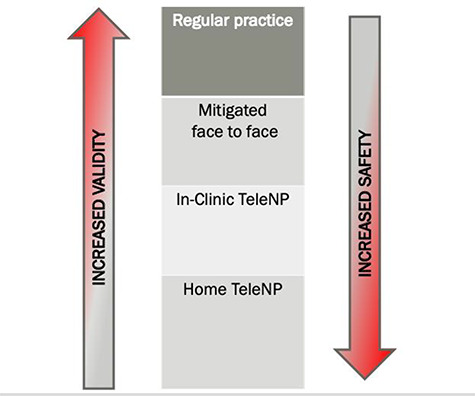
Balancing safety and validity.
In this context, clinicians are encouraged to consider combined/staged or hybrid models where many aspects of the episode of NP care can be provided via TeleNP platforms and carefully consider the incremental validity of any proposed test administration if that is to be included in a larger assessment process.
Mitigation Procedures
Multiple governmental agencies and professional organizations have released guidance on minimizing risk of patient and healthcare provider exposure. Clinicians are encouraged to utilize these resources in formulating mitigation plans. Additionally, state and local government guidance regarding conditions of reopening as well as mitigation strategies should be consulted. Malpractice insurance carriers may offer consultations regarding a practice mitigation plan as a service to their insured, and if this is available, clinicians are strongly recommended to take advantage of this service.
Center for Disease Control: https://bit.ly/CDCminimize and CDC Preparing your Clinic https://bit.ly/CDCprepclinic
World Health Organization: Getting Your Workplace Ready: https://bit.ly/WHOworkready
OSHA Guidance on Preparing the Workplace for COVID-19: https://bit.ly/OHSAworkplace
The Johns Hopkins Center for Health Security has released a very helpful Operational Toolkit for Businesses Considering Reopening or Expanding Operations in COVID-19 that walks one through mitigation procedures that depend on stratified risk levels: https://bit.ly/JHtoolkit
American Professional Agency preparing to reopen The Nuts and Bolts of Reopening Your Practice after COVID-19: https://bit.ly/APAnutsbolts
American Medical Association—Reopening Guide: https://bit.ly/AMAreopen
There are basic commonalities noted across various federal, state, local, and professional organization regulations and guidelines that must be in place prior to reopening for in-person services. An outline/discussion of these essential infection mitigation processes is included below but is not meant to be exhaustive. For an expanded discussion of mitigation procedures, see https://iopc.online.
Prior to resuming in-person clinical care, it is important for clinicians to have infection mitigation plans in place, along with contingency plans for possible scenarios where the planned procedures cannot be followed. Once a plan is in place, most guideline documents strongly recommend opening in an incremental, step-by-step fashion. This means starting with a very low volume of patients, following the plan that was developed as literally as possible. Once a few patients are seen, the plan can be modified as needed based on real-time patient contact activities. Increases in patient volume can occur incrementally, with maximum patient load determined by your setting and ability to follow pandemic mitigation processes.
Prior to Reopening
Develop a model of care plan for patients. In a lifespan practice, a separate plan might be developed for pediatric, adult, and geriatric patients. The plan will ideally include multiple options that take into account risk stratification for each individual patient.
Create appropriate signage for waiting areas, treatment rooms, and in paper form outlining the policies/procedures for infection mitigation in your office(s).
-
Create a written plan for:
Pre-appointment screening for potential symptoms of COVID-19 (see https://iopc.online for example screening forms). The plan should include a clear policy regarding what happens if screening is failed.
Day-of-appointment screening policy for both patients and staff that might include temperature screens. The plan should include a clear policy regarding what happens if screening is failed.
Personal protective equipment that staff and patients will be expected to use. This includes masks and might include (depending on the setting and risk level) gloves, face shields, goggles, or safety glasses that cover the eyes, use of scrubs, and gowns.
-
Maintaining appropriate social distancing. The plan may include
specific flow patterns through the office
limits on family members accompanying patients
use of virtual (parking lot) waiting rooms
removal of some chairs in waiting areas as needed area to promote social distancing
use of clear (plexiglass) barriers across a testing table with or without openings for stimuli to be presented (does not eliminate need for masks)
staggering appointment times to minimize patient contact and to allow for additional cleaning/ventilation time in between
Hand washing and/or use of hand sanitizer procedures to be used by all parties before and after any contact with a patient, caregiver, staff, or provider.
Cleaning/disinfecting office areas, furniture, surfaces, doors, and manipulative items (including writing utensils) before and after every patient contact. The plan should include a daily use checklist. (See https://iopc.online/ for sample checklists.)
-
Implementing structural mitigation procedures. The plan might include:
Designation of “clean” (i.e., unexposed) materials, forms, etc. area and a separate area for “dirty” (i.e., exposed) materials so as avoid cross-contamination of items.
Use of HEPA air filters for a period of time prior to and after exam room use. HEPA filters can also be run on lower speeds during the assessment.
Changing fabric furniture to furniture that can be cleaned with recommended cleaning agents or covering fabric furniture with wipeable protective covers.
Use of foot-operated trash cans.
Obtain personal protective equipment including masks to be worn by patients, providers, and any office staff, as well as plexiglass barriers if these are part of the social distancing plan.
Timeline of Infection Mitigation Activities
Activities prior to patient arrival
COVID screening questionnaire administered at the time of scheduling and 48 hr prior to the appointment (either via phone contact or email).
Send link to electronic registration forms that can be completed and submitted online prior to arrival as well as written instructions regarding safety requirements for visit (masks, etc.), any limitation on number of persons present (e.g., only one caregiver, no siblings), and specific instructions for a virtual waiting room if one is being used.
Clean rooms and materials (use of checklist with time and date recommended). See https://iopc.online/ for an example that can be edited to fit individual clinic needs.
Initial entry
Patient and visitors screened again for symptoms. This may include temperature screening.
Review of mitigation/hygiene procedures with patients.
Hand sanitizer or hand washing upon arrival.
-
If forms cannot be completed electronically prior to arrival:
Complete forms in a controlled room rather than bringing forms from home
Consider use of verbal consent and related documentation
Use of “clean” and “dirty” folders or containers for forms.
Interview
Consider patient and collateral interviews via in-home TeleNP to minimize time in office.
Testing activities
Maximize efficiency of test session to minimize time in office.
Minimize testing where contact of materials is needed.
-
“Clean” versus “dirty” side of the room (including folders of paper—clean and dirty).
No touching of “dirty” forms for 24 hr or wash hands after handling
Cleaning of manipulative stimuli with disinfecting wipes and/or separating them for cleaning after the assessment.
Repeated use of hand sanitizer and hand washing during the session as needed (e.g., if a person touches his or her face, sneezes, coughs, etc.).
If used, gloves should be discarded and replaced in any instance where hands would have been washed or sanitized (e.g., touching face, coughing into hands).
Laminate paper stimuli or cards or put them in plastic sheets for easy cleaning.
Consider using orally administered measures of visual information processing to maximize social distancing and minimize contact with materials.
Place garbage can close to the patient—foot-operated or open, with plastic liner for easy removal.
Separate pencils/pens for patients and examiner.
End of session
No hand shaking or physical contact.
Be mindful of social distancing as you leave the room.
After the session
-
Clean room, furniture, contact surfaces, materials, etc. (note that some disinfecting wipes require use of gloves).
Timing of cleaning—may benefit from at least a 30-min waiting period before cleaning, to minimize airborne droplets
Wash hands or use hand sanitizers after handling forms (e.g., when scoring) and/or allow a 24-hr waiting time before handling forms touched by the patient.
Engage room HEPA air filter system.
Feedback options to consider
Feedback may be conducted where possible via in-home TeleNP.
Same day, in same room, immediately following the testing or after a short break.
If separate day in clinic, use the same precautions noted earlier for the return visit. It is recommended that providers remain vigilant to local, state, federal, and professional organization guidelines regarding the resumption of in-person clinical practices. Regular monitoring of recommendations by the CDC, WHO, and other trusted sources is also recommended to stay as up-to-date as possible regarding infection mitigation strategies. Finally, providers are advised to visit the IOPC website (https://iopc.online/) for additional updates and recommendations.
Informed Consent
Providing NP care in the context of a pandemic requires complex decision-making about risks and benefits. As clinicians, we are ethically mandated to engage patients in a consent process where both risks and benefits are clearly explained. This is likely to be a departure from the relatively straightforward consent conversations neuropsychologists are used to, where there are minimal risks to physical well-being and validity. Additionally, neuropsychologists may be personally uncomfortable with proceeding with an assessment (whichever above model is chosen) without a clear-cut “right answer” and when each option holds its own risks to validity and/or safety. The discomfort, if present, may create a barrier to a clear, thorough consent process.
In most cases, a thorough consent conversation will need to include the benefits and risks of all three options (in-person, TeleNP and hybrid models), with a recommendation from the clinician regarding the best path forward. It is important that the language is clear and avoids jargon. Words like “mitigation,” “validity,” “standardized assessment,” and “reliability,” for example, are likely to be experienced as jargon. It is also important to not overstate clinicians’ ability to “take into account” the impact of nonstandard assessment.
Consent for TeleNP
Informed consent for TeleNP has been described at length in the IOPC Recommendations/Guidance for Teleneuropsychology (TeleNP) in Response to the COVID-19 Pandemic (Bilder et al., 2020). Additionally, Parma Trust insurance has developed an informed consent document for TeleNP: https://bit.ly/TrustConsent. Key points to cover include:
Modification of standard test administration affects results in ways that are so far unknown. This reduces confidence in the diagnostic conclusions and may affect recommendations for treatment.
Involvement of a caregiver, guardian, parent, and facilitator is a nonstandard condition for testing and also threatens confidence in diagnostic conclusions.
Error may be compounded with patients from culturally and linguistically diverse populations, patients who require an interpreter, or patients who have limited experience/comfort with the technology being used.
Some qualitative data usually obtained during an in-person exam will be lost, and this may reduce the richness of the clinical data and further limit conclusions and recommendations.
TeleNP may pose risks to privacy and confidentiality.
Assessment results may not be acceptable by organizations for administrative purposes.
A discussion of the risks and benefits of in-person assessment, hybrid TeleNP, or no assessment as an alternative to TeleNP assessment.
Appropriate disclosure and referral to a provider who is conducting in-person assessments, if a factor in recommending TeleNP is a health condition of the clinician that makes in-person assessment risky to the provider.
Consent for in-person assessments
The American Psychological 2018 Association has developed a sample informed consent form for resuming in-person services: https://bit.ly/APAconsent. The document is largely geared toward psychotherapy services. Additional risks of exposure emerge in the context of the typically greater number of hours spent in NP assessment services. See IOPC.online for sample informed consents for return to in-person NP practice. Key points to cover include:
By coming to an office or hospital, patients have an increased risk of exposure to the virus compared with staying home.
A clear set of measures patients and their families need to agree to take to minimize the risk of exposure to others in the office (including staff and other patients).
A clear set of measures clinicians will take to minimize the risk of exposure for patients.
Explanation of any screening measures, including temperature checks, at the beginning of services and the expectation that individuals who are ill will be expected to leave the office.
A recognition that the procedures for minimizing risk may change over time and both parties will discuss necessary changes in procedure.
The expectation that if the risk conditions change (e.g., a resurgence of cases in the vicinity), in-person services may no longer be feasible.
Confidentiality in the case of infection (with potential duty to notify local authorities depending on jurisdiction).
Discussion of the potential threats to diagnostic conclusions in the context of the possibility that viral risk mitigation procedures such as masks might affect standard test administration.
A discussion of the risks and benefits of TeleNP, hybrid TeleNP, or no assessment as an alternative to in-person assessment.
Consent for Combined Models
Clinicians will need to discuss the aspects of consent for both in-person and TeleNP.
Documentation/Explanation of Nonstandard Procedures in Reports and During Feedback
Any departure from the nonmitigated in-person NP assessment procedure will need to be clearly documented in easy to understand language within the body of the NP report. Ideally, this should be included in the procedure section and then referenced in the discussion section, with appropriate diagnostic limitations. The IOPC Recommendations/Guidance for Teleneuropsychology (TeleNP) in Response to the COVID-19 Pandemic (Bilder et al., 2020) suggests the following (or similar) statement be included in NP assessment reports where TeleNP is utilized:
Due to circumstances that prevent in-person clinical visits, this assessment was conducted using telehealth methods (including remote audiovisual presentation of test instructions and test stimuli, and remote observation of performance via audiovisual technologies). The standard administration of these procedures involves in-person, face-to-face methods. The impact of applying non-standard administration methods has been evaluated only in part by scientific research. While every effort was made to simulate standard assessment practices, the diagnostic conclusions and recommendations for treatment provided in this report are being advanced with these reservations.
Similarly, the impact on diagnostic conclusions and recommendations of departing from standard nonmitigated in-person NP assessment will need to be restated at the beginning of feedback sessions. It is important not to overstate clinicians’ ability to “take into account” nonstandard test administration.
Conflict of Interest
No potential conflict of interest was reported by the authors.
This article has been co-published with permission in ARCHIVES OF CLINICAL NEUROPSYCHOLOGY and THE CLINICAL NEUROPSYCHOLOGIST. All rights reserved in respect of ARCHIVES OF CLINICAL NEUROPSYCHOLOGY, © The Authors, and in respect of THE CLINICAL NEUROPSYCHOLOGIST, © The Authors. The articles are identical except for minor stylistic and spelling differences in keeping with each journal’s style. Either citation can be used when citing this article.
Footnotes
The Inter Organizational Practice Committee (IOPC) is a committee of the practice chairs of the American Academy of Clinical Neuropsychology/American Board of Clinical Neuropsychology, the National Academy of Neuropsychology, Division 40 of the American Psychological Association, the American Board of Professional Neuropsychology, and the American Psychological Association Services, Inc. (APAS) tasked with coordinating advocacy efforts and improving the practice climate for Neuropsychology.
It is generally agreed that these three terms are to be interpreted in descending order of immediacy but the boundaries separating the conditions may be unclear, and there are multiple frameworks for understanding the level of urgency. See for example https://bit.ly/ ElectiveRecs
Contributor Information
Karen S Postal, Department of Psychiatry, Harvard Medical School, Cambridge, MA, USA.
Robert M Bilder, Psychiatry & Biobehavioral Sciences and Psychology, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, CA, USA.
Margaret Lanca, Department of Psychiatry, Harvard Medical School, Cambridge Health Alliance, Boston, MA, USA.
Darrin M Aase, Wexner Medical Center, The Ohio State University, Columbus, OH, USA.
Mark Barisa, Performance Neuropsychology, Frisco, TX, USA; University of North Texas, Denton, TX, USA.
Alice Ann Holland, Psychiatry, University of Texas Southwestern Medical School, Dallas, TX, USA; Children’s Medical Center of Dallas, Dallas, TX, USA.
Laura Lacritz, Psychiatry, University of Texas Southwestern Medical School, Dallas, TX, USA.
David M Lechuga, Neurobehavioral Clinic and Counseling Center, Lake Forest, CA, USA.
Susan McPherson, Private Practice, Edina, MN, USA.
Jennifer Morgan, American Psychological Association, Washington, DC, USA.
Christine Salinas, Neuropsychology Concierge, Indialantic, FL, USA; College of Medicine, University of Central Florida, Orlando, FL, USA.
References
- American Educational Research Association, American Psychological Association, National Council on Measurement in Education, & Joint Committee on Standards for Educational and Psychological Testing (U.S.) (2014). Standards for educational and psychological testing. AERA. [Google Scholar]
- American Psychological Association (APA) (2017). Ethical principles of psychologists and code of conduct (2002, amended effective June 1, 2010, and January 1, 2017). https://www.apa.org/ethics/code/
- Bauer R. M., Iverson G. L., Cernich A. N., Binder L. M., Ruff R. M., & Naugle R. I. (2012). Computerized neuropsychological assessment devices: joint position paper of the American Academy of Clinical Neuropsychology and the National Academy of Neuropsychology. Archives. [DOI] [PMC free article] [PubMed]
- Bilder R., Postal K., Barisa M., Aase D. M., Cullum M., Gillaspy S. et al. (2020). Inter Organizational Practice Committee Recommendations/Guidance for Teleneuropsychology (TeleNP) in Response to the COVID-19 Pandemic. The Clinical Neuropsychologist. doi: 10.1080/13854046.2020.1767214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun M., Tupper D., Kaufmann P., McCrea M., Postal K., Westerveld M. et al. (2011). Neuropsychological assessment: A valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cognitive and Behavioral Neurology: Official Journal of the Society for Behavioral and Cognitive Neurology, 24(3), 107–114. doi: 10.1097/WNN.0b013e3182351289. [DOI] [PubMed] [Google Scholar]
- Donders J. (2020). The incremental value of neuropsychological assessment: A critical review. The Clinical Neuropsychologist, 34(1), 56–87. doi: 10.1080/13854046.2019.1575471. [DOI] [PubMed] [Google Scholar]
- Lanca M. (2018). Integration of neuropsychology in primary care. Archives of Clinical Neuropsychology: The Official Journal of the National Academy of Neuropsychologists, 33(3), 269–279. doi: 10.1093/arclin/acx135. [DOI] [PubMed] [Google Scholar]
- National Institute of Health Office of Behavioral and Social Sciences Research (2020). BSSR research tools. https://www.nlm.nih.gov/dr2/COVID-19_BSSR_Research_Tools.pdf.
- Parma Trust Insurance (2020). Factors to consider in reopening in-person psychological services during the COVID-19 crisis. https://parma.trustinsurance.com/Portals/0/documents/The%20Trust’s%20Statement%20on%20Returning%20to%20In-Person%20Services.pdf
- Pew Research (2015). https://www.pewresearch.org/fact-tank/2015/04/30/racial-and-ethnic-differences-in-how-people-use-mobile-technology/
- Pew Research (2017). https://www.pewresearch.org/fact-tank/2017/04/07/disabled-americans-are-less-likely-to-use-technology/
- Pew Research (2019). https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/
- Sobell M. B., & Sobell L. C. (1999). Stepped care for alcohol problems: An efficient method for planning and delivering clinical services In Tucker J. A., Donovan D. A., & Marlatt G. A. (Eds.), Changing addictive behavior. Bridging clinical and public health strategies (, pp. 331–343). Guilford Press. [Google Scholar]
- Sobell M. B., & Sobell L. C. (2000). Stepped care as a heuristic approach to the treatment of alcohol problems. Journal of Consulting and Clinical Psychology, 68(4), 573–579. doi: 10.1037/0022-006X.68.4.573. [DOI] [PubMed] [Google Scholar]
- Watt S., & Crowe S. F. (2018). Examining the beneficial effect of neuropsychological assessment on adult patient outcomes: A systematic review. The Clinical Neuropsychologist, 32(3), 368–390. doi: 10.1080/13854046.2017.1414885. [DOI] [PubMed] [Google Scholar]


