Cardiovascular manifestations of coronavirus disease 2019 (COVID-19) include myocardial injury, myocarditis, and cardiac arrhythmias. Recent reports have demonstrated Takotsubo cardiomyopathy (TCM) as a complication of COVID-19.1 A review of the literature has yielded 10 cases of TCM in patients with COVID-19; 90% of the cases occurred in women with a mean age of 64.6 years. Apical involvement was the most common form.
TCM, also known as stress-induced cardiomyopathy, is a clinical syndrome that is characterized by a transient reversible wall motion abnormality of the left ventricle in the absence of significant obstructive coronary artery disease.2 Apical TCM is the most common form (>80%) followed by the midventricular form.2 TCM is typically associated with intense emotional or physical stress, and is most commonly seen in women (>90%). Patients with a physical stress (e.g. infectious, surgical, or hypoxic) typically have a worse prognosis compared with those with an emotional trigger.
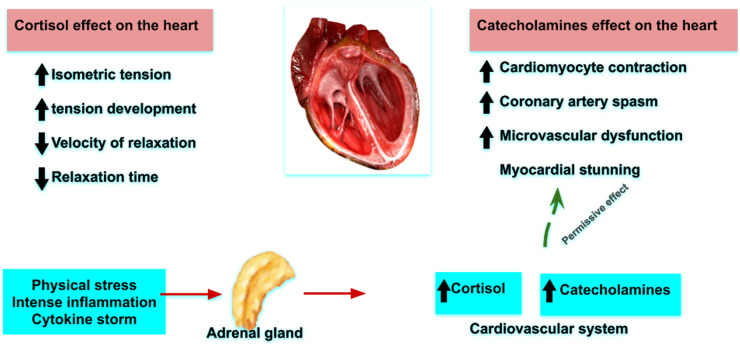
The pathophysiology of TCM is not well understood. In a study of 19 patients with TCM, Wittstein et al.3 reported very high plasma levels of catecholamines (epinephrine, norepinephrine, and dopamine) compared with the normal population. Intense sympathetic overstimulation by catecholamines (catecholamine-mediated myocardial stunning) might result in myocardial stunning as a direct effect of catecholamines on cardiomyocytes, hyperdynamic contractility, epicardial spasm, and/or microvascular dysfunction.
Tan et al.4 showed that patients with COVID-19 have a markedly high level of cortisol that is higher than that observed in patients undergoing major surgery. Penefsky et al. reported that administration of glucocorticoid increased isometric tension and tension development, reduced the velocity of relaxation in papillary muscle, and shortened the total relaxation time without a significant change in contraction time.5 Although the precise basis of adverse effect of these changes on regional cardiac dysfunction is not known, it is possible that the very high levels of cortisol in concert with high levels of catecholamines related to the common underlying mediator(s) (inflammation and cytokine storm) might exert a direct ‘toxic’ effect on cardiomyocytes in COVID-19 patients, and play a role in the development of TCM.
Studies that compare the levels of cortisol and other stress-related hormones between patients with TCM and COVID-19 infection and others with COVID-19 without TCM are needed. Such studies will advance our understanding of the pathophysiology of TCM and the role of stress-related hormones in this disease.
Conflict of interest: none declared.
Figure 1.
Proposed mechanism for the pathophysiology of Takotsubo cardiomyopathy in patients with COVID-19 infection.
References
- 1. Nguyen D, Nguyen T, de Bels D, Castro Rodriguez J. A case of Takotsubo cardiomyopathy with COVID 19. Eur Heart J Cardiovasc Imaging 2020;XXXdoi:10.1093/ehjci/jeaa152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschöpe C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfister R, Ukena C, Böhm M, Erbel R,, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun-Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T,, Airaksinen KE, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L,, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Lüscher TF. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015;373:929–938. [DOI] [PubMed] [Google Scholar]
- 3. Wittstein IS, Thiemann DR, Lima JAC, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, Rade JJ, Bivalacqua TJ, Champion HC. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–548. [DOI] [PubMed] [Google Scholar]
- 4. Tan T, Khoo B, Mills EG, Phylactou M, Patel B, Eng PC, Thurston L, Muzi B, Meeran K, Prevost AT, Comninos AN, Abbara A, Dhillo WS. Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol 2020;8:659–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Penefsky ZJ, Kahn M. Inotropic effects of dexamethasone in mammalian heart muscle. Eur J Pharmacol 1971;15:259–266. [DOI] [PubMed] [Google Scholar]