Clinical Implications.
-
•
The adoption of telemedicine services by the allergist community was minimal before the severe acute respiratory syndrome coronavirus 2 pandemic, but has gained dramatic momentum in recent months. We present the results of a survey study aimed at measuring patient satisfaction with a cloud-based telemedicine platform and performed at an academic allergy clinic during the pandemic.
Despite the exponential growth in telemedicine in the past 5 years in the United States, its adoption by the allergist community was minimal before the pandemic.1 The delay in uptake is notable because this specialty is especially prime for telehealth services.2 Allergists treat a generally healthy patient base and manage a range of diagnoses amenable to telemedicine modalities. However, allergists also rely on several procedures for effective patient management. These can be challenging to conduct using telehealth alone and may account for some of the inertia in adopting these services.
Direct-to-consumer telehealth, dominated by the for-profit private sector, was the most popular form of telemedicine before the severe acute respiratory syndrome coronavirus 2 pandemic.3 With the current pandemic and the advent of improved Centers for Medicare and Medicaid Services and third-party reimbursement for telehealth, the expansion of direct-to-consumer telehealth among allergists has gained abrupt and dramatic momentum. At the Emory Allergy Clinic, a telemedicine program was rolled out in a highly expedited fashion within 1 week to maintain access while limiting infectious risk. From a provider and administrative standpoint, we have continually sought to fine-tune and readjust delivery of services. It is however imperative to evaluate telehealth delivery models not only in terms of efficiency and efficacy but also in terms of patient acceptance and satisfaction. We performed a survey study aimed at measuring patient satisfaction with a cloud-based telemedicine platform. Patient data from our academic adult clinic were collected over the first 2 months following its implementation (March 24 to May 29, 2020). We used a questionnaire-based survey that was sent to all patients who used telemedicine services during this time. Qualifying visits were defined as those involving synchronous 2-way audiovisual encounters between the allergy provider and the patient using Zoom and transcribed into PowerChart.
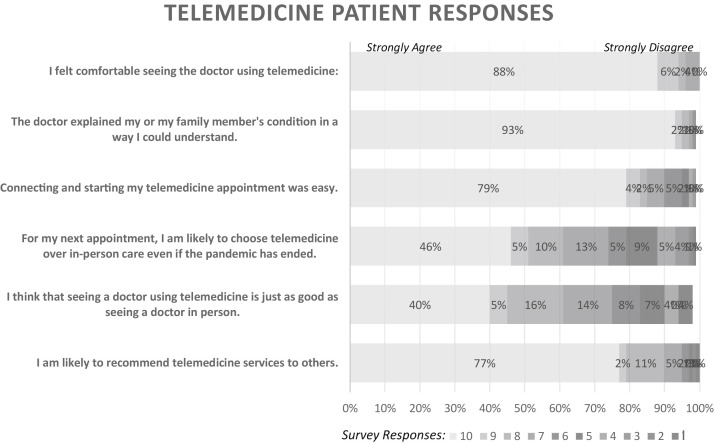
Patients were contacted to complete the survey by a member of the study team who was not present during the telemedicine appointment to minimize bias. The questionnaire consisted of 6 questions that prompted patients to grade their satisfaction with various aspects of their telemedicine visit (Figure 1 ). Their responses were scaled from 0 to 10, with 10 representing the highest satisfaction score. The scale was dichotomized as a response of 10 versus less than 10, in accordance with other measures of patient satisfaction.4
Figure 1.
Survey responses scale: 1 (strongly disagree) to 10 (strongly agree).
A total of 297 patients were seen in 289 encounters during the 2-month study period. Seventeen percent of visits were new consultations and 83% were established follow-ups. There was a 58% response rate. Seventy-eight of respondents were female, and the mean age was 45 years. Patient demographics as well as insurance information are outlined in Table I . The primary diagnoses were asthma in 48% of patients, immune deficiency in 20%, rhinitis in 14%, urticaria/angioedema in 9%, food allergy in 6%, and drug allergy in 3%.
Table I.
Telemedicine patient demographics
| Characteristic | Respondents, n | Respondents, % | Total telehealth patients |
|---|---|---|---|
| Age (y) | |||
| 18-39 | 64 | 40 | 106 |
| 40-59 | 63 | 39 | 115 |
| 60+ | 35 | 22 | 68 |
| Sex | |||
| Female | 126 | 78 | 225 |
| Male | 36 | 22 | 64 |
| Ethnicity | |||
| Asian | 5 | 4 | 8 |
| Black | 49 | 30 | 100 |
| White | 95 | 58 | 166 |
| Hispanic | 2 | 1 | 4 |
| Unidentified | 11 | 7 | 11 |
| Insurance | |||
| Government | 48 | 30 | 82 |
| Private | 114 | 70 | 207 |
| Type of visit | |||
| Established | 134 | 83 | 235 |
| New | 28 | 17 | 54 |
| Primary diagnoses | |||
| Asthma | 78 | 48 | 126 |
| Drug allergy | 5 | 3 | 10 |
| Food allergy | 9 | 6 | 14 |
| Immune deficiency | 32 | 20 | 50 |
| Rhinitis | 23 | 14 | 59 |
| Urticaria/angioedema | 15 | 9 | 30 |
Overall, 88% of patients rated their comfort level seeing a doctor via telemedicine as a 10. Ninety-three percent of respondents stated that their doctor explained their condition in an easily understood manner; 79% strongly agreed that connecting their telehealth appointments was easy. Only 46% indicated their preference for future telemedicine visits following resolution of the pandemic, while 77% would strongly recommend telemedicine services to others. Forty percent rated their virtual visit equivalent or superior to a traditional outpatient encounter. Figure 1 illustrates responses to each question. There were various reasons stated by responders who would not preferentially elect for telehealth again. Some were disappointed with the limitations of the physical examination and access to ancillary testing such as laboratories and pulmonary function tests. Others expressed discomfort with video conferencing technology, whereas a minority expressed a compromise to the level of rapport with the doctor. Those who highly prefer telehealth visits expressed satisfaction with convenience, decreased wait times, and saving money and transportation time.
Logistic regression analysis was performed to evaluate potential factors influencing patient satisfaction. Notably, white patients were 18.5 times more likely to express comfort with telemedicine encounters as compared with Hispanic patients. Patients with government insurance were 2.5 times more likely to choose telemedicine even after the pandemic and 2.7 times more likely to recommend telemedicine to others. We did not ascertain significant associations with satisfaction scores for sex or underlying diagnosis.
Our data have implications for present and continuing service delivery. It remains to be seen whether current practice will translate into a longer-term acceptance of telehealth in allergy following resolution of the coronavirus disease 2019 pandemic. Telemedicine has been shown in previous studies to increase access to care, improve health outcomes, and reduce costs,5 but a Zoom platform has obvious limitations, and is less suitable for visits requiring a physical examination or diagnostic evaluation. In a large cohort of telehealth patients from a tertiary center, only 25% of new allergy consults and less than 10% of follow-up encounters requested in-person evaluations.6 In a pediatric study, asthma outcomes were comparable in matched cohorts seen either via telemedicine or in person,7 and this study design would be helpful for each allergy diagnosis in the future.
Our study has several shortcomings. The questionnaire was numerically scored and not open-ended, and did not formally elicit patient-specific feedback. In addition, our study only included adult patients older than 18 years and cannot be generalized to pediatric populations. Also, the study design self-selected patients with experience in videoconferencing, thus excluding those without access to this technology who were unable to schedule a visit. In addition, our telehealth platform is nonfacilitated and few of our providers had previously used telehealth. Thus, our outcomes and experiences cannot be extrapolated to other centers with different levels of resources and training.
In conclusion, it appears feasible for allergists to provide high-quality care via telemedicine based on patient satisfaction; however, there is a great deal of reluctance to preferentially elect telehealth over in-person visits. These findings are congruent with previous reports on patient experience with telehealth, which have been overall favorable.8 , 9 Future studies should focus on clinical outcomes stratified by underlying diagnosis. We also recognize that our findings are applicable only to patients with the technical proficiency to perform these visits, and the opinions of those without such experience must be accounted for.
Acknowledgments
We acknowledge the contribution of Grace Kim with the Biostatistics, Epidemiology, & Research Design Research Forum for her assistance with the statistical analysis and the development of this manuscript.
Footnotes
Conflicts of interest: The authors declare they have no relevant conflicts of interest.
References
- 1.Portnoy J., Waller M., Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elliott T., Yopes M.C. Direct-to-consumer telemedicine. J Allergy Clin Immunol Pract. 2019;7:2546–2552. doi: 10.1016/j.jaip.2019.06.027. [DOI] [PubMed] [Google Scholar]
- 3.Elliott T., Shih J. Direct to consumer telemedicine. Curr Allergy Asthma Rep. 2019;19:1. doi: 10.1007/s11882-019-0837-7. [DOI] [PubMed] [Google Scholar]
- 4.Giordano L.A., Elliott M.N., Goldstein E., Lehrman W.G., Spencer P.A. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67:27–37. doi: 10.1177/1077558709341065. [DOI] [PubMed] [Google Scholar]
- 5.Elliott T., Shih J., Dinakar C., Portnoy J., Fineman S. American College of Allergy, Asthma & Immunology Position Paper on the Use of Telemedicine for Allergists. Ann Allergy Asthma Immunol. 2017;119:512–517. doi: 10.1016/j.anai.2017.09.052. [DOI] [PubMed] [Google Scholar]
- 6.Waibel K.H., Bickel R.A., Brown T. Outcomes from a regional synchronous tele-allergy service. J Allergy Clin Immunol Pract. 2019;7:1017–1021. doi: 10.1016/j.jaip.2018.10.026. [DOI] [PubMed] [Google Scholar]
- 7.Portnoy J.M., Waller M., De Lurgio S., Dinakar C. Telemedicine is as effective as in-person visits for patients with asthma. Ann Allergy Asthma Immunol. 2016;117:241–245. doi: 10.1016/j.anai.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Ratanjee-Vanmali H., Swanepoel W., Laplante-Levesque A. Patient uptake, experience, and satisfaction using web-based and face-to-face hearing health services: process evaluation study. J Med Internet Res. 2020;22:e15875. doi: 10.2196/15875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slightam C., Gregory A.J., Hu J., Jacobs J., Gurmessa T., Kimerling R. Patient perceptions of video visits using Veterans Affairs telehealth tablets: survey study. J Med Internet Res. 2020;22:e15682. doi: 10.2196/15682. [DOI] [PMC free article] [PubMed] [Google Scholar]