ABSTRACT
Introduction
The medical treatment facilities (MTF) represent the equivalent of the healthcare system in the home countries, but they face the limitations of an outpost at the end of the supply chain. The capabilities are limited, and the necessary effort to extend the treatment capacity is tremendous.
Algorithms based on scientific evidence or at least profound medical expertise are a tool to facilitate the decision-making process in triage under difficult circumstances. The aim of this article is to present a protocol that regards the specific entities military MTF abroad have to deal with in context of the COVID-19 pandemic.
Material and Methods
To prepare our own health system within the Resolute Support mission, an interdisciplinary team of consultants and nurses located at the multinational role 2E, Camp Marmal, Mazar-e-Sharif, Afghanistan, individually reviewed medical databases and the current literature concerning triage on intensive care units. The identified literature was evaluated by all authors. In the next step, an adapted flow chart for triage on intensive care unit in MTF abroad was set up on the basis of existing triage tools found in the reviewed literature.
Results
The authors created the “Structured Approach for Intensive Care Unit Triage (SAINT)” protocol. It is an approach that fits to the specific entities (e.g., limited medical resources in the whole system, limited intensive care unit capabilities for long-term stay or organ replacement therapy, etc.) that determine the framework of the special military health system abroad.
Conclusions
The presented triage protocol may be a tool for medical personnel to facilitate the difficult task of triaging. It provides guidance along patient-centered criteria like individual medical, ethical, and legal issues while taking into account the available resources. Future studies are needed to investigate the effectiveness of the SAINT protocol.
INTRODUCTION
In military field camps, especially in the deployed setting, soldiers live close together, sharing accommodation, bathrooms, gyms, and dining facilities. Outbreaks of infectious diseases have the potential to easily spread within the population and infect every soldier thereby jeopardizing the mission. Social distancing, as it is defined by the World Health Organization is challenging to achieve and even harder to maintain. Military healthcare providers have multiple roles. In addition to their responsibility to save lives, they must educate the force with regard to the risks of disease, conserve the fighting strength of the force in their area of responsibility, and enable the military leaders to achieve the mission. Compared to the conditions of healthcare providers in the non-deployed setting in their home countries, the situation during deployment has several challenges. The medical treatment facilities (MTF) represent the equivalent of the healthcare system in their home countries, but they are confronted with constraints and limitations because of their positions as outposts at the end of the supply chain. The capabilities are limited and the efforts to extend their capacity require dedication, flexibility, and ingenuity.
Within the area or responsibility (AOR) of the NATO Resolute Support mission in Afghanistan, several ad-hoc task groups focused on different topics related to the COVID-19 pandemic and their impact on the mission. The “COVID-19 strategy group” of the multinational medical task force discussed frequently the dynamic process of the pandemic. These medical experts reassessed the growing evidence on COVID-19 and established a combined joint operations area-wide framework for all medical assets. The aim was to optimize the capabilities of the whole system to face the potential surge of patients if an outbreak of COVID-19 should occur.
The surge of the COVID-19 pandemic has stretched the even well-established health systems in Europe and the USA. Limited resources may lead to the point that medical personnel have to perform triage decisions, a well-known military scenario that was unfamiliar in the civilian setting before the COVID-19 pandemic. Algorithms based on scientific evidence or at least profound medical expertise are tools to facilitate the decision-making process under difficult circumstances like triage, which may result in an end-of-life situation for the individual patient. Assuming a vast number of COVID-19 patients facing limited resources, efforts are made to prepare all MTF in the best possible way.
This article describes the clinical approach of the medical experts at the multinational role 2E at Camp Marmal in Afghanistan to establish an evidence-based triage algorithm for the prioritization of category-A-patients—which means patients that need life-sustaining therapy—when adequate treatment capabilities are limited.
Ethics in medicine is a mandatory component of postgraduate training for residents to become anesthesiologists in Europe. As a result of the regular activity in intensive care units (ICUs) and in palliative medicine, two of the authors often deal with ethical questions in the context of end-of-life decisions.
Although frequently dealing with ethical issues in the daily routine and with common sense, as a result of a limited scientific expertise in this certain field all ethical considerations were extracted out of current literature.
METHODS
Triage situations during the COVID-19 pandemic already occurred in Italy and other countries around the globe. Other health systems are preparing for the surge of COVID-19 patients arriving in the ICUs.
To prepare our own health system within the Resolute Support mission, an interdisciplinary team of physician consultants and nurses located at the multinational role 2E, Camp Marmal, Afghanistan, individually reviewed medical databases (PubMed, EMBASE, and EBSCO Information Services) and the current literature according the rubric “triage on intensive care units” and associated search terms concerning “decision-making,” “ethical aspects,” and “legal considerations.” The process was not structured like a systematic research according PRISMA guidelines because initially the main issue of this process was to collect scientific data to create a tool for our own specific situation. All published data with an immediately available full text were eligible for this work. Every member of the team selected publications (including reviews, original works, editorials, comments/letters to the editor, etc.) that he or she found personally most appropriate. In a second step, our team of medical professionals reviewed the findings of the presented literature in a group approach and ranked it according eligibility to our specific situation.
On the basis of a publication by the German interdisciplinary association for intensive care medicine,1 we discussed necessary changes and created the “Structured Approach for Intensive Care Unit Triage (SAINT)” protocol. It is an approach that takes the specific entities that are determining the framework of the special military health system abroad into account. Such special determinants are, for example, the limited medical capacities in the entire system, which are primarily geared toward short-term care for trauma patients or the need for medical repatriations over thousands of kilometers to relieve the system.
RESULTS
All members of the working group approved the latest and now presented version of this algorithm (Fig. 1).
FIGURE 1.
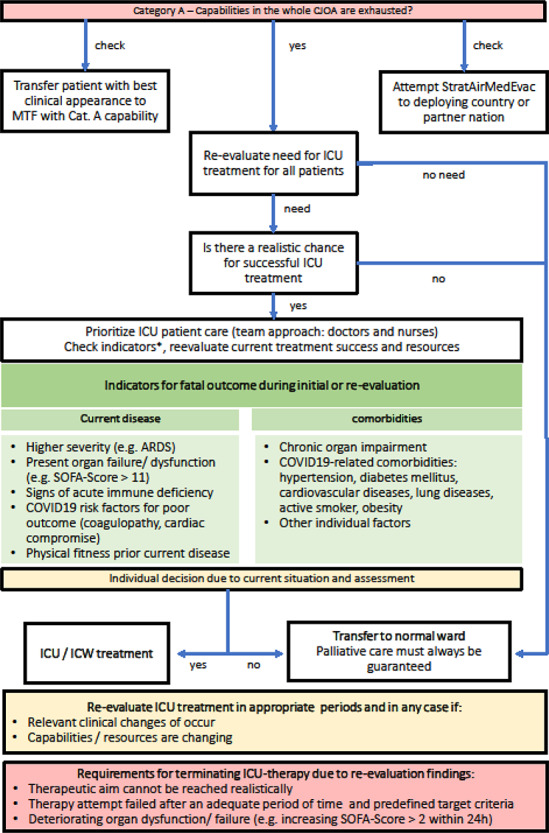
Structured Approach for Intensive Care Unit Triage (SAINT) protocol. CJOA: combined joint operations area, COVID-19: coronavirus disease 2019, ICU/ICW: intensive care unit/ward, SOFA: sequential organ failure assessment, StratAirMedEvac: strategic aeromedical evacuation.
Initially, we presented the protocol to the abovementioned COVID-19 strategy group and want to make it available to a broad audience. We tried to create brief explanations for each step within the algorithm to enable other healthcare providers to follow our rationale.
DISCUSSION
Healthcare professionals are accustomed to make decisions that directly affect the life of other human beings. In a routine setting, these decisions are patient-centered which means that all decisions are strictly focusing on the most appropriate level of care for the individual patient. This includes acute lifesaving interventions or organ replacement therapies as well as the choice to give a patient best supportive care in a palliative setting when other therapies are futile.
The basic requirement for this strategy is the availability of unrestricted intensive care resources. All decisions are made focused on the individual, without comparing the casualty to other patients that might have a better chance for survival.
In times where the ICU capacity (space, personnel, equipment, and supply resources) is exhausted, a need exists to augment this patient-centered approach with a resource-oriented decision. This places it in the operational context of mission focus in the deployed environment.
To further elucidate, this is not a decision weighing one life against another. All human beings are respected as equal and all decisions should be done in an ethical, and of course legal manner.
The resource-oriented decision focuses on the need to optimize the utilization of the available resources to save as many lives as possible—triage. In times of COVID-19 a well-known task from the battlefield is now facing medical personnel as a new challenge.
The first step in the proposed protocol is the re-evaluation of the available resources, not only in the local MTF but as well in other MTF across the entire combined joint, multinational AOR. In our opinion, it is still preferable to optimize capabilities by transferring an acutely ill patient to higher capability MTF if there are still capacities and the patient’s condition (or another patient on the local ICU) is medically stable enough for transportation and has an expected favorable outcome.
Another option is the early initiation of strategic aeromedical evacuation (StratAirMedEvac) out of theater. This option might save available ICU resources but might be unavailable. However, since Germany and the European Air Transport Command had already flown numerous COVID-19 patients from European countries to Germany at this point, we knew that this was logistically possible (e.g., regarding infection control risks or safety of the air crews). Therefore, this option is still one of the main relief factors in case of increased patient numbers for all missions abroad. The same hygiene measures have been established for patient transfer within the AOR and corresponding resources have been planned by the COVID-19 strategy group.
If both options have been exhausted, every patient on the local ICU has to be re-evaluated/re-triaged to determine if they still warrant an ICU level of care.
If the patient’s condition is good enough for normal ward care, an early transfer would save resources. On the other hand, if the patient’s condition is progressively deteriorating or if there is no realistic chance for a successful treatment in an ICU, an early initiation of best supportive palliative care in a normal ward should be done.
The decision that will affect the resilience of medical personnel most is to make a life-or-death choice caused by limited resources. This situation may arise, for example, when patients that need ICU-level care are denied because of lacking resources or to withdraw life-sustaining therapy from one patient to allocate the necessary resource to another patient with an assumed better chance for survival.
For these triage situations, the authors agree that medical expertise and ethics must guide the decisions.
However, just like in trauma, re-triage, re-evaluation, and prioritization should be done as a team and that this team should find a consensus for the result of this process. We assume that this may lead to a better resilience of the involved personnel. Truog et al. described a system using a triage team consisting from respected members of the peer group that are volunteering for this task and who are not directly involved in patient care.2 In smaller MTF, this concept is not feasible secondary to the small medical footprint. Using a team approach not only augments the capability but enables medical personnel to share the burden with support elements.
Considering all factors, the triage system helps to assume the predicted outcome of each individual.
For example, organ failure or dysfunction might be a limiting factor of ICU therapy in MTF abroad. The lack of organ replacement therapy capabilities can become crucial for the patient’s outcome.
A further aspect inherent to the decision-making process should be the course over the last 24 to 48 hours of the patient’s stay in ICU rigorously evaluated in 24-hour increments. If necessary therapeutic aims cannot be reached realistically, an attempt to address a certain problem failed because predefined criteria were not met, or the patient is deteriorating although receiving maximum intensive care resources for the last 24 hours, an early termination of further ICU care is reasonable and appropriate in situations of limited resources.
The authors disagree with the proposal of Cheung et al. to end life-sustainment therapy after a predefined period (e.g., 7 days) in ICU without regarding the individual’s course as key aspect of a dynamic process.3
Scoring systems like the SOFA-score, STSS, or NEWS4,5,6 are a good method to assess the patient’s situation, especially when done in a serial sequence to highlight progress or deterioration. But they should not be used as single criterion to justify the decision to start, continue, or withdraw intensive care treatment.3,7
From the ethical point of view, priority for limited resources should aim both at saving the most lives and at maximizing improvements in individuals’ post-treatment length of life. Saving more lives and more years of life is a consensus value across expert reports.8
Nevertheless, there will arise circumstances were two or more patients who are judged as equal in a medical and ethical way compete for limited resources. Withholding, for example, a ventilator will result usually in the death of the affected patient.
In this specific situation, an operationalized random allocation could be performed.8
The individual need for ICU treatment should be re-evaluated in appropriate periods and every time, when there are significant changes either in the availability of ICU resources or in the patient’s medical situation.
One reason to stop ICU therapy is not mentioned in the provided flow chart: the patient’s decision to reject ICU treatment. It is one of the most common reasons to end therapy.1
In the military setting, especially during deployments, we are dealing with a majority of young and healthy soldiers. A written patient directive is often not available, nor are there surrogates that could claim it. That’s why in our point of view this aspect seems not to be appropriate in this protocol.
For further deep dive into the topic, we suggest the recently published detailed guideline for triage of scarce critical care resources by Maves et al. The authors describe in detail operational steps for implementation of a triage system in hospitals and give guidance for ethical implications during triage. Furthermore, they provide a concept for different levels of triage depending on the degree of demand in relation to system capacity.9
CONCLUSION
The COVID-19 pandemic is a huge challenge for civilian and military health systems around the globe.
The triage algorithm presented may be a tool for medical personnel to facilitate the difficult task of triaging. It provides guidance along patient-centered criteria while regarding the available resources. Knowing that in the end always the responsible medical leader must be responsible for the decisions that have been made, the team approach should help to share the burden and relieve the individual’s conflict between ethical considerations, medical needs, and the operational setting.
We also want to encourage every healthcare provider to think about and discuss all considerations we stated. Dealing in advance with all implications such a situation might bring may increase the personal resilience level.
ACKNOWLEDGMENTS
None.
Contributor Information
CDR Dr Christoph Jänig, Role 2E, MN MedCoy TAAC N, Mazar-e-Sharif, Afghanistan; Department for Anesthesiology and Intensive Care Medicine, Bundeswehr Central Hospital, 56072 Koblenz, Germany.
LCOL Dr Roger Forklage, Role 2E, MN MedCoy TAAC N, Mazar-e-Sharif, Afghanistan; Department for Anesthesiology, Pain Medicine and Palliative Care, Elisabeth-TweeSteden Ziekenhuis, 5042 AD Tilburg, The Netherlands.
COL Dr Jennifer M Gurney, NATO Role 2E Commander, Kabul, Afghanistan; Department for Trauma Surgery, RadboudUMC, Nijmegen, 6525 GA, The Netherlands.
MAJ Robin Groth, Role 2E, MN MedCoy TAAC N, Mazar-e-Sharif, Afghanistan; Department for Anesthesiology and Intensive Care Medicine, Bundeswehr Central Hospital, 56072 Koblenz, Germany.
SGM Christine Wirth, Role 2E, MN MedCoy TAAC N, Mazar-e-Sharif, Afghanistan; Department for Anesthesiology and Intensive Care Medicine, Bundeswehr Central Hospital, 56072 Koblenz, Germany.
COL Dr Hendrik van de Krol, Role 2E, MN MedCoy TAAC N, Mazar-e-Sharif, Afghanistan; Department for Trauma Surgery, RadboudUMC, Nijmegen, 6525 GA, The Netherlands.
COL Willi Schmidbauer, Department for Anesthesiology and Intensive Care Medicine, Bundeswehr Central Hospital, 56072 Koblenz, Germany.
COL Dr Christoph Güsgen, Role 2E, MN MedCoy TAAC N, Mazar-e-Sharif, Afghanistan; Department for General, Visceral and Thoracic Surgery, Bundeswehr Central Hospital, 56072 Koblenz, Germany.
FUNDING
None.
CONFLICT OF INTEREST
None declared.
SUPPORT SOURCES
None.
REFERENCES
- 1. Jochen Dutzmann DIVI, Hartog C, Janssens U. et al. : Entscheidungen über die Zuteilung von Ressourcen in der Notfall- und der Intensivmedizin im Kontext der COVID-19-Pandemie. Published online: March26, 2020. https://www.divi.de/empfehlungen/publikationen/covid-19/1540-covid-19-ethik-empfehlung-v2/file; accessed April 08, 2020.
- 2. Truog RD, Mitchell C, Daley GQ: The toughest triage—allocating ventilators in a pandemic. N Engl J Med 2020. doi: 10.1056/NEJMp2005689 [DOI] [PubMed] [Google Scholar]
- 3. Cheung W, Myburgh J, Seppelt IM: Development and evaluation of an influenza pandemic intensive care unit triage protocol. Crit Care Resusc 2012; 14: 185-90. [PubMed] [Google Scholar]
- 4. Vincent JL, Moreno J, Takala J, et al. : The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 1996; 22: 707-10. [DOI] [PubMed] [Google Scholar]
- 5. Adeniji KA, Cusack R: The Simple Triage Scoring System (STSS) successfully predicts mortality and critical care resource utilization in H1N1 pandemic flu: a retrospective analysis. Critical Care 2011; 15: R39. doi: 10.1186/cc10001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smith GB, Prytherch DR, Meredith P, et al. : The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death resuscitation. Resuscitation 2013; 84(4): 465-70. doi: 10.1016/j.resuscitation.2012.12.016 [DOI] [PubMed] [Google Scholar]
- 7. Nates JL, Nunally M, Kleinpell R, et al. : ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med 2016; 44: 1553-602. [DOI] [PubMed] [Google Scholar]
- 8. Emanuel EJ, Persad G, Upshur R, et al. : Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020; 382: 2049-55. doi: 10.1056/NEJMsb2005114 [DOI] [PubMed] [Google Scholar]
- 9. Maves RC, Downar J, Dichter JR, et al. : Triage of scarce critical care resources in COVID-19: an implementation guide for regional allocation. Chest 2020; 158: P212-25. doi: 10.1016/j.chest.2020.03.063 [DOI] [PMC free article] [PubMed] [Google Scholar]


