Rheumatology key message
Neutrophilic arterial vasculitis in COVID-19 represents a novel finding and could be responsible for thrombotic complications.
Sir, Thrombosis in patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection represents the most relevant extra-pulmonary manifestation of COVID-19 and recognizes a multifactorial pathogenesis [1]. Cases of SARS-CoV-2 disease (COVID-19)-related vasculitis are reported in the literature [2–9] and this could represent a possible alternative mechanism of arterial thrombosis secondary to inflammation in COVID-19. Herein, we report the first case of neutrophilic arterial vasculitis in COVID-19.
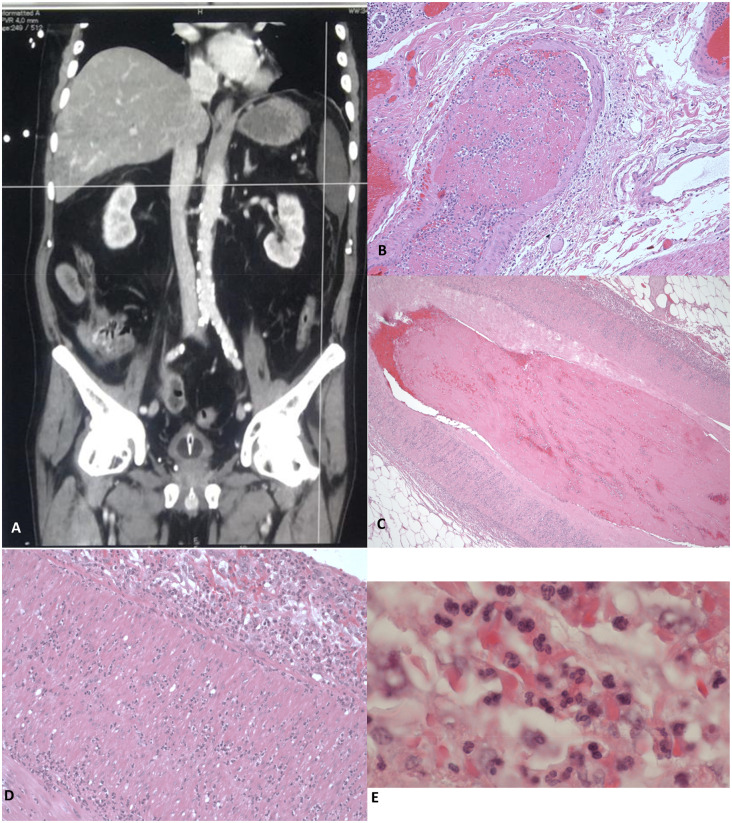
A 73-year–old man with a past history of type II diabetes, chronic kidney disease (CKD) and ischaemic coronary disease was admitted to the University Hospital of Modena for shortness of breath and dry cough. Oro-rhino-pharyngeal swab was positive for SARS-CoV-2 and radiological findings showed interstitial pneumonia. At admission, he had abdominal pain, decompensated ketoacidosis, and acute on CKD (stage 3 b) although he had no respiratory failure (PaO2/FiO2 = 341 mmHg). He received antithrombotic prophylaxis with low-molecular-weight heparin (LMWH) (4000 U once a day) and continued previous therapy with acetylsalicylic acid (100 mg once a day). Laboratory exams revealed elevated CRP (48 mg/dl) and D-dimer (6910 ng/ml) with normal prothrombin time and activated partial thromboplastin time. The Sequential Organ Failure Assessment (SOFA) score was 2. Antiphospholipid antibodies were not detected. The following day he presented an acute abdomen. Angio-CT showed arterial multifocal thrombosis with total occlusion involving coeliac tripod and superior mesenteric artery with splenic and distal ileum infarction (Fig. 1A). He underwent splenectomy and resection of the ischaemic bowel loop. Two days after surgery, he was discharged from the Intensive Care Unit. He has never been subjected to mechanical ventilation. His post-surgery course was characterized by a second episode of diabetic decompensation, intra-abdominal infection and acute exacerbation of CKD requiring temporary haemodialysis. Sixteen days after the first test, oro-rhino-pharyngeal swab for SARS-CoV-2 turned negative. Sixty days after admission, the patient is still hospitalized. Surgical complications led to prolonged hospitalization due to nosocomial infections that necessitated specific treatment, such as central venous catheter-related candidemia and infection of a sacral decubitus plaque. Then, in consideration of the patient’s frailty, he underwent a careful and prolonged rehabilitation programme.
Fig. 1.
Arterial and venous thrombotic complications and neutrophilic vasculitis in splenic artery
(A) Thrombosis of the coeliac tripod immediately after its origin, extended to ∼15 mm. The superior mesenteric artery presents thrombosis as well as some of its branches. Almost complete infarction of an ileal segment and spleen. (B–E) All anatomic specimens were fixed in 4% neutral buffered formaldehyde and, after paraffin embedding, 3 micra thick sections were cut and routinely stained with haematoxylin and eosin (HE). (B) Venous vessel of the splenic hilum with fibrin thrombus in the lumen. HE, ×100 (original magnification). (C) Wall of the splenic artery with fibrin thrombus in the lumen and granulocytic infiltration. HE, ×100 (original magnification). (D) High magnification of the splenic artery showing transmural infiltration of neutrophils, from adventitia (top) to intima (bottom left). HE, ×200 (original magnification). (E) Diffuse infiltration of neutrophilic granulocytes in the arterial wall. HE, ×1000 (original magnification).
Histopathological findings confirmed mesenteric and splenic thrombosis with a large splenic infarction. In the splenic hilar area, thrombotic material was observed in the lumen of venous (Fig. 1B) and arterial blood vessels (Fig. 1C). The arterial wall showed transmural necrosis with massive infiltration of neutrophils, mainly in the adventitia and media, the intima being less affected (Fig. 1D and E), providing a histopathological diagnosis of neutrophilic vasculitis. Veins were not involved in the vasculitic process. SARS-CoV-2 was not detected by PCR performed on a paraffinized splenic artery wall specimen.
As the patient’s clinical condition significantly improved after surgery, no immunosuppressive therapy was initiated, despite the detection of arterial vasculitis.
This complex case scenario and the potential related clinical implications required multidisciplinary discussion among haematologist, rheumatologist, pneumologist and nephrologist. Herein, we report the main issues addressed by each specialist.
The haematologic perspective: thrombosis related to inflammation is described both in systemic inflammatory response syndrome and in decompensated ketoacidosis [10]. Recent evidence suggests that patients with severe COVID‐19 often meet sepsis‐induced coagulopathy criteria and may benefit from anticoagulant therapy [10].
The rheumatologist perspective: histopathological findings of arterial thrombosis in the splenic hilum (Fig. 1C–E) appear to be related to a neutrophilic vasculitis process. These findings share similarities with those described in the acute stage of polyarteritis nodosa (PAN), a medium-sized vessel vasculitis [11] that recognizes an immune-pathogenetic mechanism sometimes associated with viral infections. Similarly to PAN, this patient presented gastrointestinal and splenic involvement with ischaemic complications. However, his clinical condition improved without immunosuppressive treatment while he was using anticoagulant therapy similar to that indicated in thrombotic complications of PAN [12].
The pneumologist perspective: in patients with COVID-19, lung involvement is sustained by direct viral infection alongside cytokine-driven endothelial damage that enhances local inflammation and promotes pulmonary vascular micro-thrombosis [13]. Given these premises, pulmonary vasculitis may enhance lung damage, increasing interstitial involvement with significant deterioration of lung elastance without affecting compliance [13]. The low amount of non-aerated tissue justifies the low recruitability, mimicking the mechanical model of interstitial lung disorders [14–16] and explaining the presence of shortness of breath on admission despite lack of respiratory failure or significant parenchymal involvement. Moreover, pulmonary vasculitis might extend the loss of hypoxic vasoconstriction, preventing the compensation mechanism of vascular redistribution in inhomogeneous lungs, with further dysregulation of alveolar micro-perfusion and increased risk of micro-thrombosis15.
The nephrologist perspective: The patient presented severe acute kidney injury (AKI) requiring renal replacement therapy in the context of diabetes-related CKD. The differential diagnosis of AKI in a setting of systemic vasculitis included ‘kidney vasculitis’ and acute tubular necrosis.
Widespread inflammation of the medium-sized vessels is a potential, albeit rare, cause of rapidly progressive renal failure. Fibrinoid necrosis of the arterial wall may involve smaller vessels such as interlobar and arcuate arteries resulting in AKI due to glomerular hypoperfusion and tubular necrosis [17]. Conversely, the abrupt decline of renal function after major abdominal surgery suggested tubular necrosis as a potential cause of kidney failure. Pre-existent chronic kidney injury, diabetes, prolonged surgical time and concomitant use of contrast media were recognized risk factors responsible for developing AKI. Although the partial recovery of kidney function without immunosuppressive therapy may suggest pre-renal status and nephrotoxicity as aetiology of kidney injury, we cannot exclude the possibility that resolution of the viral infection attenuated the immune response and led to a partial improvement of renal function. In the absence of renal biopsy, the aetiology of AKI remains elusive.
The multidisciplinary perspective presented above elucidates a very novel and significant disease pathophysiology in the context of COVID-19.
Norsa et al. described the case of a 62-year-old man presenting a picture of small bowel ischaemia, thromboembolic filling defects in inferior vena cava and superior mesenteric vein. The patient was tested for SARS-CoV-2 and was found negative in nasopharyngeal swab and bronco-alveolar lavage. The histological examination on the resected small bowel showed complete ischaemic necrosis of the mucosal layer and acute perivisceral inflammation; the mesenteric vessel was characterized by complete recent thrombosis and mixed inflammatory infiltration of arterial and venous vessels mainly involving the endothelium [9]. On the contrary, we observed a vasculitic involvement constituted by neutrophilic infiltration of adventitia and media.
Furthermore, the authors detected a SARS-CoV-2 trough in situ hybridization in a resected ischaemic small bowel, suggesting a direct viral role in the ischaemic process. In our case, the lack of the detection of SARS-CoV-2 could be due to a low sensitivity of RT-PCR compared with RNA in situ hybridization or to a real absence of the virus in the examined specimens, allowing us to speculate that the viral infection could represent a trigger for a cascade of systemic inflammatory-mediated events [18].
The main limitation in this analysis is related to a scarce availability of diagnostic procedures. Furthermore, data available do not permit an estimation of the size effect of COVID-19 neutrophilic vasculitis on the overall burden of thrombotic complication, as the CT scan also shows severe atheromatosis, which can worsen the complex clinical picture of our patient.
Based on the hypothesis of a relationship between SARS-CoV-2 infection and our PAN-like disorder, treatment with a short course of glucocorticoids and/or plasma exchange could represent a therapeutic option as had been observed by Guillevin et al. in HBsAg-related PAN [19, 20]. However, the patient was not treated with glucocorticoids and/or traditional immunosuppressive treatment because there was a spontaneous improvement with supportive treatment.
In conclusion, it is conceivable to attribute a leading role to anticoagulant treatments in the management of COVID-19. Nevertheless, while primary LMWH may be effective in the prevention of endothelial activation-induced thrombosis, this might not be the case when thrombotic phenomena are secondary to vasculitis, which could benefit from immunosuppressive therapy.
Acknowledgements
C.V., M.Mes., J.M., R.T., G.A., M.Ma., S.V., M.F., G.F., G.C., E.B., M.T., A.R., M.Men., E.F., G.C., G.O., A.S., M.D., C.P., F.C., A.B., A.C., I.C., G.L., N.D., G.M., G.R., R.G., A.M., M.G., M.T.M., C.M., C.S., G.G. were in charge of the case. A.M. described pathohistological findings. C.V., C.M., C.S., G.G., M.Ma., G.A., R.T. conceptualized and designed the manuscript and contributed with an expert opinion. C.V., J.M., G.G., R.T. wrote and revised the manuscript. G.G., C.M., C.S. did the supervision of the final version of the manuscript. All the authors contributed to discussion and revised the manuscript.
Funding: No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this manuscript.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1. Klok FA, Kruip MJHA, van der Meer NJM. et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;10:145–147. S0049-3848(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Castelnovo L, Capelli F, Tamburello A, Faggioli PM, Mazzone A. Symmetric cutaneous vasculitis in COVID-19 pneumonia. J Eur Acad Dermatol Venereol 2020;34:e362-e363 doi: 10.1111/jdv.16589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Roncati L, Ligabue G, Fabbiani L. et al. Type 3 hypersensitivity in COVID-19 vasculitis. Clin Immunol 2020;217:108487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bouaziz JD, Duong T, Jachiet M. et al. Vascular skin symptoms in COVID-19: a French observational study. J Eur Acad Dermatol Venereol 2020;27. doi: 10.1111/jdv.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mayor-Ibarguren A, Feito-Rodriguez M, Quintana Castanedo L. et al. Cutaneous small vessel vasculitis secondary to COVID-19 infection: a case report. J Eur Acad Dermatol Venereol 2020;22. doi: 10.1111/jdv.16670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dominguez-Santas M, Diaz-Guimaraens B, Garcia Abellas P, Moreno-Garcia Del Real C, Burgos-Blasco P, Suarez-Valle A. Cutaneous small-vessel vasculitis associated with novel 2019 coronavirus SARS-CoV-2 infection (COVID-19). J Eur Acad Dermatol Venereol 2020;26. doi: 10.1111/jdv.16663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Perosanz-Lobo D, Fernandez-Nieto D, Burgos-Blasco P. et al. Urticarial vasculitis in COVID-19 infection: a vasculopathy-related symptom? J Eur Acad Dermatol Venereol 2020;8. doi: 10.1111/jdv.16713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Papa A, Salzano AM, Di Dato MT, Varrassi G. Images in practice: painful cutaneous vasculitis in a SARS-Cov-2 IgG-positive child. Pain Ther 2020;21:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Norsa L, Valle C, Morotti D. et al. Intestinal ischemia in the COVID-19 era. Dig Liver Dis 2020. [Published online ahead of print, 2020 Jun 9]. doi: 10.1016/j.dld.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carl GF, Hoffman WH, Passmore GG. et al. Diabetic ketoacidosis promotes a prothrombotic state. Endocr Res 2003;29:73–82. [DOI] [PubMed] [Google Scholar]
- 11. Karadag O, Jayne DJ. Polyarteritis nodosa revisited: a review of historical approaches, subphenotypes and a research agenda. Clin Exp Rheumatol 2018;36(Suppl):135–42. [PubMed] [Google Scholar]
- 12. Sontichai W, Natesirinilkul R, Pruksachatkun C, Katanyuwong K. Childhood polyarteritis nodosa presenting with symmetric digital gangrene and hyperesthesia. J Clin Rheumatol 2018;24:99–102. [DOI] [PubMed] [Google Scholar]
- 13. Wang T, Du Z, Zhu F. et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet 2020;395:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chang JC. Acute respiratory distress syndrome as an organ phenotype of vascular microthrombotic disease: based on hemostatic theory and endothelial molecular pathogenesis. Clin Appl Thromb Hemost 2019;25:107602961988743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gattinoni L, Chiumello D, Caironi P. et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 2020;46:1099–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Marchioni A, Tonelli R, Rossi G. et al. Ventilatory support and mechanical properties of the fibrotic lung acting as a ‘squishy ball’. Ann Intensive Care 2020;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yokota K, Inoue T, Akiyama Y. et al. Acute kidney injury in a patient with polyarteritis nodosa and multiple myeloma. Intern Med 2014;53:263–7. [DOI] [PubMed] [Google Scholar]
- 18. Smatti MK, Cyprian FS, Nasrallah GK. et al. Viruses and autoimmunity: a review on the potential interaction and molecular mechanisms. Viruses 2019;11:762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guillevin L, Lhote F. Treatment of polyarteritis nodosa and Churg-Strauss syndrome: indications of plasma exchanges. Transfus Sci 1994;15:371–88. [DOI] [PubMed] [Google Scholar]
- 20. Trepo C, Guillevin L. Polyarteritis nodosa and extrahepatic manifestations of HBV infection: the case against autoimmune intervention in pathogenesis. J Autoimmun 2001;16:269–74. [DOI] [PubMed] [Google Scholar]