Abstract
Background
Aim of the present study was to assess if the presence of high cardiovascular risk, left ventricle systolic dysfunction or elevated BNP or Troponin are able to independently predict the outcome of patients with known cardiac disease and COVID-19 pneumonia.
Methods and results
From March 7th to April 28th, forty consecutive patients with known cardiac disease (chronic coronary artery disease, n=38; atrial fibrillation, n = 7; valvular disease, n = 13) referred to our emergency department for symptoms of suspected COVID-19, laboratory diagnosis of COVID-19 and typical signs of viral pneumonia at chest CT were enrolled in the study. The only predictor of the composite end-point (all cause of death + invasive ventilation + thromboembolic event) was the lung involvement % at chest CT (OR: 1.06; 95%CI: 1.01–1.11, P = 0.02). In the multivariate analysis, the lung involvement % at chest CT was the only independent predictor of the composite end-point (OR: 1.06; 95%CI: 1.01–1.11, P = 0.034).
Conclusions
The extent of lung involvement by COVID-19 is the only independent predictor of adverse outcome of patients and is predominant over the severity of cardiac disease.
Keywords: Covid-19, non-contrast CT scan, lung disease, cardiovascular disease
Highlights
-
•
Severity of cardiac disease is not an independent predictor of adverse outcome in COVID-19 pneumonia
-
•
The extent of lung involvement is an independent predictor of adverse outcome
-
•
CT scan could be useful in patients with COVID-19 and cardiovascular co-morbidities
1. Introduction
Lombardy is a region of northern Italy with one of the higher prevalence worldwide of coronavirus disease 2019 (COVID-19) associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [1,2]. Since the first case diagnosed on February 20, 2020, the infection has rapidly spread throughout Lombardy, reaching 80,089 confirmed cases, with 14,745 deaths and a peak of more than 1500 patients admitted in intensive care unit as of May 7, 2020. Our hospital, Centro Cardiologico Monzino, is the largest center completely dedicated to cardiovascular disease in Italy. For this reason, Monzino was designed since March 8, 2020 from the regional government as Hub center for cardiovascular emergencies. A high proportion of COVID-19 patients have comorbidities and early studies from China showed a history of cardiac disease in 15–40% and laboratory signs of cardiac injury in 10–30% of them, associated with a more severe clinical course [3,4]. Recently, a study from another large center in Lombardy showed that hospitalized COVID-19 patients with concomitant cardiac disease have a poor prognosis compared with subjects without a history of cardiac disease, with higher mortality and thrombo-embolic events [5]. However, the influence of cardiac disease severity on prognosis of patients with COVID-19 pneumonia remains uncleared.
2. Aim of the study
Aim of the present study was to assess if the presence of high cardiovascular risk (presence of more than 2 cardiovascular risk factors), left ventricle systolic dysfunction or elevated BNP or Troponin are able to independently predict the outcome of patients with known cardiac disease and COVID-19 pneumonia.
3. Materials and methods
From March 7th to April 28th, forty consecutive patients with known cardiac disease referred to our emergency department for symptoms of suspected COVID-19, laboratory diagnosis of COVID-19 and typical signs of viral pneumonia at chest CT at the time of diagnosis were enrolled in the study. Demographic, clinical, laboratory and outcome data were extracted from the in-hospital medical records. All CT examinations were performed using a 256- slices CT scanner (Revolution CT; GE Healthcare, Milwaukee, WI) using the following parameters: spiral caudo-cranial not gated acquisition with 100 kV peak tube voltage and mAs ranging from 250 to 450 depending on patients body mass index. Section configuration, 256 × 0.625 mm; voxel size, 0.625 mm; gantry rotation time 280 msec and last generation iterative reconstruction algorithm (ASIR-V; GE Healthcare) at 50% level. No contrast media were administered to the patients. The % extent of lung parenchyma affected by COVID-19 pneumonia was processed by a dedicated workstation (ADW 4.6, GE Healthcare) using a specific reconstruction software (Thoracic-V-Car software. GE Healthcare). This quantitative approach enables an automated assessment of the pulmonary infection, depicting infection areas as high attenuation areas (HAAs) in respect of a defined threshold value ranging from −650 Hounsfield unit (HU) to 3071 HU. The amount of infected lung defined as the percentage of lung parenchyma above the predefined vendor-specific threshold of −650 HU (HAA%, HAA/total lung volume) was automatically calculated by the dedicated software for both lungs. Moreover, qualitative parameter of lung involvement (ground-glass opacification and parenchymal consolidation) were reported. Logistic regression analysis was used in order to evaluate the relationship between clinical and CT variables with outcome both for univariate and multivariate analysis. A composite of all cause of death + invasive ventilation + thromboembolic event was considered as primary endpoint for the analysis. A p-value <0.05 was considered statistically significant. Statistical analysis and graphics were produced with MedCalc (version 11.6.1.0, Med-Calc Software; 1993–2011).
4. Results
Demographic and main clinical characteristics of the study population are reported in Table 1 . The mean age was 71.6 ± 13.4 years-old and 28 patients were male. The prevalence of cardiac disease was: chronic coronary artery disease 38 case (95%); atrial fibrillation 7 case (17.5%) and valvular disease 13 cases (32.5) The prevalence of CV risk factors was: diabetes 17 cases (42%), hypertension 33 cases (82%), familiar history of CAD 14 cases (35%), active smoking 9 cases (22%) and hypercholesterolemia 23 cases (57%).
Table 1.
Univariate an multivariate analysis for prediction of clinical end-points.
| All population (n = 40) | All cause of death, invasive ventilation, thromboembolic event (n = 9) |
p | |
|---|---|---|---|
| Univariate analysis | |||
| Age (y) | 71.6 ± 13.4 | 1.06 (0.98–1.15) | 0.132 |
| Sex (male) | 28 (70) | 1.66 (0.29–9.52) | 0.565 |
| BMI (Kg/m2) | 26.1 ± 4.6 | 0.98 (0.79–1.22) | 0.917 |
| BNP (pg/ml) | 471 (138–867) | 1.00 (0.99–1.01) | 0.428 |
| Hs-TnI (ng(ml) | 28.2 (10.7–80.1) | 0.99 (0.99–1.00) | 0.665 |
| At least 2 RF n(%) | 26 (65) | 2.21 (0.39–12.46) | 0.368 |
| LVEF < 35% (%) | 9 (22.5) | 0.97 (0.64–5.82) | 0.981 |
| p/f ratio | 254 ± 130.2 | 1.01 (0.99–1.01) | 0.829 |
| GGO stage + parenchymal consolidation n, (%) | 9 (22.5) | 1.64 (0.34–7.80) | 0.529 |
| Total lung disease at CT (%) | 15.1 (9.8–25.1) | 1.06 (1.01–1.11) | 0.022 |
| All population (n = 40) | All cause of death, Invasive ventilation, and thromboembolic event (n = 9) |
p | |
| Multivariate analysis | |||
| Age (y) | – | 1.05 (0.97–1.15) | 0.177 |
| Total lung disease at CT (%) | – | 1.06 (1.01–1.11) | 0.034 |
Values are n (%), mean ± SD or median (IQR) as appropriate.
BMI = body mass index; BNP = brain natriuretic peptide; LVEF = left ventricle ejection fraction; CT = computed tomography.
In the entire population a median of 15.1% of disease lung involvement at CT was recorded and 9 patients (22.5%) presented both ground glass and lung parenchymal consolidation at CT scan.
During the hospitalization, the following clinical events were recorded in nine patients: 6 deaths, 3 invasive ventilations and 2 thromboembolic events. The mean time from admission to event was 13.6 days. The only predictor of the composite end-point (all cause of death + invasive ventilation + thromboembolic event) was the lung involvement % at chest CT (OR: 1.06; 95%CI: 1.01–1.11, P = 0.02). In the multivariate analysis, the lung involvement % at chest CT was the only independent predictor of the composite end-point (OR: 1.06; 95%CI: 1.01–1.11, P = 0.034).
5. Discussion
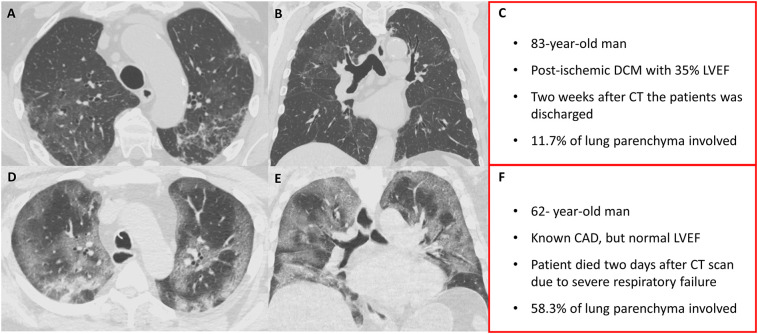
In agreement with previous studies [6], our findings show a high mortality and rate of major complications as thromboembolic events in patients with COVID-19 pneumonia and cardiac disease that are of 15% (6/40 patients) and 22.5% (9/40 patients), respectively. However, the main finding of our study is that the extent of lung involvement by COVID-19 is the only independent predictor of adverse outcome of patients and is predominant over the severity of cardiac disease (Fig. 1 ). Indeed, the presence of significant left ventricle dysfunction (represented in the analysis by ejection fraction <35%), the value of myocardial damage represented by level of high sensitivity Troponin I, elevated BNP or high cardiovascular risk burden (at least 2 risk factors) were not independent predictors of adverse clinical outcome in the specific setting of patients with known cardiovascular disease. This finding was probably due to the intrinsic severity of lung inflammation by SARS-CoV2 infection and by the high grade of lung involvement (median value of the percentage of lung parenchyma interested by COVID disease of 15.15% at the time of diagnosis) in our population. Thus, extent and degree of lung involvement exhibited a pivotal role in determining patients prognosis especially in a population of subjects with cardiovascular disease, even if the inclusion in the present study of a population with selected cardiovascular profile may theoretically represent a bias towards possible trend of underestimation of cardiovascular disease impact on COVID-19. Thus, we cannot excluded that in an unselected population the presence of cardiovascular disease may have a more relevant prognostic role. Indeed, as previously reported [7], in a population without known CAD, elevated calcium score (>400) has been associated with worse prognosis among patients affected by COVID-19.
Fig. 1.
In a 83-year-old male, with known post-ischemic DCM with 35% LVEF, unenhanced chest CT (A-B-C) shows “patchy” peripheral ground glass opacities with superimposed irregular linear opacities in the upper lobes. In a 62- year-old male, with known CAD, but normal LVEF, chest CT (D-E-F) shows extensive bilateral ground-glass opacities involving most of the upper and lower lobes, with smooth interlobular septal thickening, giving a white lung appearance.
From a clinical point of view, a non-contrast CT scan could be proposed as a mandatory test in the acute phase of COVID-19 in the presence of cardiovascular co-morbidities, in order to better stratify patients prognosis that does not appear to be strictly related to the severity of pre-existent cardiovascular disease. Moreover, a follow-up CT scan in the survivors could be reasonable, in order to identify possible long-term sequelae of extensive lung disease.
References
- 1.Giulio G. Stefanini, Elena Azzolini, Gianluigi Condorelli. Critical Organizational Issues for Cardiologists in the COVID-19 Outbreak: A Frontline Experience From Milan, Italy. 10.1161/CIRCULATIONAHA.120.047070. [DOI] [PubMed]
- 2.Rosenbaum L. Facing Covid-19 in Italy — Ethics, Logistics, and Therapeutics on the Epidemic’s Front Line. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 3.Guan W.J., Ni Z.Y., Hu Y. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi S., Qin M., Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riccardo Inciardi, Marianna Adamo, Laura Lupi, et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur. Heart J. (2020) 0, 1–9. 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed]
- 6.Ferrari R., Di Pasquale G., Rapezzi C. Commentary: What is the relationship between Covid-19 and cardiovascular disease? Int. J. Cardiol. 2020;310:167–168. doi: 10.1016/j.ijcard.2020.03.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nai Fovino L., Cademartiri F., Tarantini G. Subclinical coronary artery disease in COVID-19 patients. Eur Heart J Cardiovasc Imaging. 2020 Jul 16:jeaa202. doi: 10.1093/ehjci/jeaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]