Abstract
Background:
There are few studies of patient-facing decision aids that include supportive kidney care as an option. We tested the efficacy of a video decision aid on knowledge of supportive kidney care among older patients with advanced chronic kidney disease.
Methods:
Participants (age ≥ 65 years with advanced chronic kidney disease) were randomized to receive verbal or video education. Primary outcome was knowledge of supportive kidney care (score range 0–3). Secondary outcomes included preference for supportive kidney care, and satisfaction and acceptability of the video.
Results:
Among all participants (n=100), knowledge of supportive kidney care increased significantly after receiving education (p < 0.01); however, there was no difference between study arms (p = 0.68). There was no difference in preference for supportive kidney care between study arms (p = 0.49). In adjusted analyses, total health literacy score (aOR 1.08 [95% CI, 1.003 – 1.165]) and nephrologists’ answer of “No” to the Surprise Question (aOR 4.87 [95% CI, 1.22–19.43]) were associated with preference for supportive kidney care. Most felt comfortable watching the video (96%), felt the content was helpful (96%) and would recommend the video to others (96%).
Conclusions:
Among older patients with advanced chronic kidney disease, we did not detect a significant difference between an educational verbal script and video decision aid in improving knowledge of supportive kidney care or preferences. However, patients who received video education reported high satisfaction and acceptability ratings. Future research will determine the effectiveness of a supportive kidney care video decision aid on real-world patient outcomes.
Trial registration:
Keywords: Chronic kidney disease, dialysis decision-making, supportive kidney care, palliative nephrology
Introduction
The proportion of older patients with chronic kidney disease (CKD) continues to increase in the United States. Indeed, in the past decade, the prevalence of CKD has grown from 9.2% to 14.5% among Medicare beneficiaries.[1] Furthermore, among those with more advanced disease in this population, nearly 20% will progress to end-stage renal disease (ESRD) within 5 years.[2] Treatment options for patients with ESRD include renal transplantation, hemodialysis, peritoneal dialysis and uncommonly, supportive kidney care. For older and frail patients for whom transplant is not an option, dialysis may not improve health-related quality of life or result in a significant increase in survival compared to those who receive medical management of kidney disease.[3–6] Supportive kidney care includes non-dialytic medical therapy focused on treatment of fluid balance, anemia, blood pressure, nutrition, in addition to other physical and emotional symptoms.[7] As supportive kidney care allows people to maintain their quality of life and achieve quality end-of-life care, it is a reasonable treatment option for older and frail patients with advanced CKD.[8–10]
Patients with advanced CKD and their caregivers desire patient-centered information regarding their ESRD treatment options but supportive kidney care is often not discussed.[11–13] Also, there is limited evidence about how best to inform patients about non-dialytic treatments and pre-dialysis education program processes vary widely.[14–19] Educational video decision aids have been studied in randomized controlled trials (RCT) to better promote informed decision-making among patients with kidney disease, dementia, heart failure and cancer, however none have included supportive kidney care.[20–23] Thus, we conducted an RCT to test preliminary efficacy of a video decision aid on supportive kidney care knowledge and preferences among older patients with advanced CKD.
Methods
Trial Design
We performed this prospective two parallel-arm RCT among patients with advanced CKD in Boston, Massachusetts and Philadelphia, PA. We calculated that 50 participants per arm would achieve 85% power to detect a 0.5 standard deviation of change in supportive kidney care knowledge after receiving education.[24],[25] Although the video featured older adults, study enrollment was initially open to include all adult patients (≥ 18 years) to achieve enrollment targets more rapidly. However, the protocol was subsequently changed to limit enrollment to older participants in line with suitability of the educational content. Participants were randomized in a 1:1 fashion to receive either video or verbal education about hemodialysis, peritoneal dialysis, and supportive kidney care. One of the study investigators (N.D.E) generated random numbers by computer and concealed these in envelopes. Study coordinators produced allocation results immediately before receiving education. Participants were enrolled between July 2016 and March 2019. This study is registered at ClinicalTrials.gov (NCT02698722) and was approved by the Institutional Review Boards at Partners Healthcare and The University of Pennsylvania. Reporting was done in accordance with the CONSORT statement for randomized controlled trials.[26]
Settings and Participants
Study participants were recruited from nephrology clinics associated with Massachusetts General Hospital and The University of Pennsylvania. Inclusion criteria identified in the patient’s electronic medical record included: age ≥ 65, advanced CKD (as defined by the Chronic Kidney Disease Epidemiology Collaboration[27] estimated glomerular filtration rate < 30), and English-speaking. Patients were ineligible if they had a documented history of dementia, had a documented history of legal blindness, or were active on a kidney transplantation waitlist. For patients who met the inclusion criteria, primary nephrologists confirmed study eligibility and appropriateness with the study coordinators. The study coordinators then approached potential participants at the beginning or end of their clinic appointment. If interested in the study, the study coordinators obtained written informed consent. Enrolled participants who were deemed to have severe cognitive deficit (as determined by eight or more errors on the Short Portable Mental Status Questionnaire[28]) were withdrawn from the study. All study procedures were conducted in a private room in the nephrology clinic.
Video education (Intervention)
An 11.5-minute video script was developed in an iterative process by a national panel of nephrologists with an expertise in shared-decision making in the CKD population. The video included images of older patients undergoing hemodialysis as well as patients doing peritoneal dialysis. For supportive kidney care, images of patients filmed in their home and clinic settings were used. The visual scenes were filmed without the use of prompts or stage directions to convey a candid realism in the style known as cinéma vérité.[29, 30] All filming and editing were performed by a research team member (A.E.V.). All patients who were included in the video gave informed consent to be filmed, and no actors or special effects were used.
Verbal education (Control)
Similar to previously published RCT’s of video decision aids, a short script was developed based on the script used for the video.[31, 21] The language used in the script was written to target a low health literacy audience. Study coordinators read the script aloud to each participant.
Outcome measures
The primary outcome was participants’ knowledge of supportive kidney care. A 1-item survey was used to ascertain knowledge about supportive kidney care and featured three correct answers. Each correct response contributed one point. Incorrect or “I don’t know” responses contributed no points. Knowledge scores ranged from 0–3 (eTable 1).
Secondary outcomes included participant preference for supportive kidney care if their kidney disease worsened to end-stage renal disease (one item) as well as satisfaction (one item) and acceptability (three items) ratings for participants who received video education (see Supplement). Study coordinators administered all surveys pre-randomization and immediately post-education to each participant.
Other measures
We ascertained participant demographic information (age, sex, race, ethnicity, education level, and income level) via interviewer-assisted surveys. Health literacy was measured using the Rapid Estimate of Adult Literacy in Medicine (REALM) which has been used widely among patients with CKD and ESRD.[32–35] A score of ≤ 60 is consistent with inadequate health literacy. We performed medical chart review to ascertain comorbidities to calculate a Charlson Comorbidity Index score for each participant.[36] Lastly, the participant’s nephrologist was asked two questions: 1) “Have you referred your patient for pre-dialysis education?”, and 2) “Would you be surprised if this patient died in the next one year?” (also known as the Surprise Question)[37]. We included these two items to better understand participants’ views of supportive kidney care and to also identify those with limited prognoses who might benefit from this treatment.
Statistical analyses
All analyses were performed using SAS version 9.4 (SAS Institute, Inc. Cary, NC). All participant characteristics and outcomes were described using proportions for categorical variables and means (± standard deviations) or medians (interquartile range) for continuous variables depending on their distribution. Participant characteristics were summarized and then stratified by those who received verbal script education versus those who received video education.
Mean knowledge scores, the proportion of participants who achieved correct knowledge of all three supportive kidney care items (yes/no) and the proportion of participants who indicated preference for supportive kidney care (yes/no) were tabulated before and after receiving education. We compared overall post-intervention knowledge scores with pre-intervention knowledge scores using paired t-tests and binary outcomes between the study arms using Fisher’s exact test. We used McNemar’s statistic to summarize agreement, or the effect of education on the outcome, for each study arm. Multivariable logistic regression analyses were performed to identify independent association of participant characteristics (age, sex, race, ethnicity, income level, educational level, Charlson comorbidity score, and health literacy), physician characteristics (referral pre-dialysis education, answer to the Surprise Question) and educational arm with correct knowledge and preference for supportive kidney care. Odds ratios with 95% confidence intervals were calculated as the measure of association. Variables were checked for collinearity. Significance was determined at a two-sided alpha level of 0.05.
Results
Baseline characteristics
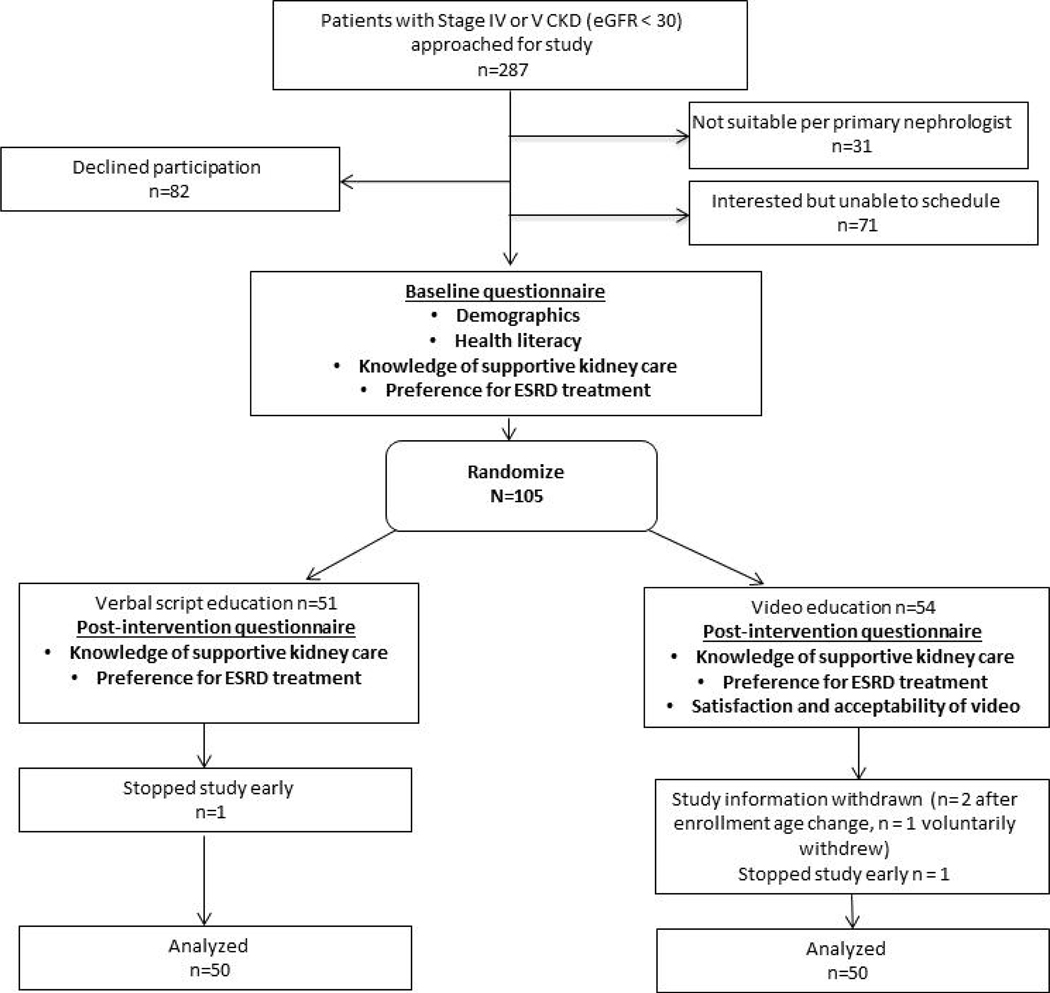
Two hundred and eighty-seven eligible patients were approached for study participation during their nephrology clinic visit (Figure 1). Of these, 31 were not suitable for enrollment as determined by their primary nephrologist, 82 declined to participate, and 71 were interested but could not be enrolled due to the logistics of arranging and completing study procedures. Two participants consented but did not wish to complete the study. Three participants’ study information were withdrawn (two after study enrollment age changed to ≥ 65 and one voluntarily). We continued to recruit to achieve our enrollment target and a total of 100 participants provided information for final study analyses.
Figure 1.
Study Schema
The median age of all participants was 75 years [interquartile range: 70, 81] and the majority of participants were male (51%), of White race (66%) and of Non-Hispanic ethnicity (97%) (Table 1). Thirty-eight percent of patients had an annual income of less than $30,000, 15% had not completed a high school education and 32% had limited health literacy. Median Charlson Comorbidity Index score was 7 [interquartile range: 6, 8]. Only 22% of nephrologists had referred their patients for formal pre-dialysis education at the time of enrollment. Additionally, 23% of nephrologists responded “No” to the Surprise Question. There was a higher proportion of male participants in the verbal arm (64% vs. 38%) and a higher proportion of participants who had been referred for standard pre-dialysis education in the video arm (32% vs. 12%).
Table 1.
Baseline characteristics
| Variable | Total (N= 100) | Verbal Script (N = 50) | Video (N = 50) |
|---|---|---|---|
| Median age, years [interquartile range] | 75 [70, 81] | 75 [70,81] | 76 [70, 81] |
| Male gender (%) | 51 (51) | 32 (64) | 19 (38) |
| Race (%) | |||
| White | 66 (66) | 35 (70) | 31 (62) |
| Black | 31 (31) | 14 (28) | 17 (34) |
| Asian | 1 (1) | 0 | 1 (2) |
| Other | 2 (2) | 1 (2) | 1 (2) |
| Non-Hispanic ethnicity | 97 (97) | 49 (98) | 48 (96) |
| Education (% < high school) | 15 (15) | 4 (8) | 11 (22) |
| Income (% < 30k) | 38 (38) | 16 (32) | 22 (44) |
| Limited health literacy (% ≤ 60 on REALM) | 32 (32) | 14 (28) | 18 (36) |
| Median Charlson Comorbidity Index score [interquartile range] | 7 [6,8] | 7 [6,8] | 7 [6,8] |
| Nephrologist referred for pre-dialysis education (%) | 22 (22) | 6 (12) | 16 (32) |
| Surprise question (% nephrologists that answered no) | 23 (23) | 9 (18) | 14 (28) |
Knowledge of supportive kidney care
Prior to receiving education, all participants achieved a mean knowledge score of 2.02 (SD ± 0.96) and 41% of participants had correct knowledge of supportive kidney care at baseline (Table 2). There was no significant difference in baseline knowledge score (mean score, verbal arm vs. video arm: 1.94 (SD ± 1.02) vs. 2.1 (SD ± 0.91), p = 0.41), or proportion of those with correct knowledge (verbal arm vs. video arm: 38% vs 44%, p = 0.68, Table 2).
Table 2.
| Total (N= 100) | Verbal Script (N = 50) | Video (N = 50) | P-value | |
|---|---|---|---|---|
| Pre-education | ||||
| Mean supportive kidney care knowledge score (± SD) | 2.02 (± 0.96) | 1.94 (± 1.02) | 2.1 (± 0.91) | 0.41 |
| Correct knowledge of supportive care (%) | 41 | 38 | 44 | 0.68 |
| Preference for supportive care (%) | 21 | 26 | 16 | 0.33 |
| Post-education | ||||
| Mean supportive kidney care knowledge score (± SD) | 2.36 (± 0.93) | 2.38 (± 0.90) | 2.34 (± 0.91) | 0.83 |
| Correct knowledge of supportive care (%) | 61 | 58 | 64 | 0.68 |
| Preference for supportive care (%) | 26 | 30 | 22 | 0.49 |
Post-education knowledge McNemar’s test: Overall – 13.33, p < 0.01; Verbal – 7.14, p = 0.01; Video – 6.25, p = 0.01
Post-education preference McNemar’s test: Overall – 2.27, p = 0.13; Verbal – 0.67, p = 0.41; Video – 1.80, p = 0.18
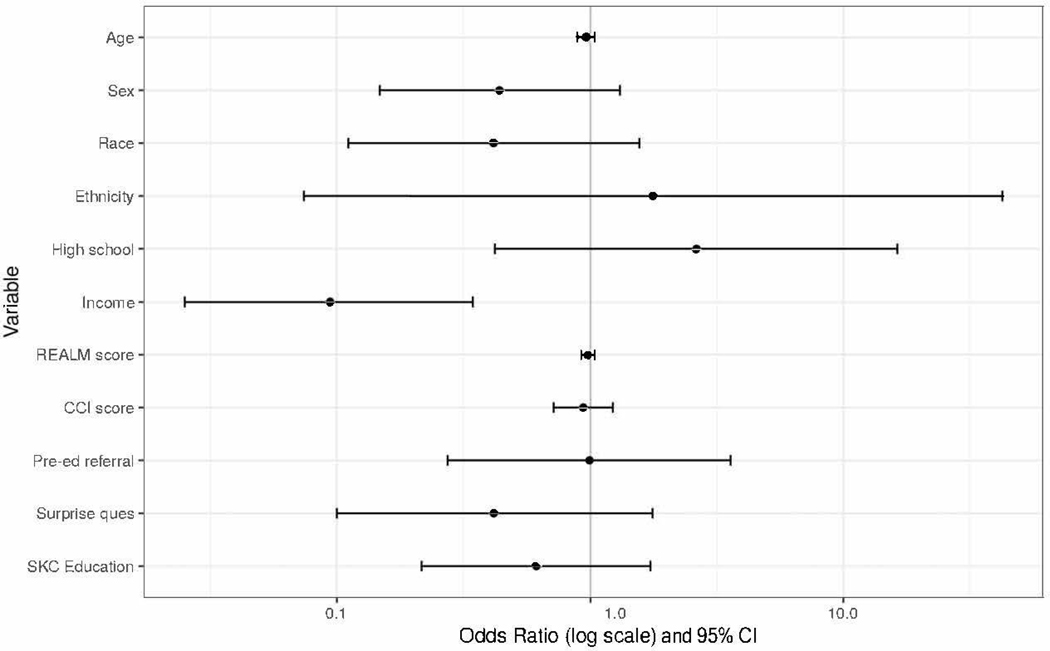
After receiving education, mean knowledge scores increased significantly (overall 2.36 [± SD 0.93], p < 0.01) although there was no difference in post-education knowledge scores between the study arms (verbal arm vs. video arm: 2.38 [SD ± 0.90] vs. 2.34 [SD ± 0.91], p = 0.83, Table 2). Furthermore, 61% of participants had significantly greater knowledge of supportive kidney care (McNemar’s statistic = 13.33, p < 0.01) and the effect of education was similar among participants in the verbal (McNemar’s statistic = 7.14, p = 0.01) and video arms (McNemar’s statistic = 6.25, p = 0.01). On multivariable analyses, an income of less than $30,000 was significantly associated with lower odds of correct knowledge of supportive kidney care (aOR 0.10 [95% CI, 0.03–0.35], Figure 2).
Figure 2. Factors Associated with Correct Supportive Care Knowledge*.
*Patients of Asian or Other race (n=3) removed from analyses due to cells with no preference for supportive kidney care.
Variables: Sex = Male vs. Female; Race = White vs. Black; Ethnicity = Non-Hispanic vs Hispanic; High school = Greater than 12th grade education vs. Less than 12th grade education; Income = Income ≤ 30k vs. > 30k; REALM score = REALM score; CCI score = Charlson Comorbidity Index Score; Pre-ed referral = Have you referred your patient for pre-dialysis education? (yes vs. no); Surprise ques = Would you be surprised if your patient died in the next one year? (no vs. yes); SKC (Supportive kidney care) education = Verbal script vs. Video.
Preference for supportive kidney care
At baseline, 21% of participants preferred supportive kidney care if their disease progressed to ESRD. There was no significant difference in preference for supportive kidney care between the two study arms (verbal arm vs. video arm: 26% vs. 16%, p = 0.33, Table 2).
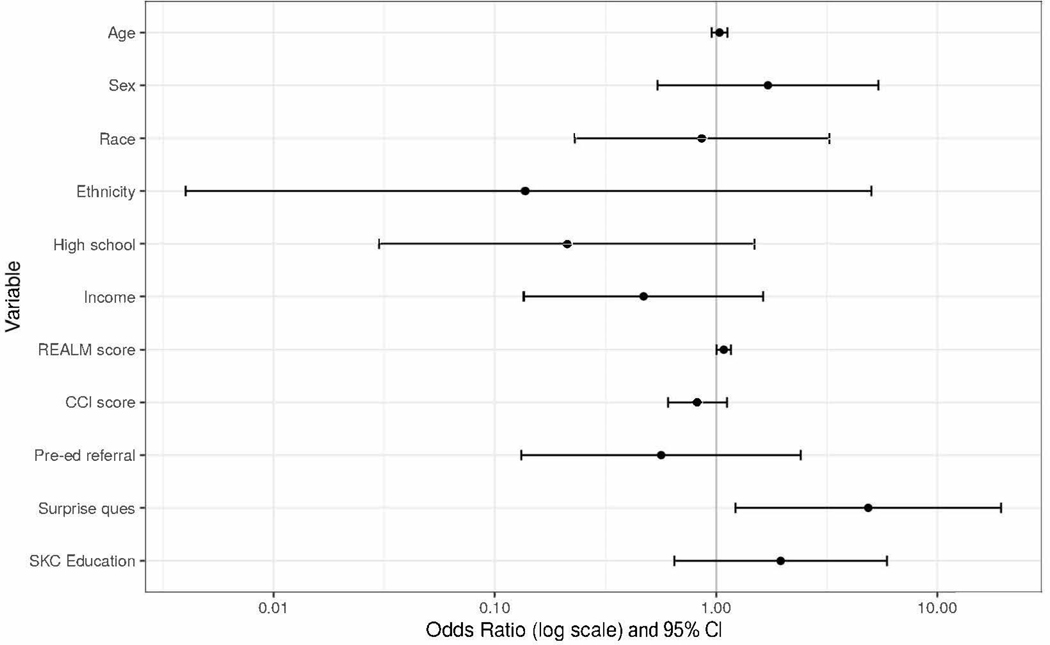
After receiving education, 26% of participants preferred supportive kidney care; however, this was not significantly different compared to baseline (overall McNemar’s statistic = 2.27, p = 0.13; verbal arm McNemar’s statistic = 0.67, p = 0.41; video arm McNemar’s statistic = 1.80, p = 0.18, Table 2). In addition, there was no difference in the proportion of participants who preferred supportive kidney care between the verbal and video arms (p = 0.49, Table 2). On multivariable analyses, total health literacy score and nephrologists’ answer of “No” to the Surprise Question were significantly associated with higher odds of preference for supportive kidney care treatment. (Health literacy aOR 1.08 [95% CI, 1.003 – 1.17]; Surprise Question aOR 4.87 [95% CI, 1.23–19.43], Figure 3).
Figure 3. Factors Associated with Preference for Supportive Kidney Care*.
*Patients of Asian or Other race (n=3) removed from analyses due to cells with no preference for supportive kidney care.
Variables: Sex = Male vs. Female; Race = White vs. Black; Ethnicity = Non-Hispanic vs Hispanic; High school = Greater than 12th grade education vs. Less than 12th grade education; Income = Income ≤ 30k vs. > 30k; REALM score = REALM score; CCI score = Charlson Comorbidity Index Score; Pre-ed referral = Have you referred your patient for pre-dialysis education? (yes vs. no); Surprise ques = Would you be surprised if your patient died in the next one year? (no vs. yes); SKC (Supportive kidney care) education = Verbal script vs. Video.
Satisfaction and acceptability
Of participants who viewed the video, 96% found it to be helpful, 96% felt comfortable while watching, 98% felt satisfied with the content, and 96% would recommend the video to others (e Table 2).
Discussion
Among older participants with advanced CKD, we found knowledge of supportive kidney care increased significantly after receiving verbal and video education. However, we did not detect a significant difference between the two educational arms. Additionally, participants who had lower income were less likely to have correct knowledge of supportive kidney care. Preferences for supportive kidney care did not change post-education due to receiving education; however, health literacy score and nephrologists’ answer to the Surprise Question were significantly associated with patient preference for this type of care. Lastly, among participants who received video education, the majority reported high satisfaction and acceptability ratings.
Our results demonstrate the impact of a supportive kidney care video decision aid on improving knowledge of this treatment among older patients with advanced CKD. Although the clinical relevance of change in knowledge score in this study is unknown, we were reasonably able to demonstrate that enrolled participants had lower baseline knowledge about supportive kidney care. This confirms previous literature that shows routine care for advanced CKD likely does not include adequate information about this treatment. Our results align with published data from a qualitative study of older patients in the United Kingdom that showed patients who were managed in nephrology clinics without established supportive kidney care pathways were less likely to have knowledge of this option.[11] In contrast, patients who were managed with supportive kidney care not only had a good understanding of how their livelihood could be affected by dialysis, but also how supportive kidney care was not fixed and courses of future treatment could indeed include dialysis as desired. Given time constraints during clinical encounters, a short supportive kidney care video decision aid may be used before or after visits to improve knowledge and facilitate subsequent care discussions.
Shared-decision making for ESRD treatments should encompass conversations between clinicians, patients and caregivers about the risk and benefits of both dialytic and non-dialytic treatments in the context of a patient’s goals and values.[38] However, despite longstanding advocacy for supportive kidney care among national and international nephrology organizations, educational tools that inform patients and their loved ones are limited and fewer have established efficacy on objective knowledge.[39, 40, 14, 17, 19] We also demonstrated that a supportive kidney video decision aid was well received among our study cohort which counters historic beliefs among clinicians that speaking about non-dialytic treatments may cause unintended psychological harm towards patients.[41] In this context, patients and their loved ones may feel more empowered to discuss their hopes, worries and fears with their clinicians and how these may best be integrated into future care plans.
Participants in our study largely endorsed preference for dialytic care if their kidney disease were to progress – even after receiving education about supportive kidney care. This finding was not unexpected given that we did not assess participants’ prognostic awareness, which is strongly associated with future preference for care.[42] Although knowledge of treatment options is essential to decision-making, readiness to make decisions and discussion of treatment options with clinicians are also significant factors.[25] Consistent with these notions, we found that physicians’ answer to the Surprise Question was strongly associated with participants’ preference for supportive kidney care. This may have reflected previous prognostic and goals of care discussions between participants and their clinicians during clinical encounters. Recent studies have shown that the Surprise Question may be useful in helping clinicians identify poor prognoses and functional statuses as well as frailty among older patients with advanced CKD.[43, 37, 44] We also found that higher health literacy was associated with preference for supportive kidney care which reinforces the importance of clear communication and dialogue between clinicians and patients to better assist them in navigating their health decisions.[45] Health literacy has been associated with advance care planning – an important consideration for older patients with advanced chronic kidney disease.[46–48] Further investigation is warranted to ascertain whether the addition of an educational supportive kidney care video decision aid in clinical practice can influence patient-centered outcomes including advance care planning and preferences for care.
Our study has several limitations. Study coordinators who collected study data were not blinded to randomization and this may have introduced bias. The cross-sectional nature of this study did not allow longitudinal follow-up to assess participant retention of knowledge or change in preference of care. As our primary outcome was proximal knowledge, we also did not assess other important decision-making outcomes including decisional conflict and confidence. Further, we cannot comment on generalizability of results among patients living in different regions, patients of different socioeconomic statuses, younger patients, or patients with different stages of kidney disease including those receiving dialysis. We also did not ascertain participants’ previous conversations about supportive kidney care with clinicians and were unable to control for these in the analyses. Lastly, there are no validated knowledge surveys about supportive kidney care; therefore, we used a question that was largely developed from literature review and expert opinion. This survey item may have caused a ceiling effect which resulted in a lack of demonstrated efficacy of the video decision aid.
To the best of our knowledge, this study represents the first pilot randomized trial of a video decision aid on knowledge of supportive kidney care. The landscape of care for older and frail patients with advanced chronic kidney disease has changed to prioritize shared decision-making, quality of life, and better transitions of care at the end of life.[49–51] Our trial demonstrated that knowledge of supportive kidney care improved significantly among participants regardless of the educational intervention - this only enriches shared decision-making. Rigorous development and testing of patient-facing decision aids are crucial to achieving high quality care for this patient population. Video decision aids offer an innovative and scalable tool to empower patients and families in shared decision-making that includes supportive kidney care.
Supplementary Material
Acknowledgements:
We thank Dr. Ravi Thadhani who provided research coordinator support for this project.
Statement of Ethics: All participants provided written informed consent. This study was approved by the Institutional Review Boards at Partners Healthcare and The University of Pennsylvania.
Funding: NDE is supported by NIH grant K23DK114526. The funder did not have a role in study design, collection, analyses, interpretation of data, writing the report, and the decision to submit the report for publication.
Footnotes
Disclosure Statement: Dr. Volandes has a financial interest in the nonprofit foundation Nous Foundation (d/b/a ACP Decisions, 501c3). The nonprofit organization develops advanced care planning video decision aids and support tools. Dr. Volandes’ interests were reviewed and are managed by Massachusetts General Hospital and Partners HealthCare in accordance with their conflict of interest policies. All other authors declare that they have no relevant conflict of interests.
Data sharing: De-identified data from this project are available to qualified researchers for approved scientific use immediately following publication for up to 3 years. Data access proposals that are methodologically sound should be directed to the corresponding author.
References
- 1.Saran R, Robinson B, Abbott KC, Bragg-Gresham J, Chen X, Gipson D, et al. US Renal Data System 2019 Annual Data Report: Epidemiology of Kidney Disease in the United States. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2020. January;75(1s1):A6–a7. [DOI] [PubMed] [Google Scholar]
- 2.Saran R, Robinson B, Abbott KC, Agodoa LYC, Bragg-Gresham J, Balkrishnan R, et al. US Renal Data System 2018 Annual Data Report: Epidemiology of Kidney Disease in the United States. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2019. March;73(3s1):A7–a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rouveure AC, Bonnefoy M, Laville M. [Conservative treatment, hemodialysis or peritoneal dialysis for elderly patients: The choice of treatment does not influence the survival]. Nephrologie & therapeutique. 2016. February;12(1):32–7. [DOI] [PubMed] [Google Scholar]
- 4.Verberne WR, Geers AB, Jellema WT, Vincent HH, van Delden JJ, Bos WJ. Comparative Survival among Older Adults with Advanced Kidney Disease Managed Conservatively Versus with Dialysis. Clinical journal of the American Society of Nephrology : CJASN. 2016. April 7;11(4):633–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raman M, Middleton RJ, Kalra PA, Green D. Outcomes in dialysis versus conservative care for older patients: A prospective cohort analysis of stage 5 Chronic Kidney Disease. PloS one. 2018;13(10):e0206469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Loon IN, Goto NA, Boereboom FTJ, Verhaar MC, Bots ML, Hamaker ME. Quality of life after the initiation of dialysis or maximal conservative management in elderly patients: a longitudinal analysis of the Geriatric assessment in OLder patients starting Dialysis (GOLD) study. BMC nephrology. 2019. March 29;20(1):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Connor NR, Kumar P. Conservative management of end-stage renal disease without dialysis: a systematic review. Journal of palliative medicine. 2012. February;15(2):228–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong SPY, Yu MK, Green PK, Liu CF, Hebert PL, O’Hare AM. End-of-Life Care for Patients With Advanced Kidney Disease in the US Veterans Affairs Health Care System, 2000–2011. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2018. July;72(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubio Rubio MV, Lou Arnal LM, Gimeno Orna JA, Munguia Navarro P, Gutierrez-Dalmau A, Lamban Ibor E, et al. Survival and quality of life in elderly patients in conservative management. Nefrologia : publicacion oficial de la Sociedad Espanola Nefrologia. 2019. Mar-Apr;39(2):141–50. [DOI] [PubMed] [Google Scholar]
- 10.Saeed F, Adams H, Epstein RM. Matters of Life and Death: Why Do Older Patients Choose Conservative Management? American journal of nephrology. 2020;51(1):35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tonkin-Crine S, Okamoto I, Leydon GM, Murtagh FE, Farrington K, Caskey F, et al. Understanding by older patients of dialysis and conservative management for chronic kidney failure. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2015. March;65(3):443–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karlin J, Chesla CA, Grubbs V. Dialysis or Death: A Qualitative Study of Older Patients’ and Their Families’ Understanding of Kidney Failure Treatment Options in a US Public Hospital Setting. Kidney Medicine. 2019;1(3):124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Selman LE, Bristowe K, Higginson IJ, Murtagh FEM. The views and experiences of older people with conservatively managed renal failure: a qualitative study of communication, information and decision-making. BMC nephrology. 2019. February 4;20(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fortnum D, Grennan K, Smolonogov T. End-stage kidney disease patient evaluation of the Australian ‘My Kidneys, My Choice’ decision aid. Clinical kidney journal. 2015. August;8(4):469–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Isnard Bagnis C, Crepaldi C, Dean J, Goovaerts T, Melander S, Nilsson EL, et al. Quality standards for predialysis education: results from a consensus conference. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2015. July;30(7):1058–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roderick P, Rayner H, Tonkin-Crine S, Okamoto I, Eyles C, Leydon G, et al. Health Services and Delivery Research. A national study of practice patterns in UK renal units in the use of dialysis and conservative kidney management to treat people aged 75 years and over with chronic kidney failure Southampton (UK): NIHR Journals Library Copyright (c) Queen’s Printer and Controller of HMSO; 2015. This work was produced by Roderick et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.; 2015. [Google Scholar]
- 17.Winterbottom AE, Gavaruzzi T, Mooney A, Wilkie M, Davies SJ, Crane D, et al. Patient Acceptability of the Yorkshire Dialysis Decision Aid (YoDDA) Booklet: A Prospective Non-Randomized Comparison Study Across 6 Predialysis Services. Perit Dial Int. 2016. Jul-Aug;36(4):374–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis JL, Davison SN. Hard choices, better outcomes: a review of shared decision-making and patient decision aids around dialysis initiation and conservative kidney management. Current opinion in nephrology and hypertension. 2017. May;26(3):205–13. [DOI] [PubMed] [Google Scholar]
- 19.Subramanian L, Zhao J, Zee J, Knaus M, Fagerlin A, Perry E, et al. Use of a Decision Aid for Patients Considering Peritoneal Dialysis and In-Center Hemodialysis: A Randomized Controlled Trial. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2019. September;74(3):351–60. [DOI] [PubMed] [Google Scholar]
- 20.Stacey D, Legare F, Col NF, Bennett CL, Barry MJ, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;1:Cd001431. [DOI] [PubMed] [Google Scholar]
- 21.El-Jawahri A, Mitchell SL, Paasche-Orlow MK, Temel JS, Jackson VA, Rutledge RR, et al. A Randomized Controlled Trial of a CPR and Intubation Video Decision Support Tool for Hospitalized Patients. Journal of general internal medicine. 2015. August;30(8):1071–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitchell SL, Shaffer ML, Cohen S, Hanson LC, Habtemariam D, Volandes AE. An Advance Care Planning Video Decision Support Tool for Nursing Home Residents With Advanced Dementia: A Cluster Randomized Clinical Trial. JAMA internal medicine. 2018. July 1;178(7):961–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waterman AD, Peipert JD, McSorley AM, Goalby CJ, Beaumont JL, Peace L. Direct Delivery of Kidney Transplant Education to Black and Low-Income Patients Receiving Dialysis: A Randomized Controlled Trial. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2019. November;74(5):640–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003. May;41(5):582–92. [DOI] [PubMed] [Google Scholar]
- 25.Prakash S, McGrail A, Lewis SA, Schold J, Lawless ME, Sehgal AR, et al. Behavioral stage of change and dialysis decision-making. Clinical journal of the American Society of Nephrology : CJASN. 2015. February 6;10(2):197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ (Clinical research ed). 2010. March 23;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine. 2009. May 5;150(9):604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975. October;23(10):433–41. [DOI] [PubMed] [Google Scholar]
- 29.Grant BK SJ. Documenting the documentary: close readings of documentary film and video. Detroit, MI, Wayne Stage University Press; 1998. [Google Scholar]
- 30.Volandes AE, Barry MJ, Wood F, Elwyn G. Audio-video decision support for patients: the documentary genre as a basis for decision aids. Health Expect. 2013. September;16(3):e80–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Epstein AS, Volandes AE, Chen LY, Gary KA, Li Y, Agre P, et al. A randomized controlled trial of a cardiopulmonary resuscitation video in advance care planning for progressive pancreas and hepatobiliary cancer patients. Journal of palliative medicine. 2013. June;16(6):623–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993. June;25(6):391–5. [PubMed] [Google Scholar]
- 33.Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, Wallston KA, et al. Low health literacy associates with increased mortality in ESRD. Journal of the American Society of Nephrology : JASN. 2010. November;21(11):1979–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright JA, Wallston KA, Elasy TA, Ikizler TA, Cavanaugh KL. Development and results of a kidney disease knowledge survey given to patients with CKD. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2011. March;57(3):387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cavanaugh KL, Osborn CY, Tentori F, Rothman RL, Ikizler TA, Wallston KA. Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clinical kidney journal. 2015. August;8(4):462–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 37.Baddour NA, Robinson-Cohen C, Lipworth L, Bian A, Stewart TG, Jhamb M, et al. The Surprise Question and Self-Rated Health Are Useful Screens for Frailty and Disability in Older Adults with Chronic Kidney Disease. Journal of palliative medicine. 2019. December;22(12):1522–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li KC, Brown MA. Consenting for Dialysis or Its Alternative: Systematic Process Is Needed. Clinical journal of the American Society of Nephrology : CJASN. 2020. February 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moss AH. Revised dialysis clinical practice guideline promotes more informed decision-making. Clinical journal of the American Society of Nephrology : CJASN. 2010. December;5(12):2380–3. [DOI] [PubMed] [Google Scholar]
- 40.Davison SN, Levin A, Moss AH, Jha V, Brown EA, Brennan F, et al. Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney international. 2015. September;88(3):447–59. [DOI] [PubMed] [Google Scholar]
- 41.Ladin K, Pandya R, Kannam A, Loke R, Oskoui T, Perrone RD, et al. Discussing Conservative Management With Older Patients With CKD: An Interview Study of Nephrologists. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2018. May;71(5):627–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wachterman MW, Marcantonio ER, Davis RB, Cohen RA, Waikar SS, Phillips RS, et al. Relationship between the prognostic expectations of seriously ill patients undergoing hemodialysis and their nephrologists. JAMA internal medicine. 2013. July 8;173(13):1206–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Salat H, Javier A, Siew ED, Figueroa R, Lipworth L, Kabagambe E, et al. Nephrology Provider Prognostic Perceptions and Care Delivered to Older Adults with Advanced Kidney Disease. Clinical journal of the American Society of Nephrology : CJASN. 2017. November 7;12(11):1762–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schmidt RJ, Landry DL, Cohen L, Moss AH, Dalton C, Nathanson BH, et al. Derivation and validation of a prognostic model to predict mortality in patients with advanced chronic kidney disease. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2019. September 1;34(9):1517–25. [DOI] [PubMed] [Google Scholar]
- 45.Cassidy BP, Harwood L, Getchell LE, Smith M, Sibbald SL, Moist LM. Educational Support Around Dialysis Modality Decision Making in Patients With Chronic Kidney Disease: Qualitative Study. Canadian journal of kidney health and disease. 2018;5:2054358118803323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Waite KR, Federman AD, McCarthy DM, Sudore R, Curtis LM, Baker DW, et al. Literacy and race as risk factors for low rates of advance directives in older adults. Journal of the American Geriatrics Society. 2013. March;61(3):403–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ladin K, Buttafarro K, Hahn E, Koch-Weser S, Weiner DE. “End-of-Life Care? I’m not Going to Worry About That Yet.” Health Literacy Gaps and End-of-Life Planning Among Elderly Dialysis Patients. The Gerontologist. 2018. March 19;58(2):290–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nouri SS, Barnes DE, Volow AM, McMahan RD, Kushel M, Jin C, et al. Health Literacy Matters More Than Experience for Advance Care Planning Knowledge Among Older Adults. Journal of the American Geriatrics Society. 2019. October;67(10):2151–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.O’Hare AM, Richards C, Szarka J, McFarland LV, Showalter W, Vig EK, et al. Emotional Impact of Illness and Care on Patients with Advanced Kidney Disease. Clinical journal of the American Society of Nephrology : CJASN. 2018. July 6;13(7):1022–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wong SPY, McFarland LV, Liu CF, Laundry RJ, Hebert PL, O’Hare AM. Care Practices for Patients With Advanced Kidney Disease Who Forgo Maintenance Dialysis. JAMA internal medicine. 2019. January 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong SPY, Boyapati S, Engelberg RA, Thorsteinsdottir B, Taylor JS, O’Hare AM. Experiences of US Nephrologists in the Delivery of Conservative Care to Patients With Advanced Kidney Disease: A National Qualitative Study. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2020. February;75(2):167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.