Abstract
Background
There are limited nationwide data regarding breast cancer surgery in China. The Chinese Anti‐Cancer Association's Committee of Breast Cancer Society and the Chinese Society of Breast Surgeons conducted a nationwide survey to examine the use of and barriers associated with surgical options among patients with breast cancer.
Methods
Surveys were sent via e‐mail to the directors of 110 centers that performed at least 200 breast cancer operations in 2017. The electronic questionnaire contained 183 questions and covered six aspects, including demographic information about the hospitals and surgeons, surgical practice, and application of breast reconstruction.
Results
The selected hospitals were from 31 provinces or municipalities. The overall proportion of breast‐conserving surgery (BCS) was 22%. Local gross domestic product was significantly related to the rate of BCS (p = .046). Sentinel lymph node biopsy was performed routinely in 76% of hospitals. Only 14.5% (16/110) of hospitals used the dual‐tracer method, including radioisotopes. For patients with cN0 disease receiving BCS with one or two positive sentinel lymph nodes, 20% (22/110) of hospitals accepted omitting axillary lymph node dissection (ALND). For patients who underwent mastectomy, only 4% (4/110) of hospitals accepted omitting ALND. There was an obvious polarization trend in the proportion of oncoplastic breast‐conserving surgery (OPS); 35/110 (32%) performed OPS in fewer than 10% of cases, whereas 36/110 (33%) performed OPS in more than 50% of cases. OPS was more likely to be performed in academic hospitals. Volume displacement was more commonly used than volume replacement (p < .001). Breast reconstruction was routinely performed in 96/110 (87%) of hospitals, 62% of which involved cooperation with the plastic surgery department. Factors influencing breast reconstruction after mastectomy included the establishment of a plastic surgery department, regional economy, and cooperation between the plastic and general surgery departments. Overall, the proportion of breast reconstruction procedures after mastectomy was 10.7%, with 70% being implant‐based reconstruction, 17% autologous tissue reconstruction, and 13% a combination. Overall, 22% of the hospitals predominantly performed immediate breast reconstruction. For delayed reconstruction, two‐stage implant‐based breast reconstruction was the first choice for 46% of centers, whereas 20% of centers chose autologous reconstruction. Among the 96 centers that performed autologous‐based reconstruction, 96% performed latissimus dorsi flap reconstruction, 65% performed transverse rectus abdominis musculocutaneous flap reconstruction, and 45% used deep inferior epigastric artery perforator flaps.
Conclusion
The results are of great value for promoting the implementation of a consensus on diagnostic and treatment standards, development of guidelines for breast cancer, and training of breast specialists.
Implications for Practice
This study aimed to establish comprehensive baseline data on the status of current breast cancer treatment in China by presenting the statistics on clinical treatments and surgeries, the distribution of clinical stages, and the demographic characteristics of patients. This report is based on a survey conducted by the Chinese Anti‐Cancer Association's Committee of Breast Cancer Society and the Chinese Society of Breast Surgeons, which examined the use of breast cancer surgical options in hospitals all over the country and the factors hindering the adoption of procedures and techniques. This study makes a significant contribution to the literature because there are limited nationwide data regarding breast cancer surgery in China.
Keywords: Breast cancer, China, Breast surgery, Breast reconstruction, Questionnaire survey
Short abstract
On the basis of a survey that examined the use of breast cancer surgical options in hospitals across China, this article reports statistics on clinical treatments and surgeries, the distribution of clinical stages, and demographic characteristics of patients, in order to establish comprehensive baseline data on the current status of breast cancer treatment in China.
Introduction
Breast cancer is the most common cancer among Chinese women according to data from the Global Cancer Observatory (2018), with an age‐standardized rate of 39.2 cases per 100,000 women in eastern Asia 1. Access to and timely delivery of optimum care for breast cancer affects clinical outcomes, but important disparities in the availability of surgical options exist across China. Patterns of practice for the surgical management of breast cancer vary considerably among regions and among hospitals.
Since the first edition of the Chinese Anti‐Cancer Association Guideline for Breast Cancer was published in 2007, breast‐conserving surgery (BCS) has become the guideline‐recommended surgical modality. However, in a retrospective study 2 that included 20,551 patients who had undergone surgical treatment for breast cancer at the Fudan University Shanghai Cancer Center between January 1999 and June 2014, the proportions of patients who had undergone mastectomy and BCS were 81.2% (17,040 cases) and 15.3% (3,216 cases), respectively. A 10‐year nationwide multicenter retrospective study (1999–2008) conducted in China indicated that modified radical mastectomy remained the primary strategy for treating breast cancer 3. This is thought to be due to the smaller size of breasts in Chinese women, a shortage of resources for applying radiation therapy, and the deep‐rooted traditional beliefs concerning cancer among Chinese patients, which persist despite the growing proportion of patients being diagnosed at much earlier stages thanks to increasing public awareness and the development of screening programs 4.
Complete axillary lymph node dissection (ALND), with its attendant risks of complications such as lymphedema and other local morbidities, was conducted in 84.1% of patients in Beijing in 2008 5, 57.6% of whom had no lymph node involvement. In 2018, a national survey conducted in Guangzhou reported that sentinel lymph node biopsy (SLNB) was routinely performed at 93.2% of hospitals for patients with clinically negative axillary lymph nodes 6.
In the aforementioned study 2 conducted at Fudan University Shanghai Cancer Center, the rate of breast reconstruction was found to be 3.4% (718 cases) from January 1999 to June 2014. Among 4,185 patients in China registered in a Chinese database from 1999 to 2008, 0.02% underwent immediate reconstruction, whereas among 74,502 patients with breast cancer registered in the Surveillance, Epidemiology, and End Results database from 2000 to 2010, the immediate reconstruction rate was 9.9% 7. Factors related to the restricted adoption of new surgical techniques include the high level of technical difficulty, the long period of personnel training in reconstruction surgery, and the difficulties in acquiring prostheses and other materials. Although informative, most studies on the status of breast cancer treatment in China were primarily single‐center and retrospective studies: hence the need for a panoramic multicenter survey.
This study aimed to establish comprehensive baseline data on the status of current breast cancer treatment in China by presenting the statistics on clinical treatments and surgeries, the distribution of clinical stages, and the demographic characteristics of patients. This report is based on a survey conducted by the Chinese Anti‐Cancer Association's Committee of Breast Cancer Society (CACA‐CBCS) and the Chinese Society of Breast Surgeons (CSBS), which examined the use of breast cancer surgical options in hospitals all over the country and the factors hindering the adoption of procedures and techniques. The survey is available as supplemental online Appendix 1. This survey also revealed the implementation of cutting‐edge surgical techniques in the diagnosis and treatment of breast cancer, which should guide the design of training programs for vocational education of clinical specialists in the future.
Materials and Methods
Questionnaire
The survey questionnaire was designed by a committee directed by Professor Jiong Wu of the Fudan University Cancer Hospital, and attention was paid to creating unbiased nonleading questions.
The questionnaire comprised six sections, including 183 multiple‐choice questions in total, of which 92.3% required single answers and the rest required multiple answers. The first section focused on the demographics of surgeons and their practice characteristics. The second section collected information about the hospital or institution that was enrolled in the study, including the general situation regarding breast cancer surgery and breast reconstruction after mastectomy. The third section concentrated on breast reconstruction surgery among all new breast cancer cases treated during 2017. The fourth section focused on the details of breast reconstruction, including the type and timing of reconstruction and associated complications. The fifth section collected information about other revision techniques, such as nipple‐areola reconstruction, fat grafting, and breast symmetry correction. The last section inquired about the respondents’ personal opinions regarding factors that restricted the development of breast reconstruction in China. The responses were tabulated and assessed.
A number of questions concerning the proportion of certain types of patients or surgeries asked the respondent to choose from several ranges of options. In some cases, the medians of these ranges were taken and then weighted by the number of surgeries performed at each hospital to calculate an overall proportion.
Survey Methodology
Among all centers in China in which at least 200 cases of breast cancer were surgically managed in 2017, survey respondents were selected according to the province and the number of surgeries to maximize diversity. The survey attempted to cover all provinces, although for a few provinces this was not possible; details are provided below. In each province, hospitals were sampled from each range of surgery cases (200–300, 300–400, 400–500, 500–600, 600–700, 700–800, 800–900, 900–1,000, 1,000–2,000, 2,000–30,00, 3,000–4,000) where possible. This selection method resulted in the inclusion of 110 centers.
The offices of CACA‐CBCS and CSBS issued a notification about the research project, which was sent to the directors of the selected centers. Five centers were unable to complete the survey and were replaced by five other centers. All the information was gathered from the hospital information system of each center by the participants. The entire survey was web‐based, and all the data were complete by September 7, 2018. The provincial per capita gross domestic products (GDPs) of the survey areas were based on data published by the National Bureau of Statistics in 2016.
Statistical Analysis
The results of the survey were entered into a database. The quality of the data was verified twice: initially via an automatic survey system logic check and then via manual review. The data were then analyzed using R (version 3.5.1; R Development Core Team, Vienna, Austria). The data were analyzed using Pearson's chi‐square test, the likelihood ratio chi‐square test, Fisher's exact test, Welch's two‐sample t test, Kruskal‐Wallis rank sum test, Wilcoxon rank sum test, and Cochran‐Armitage test for trend; the results are presented descriptively. The questionnaire contained several questions regarding the proportion of patients receiving a certain treatment, where the respondent was asked to choose from several ranges of proportions. These results are shown as figures. In addition, for ease of interpretation, an overall proportion is also presented for reference. For each question, this figure was defined as
where A refers to the number of choices, P refers to the midpoint of each range represented by the answer, n refers to the total number of surgery cases of the hospitals that chose this answer, and N refers to the number of respondents to this question.
Results
Hospital Characteristics
The respondent hospitals covered 31 provinces all over the country (Fig. 1); Qinghai, Tibet Autonomous Region, Hong Kong, Macau Special Administrative Region, and Taiwan were not included. Of the respondent hospitals, 97.3% (107/110) were tier 3A hospitals, which classified as the highest level in Chinese health care system; 88.2% (97/110) were academic hospitals, 28.2% (29/110) were cancer hospitals, and 70.9% (81/110) were general hospitals. A total of 85,721 breast cancer surgeries were performed in these hospitals in 2017. Among them, 53 centers (48.2%) performed fewer than 500 breast cancer surgeries, and 24 centers (21.8%) performed more than 1,000 surgeries.
Figure 1.
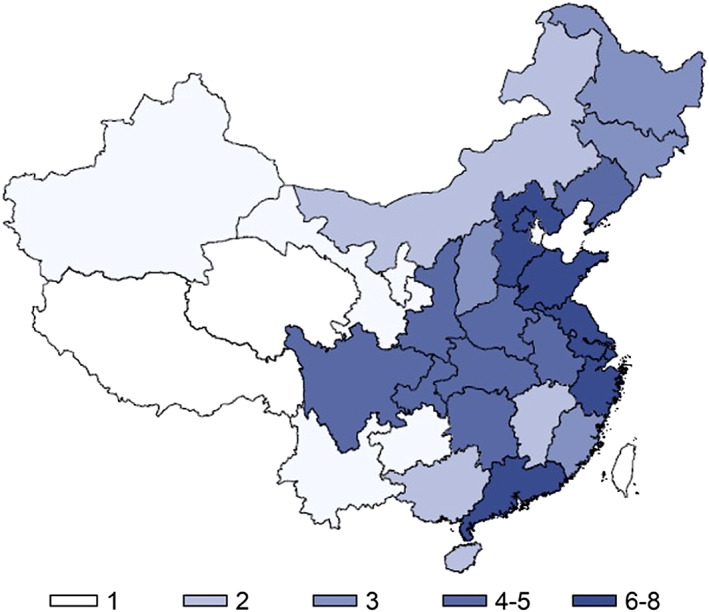
Number of hospitals sampled from each province.
Breast Cancer Surgeries
The overall proportion of BCS performed on account of early‐stage breast cancer was 22%. There was a significantly positive correlation between provincial GDP and the rate of BCS (p = .046). A higher proportion of BCS was performed in academic hospitals than in nonacademic hospitals, but the difference was not statistically significant. Subgroup analyses were carried out according to tumor stage and type of hospital. Compared with nonacademic hospitals, more patients with stage I breast cancer underwent BCS in academic hospitals (p = .029). More BCS procedures were performed at cancer hospitals than at general hospitals for patients with stage II breast cancer (p = .039). The overall rate of BCS after neoadjuvant chemotherapy was quite low. In more than 80% of hospitals surveyed, BCS was performed in fewer than 20% of cases that underwent neoadjuvant chemotherapy (Fig. 2A, B).
Figure 2.
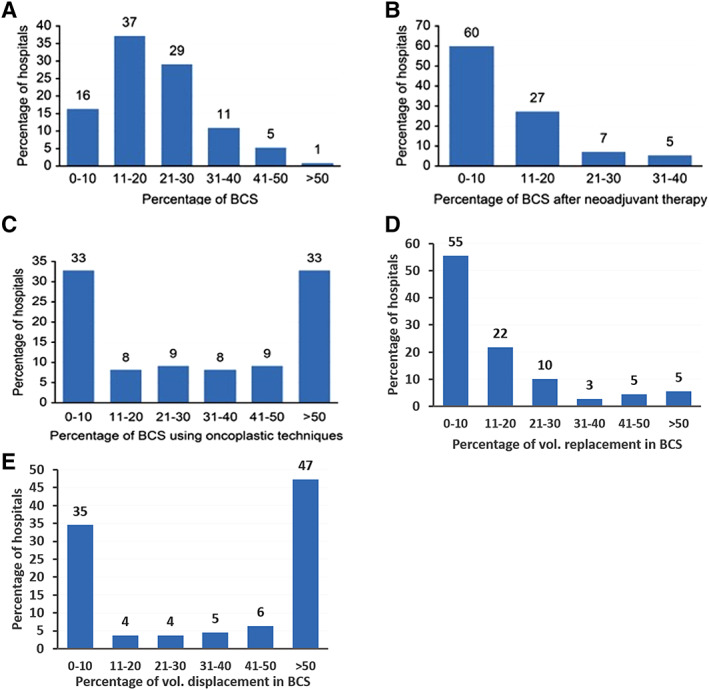
How the respondent hospitals use BCS. (A): Proportion of BCS among all respondent hospitals. (B): Proportion of BCS after neoadjuvant chemotherapy among all respondent hospitals. (C): Proportion of BCS using oncoplastic techniques among all respondent hospitals. (D): Proportion of volume replacement techniques in BCS among all respondent hospitals. (E): Proportion of volume displacement techniques in BCS among all respondent hospitals.
Abbreviation: BCS, breast‐conserving surgery.
Seventy percent of the hospitals did not perform routine cavity shaving during BCS. In the assessment of resection margins, only 25% of hospitals used radial sections perpendicular to the margin, whereas the others used shave sections of the margin. Only 25% of hospitals used “no ink on tumor” as the standard of margin evaluation, whereas others chose intraoperative frozen sections to assess the margin status. Among 70 of the 110 centers surveyed, the reoperation rate after BCS was less than 5%, which indicates that surgeons may perform more extensive resection during BCS in China.
SLNB was performed routinely in 76% of hospitals. Among all hospitals surveyed, only 15% (17/110) used internal mammary SLNB. In 20% (22/110) of hospitals, ALND was omitted for patients with cN0 disease with one or two positive sentinel lymph nodes who underwent BCS, whereas half of the hospitals surveyed still performed ALND in these patients. In contrast, only 4% (4/110) of hospitals accepted omitting ALND during mastectomy. Regarding the choice of tracer agent, most hospitals (62.7%, 69/110) surveyed used methylene blue alone, whereas only 14.5% (16/110) of hospitals used methylene blue and radioisotopes simultaneously. For the intraoperative assessment of sentinel lymph nodes, almost all the hospitals (97%) used frozen sections, and only two hospitals included used intraoperative touch imprint cytology.
There was a great disparity in the proportion of lumpectomy with oncoplastic techniques performed based on the hospital survey. In one third of the hospitals (36/110), the rate of oncoplastic surgery was over 50%. On the other hand, the proportion was less than 10% in another third (35/110) of the hospitals (Fig. 2C). Although there were no statistically significant differences, more oncoplastic breast surgeries were performed in cancer centers than in general hospitals. There was no significant correlation between provincial GDP and the proportion of oncoplastic techniques. The proportion of oncoplastic techniques applied in academic hospitals was higher than that in nonacademic hospitals, but the difference was not statistically significant.
Regarding the different oncoplastic techniques used in BCS, the volume displacement technique was significantly more commonly used than the volume replacement technique (p < .001; Fig. 2D).
Breast Reconstruction Surgery
In total, 96/110 (87.3%) of the centers routinely performed breast reconstruction, and 62% of these standard cooperated with a plastic surgery department. There was no correlation between the proportion of different types of breast reconstruction and the level of the hospital, provincial GDP, or whether the hospital was an academic facility. The overall rate of breast reconstruction was 10.7%, with 65.7% for implant‐based reconstruction, 20.1% for autologous tissue reconstruction, and 14.2% for combination reconstruction (Fig. 3A–C). Regarding the timing of reconstruction, 67.6% of cases underwent immediate reconstruction, and 32.4% underwent delayed surgery.
Figure 3.
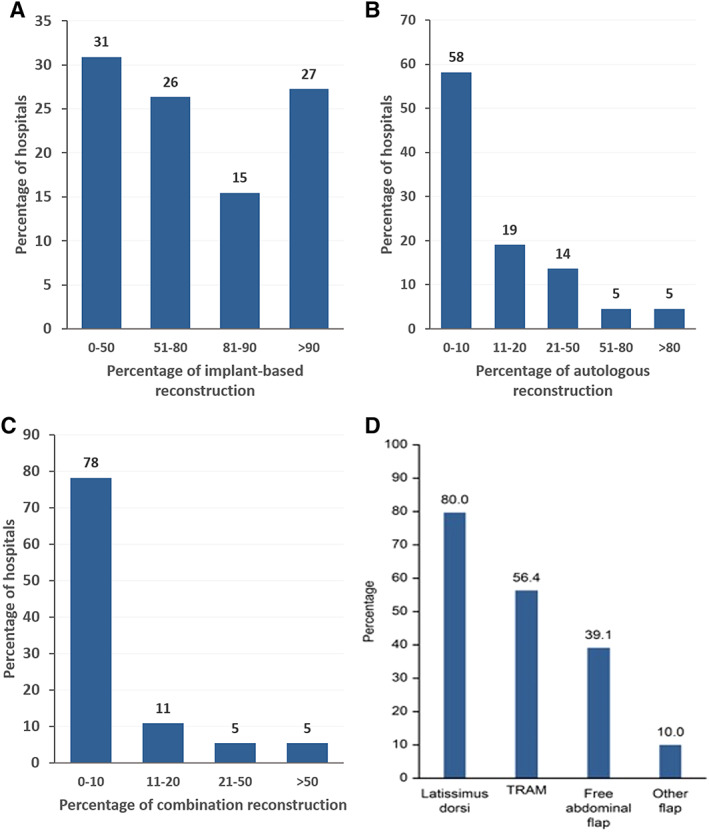
How the respondent hospitals use reconstruction. (A): Proportion of implant‐based reconstruction among all respondent hospitals. (B): Proportion of autologous reconstruction among all respondent hospitals. (C): Proportion of combination reconstruction among all respondent hospitals. (D): Autologous reconstruction rates of four subtypes.
Abbreviation: TRAM, transverse rectus abdominus myocutaneous reconstruction.
Implant‐based reconstruction was the most frequently performed type of reconstructive surgery. Implant‐based reconstruction accounted for more than 80% of all reconstructive operations in 35.5% (39/110) of hospitals that routinely performed reconstruction. However, regarding implant material, approximately 60% of hospitals used acellular dermal matrix or titanized polypropylene mesh.
Autologous breast reconstruction was performed at 91 out of 110 hospitals surveyed. The latissimus dorsi flap was the most commonly used flap in autologous reconstruction (Fig. 3D; 79% of hospitals, 87/110).
However, only 56.4% of hospitals (62/110) had performed transverse rectus abdominis myocutaneous (TRAM) flap reconstruction, and the proportion of TRAM reconstructions among all reconstructions was quite low. The proportion of TRAM reconstructions was over 10% in only 17.8% (11/62) of hospitals that performed TRAM reconstructions. Additionally, the usage rate of abdominal patches in these hospitals was quite polarized. In more than 40% of these hospitals, the usage rate was less than 10%, whereas in another 40%, the usage rate was more than 50%. Finally, free abdominal flaps (including free‐TRAM and deep inferior epigastric artery perforator flap) reconstruction were performed in fewer than half (43/110) of the hospitals surveyed.
Only 65% of the hospitals surveyed conducted a satisfaction evaluation after breast reconstruction, and patients reported outcome measures in fewer than 20% of these. The Breast‐Q was most commonly used to measure patient outcomes, and 90% of hospitals took pictures of patients before and after surgery.
Discussion
This is the first survey on this topic in China that covers such a broad geographic range. The respondent hospitals were chosen from among hospitals that had performed more than 200 breast cancer surgeries in 2017; thus, they have significant local influence and could represent the local level of health care. Because breast reconstruction procedures require highly qualified surgeons who have undergone long periods of training, these operations are often concentrated in large centers; therefore, this is a highly comprehensive survey.
Compared with earlier studies 3, 5, 6, 7, much improvement is apparent in the application of new surgical techniques, including BCS, SLNB, oncoplastic surgery, and breast reconstruction. However, a considerable gap remains between the current situation and that in more developed areas, such as Europe and the U.S. Because breast cancer is diagnosed at later stages 4, a higher proportion of women in China undergo total mastectomy rather than BCS, according to our data. In addition, neoadjuvant chemotherapy has been indicated to minimize surgical damage by increasing the rates of breast conservation. In the National Surgical Adjuvant Breast and Bowel Project Protocol B‐18 trial 8, 59.8% of BCS procedures were performed in the neoadjuvant setting. In our study, more than 80% of hospitals performed BCS after neoadjuvant chemotherapy in fewer than 20% of cases. Additionally, the lack of high‐quality pathology training has limited the development of BCS. Only 25% of hospitals used radial sections perpendicular to the margin and the “no ink on tumor” standard of evaluating margins, which are considered standard methods for evaluating margins in the literature 9, 10. The proportion of reoperations in most hospitals due to positive margins was less than 10%, which is significantly lower than that reported in the literature 11. This shows that the indications for BCS in China are stricter, although it is also possible that breast surgeons are more conservative and that the scope of breast‐conserving resection is wider. Oncoplastic BCS includes two fundamentally different approaches: volume replacement and volume displacement. The former involves partial mastectomy and immediate reconstruction of the breast with the transposition of autologous tissue from elsewhere, whereas the latter involves partial mastectomy and using the remaining breast tissue to fill the defect resulting from extirpation of the tumor 12. The percentage of oncoplastic surgery was over 50% in one third of hospitals. Although over 50% of breast lumpectomies with oncoplastic techniques were performed in 36 (33%) hospitals, fewer than 10% were performed in 35 (32%) hospitals. The “high at both ends, low in the middle” phenomenon indicates that most of oncoplastic surgeries were performed in high‐level hospitals.
SLNB is now the first‐line procedure for axillary evaluation in patients with clinical node‐negative disease. However, the lack of isotope tracers led to the use of the blue dye single tracer method for the routine detection of sentinel lymph nodes, which is less evidence‐based than the dual‐tracer method 13, 14. Most hospitals require intraoperative pathological evaluation 15 to decide whether ALND should be performed.
The overall rate of breast reconstruction in the present study was 10.7%. Another survey 16 conducted in Singapore found that the breast reconstruction rate from 2001 to 2010 was 24.3%. Albornoz et al. 17 reported immediate breast reconstruction trends in the U.S. using the Nationwide Inpatient Sample database from 1998 to 2008. The rate of immediate breast reconstruction increased on average by 5% per year, from 20.8% to 37.8% (p < .01). Most reconstruction surgeries were concentrated in several large centers. The economy remains the primary factor limiting the increased application of breast reconstruction, but the importance of other factors should not be discounted, including physician beliefs, patient education, and multidisciplinary collaboration. In most cities, reconstructive treatment was not covered by insurance. Some patients abandoned immediate reconstruction due to the high price of implants or mesh and concerns about the future cost of systematic therapy. Additionally, in the present study, most reconstruction surgeries were performed by breast surgeons, general surgeons, or oncological surgeons, who had much less access to professional training in reconstructive surgery. Implant‐based reconstruction was the most commonly used type of reconstructive surgery. In addition, the multidisciplinary cooperation model and the lack of a specialist training system have also contributed to the slow development of the breast reconstruction discipline and the vast regional differences. The paucity of areas or hospitals that provide breast reconstruction has further reduced the surgeons’ learning curve because there are fewer reconstruction procedures. This not only limits the development 18 of the technique but also affects the quality of surgical treatments and increases the incidence of complications. Therefore, breast surgeons and plastic surgeons still need to work together so that more patients can benefit from breast reconstruction. Prosthesis‐based reconstruction accounted for more than 80% of all reconstructive operations in 35.5% of hospitals that routinely perform this procedure. The acquisition of different sizes of implants or mesh remains a problem in most hospitals. In addition, the rate of implant use increased by an average of 11% per year (p < .01), surpassing those autologous methods as the leading reconstructive modality after 2002 in the U.S. This may contribute to the increasing rate of bilateral mastectomy. The shape of the breast in Chinese women is significantly different from that in Western countries; therefore, locating the implant product plays an important role 19.
Autologous reconstruction surgeries were performed in a total of 82.7% of hospitals; the absolute number of cases was still quite low compared with the number of mastectomies. The latissimus dorsi flap was the most commonly used flap in 79% of hospitals (87/110). The survey data also showed that very few doctors who perform breast reconstruction value patient‐reported outcome systems, which are a great way to assess the effects of breast reconstruction 20, 21.
The limitations of this survey include responder bias. This survey was mainly conducted among large hospitals and did not represent the overall level of breast cancer care for the entire country. The surgical management of breast cancer in some district‐level hospitals varies greatly in areas where breast reconstruction surgery is rarely performed.
Conclusion
Over 110 centers from most of the provinces in China were investigated in this survey. We provide great insight into the existing surgical practices in China. From the results, the progress that has been achieved is quite obvious, although some problems remain to be solved. The results are of great value for promoting the implementation of a consensus on diagnosis and treatment standards and guidelines for breast cancer and for carrying out the training of breast specialists. The CBCS will also launch a prospective breast cancer surgery data registration project.
Author Contributions
Conception/design: Benlong Yang, Zhimin Shao, Jiong Wu
Provision of study material or patients: Erwei Song, Da Pan, Jing Zhang, Yongsheng Wang, Ning Liao, Jinhai Tang, Xiang Wang, Shude Cui, Feng Jin, Cuizhi Geng, Qiang Sun, Hongyuan Li, Zhimin Fan, Xuchen Cao, Haibo Wang, Shu Wang
Collection and/or assembly of data: Erwei Song, Da Pan, Jing Zhang, Yongsheng Wang, Ning Liao, Jinhai Tang, Xiang Wang, Shude Cui, Feng Jin, Cuizhi Geng, Qiang Sun, Hongyuan Li, Zhimin Fan, Xuchen Cao, Haibo Wang, Shu Wang
Data analysis and interpretation: Benlong Yang, Jiong Wu
Manuscript writing: Benlong Yang
Final approval of manuscript: Benlong Yang, Guosheng Ren, Erwei Song, Da Pan, Jing Zhang, Yongsheng Wang, Ning Liao, Jinhai Tang, Xiang Wang, Shude Cui, Feng Jin, Cuizhi Geng, Qiang Sun, Hongyuan Li, Zhimin Fan, Xuchen Cao, Haibo Wang, Shu Wang, Zhimin Shao, Jiong Wu
Disclosures
The authors indicated no financial relationships.
Supporting information
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1. Supporting Information.
Appendix S2. Supporting Information.
Acknowledgments
We would like to acknowledge the staff members of the Committee of Breast Cancer Society and the Chinese Society of Breast Surgeons working group for participant recruitment and data collection.
This work was supported by the Shenkang Center City Hospital Emerging Frontier Technology Joint Research Project (SHDC12015119) and National Key R&D Program of China (2017YFC1311004).
Disclosures of potential conflicts of interest may be found at the end of this article.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact Commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. Bray F, Ferlay J, Soerjomataram I et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2. Jia‐jian C, Nai‐si H, Jing‐yan X et al. Current status of breast reconstruction in southern China: A 15 year, single institutional experience of 20,551 breast cancer patients. Medicine (Baltimore) 2015;94:e1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Li J, Zhang BN, Fan JH et al. A nation‐wide multicenter 10‐year (1999‐2008) retrospective clinical epidemiological study of female breast cancer in China. BMC Cancer 2011;11:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fan L, Strasser‐Weippl K, Li JJ et al. Breast cancer in China. Lancet Oncol 2014;15:e279–e289. [DOI] [PubMed] [Google Scholar]
- 5. Yuan XM, Wang N, Ouyang T et al. Current status of diagnosis and treatment of primary breast cancer in Beijing, 2008. Chin J Cancer Res 2011;23:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang X, Wang Y. A survey of current surgical treatment of early stage breast cancer in China. Oncoscience 2018;5:239–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sivasubramaniam PG, Zhang BL, Zhang Q et al. Breast cancer disparities: A multicenter comparison of tumor diagnosis, characteristics, and surgical treatment in China and the U.S. The Oncologist 2015;20:1044–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fisher B, Bryant J, Wolmark N et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 1998;16:2672–2685. [DOI] [PubMed] [Google Scholar]
- 9. Hodi Z, Ellis IO, Elston CW et al. Comparison of margin assessment by radial and shave sections in wide local excision specimens for invasive carcinoma of the breast. Histopathology 2010;56:573–580. [DOI] [PubMed] [Google Scholar]
- 10. DeSnyder SM, Hunt KK, Smith BD et al. Assessment of practice patterns following publication of the SSO‐ASTRO consensus guideline on margins for breast‐conserving therapy in stage I and II invasive breast cancer. Ann Surg Oncol 2015;22:3250–3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Havel L, Naik H, Ramirez L et al. Impact of the SSO‐ASTRO margin guideline on rates of re‐excision after lumpectomy for breast cancer: A meta‐analysis. Ann Surg Oncol 2019;26:1238–1244. [DOI] [PubMed] [Google Scholar]
- 12. Noguchi M, Yokoi‐Noguchi M, Ohno Y et al. Oncoplastic breast conserving surgery: Volume replacement vs. volume displacement. Eur J Surg Oncol 2016;42:926–934. [DOI] [PubMed] [Google Scholar]
- 13. Zhang J, Shen K, Nirmal L et al. Lymphoscintigraphy in sentinel lymph node biopsy of breast cancer [in Chinese]. Zhonghua Zhong Liu Za Zhi 2002;24:616–618. [PubMed] [Google Scholar]
- 14. Huang XY, Wu J, Liu ZB et al. Application of methylene blue dye to sentinel lymph node biopsy in breast cancer and its influencing factors [in Chinese]. Ai Zheng 2007;26:1133–1137. [PubMed] [Google Scholar]
- 15. Chen JJ, Yang BL, Zhang JX et al. The evaluation and optimization of intraoperative touch imprint cytology for sentinel lymph nodes in early‐stage breast cancer in China. World J Surg 2010;34:2325–2332. [DOI] [PubMed] [Google Scholar]
- 16. Sim N, Soh S, Ang CH et al. Breast reconstruction rate and profile in a Singapore patient population: A National University Hospital experience. Singapore Med J 2018;59:300–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Albornoz CR, Bach PB, Mehrara BJ et al. A paradigm shift in U.S. breast reconstruction: Increasing implant rates. Plastic Reconstr Surg 2013;131:15–23. [DOI] [PubMed] [Google Scholar]
- 18. Cordeiro PG, McCarthy CM. A single surgeon's 12‐year experience with tissue expander/implant breast reconstruction: Part I. A prospective analysis of early complications. Plastic Reconstr Surg 2006;118:825–831. [DOI] [PubMed] [Google Scholar]
- 19. Parajuly SS, Lan PY, Yan L et al. Breast elastography: A hospital‐based preliminary study in China. Asian Pac J Cancer Prev 2010;11:809–814. [PubMed] [Google Scholar]
- 20. Alderman AK, Wilkins EG, Kim HM et al. Complications in postmastectomy breast reconstruction: Two‐year results of the Michigan Breast Reconstruction Outcome Study. Plastic Reconstr Surg 2002;109:2265–2274. [DOI] [PubMed] [Google Scholar]
- 21. Hu ES, Pusic AL, Waljee JF et al. Patient‐reported aesthetic satisfaction with breast reconstruction during the long‐term survivorship period. Plastic Reconstr Surg 2009;124:1–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1. Supporting Information.
Appendix S2. Supporting Information.


