Abstract
Coronavirus disease 2019 (COVID-19) started as an epidemic in Wuhan in 2019, and has since become a pandemic. Groups from China identified and sequenced the virus responsible for COVID-19, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and determined that it was a novel coronavirus sharing high sequence identity with bat- and pangolin-derived SARS-like coronaviruses, suggesting a zoonotic origin. SARS-CoV-2 is a member of the Coronaviridae family of enveloped, positive-sense, single-stranded RNA viruses that infect a broad range of vertebrates. The rapid release of the sequence of the virus has enabled the development of diagnostic tools. Additionally, serological tests can now identify individuals who have been infected. SARS-CoV-2 infection is associated with a fatality rate of around 1–3%, which is commonly linked to the development of acute respiratory distress syndrome (ARDS), likely resulting from uncontrolled immune activation, the so called “cytokine storm”. Risk factors for mortality include advanced age, obesity, diabetes, and hypertension. Drug repurposing has been used to rapidly identify potential treatments for COVID-19, which could move quickly to phase III. Better knowledge of the virus and its enzymes will aid the development of more potent and specific direct-acting antivirals. In the long term, a vaccine to prevent infection is crucial; however, even if successful, it might not be available before 2021-22. To date, except for intravenous remdesivir and dexamethasone, which have modest effects in moderate to severe COVID-19, no strong clinical evidence supports the efficacy of any other drugs against SARS-CoV-2. The aim of this review is to provide insights on the discovery of SARS-CoV-2, its virology, diagnostic tools, and the ongoing drug discovery effort.
Keywords: SARS-CoV-2, Coronavirus, Pathogenesis, Drug repurposing, Remdesivir
Introduction
The World Health Organization (WHO) announced on March 11th 2020, that the outbreak of “COronaVIrus Disease 2019” (COVID-19), which initially started in Asia, had become a pandemic. As of September 4th 2020 the aetiologic agent, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread all over the world, leading to around 26 million confirmed cases and around 865,000 deaths.1 The rapid availability of the genomic sequence of the viral RNA has been instrumental in the development of diagnostic tools and for the identification of experimental treatments. In this review, we will focus on the discovery of SARS-CoV-2, its virological features and pathogenesis, as well as diagnostic tools and, of course, drug development.
Overview of SARS-CoV-2 virology
The causative agent of COVID-19 is a novel coronavirus officially named SARS-CoV-2. It was named after SARS-CoV, because of their genomic homology.2 Coronaviruses are enveloped, large, positive-sense single-stranded RNA viruses (+ssRNA) of the Coronaviridae family. Coronaviruses can infect a broad range of vertebrates, including bats, birds, pangolins, snakes, mice, and humans. Due to sequence similarities with RaTG13 bat and pangolin coronavirus strains, it is currently thought that SARS-CoV-2 has a zoonotic origin and has secondarily acquired human-to-human spreading capacity.3 In particular, the acquisition of i) mutations in the receptor-binding area, ii) a polybasic furin cleavage site (RRRAR) at the junction of subdomain 1 and 2 of the spike protein and iii) a site of O-linked glycosylation in the same area, have enabled the virus to efficiently interact with high affinity (via its spike protein) with its bona fide cellular receptor (angiotensin-converting enzyme 2 [ACE-2]),4 to become more virulent and pathogenic, while potentially evading immune responses through O-glycan epitope masking.3
Key point.
An epidemic of acute respiratory syndrome (COVID-19) started in humans in Wuhan in 2019, and has since become a pandemic.
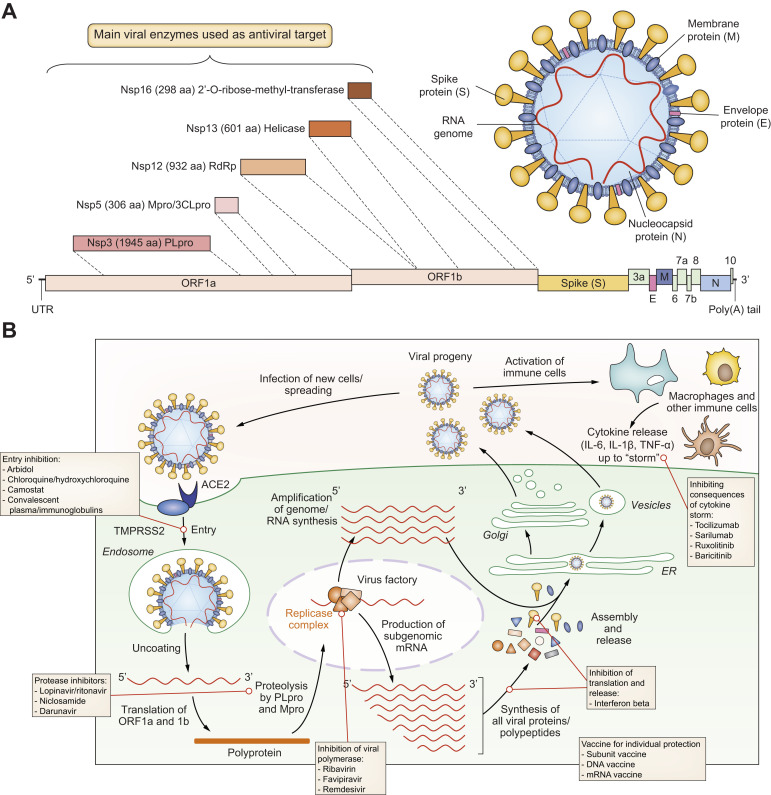
Fig. 1 provides general information on SARS-CoV-2 and its replication cycle, as well as a schematic representation of targets for drug development.
Fig. 1.
Virology, replication cycle and targets for drug development.
(A) Coronaviruses have a long, capped and poly-adenylated RNA genome, which contains between 8 to 10 ORFs, allowing structural, non-structural and accessory viral protein synthesis.87 SARS-CoV-2 is 29,903 base-long and contains 6 majors ORFs, as well as additional accessory genes; the reference sequence is registered in GenBank with ID: MN908947.3.1 (A, B) Up to 28 different polypeptides are potentially produced in fine from the different ORFs and after polyprotein processing by viro-encoded proteases.87 If the RNA genome contained in virions can already serve, after cell entry, as a template for the synthesis of non-structural proteins, which are involved in the early phase of virus replication (mainly by forming the replicase complex), subgenomic messenger RNAs are also produced in the late phase of the cycle to allow the synthesis of structural proteins (e.g. spike (S), envelope (E), membrane (M) and nucleocapsid (N) proteins), as well as other accessory polypeptides. Another main replication intermediate is the complementary minus-sens RNA, which is used by the viro-encoded RdRp, within the replicase complex, to amplify the full-length genome, which is then capped and polyadenylated by both viral and host enzymes before being incorporated into the viral progeny. (B) After entry into ACE2-positive (entry receptor) and TMPRSS2-positive (co-factor for entry) cells, and membrane fusion (i.e. uncoating process), a full-length genome is released into the cytoplasm of cells. This full-length polycistronic RNA is directly used to efficiently encode a polyprotein from the first ORFs present on the molecule, starting from 5′ extremity, i.e. ORF1a and ORF1b; the latter is read after a frame-shift from ribosomal scanning of ORF1a. (A, B) The polyprotein is then processed by 2 viro-encoded proteases, PLpro/Nsp3 and 3CLpro/Nsp5 (also known as main protease [Mpro]), into 16 proteins/polypeptides (Nsp1 to 16). (B) These non-structural proteins/polypeptides are important for the early stages of infection, as they enable the formation of the replicase complex around the RdRp enzymatic activity, which is involved in the synthesis of negative-sense full-length RNA, as well as subgenomic messenger RNAs by a discontinuous transcription strategy.87 The latter enables the efficient and stochiometric synthesis of all other viral proteins/polypeptides, which are important for virus assembly and release of progeny virions. (B) Specific targets for drug development and current treatment options are indicated. ACE2, angiotensin-converting enzyme 2; 3CLpro/Nsp5, chemotrypsin-like protease; ORF, open reading frame; PLpro/Nsp3, papain-like cysteine protease; RdRp, RNA-dependent RNA polymerase; SARS-CoV-2, severe acute respiratory syndrome-coronavirus 2.
Where does the virus replicate?
Following replication and subgenomic RNA synthesis, the viral structural proteins are translated and inserted into the endoplasmic reticulum (ER). These proteins move along the secretory pathway into the ER–Golgi intermediate compartment. In infected cells, the CoV RNA-synthesising machinery associates with modified ER membranes that are transformed into the viral replication organelle; double-membrane vesicles appear to be the central hub for viral RNA synthesis.5 Notably, SARS-CoV-2 is present for significantly longer in stool samples than in respiratory samples.6
Mechanisms of virus-induced toxicity
The virus may be cytotoxic during the first days of infection. In biopsy or autopsy studies of patients infected with COVID-19, pulmonary pathology showed diffuse alveolar damage with the formation of hyaline membranes, infiltration of air spaces by mononuclear cells/macrophages, and a diffuse thickening of the alveolar wall.7 , 8 The lungs from patients with COVID-19 also showed severe endothelial injury associated with the presence of intracellular virus and disrupted cell membranes.9 Viral particles were observed in the epithelial cells by electron microscopy, suggesting that these lesions might be partially caused by direct cytotoxicity.
Future directions for basic research and target identification
A better understanding of the functions/roles of viral proteins, as well as of the viral replication cycle, with a particular attention on host-cell/virus interactions, will enable the identification of novel, or a better characterisation of existing, targets for antiviral development. The success of drug development for HCV has inspired scientists to achieve similar results for other viruses.10
Key point.
Groups from China identified and sequenced the virus responsible for COVID-19, named SARS-CoV-2, and determined that it was a novel coronavirus that shared high sequence identity with bat-derived SARS-like coronavirus, suggesting it had originated in bats.
Entry process
Many cell types express ACE2 and transmembrane serine protease 2 (TMPRSS2), the 2 cellular factors important for viral entry,11 including nasal and lower airway epithelial cells (pneumocytes), lung resident immune cells, endothelial cells, as well as neurons, enterocytes, cardiomyocytes, hepatocytes and kidney cells.[12], [13], [14] But the presence of mRNA in these cell types is not sufficient; further studies are needed to analyse the protein expression of these entry factors and to demonstrate bona fide viral entry and active replication in all these cell types. Interestingly, it was very recently shown that ACE2 is an interferon-stimulated gene (ISG),15 meaning that the presence of interferons in the microenvironment of the virus replication site could further enhance the spreading of the virus. The molecular details of the entry process, involving the spike protein and host receptor/co-receptor, have already been studied.16 The polybasic furin cleavage site at the junction of subdomain 1 and 2 of the spike protein may explain the large number of cell types that can be infected by the virus and the consequent diverse organ manifestations, possibly including thrombotic complications resulting from endothelial cell infection. This research will facilitate the identification of neutralising antibodies or small molecules, which could target this step of the life cycle.
Viral enzymes
Coronaviruses encode several enzymes that are crucial for the replication of the virus and are ideal targets for antiviral development, including 2 proteases/proteinases (papain-like cysteine protease [PLpro] and 3-chymotrypsin-like protease [3CLpro]), the RNA-dependent RNA polymerase (RdRp), a helicase, an mRNA-cap-methyltransferase, and an exoribonuclease. These enzymes have been well studied for SARS-CoV, and thanks to the high homology between the 2 SARS-CoVs, we could expect functional similarities allowing for the possible repurposing of drugs.3 , 4 , 11
Key point.
SARS-CoV-2 is a member of Coronaviridae, a family of enveloped, positive-sense, single-stranded RNA viruses that infect a broad range of vertebrates.
The RdRp (also identified as Nsp12) bears the main enzymatic activity of the replicase complex. Recent advances in antiviral research against HCV10 , 17 have confirmed that RdRps are major targets for very specific antiviral discovery. Like HCV, the SARS-CoV-2 genome is characterised by a positive-sense single-strand RNA and both viruses share a similar replication cycle requiring an RdRp. This polymerase displays similar catalytic mechanisms and key conserved amino acids in the active site. The 3D structure of the SARS-CoV-2 RdRp was recently characterised.18 , 19 Interestingly it has a large N-terminal extension containing a kinase-like fold. The polymerase domain, like in HCV, is composed of 3 subdomains; a fingers subdomain, a palm subdomain, and a thumb subdomain. Moreover, 3CLpro is vital to viral replication and the 3CLpro cleavage sites are highly conserved, so it could be a promising drug target.18
PLpro and 3CLpro/Mpro are essential enzymes for the proteolytic processing of the CoV replicase polyprotein; their activities are needed very early in the infection process for the step-by-step release of other viral enzymatic activities. They are also attractive targets for specific antiviral discovery. The 3D structures of the SARS-CoV and SARS-CoV-2 proteases are available. Moreover biochemical assays are also available for functional testing, at least for the SARS-CoV proteins.20 PLpro is a cysteine protease, encoded by Nsp3, and involved in the release of Nsp1 to 3, as well as in the regulation of host innate immunity, enabling viral escape.20 Although the similarity is not very high between the PLpro of SARS-CoV-2 and that of SARS-CoV, the catalytic domain, around the triad Cyst-His-Asp, is well conserved; therefore, drugs already in the pipeline for SARS-CoV might be repurposed.
3CLpro/Mpro is encoded by Nsp 5, forms a functional homodimer, utilises a catalytic dyad Cys-His, and is involved in the release of Nsp4 to 16 from polyprotein. Its activity is key in the CoV replication cycle and its inhibition is very efficient at stopping viral replication. Due to the dimeric nature of this protease, not only catalytic inhibitors, but also allosteric ones can be developed, increasing the possibility of success. Moreover the very high similarity of 3CLpro/Mpro between the SARS-CoVs may allow for drug repurposing.20 Specific antiviral screening has been started and several drug candidates that target the 3CLpro of SARS-CoV-2 have already been identified.21 , 22
Exacerbated innate immune functions
Besides the virological aspects of COVID-19, it is also important to better understand immunological factors, and how their mutual amplification is involved in the pathogenesis of the disease. While the virus can be studied in cell culture models, immunological factors can only be studied either in relevant animal models or during clinical studies, using patient samples. It is now rather well established that in patients with poor outcome there is an uncontrolled “cytokine storm”, featuring a local and systemic production of pro-inflammatory cytokines such as interleukin (IL)-6, tumour necrosis factor-α (TNF-α) and IL-1β.[23], [24], [25], [26], [27] Recently, it was reported that ACE2 is a human ISG; data suggest that SARS-CoV-2 could exploit species-specific interferon-driven upregulation of ACE2, a tissue-protective mediator during lung injury, to enhance infection.28 More studies are needed to clarify the origin of this massive and uncontrolled cytokine production.
Key point.
The sequencing of the virus has allowed for the development of diagnostic tools (e.g., RT-PCR). Additionally, serological tests have enabled the identification of individuals who have previously been infected.
Diagnostic tools for COVID-19
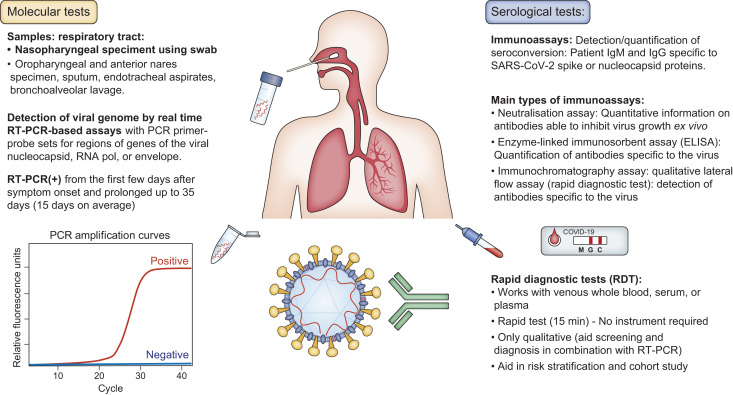
COVID-19 tests can be grouped as nucleic acid, serological, antigen, and ancillary tests, all of which play distinct roles in hospital, point-of-care, or large-scale population testing (Fig. 2 ).29
Fig. 2.
Diagnostic tools.
ELISA, enzyme-linked immunosorbent assay; RT-PCR, reverse transcription PCR.
Methods for the detection of viral nucleic acid
PCR tests for SARS-CoV-2 have been available since January 2020. Reverse transcription quantitative PCR (RT-qPCR)-based assays performed on respiratory specimens have emerged as the cornerstone of COVID-19 diagnostic testing. The USA Centers for Disease Control and prevention has developed a widely used SARS-CoV-2 RT-qPCR assay.30 The kit contains PCR primer-probe sets for 2 regions of the viral nucleocapsid gene (N1 and N2), and for the human RNase-P gene to ensure that RNA extraction was successful. This assay differs from the WHO's assay, which targets SARS-CoV-2 RdRP and E genes.31 To avoid potential cross-reaction with other endemic coronaviruses, as well as potential genetic drift, at least 2 molecular targets should be included in the assay. Evolution and potential mutations in the SARS-CoV-2 genome support the need to continue optimising the oligonucleotides through global sharing of updated SARS-CoV-2 genomes.32 The theoretical specificity of most RT-qPCR assays is 100% because the primer design is specific to the SARS-CoV-2 genome. Occasional false positive results may occur due to technical errors or reagent contamination.33 A cycle threshold (Ct) value of RT-qPCR less than 40 is generally interpreted as positive when results are interpreted as qualitative.34 , 35 Quantitative interpretation of Ct as an indicator of the copy number of SARS-CoV-2 RNA in specimens requires an appropriate standard curve with an adequate limit of detection.36 A rigorous assessment of the diagnostic accuracy of the many newly introduced SARS-CoV-2 assays has been hampered by availability.37 , 38 The sensitivity of viral RNA testing varies depending on the timing of testing relative to exposure. A false positive result erroneously labels a person as infected, with consequences including unnecessary quarantine and contact tracing.39 False-negative results are more consequential, because infected people may not be isolated and can infect others. One modelling study estimated that the probability of a false-negative result in an infected patient decreases from 100% on day 1 to 67% on day 4.40 On the day of symptom onset, the median false-negative rate estimation was 38%. A sample pooling strategy was suggested to offer a viable alternative to detect community transmission at a time when tests are in short supply globally.[41], [42], [43] One potential limitation of pool testing is that the false-negative rate may increase, owing to dilution of positive samples. Point-of-care PCR kits can shorten the turnaround time for screening and diagnosing patients with suspected SARS-CoV-2. These rapid tests typically have lower throughput and are generally more expensive than other tests. Time efficient methods that do not require thermal cycling have been designed.44 CRISPR-Cas12/Cas13-based assays are also currently in development for point-of-care use.45 , 46
Nature of samples tested
The current diagnostic strategy to identify patients with COVID-19 is to test samples taken from the respiratory tract for the presence of SARS-CoV-2-specific nucleic acid targets.47 A nasopharyngeal specimen is the preferred choice for testing, but oropharyngeal, mid-turbinate, or anterior nares samples are also acceptable.48 Pharyngeal virus shedding was shown to be very high during the first week of symptoms.49 Infectious virus was readily isolated from throat and lung samples, but not from stool samples. Serum and urine were usually negative for the presence of viral nucleic acid.50 , 51 The viral load in nasopharyngeal samples peaks within the first few days after symptom onset, before declining.48 , 51 , 52 For nasopharyngeal specimens, samples should be obtained using a flocked swab to enhance the collection and release of cellular material.53 , 54 Samples taken from sputum, endotracheal aspirates, and bronchoalveolar lavage may have greater sensitivity than upper respiratory tract specimens.50 Inadequate sample collection may result in a false-negative test. The highest rates of SARS-CoV-2 positivity on RT-qPCR assays were obtained with bronchoalveolar lavage specimens.50 A single nasopharyngeal swab has become the preferred swab, as it is well tolerated and safe. Saliva may also be an alternative specimen source that requires less personal protective equipment and fewer swabs, but it requires further validation.55 , 56
Serologic testing
While RT-qPCR-based molecular assays of respiratory specimens remain the current reference standard for diagnosis, point-of care technologies and serologic immunoassays have also rapidly emerged.[57], [58], [59] Serologic tests that identify antibodies to SARS-CoV-2 from clinical specimens may be less complex than molecular tests.60 As antibody responses to infection take days to weeks to be reliably detected,60 their utility for diagnosing acute infections is limited.48 Rapid antigen detection tests have recently entered the diagnostic market. Compared with RT-PCR, they are cheaper, and easy to use with faster turn-around times. The widespread and frequent use of such tests has recently been proposed but antigen rapid antigen detection tests's differ greatly in their ability to detect infectious cases, therefore requiring careful validation before routine application. Serologic assays might be more relevant in surveying for asymptomatic infection or in scenarios in which patients present with late complications of disease, when RT-qPCR may be falsely negative.55 , 61
Seroconversion in most cases of COVID-19 occurs during the second week of symptoms.49 For SARS-CoV-2 infection, the timing of seroconversion appears to be similar to or slightly earlier than in SARS-CoV infection.62 In a study of 285 patients with COVID-19, 100% of patients tested positive for antiviral IgG within 19 days after symptom onset, with seroconversion for IgG and IgM occurring simultaneously or sequentially.61 Negative results would not exclude COVID-19 infection, particularly among those with recent exposure to the virus. The viral spike protein is perceived as the clear candidate for inclusion in an immunoassay that detects whether antibodies are present.58 , 63 The other protein that appears to be an important antigen for the development of serological assays is the N protein (structural component of the nucleocapsid). Indeed, antibodies to this protein are frequently detected in patients with COVID-19,64 , 65 suggesting that the N protein may be one of the immunodominant antigens for the early diagnosis of COVID-1.60 , 66 , 67 It is now established that pre-existing immune reactivity to SARS-CoV-2 can exist in the general population. Serum samples from patients with COVID-19 showed some cross-reactivity for the SARS-CoV nucleocapsid antigens.61 , 68 , 69 A recent study detected SARS-CoV-2-reactive CD4+ T cells in 50% of unexposed individuals, suggesting cross reactive T cell recognition between circulating “common cold” coronaviruses and SARS-CoV-2.66 T cell reactivity was highest against proteins other than the coronavirus spike protein, but T cell reactivity was also detected against the spike protein. Several monoclonal antibodies have been described that target the spike glycoprotein of SARS-CoV-2 from memory B cells of an individual who was infected with SARS-CoV in 2003.68 One antibody (S309) potently neutralises SARS-CoV-2 by engaging the receptor-binding domain of the spike glycoprotein.
Enzyme-linked immunosorbent assays (ELISA) and chemiluminescent immunoassay (CLIA) are common laboratory platforms that can measure antibody titres (IgG and IgM). A variation of these tests can use magnetic, protein-coated microparticles, known as a chemiluminescent microparticle immunoassay. Being able to quantify antibodies will be important to identify convalescent plasma donors with abundant titres and to study how the immune system responds to the virus. Neutralising antibodies play important roles in viral clearance and have been considered as a key immune product for protection or treatment against viral diseases. In COVID-19, transfusion of convalescent plasma or serum from recovered patients was also considered a promising therapy.70 , 71 The neutralisation assay is a laboratory-based test that uses live virus and cell culture methods to determine if patient antibodies can prevent viral infection in vitro.72
Because immunofluorescence assays are labour intensive, a substantial number of the new commercial COVID-19 antibody tests – developed as screening tests – are not ELISA-based. They are lateral flow immunoassays (LFIAs), which provide no quantitative information. These qualitative LFIAs represent typically small, portable rapid diagnostic tests that can be used at point-of-care.
Conclusions on serologic testing
Antibody testing is ramping up quickly, with a growing list of commercial kits and test protocols from academic researchers,57 although many questions remain to be answered. The first and most urgent is the validation of serologic tests. A recent meta-analysis showed wide ranging sensitivities, from 66% with LFIAs to 98% with CLIAs73; sensitivities were higher with increased time after symptom onset. The specificities are excellent (99%). Assays must be optimised further, independently validated, and used as part of an algorithm to achieve the highest possible accuracy for decision making.74 , 75 Second, there is insufficient data on the magnitude and duration of antibody responses after infections. Although data suggest that neutralising titres correlate with severity of infection,61 it remains unclear whether this effect is caused by ongoing somatic hypermutation or ongoing production of highly potent antibodies that were initially generated. Moreover, any documentation that limits individual freedoms on the basis of biology risks becoming a platform for restricting human rights.76
Key point.
Testing and tracing programmes will be essential. Later, testing, tracing and treating (T3) programmes will become mandatory, once effective and safe therapies are developed.
Pathophysiology and clinical characteristics of COVID-19
Pathophysiology
Several potential pathogenic mechanisms may be involved in COVID-19, including coagulopathy, endothelial dysfunction, and excessive release of pro-inflammatory cytokines. The endothelial dysfunction caused by infection activates excessive thrombin generation and inhibits fibrinolysis, leading to hypercoagulability.77 Lymphopenia is frequent in patients with COVID-19.78 The cytokine release syndrome could have a major role in patients with severe COVID-19 as in acute respiratory distress syndrome (ARDS).79 The pathological features of COVID-19-related ARDS are diffuse alveolar damage with hyaline membrane formation and fibrin deposition, as well as a few multinucleated enlarged cells.7 , 8 In patients who died from COVID-19-associated respiratory failure, the histologic pattern in the peripheral lung was diffuse alveolar damage with perivascular T cell infiltration.9 The lungs also showed distinctive vascular features, consisting of severe endothelial injury, but also widespread thrombosis with microangiopathy. Alveolar capillary microthrombi were frequent, with a high level of new vessel growth (intussusceptive angiogenesis).
Key point.
Early strong social distancing efforts are needed to stop transmission of the virus and are important measures to reduce case incidence. In addition, the use of masks, soaps, and disinfectants are critical to reduce or eliminate viral spread. Case isolation and contact tracing has also proven effective.
Transmission by asymptomatic carriers
Several findings are consistent with person-to-person transmission of this novel coronavirus in hospital and family settings.47 , 80 There is also evidence of asymptomatic transmission, including a case of SARS-CoV-2 infection acquired outside of Asia in which transmission appears to have occurred during the incubation period.81 Additionally, in a previously reported family cluster, some family members had positive RT-qPCR results without any symptoms.47
Clinical characteristics
Among 1,099 patients from China with laboratory-confirmed COVID-19, 5.0% were admitted to an intensive care unit (ICU), 2.3% underwent invasive mechanical ventilation, and 1.4% died.78 The most common symptoms were fever and cough. The median incubation period was 4 days. In another study including 191 patients, of whom 54 died in hospital, half of these patients had a comorbidity, with hypertension being the most common, followed by diabetes and coronary heart disease.52 In-hospital death was associated with older age, higher sequential organ failure assessment score, and D-dimer greater than 1 μg/ml on admission. In another study of the 1,591 patients infected with SARS-CoV-2 admitted to ICUs in Italy, the median age was 63 years and 82% were male.82 Among 1,300 patients with available data on respiratory support, 99% needed respiratory support, including 88% who received mechanical ventilation and 11% who received non-invasive ventilation. Finally, in this case series of critically ill patients admitted to ICUs, the majority were older men and ICU mortality was 26%.
Moreover, data from previous coronavirus infections such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome, as well as emerging data from the COVID-19 pandemic, suggest that there could be substantial fibrotic consequences following SARS-CoV-2 infection.83
Pulmonary imaging findings
The hallmarks of COVID-19 were bilateral and peripheral ground-glass and consolidative pulmonary opacities.84 Notably, 56% of patients with early disease had a normal CT. A longer time after the onset of symptoms, abnormal CT findings were more frequent, including consolidation, bilateral and peripheral disease, greater total lung involvement, linear opacities, “crazy-paving” pattern and the “reverse halo” sign. Bilateral lung involvement was observed in 28% of cases in the early phase and 88% in late phase of the disease. CT scans at the time of symptoms may increase diagnosis rates, since RT-qPCR sensitivity may be as low as 60%.85 Also, chest x-ray findings in patients with COVID-19 frequently showed bilateral lower zone consolidation.86
Extrapulmonary manifestations
Coagulopathies
SARS-CoV-2-induced infection can be associated with a coagulopathy consistent with infection-induced inflammatory changes, as observed in patients with disseminated intravascular coagulopathy (DIC).87 In patients with COVID-19, the initial coagulopathy is associated with elevated D-dimer and fibrin/fibrinogen-degradation products. COVID-19-associated coagulopathy should be managed as it would be for any critically ill patient, using thromboembolic prophylaxis and standard supportive care measures for those with sepsis-induced coagulopathy or DIC. Current data do not support the use of high-dose anticoagulants.87
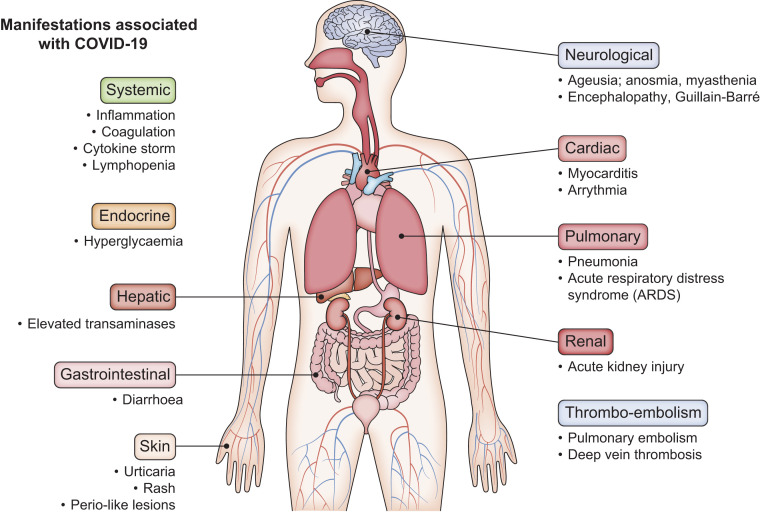
Among all the numerous clinical manifestations associated with COVID-19 infection, there have been reports of cardiological lesions with acute myocardial injury88; neurological lesions with encephalitis and myalgia,89 , 90 cutaneous manifestations with rash and urticaria,91 and acute kidney injury92 (Fig. 3 ).
Fig. 3.
Systemic manifestations of COVID-19.
COVID-19, coronavirus disease 2019.
COVID-19 and the liver
Elevation of liver enzymes occurs in 5 to 50% of patients. The pattern of liver injury is mainly hepatocellular rather than cholestatic,93 , 94 with hepatocyte degeneration, focal necrosis, capillary bile duct cholestasis and inflammation in the portal area, but interestingly SARS-CoV-2 cannot be detected in liver samples.95 Frequently, the severity of liver injury has been correlated with the severity of COVID-19. The presence of underlying chronic liver diseases could render patients with COVID-19 at higher risk of severe liver injury, such as acute-on-chronic liver failure,96 with data suggesting that non-alcoholic/metabolic fatty liver disease (NAFLD/MAFLD) could be an independent risk factor for severe COVID-19.97 , 98
The virus was found in stool samples in around 50% of patients with COVID-19, with around 18% of them complaining of abdominal pain and diarrhoea.99 It was demonstrated that SARS-CoV-2 is capable of productively replicating in ACE2-positive enterocytes.12 Due to the abundance of the virus in the small intestine, liver cell exposure through the hepatic reticular system is expected. The default immune status of the liver might play a critical role in COVID-19 infection. Indeed, it has been shown that in patients with MAFLD, the polarisation status of macrophages might be skewed due to metabolic stimuli such as fatty acids, thus affecting host-inflammatory responses to signals generated from the gut-liver axis.97 In COVID-19, the “cytokine storm” bears resemblance to that observed in patients with SARS.[100], [101], [102]
Key point.
Drug repurposing is a strategy to identify new uses for approved or investigational drugs that are outside the scope of the original medical indication. This strategy has been used to rapidly identify treatments for the COVID-19 infection that could move quickly to phase III.
However, SARS-CoV-2 could also have a direct cytotoxic effect, as its entry receptor ACE-2 is expressed on cholangiocytes.103 Also, learning from the SARS experience, the use of antibiotics and antivirals, as well as possible secondary bacterial infections, might lead to liver injury in patients with COVID-19.104 Moreover, tocilizumab has been evaluated for the treatment of patients with COVID-19 and serious lung damage accompanied by elevated blood levels of IL-6.105 Prophylactic nucleoside analogues against HBV have been recommended for HBsAg-positive patients with COVID-19 for whom immunosuppressive therapy is planned.102 Liver damage, leading to drug withdrawal, has been reported in patients treated with remdesivir. Accordingly, remdesivir is not recommended for patients with alanine aminotransferase >5x the upper limit of normal or with hepatic decompensation.106 Lastly, hypoxia and shock induced by COVID-19-related complications may also cause hepatic ischaemia.107 To manage liver injury related to COVID-19, several guidelines have been issued.[100], [101], [102] , 108
Gastrointestinal manifestations
Clinically, approximately 10% of the patients with COVID-19 suffer from gastrointestinal symptoms such as nausea or vomiting, diarrhoea and anorexia,109 with similar incidence among adults and children.110 Patients with gastrointestinal symptoms may require longer hospitalisations.78 , 79 , 111 In some patients, gastrointestinal (not respiratory) symptoms might be the presenting clinical features.112 , 113 The underlying mechanism may be related to the abundant expression of ACE2 mRNA and receptor protein on enterocytes.112 , 113 Histological changes, including plasma cell and lymphocyte infiltration into the lamina propria of enterocytes, suggested an immune-mediated response.114 The capability of SARS-CoV-2 to infect enterocytes has also been demonstrated in human intestinal organoids.12 One of the major concerns around enteric infection is whether the faecal source can lead to fomite transmission, especially when infective aerosols are generated from the toilet plume. Indeed, a cluster of COVID-19 cases potentially linked to faecal transmission, analogous to “Amoy Garden” during the SARS outbreak in 2003, has recently been reported in Hong Kong.115 In accordance with a surface stability study on plastic and different materials, SARS-CoV-2 could remain viable for up to 72 hours.116 In 1 study, faecal samples remained SARS-CoV-2 positive despite respiratory clearance in 20% of patients.114 Taken together, determining the presence of SARS-CoV-2 in the stool is of great importance for the epidemiological control of COVID-19.
Co-infections
There is major concern regarding the potential for concomitant infection of SARS-CoV-2 with influenza or other respiratory diseases, such a respiratory syncytial virus, tuberculosis or even bacterial infections or mycoplasma. Co-infection with SARS-CoV-2 and influenza A virus in a patient with pneumonia has been reported in China.117 COVID-19 might be underdiagnosed because of false-negative tests for upper respiratory specimens or co-infection with other respiratory viruses.
Key point.
To date, with the exception of intravenous remdesivir or dexamethasone which have a modest effect, no strong clinical evidence supports the efficacy of any drug against SARS-CoV-2.
Treatment strategies
Prevention and transmission control measures
Washing hands frequently, using masks and social distancing are important. China banned travel to and from Wuhan city on 23 January 2020, delaying the arrival of COVID-19 in other cities by approximately 3 days.118 Suspending intra-city public transport, closing entertainment venues and banning public gatherings were associated with reductions in case incidence. Early on, the spatial distribution of COVID-19 cases in China was explained well by human mobility data.119 Following the implementation of control measures, this correlation dropped and growth rates became negative in most locations. A contact tracing application, which builds a memory of proximity contacts and immediately notifies contacts of positive cases could achieve epidemic control if used by enough people.120
Timing of treatment
Much like with influenza, antiviral drugs likely need to be started early after infection to be effective. In turn, this makes it difficult to identify drugs that are indeed effective against the virus in clinical trials. Patients with early disease may benefit from antiviral agents to reduce viral load, patients with severe and late disease may benefit from anti-inflammatory drugs. Furthermore, in the early disease course, anti-inflammatory drugs might be harmful by increasing viral load.
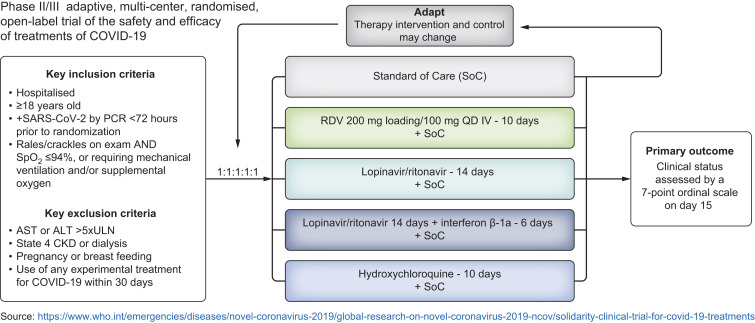
Drug repurposing
Drug repurposing (also called drug repositioning or reprofiling) involves identifying new uses for approved or investigational drugs that are outside the scope of the original medical indication.121 This strategy offers various advantages over developing an entirely new drug, with a reduced risk of failure because safety has already been evaluated. The timeframe and the cost can also be reduced, because most of the preclinical testing and safety assessments have already been done. There have been extensive efforts to repurpose approved drugs during the COVID-19 pandemic. A selection of drugs being tested for COVID-19 is presented in Table 1 . As an example, the design of "Solidarity” – a large randomised trial that is currently ongoing – is provided in Fig. 4 .
Table 1.
Drugs evaluated in clinical trials for the treatment of COVID-19 (not exhaustive).
| Drug | Company | Current use and/or initial target | Mode of Action | Mode of Administration | Clinical trials for COVID-19 (examples) (NCI)(not exhaustive) |
|---|---|---|---|---|---|
| Antiviral | |||||
| Remdesivir | Gilead | Experimental, Ebola | Nucleotide analogue | intravenous | NCT04252664; NCT04280705; Solidarity (WHO); NCT04292899 |
| Chloroquine/hydroxychloroquine (Aralen/Plaquenil) | Sanofi | Malaria | Heme polymerase inhibitor | Oral | NCT04333732; NCT04341727; NCT04358068; NCT04315948 |
| Lopinavir + ritonavir (Kaletra) | AbbVie | HIV | Protease inhibitor | Oral | NCT04307693; NCT04372628; NCT04255017; NCT04276688 |
| Favipiravir (Avigan) | Fujifilm | Experimental, Influenza | RNA polymerase inhibitor | Oral | NCT04333589; NCT04310228; NCT04346628 |
| Umifenovir (Arbidol) | Pharmstandard | Experimental, Influenza | Inhibits membrane fusion (entry) | Oral | NCT04333589 |
| Camostat | Ono Pharmaceutical | Experimental | Protease inhibitor | Oral | NCT04374019 |
| Ribavirin | Bausch Health | Hepatitis C | Lower respiratory tract infection due to RSV | Inhalation | NCT04356677 |
| Anti-inflammatory | |||||
| Interferon alfa-2b | Hepatitis C | Immune modulator | Sub-cutaneous | NCT04349410 | |
| Tocilizumab (Actemra) | Roche | Rheumatoid arthritis | IL-6R Ab | intravenous | NCT04310228; NCT04331795; NCT04320615; NCT04310228 |
| Sarilumab (Kevzara) | Sanofi | Rheumatoid arthritis | IL-6R Ab | intravenous | NCT04315298; NCT04359901 |
| Baricitinib (Olumiant) | Eli Lilly | Rheumatoid arthritis | Inhibition of JAK | Oral | NCT04340232; NCT04373044 |
Ab, antibody; COVID-19, coronavirus disease 2019; RSV, respiratory syncytial virus.
Fig. 4.
WHO master protocol: Solidarity trial.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; CKD, chronic kidney disease; COVID-19, coronavirus disease 2019; RDV, remdesivir; SARS-CoV-2, severe acute respiratory syndrome-coronavirus 2; SOC, standard of care; SpO2, oxygen saturation; ULN, upper limit of normal.
Existing antiviral medicines targeting the virus
Hydroxychloroquine
Hydroxychloroquine is a medication used to prevent and treat lupus and malaria. Hydroxychloroquine has also been combined with azithromycin, an antibiotic. Hydroxychloroquine is hypothesised to inhibit SARS-CoV-2 entry into cells, although there is limited data, mostly coming from case reports and small studies.122 A systematic review on the efficacy and safety of hydroxychloroquine for the treatment of COVID-19 concluded that there is currently no evidence from RCTs for its efficacy.123 In a multicentre, open-label, randomised controlled trial, 150 patients admitted to hospital with laboratory-confirmed COVID-19 were included in the intention-to-treat analysis (75 patients assigned to hydroxychloroquine plus standard of care [SOC], 75 to SOC).124 There was no difference in terms of efficacy between the 2 arms. Adverse events were higher in patients treated with hydroxychloroquine.
Lopinavir
Lopinavir is an antiretroviral protease inhibitor used in combination with ritonavir in HIV therapy; it has shown some antiviral activity against SARS-CoV.125 A randomised, controlled, open-label trial involving hospitalised adult patients with confirmed SARS-CoV-2 infection and COVID-19-related severe respiratory illness was performed.126 Patients were randomly assigned to receive either lopinavir-ritonavir, in addition to SOC, or SOC alone. There were no differences between groups (virological factors, duration of disease, mortality), indicating that there is no benefit in hospitalised adult patients with severe COVID-19. Cell culture data suggest that this compound demonstrates activity with an EC50 of 26.6 μM.127 One wonders why a compound with such weak activity was selected for clinical trials. Human trials of repurposed drugs that are essentially ineffective against SARS-CoV-2 in culture are being repeated over and over again, wasting time and resources.
Remdesivir
Remdesivir is a prodrug of a nucleotide analogue that is intracellularly metabolised to an analogue of adenosine triphosphate that inhibits viral RNA polymerases. Remdesivir has broad-spectrum activity against members of several virus families, including filoviruses (e.g., Ebola) and coronaviruses (e.g., SARS-CoV and MERS-CoV.128 Six large studies are ongoing (Table 2 ). Unfortunately, remdesivir must be given intravenously for at least 5 days, although an aerosol formulation is being developed.
Key point.
Better knowledge of the virus, its enzymes, and immune response is essential for the development of direct-acting antivirals and effective vaccines.
Table 2.
Clinical trials of remdesivir for treatment of COVID-19.
| Study ID | Study Design | Location | Sponsor | Study size (randomisation) | Primary endpoint/outcome |
|---|---|---|---|---|---|
| Terminated studies | |||||
| NCT04257656 (terminated) | Double-blind, placebo-controlled (severe) | Beijing, China | Capital Medical University, China | N = 453 (2:1) 10 day RDV:Placebo |
Time to clinical improvement by Day 28 |
| NCT04252664 (suspended) | Double-blind, placebo-controlled (mild/moderate) | Wuhan, China | Capital Medical University, China | N = 308 (1:1) 10 day RDV:Placebo |
Time to clinical recovery by Day 28 |
| Ongoing studies | |||||
| NCT04292899 | Open-label (severe) | Global | Gilead | Part A N = 400 (1:1) 10 day RDV:5 day RDV |
Endpoint: Clinical status at Day 14 on 7-point ordinal scale |
| NCT04292730 | Open-label (moderate) | Global | Gilead | Part A N = 600 (1:1:1) 10 day RDV:5 day RDV:SoC |
Endpoint: Clinical status at Day 11 on 7-point ordinal scale |
| NCT04280705 | Adaptive, double-blind, placebo-controlled | Global | NIAID | N = 572 (1:1) 10 day RDV:Placebo |
Outcome: Time to recovery [Timeframe: Day 1 through Day 29] |
| NCT04315948 | Adaptive, open-label | Europe | WHO/Institut National de la Santé Et de la Recherche Médicale, France | N = 3,100 (1:1:1:1:1) 10 day RDV:LPV/r: LPV/r+IFN: Hydroxychloroquine:SoC |
Outcome: Percentage of individuals reporting each severity rating on a 7-point ordinal scale [Timeframe: Day 15] |
| Solidarity master protocol | Adaptive, double-blind, placebo-controlled | Global | WHO | (1:1:1:1:1) 10 day RDV:LPV/r: LPV/r+IFN: Hydroxychloroquine:SoC |
Outcome: Clinical status assessed by a 7-point ordinal scale on Day 15 |
COVID-19, coronavirus disease 2019; IFN, interferon; LPV/r, lopinavir + ritonavir; RDV, remdesivir; SoC, standard of care.
A report based on the compassionate use of remdesivir for patients hospitalised with severe COVID-10 has been published.129 From the 53 patients whose data were analysed, clinical improvement was observed in 36/53 patients (68%). In addition, a randomised, double-blind, placebo-controlled, multicentre trial was performed in China.106 Mortality at day 28 was similar between the 2 groups (14% died in the remdesivir group vs. 13% in the placebo group). There was no difference in the 2 groups regarding clinical improvement or decrease in viral load. This trial did not attain the predetermined sample size because the outbreak of COVID-19 was brought under control in China, therefore, it is difficult to reach a definitive conclusion.
Gilead is conducting 2 randomised, open-label, multicentre, phase III clinical studies to evaluate the safety and efficacy of 2 dosing durations – 5 days and 10 days – of remdesivir in adults diagnosed with COVID-19 (The Simple studies). The first SIMPLE study includes hospitalised patients with confirmed SARS-CoV-2 infection, oxygen saturation of 94% or less while breathing ambient air, and radiologic evidence of pneumonia.130 In the second Simple study, patients were randomised to receive open-label remdesivir for 5 or 10 days or SOC alone. At Day 11, a higher proportion of patients in the 5-day treatment group achieved improvement in clinical status vs. the SOC group, achieving statistical significance for a ≥1-point improvement in ordinal scale (p = 0.026) (Gilead press release). However, most clinicians would have preferred to see a decrease in mortality on treatment. Clearly another controlled study will have to be performed soon.
Other antiviral drugs being tested for COVID-19 include arbidol,131 , 132 favipiravir,133 famotidine,134 , 135 and camostat (TMPRSS2 inhibitor).11
Existing antiviral medicines targeting inflammation
Dexamethasone
Glucocorticoids may modulate inflammation-mediated lung injury and thereby reduce progression to respiratory failure and death. In a controlled, open-label trial of patients hospitalised with COVID-19, patients were randomly assigned to receive oral or intravenous dexamethasone (6 mg once daily) for up to 10 days or to receive SOC alone.136 In the dexamethasone group, the incidence of death was lower than that in the SOC group among patients receiving invasive mechanical ventilation (29.3% vs. 41.4%) and among those receiving oxygen without invasive mechanical ventilation (23.3% vs. 26.2%) but not among those who were receiving no respiratory support at randomisation (17.8% vs. 14.0%).
In a recent trial involving patients with ARDS who were undergoing mechanical ventilation, mortality at 60 days was 15 percentage points lower among those receiving dexamethasone than among those receiving SOC.137 In the early phase of the infection, anti-inflammatory drugs may not be efficient and may even be harmful (by increasing viral load). Viral shedding in SARS-CoV-2 appears to be higher early in the illness before declining thereafter.49 , 54 , 138 The fact that dexamethasone confers a greater survival benefit in patients with COVID-19 who are receiving respiratory support, or are recruited after the first week of their illness, suggests that by this stage the disease is dominated by inflammation, with active viral replication playing a secondary role. Clearly a trial of the combination of remdesivir and dexamethasone may yield interesting results.
Interferon beta-1b
The early triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin was safe and superior to lopinavir-ritonavir alone in alleviating symptoms and shortening the duration of viral shedding and hospital stay in patients with mild to moderate COVID-19. Future clinical studies using interferon beta-1b as a backbone are warranted.139
Key point.
A vaccine to prevent infection is crucial; however, even if 50% effective or more, the immunological protection might not persist.
Tocilizumab & Sarilumab
Tocilizumab (Actemra), also known as atlizumab, and sarilumab (Kevzara) are both immunosuppressive drugs, mainly used for the treatment of rheumatoid arthritis. They are both humanised monoclonal antibodies against the IL-6R and are given by injection. Clinical trials are ongoing. Moreover, other monoclonal antibodies or agents targeting other inflammatory cytokines (TNF-α, IL-1β…) should be tested.
Kinase inhibitors
The Janus kinase (JAK)-signal transducer and activator of transcription (STAT) pathway has been implicated as a key driver in many inflammatory diseases. With the development of small molecule inhibitors that can selectively and specifically target key JAKs involved in controlling downstream inflammation, exploration of their utility across a broad range of diseases has become a rapidly expanding field,140 , 141 including for other viral infections (e.g. HIV[142], [143], [144]). Baricitinib and ruxolitinib are 2 known JAK inhibitors. Recently, artificial intelligence enabled the identification of a group of approved drugs that could inhibit clathrin-mediated endocytosis and thereby inhibit viral infection of cells.145 , 146 The drug targets are members of the numb-associated kinase (NAK) family. Baricitinib was identified as a NAK inhibitor, with a particularly high affinity for AAK1, a pivotal regulator of clathrin-mediated endocytosis. This drug is also known to target JAK and could have a dual action against the virus and inflammation.147 The NIH/NIAID sponsored ACTT-2 study is still ongoing and compares remdesivir to remdesivir plus baricitinib in patients with moderate to severe COVID-19. In a small uncontrolled cohort of Veterans Affairs patients with moderate-severe COVID-19, treatment with baricitinib plus hydroxychloroquine was associated with recovery in 11 of 15 patients.148
Two other kinase inhibitors, namely imatinib mesylate and dasatinib, could also be envisaged to treat COVID-19.149 Furthermore, ruxolitinib (another JAK inhibitor-Incyte) is being evaluated in a multicentre phase II clinical trial.150
Therapeutic antibodies
Therapeutic antibodies are becoming increasingly attractive for the treatment of SARS-CoV-2, as they can be designed to specifically target viral antigens. REGN-COV-2 is a dual-antibody cocktail that contains 2 potent, non-competing and virus-neutralising antibodies (Regeneron, press release). The 2 antibodies of REGN-COV-2 bind non-competitively to critical portions of the receptor-binding domain of the virus' spike protein. The treatment could also help prevent infection by blocking the ability of the spike protein to bind to target host cells and facilitate viral entry. In addition to Regeneron, Eli Lilly, AbCellera and other companies also began testing their antibody treatment in humans.
Convalescent plasma
The immediate use of convalescent plasma provides a promising treatment. In a preliminary uncontrolled case series of 5 critically ill patients with COVID-19 and ARDS, administration of convalescent plasma containing neutralising antibody was followed by improvement in their clinical status.71 The limited sample size of this study precludes a definitive statement about the efficacy of this treatment.
Vaccines
Vaccines are the most effective strategy for preventing infectious disease as they reduce morbidity and mortality, and they are more cost-effective than treatment. Despite previous coronavirus epidemics, there is still no approved vaccine for human coronaviruses.
We will have to improve our understanding and knowledge regarding immune responses to SARS-CoV-2. Interestingly, in rhesus macaques, comparing the humoral and cellular immunity between primary infection and re-challenge revealed notably enhanced neutralising antibody and immune responses.151 These results suggest that primary SARS-CoV-2 exposure protects against subsequent reinfection in rhesus macaques. In humans, a large study of the Icelandic population reported that the humoral response did not decline within 4 months after infection, that 44% of persons who had been infected had not been diagnosed with PCR, and that the fatality rate was 0.3%.152 We must also recall that cases of SARS-CoV-2 reinfection have been reported. Epidemiological, clinical, serological and genomic analyses confirmed that the patient had reinfection instead of persistent viral shedding from first infection.153 This case leads to several open questions: How frequent is reinfection? Are reinfections less severe than the first infection? Will a vaccine protect against reinfections? These results suggest SARS-CoV-2 may continue to circulate among the human population despite herd immunity (whether due to natural infection or vaccination). Further studies of patients with reinfection will shed light on protective correlates important for vaccine design.
In the past two decades, the world has seen three coronaviruses emerge and cause outbreaks that have caused considerable global health consternation,154 with no vaccine available up to now. Regarding vaccine development, among the different strategies, we can recall the use of recombinant subunit vaccines, DNA vaccines and mRNA vaccines. Subunit vaccines are believed to be highly safe because they are expected to induce the immune system without introducing infectious viruses.155 A better knowledge of SARS-CoV-2 spike and/or N protein organisations will be required to develop such vaccines. The SARS-CoV-2 spike glycoprotein mediates host cell attachment and is required for viral entry; it is the primary vaccine target for many candidate SARS-CoV-2 vaccines.
DNA vaccines are based on direct injection of plasmids encoding the desired viral antigens, which induce a large range of immune responses. mRNA-based vaccines contain mRNAs encoding the antigens, which are translated at the host cellular machinery by vaccination.156 mRNA vaccines have advantages over conventional vaccines, including the absence of genome integration, the improved immune responses, their rapid development, and the production of multimeric antigens .156 , 157
A preliminary report on an mRNA vaccine against SARS-CoV-2 has been published.158 The candidate vaccine mRNA-1273 (Moderna) is a lipid nanoparticle–encapsulated, nucleoside-modified mRNA–based vaccine that encodes the SARS-CoV-2 spike glycoprotein stabilised in its prefusion conformation. A phase I, dose-escalation, open-label trial was conducted including 45 healthy adults, who received 2 vaccinations, 28 days apart, with mRNA-1273. After the second vaccination, serum-neutralising activity was detected in all participants evaluated. The pseudovirus neutralising activity was low before the second vaccination, which supports the need for a 2-dose vaccination schedule. Finally, the mRNA-1273 vaccine-induced anti-SARS-CoV-2 immune responses in all participants, with no limiting safety concerns. The significance of SARS-Cov-2 binding and neutralising antibody titres and their capacity to prevent infection will have to be determined. Humoral and cell-mediated immune responses have been associated with vaccine-induced protection against challenge or subsequent re-challenge after SARS-CoV-2 infection in a rhesus macaque model.159 Long-term assessment will be relevant given that natural history studies suggest that SARS-CoV may not generate long-lived antibody responses.160 Furthermore, safety evaluations are mandatory since there have been concerns about the potential for vaccine-associated enhanced respiratory disease. Of the 3 doses evaluated, the 100 μg dose elicits high neutralisation responses and Th1-skewed CD4 T cell responses, coupled with a reactogenicity profile that is more favourable than that of the higher dose.
In addition, we want to mention the results of 2 early phase COVID-19 vaccine trials, one at Oxford University (UK), with support from AstraZeneca,161 and the second supported by CanSino Biologics in China.162 Both groups used an adenoviral vector, and both report the vaccine achieving humoral responses against the SARS-CoV-2 spike glycoprotein receptor-binding domain by day 28, as well as T cell responses. Both report local and systemic mild adverse events such as fever, fatigue, and injection site pain. Neither trial reported a severe adverse event.
Although these preliminary data are encouraging, SARS-CoV-2 is a novel pathogen in humans, and many of the technologies being used to build vaccines are relatively untested. There is still a long way to go and phase III trials of these vaccines will require thousands of participants in order to confirm efficacy and safety.
Conclusions
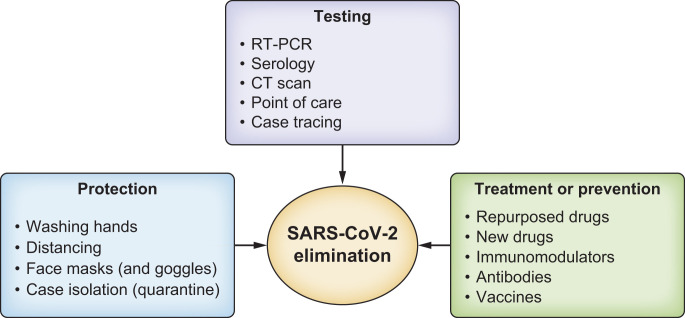
Box 1 summarises the future goals of COVID-19 research. The rapid sequencing of the virus has enabled the development of diagnostic tools. Test and trace programmes are essential and later, “test, trace and treat (T3)” programmes will become mandatory once effective drugs have been identified and safe therapies developed (Fig. 5 ). There remain several important issues that require clarification. It will be important to precisely determine how transmissible and pathogenic SARS-CoV-2 is in the ongoing and future epidemic. Furthermore, it is important to improve diagnostic tools. Ideally a single or combined test that provides virological and serological output would be ideal. In many countries, at the end of containment, strict recommended measures will be important to avoid new waves of contamination. However, few innovative treatment modalities have been discovered since the bulk of the effort to date has been focused on a vaccine. Vaccines might not be enough to quell this pandemic. Although many repurposed drug candidates are being evaluated, many are redundant and lack a strong rationale for clinical development. There is a small chance that some trials could grind to a halt, simply because the pandemic has been so well controlled by lockdowns and other measures. However, the risks of epidemics of coronavirus remain clear and present and it is imperative that work continues to develop vaccines and effective drugs for coronaviruses, to prevent future social and economic hardships around the world.
Box 1. COVID-19: future research goals.
 |
COVID-19, coronavirus disease 2019.
Fig. 5.
Milestones for SARS-CoV-2 elimination.
To achieve SARS-CoV-2 elimination there will be a need to improve protection, testing, treating and preventing strategies. Test and trace programmes will be essential. Later, test, trace and treat (T3) programmes will become mandatory once effective and safe therapies are developed. SARS-CoV-2, severe acute respiratory syndrome-coronavirus 2.
Abbreviations
ACE-2, angiotensin-converting enzyme 2; ARDS, acute respiratory distress syndrome; CLIA, chemiluminescent immunoassay; 3CLpro/Nsp5, chemotrypsin-like protease; COVID-19, coronavirus disease 2019; Ct, cycle threshold; DIC, disseminated intravascular coagulopathy; ELISA, enzyme-linked immunosorbent assay; ER, endoplasmic reticulum; ICU, intensive care unit; IL, interleukin; ISG, interferon-stimulated gene; JAK, Janus kinase; LFIAs, lateral flow immunoassays; NAK, numb-associated kinase; PLpro/Nsp3, papain-like cysteine protease; RdRp, RNA-dependent RNA polymerase; RT-qPCR, reverse transcription quantitative PCR; SARS, severe acute respiratory syndrome; SARS-CoV, SARS-coronavirus; SARS-CoV-2, SARS-coronavirus 2; SOC, standard of care; TMPRSS2, transmembrane serine protease 2; TNF-α, tumour necrosis factor-α; WHO, World Health Organization.
Financial support
Supported in part by NIH grant R01-AI-141327, the Center for AIDS Research/NIH grant P30-AI-050409 United States; and National Science Foundation grant 2032273 (to RFS).
Authors' contributions
TA designed, supervised and prepared the manuscript. All the authors contributed to the drafting of the review, the critical revision of the manuscript and its final approval.
Conflict of interest
Tarik Asselah has acted as a speaker and investigator for AbbVie, Janssen, Gilead, Roche, and Merck. David Durantel, Eric Pasmant and George Lau have nothing to declare. Raymond Schinazi was an unpaid consultant for Lilly and holds equity in Lilly and Gilead.
Please refer to the accompanying ICMJE disclosure forms for further details.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhep.2020.09.031.
Supplementary data
References
- 1.WHO Covid-19 situation report 181. Available at: https://www.who.int/. Accessed 4 September 2020.
- 2.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snijder E.J., Limpens R.W.A.L., de Wilde A.H., de Jong A.W.M., Zevenhoven-Dobbe J.C., Maier H.J., et al. A unifying structural and functional model of the coronavirus replication organelle: tracking down RNA synthesis. PLoS Biol. 2020;18(6):e3000715. doi: 10.1371/journal.pbio.3000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng S., Fan J., Yu F., Feng B., Lou B., Zou Q., et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. 2020;369:m1443. doi: 10.1136/bmj.m1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F., et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asselah T., Marcellin P., Schinazi R.F. Treatment of hepatitis C virus infection with direct-acting antiviral agents: 100% cure? Liver Int. 2018;38(S1):7–13. doi: 10.1111/liv.13673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamers M.M., Beumer J., Van der Vaart J., Knoops K., Puschhof J., Breugem T.I., et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369(6499):50–54. doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magrone T., Magrone M., Jirillo E. Focus on receptors for coronaviruses with special reference to angiotensin-converting enzyme 2 as a potential drug target - a perspective. Endocr Metab Immune Disord Drug Targets. 2020;20(6):807–811. doi: 10.2174/1871530320666200427112902. [DOI] [PubMed] [Google Scholar]
- 14.Sungnak W., Huang N., Becavin C., Berg M., Queen R., Litvinukova M., et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26(5):681–687. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ziegler C.G.K., Allon S.J., Nyquist S.K., Mbano I.M., Miao V.N., Tzouanas C.N., et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016–1035. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shang J., Ye G., Shi K., Wan Y., Luo C., Aihara H., et al. Structural basis of receptor recognition by SARS-CoV-2. Nature. 2020;581(7807):221–224. doi: 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baumert T.F., Berg T., Lim J.K., Nelson D.R. Status of direct-acting antiviral therapy for hepatitis C virus infection and remaining challenges. Gastroenterology. 2019;156:431–445. doi: 10.1053/j.gastro.2018.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao Y., Yan L., Huang Y., Liu F., Zhao Y., Cao L., et al. Structure of the RNA-dependent RNA polymerase from COVID-19 virus. Science. 2020;368(6492):779–782. doi: 10.1126/science.abb7498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirchdoerfer R.N., Ward A.B. Structure of the SARS-CoV nsp12 polymerase bound to nsp7 and nsp8 co-factors. Nat Commun. 2019;10:2342. doi: 10.1038/s41467-019-10280-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghosh A.K., Brindisi M., Shahabi D., Chapman M.E., Mesecar A.D. Drug development and medicinal chemistry efforts toward SARS-coronavirus and Covid-19 therapeutics. ChemMedChem. 2020;15(11):907–932. doi: 10.1002/cmdc.202000223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dai W., Zhang B., Su H., Li J., Zhao Y., Xie X., et al. Structure-based design of antiviral drug candidates targeting the SARS-CoV-2 main protease. Science. 2020;368(6497):1331–1335. doi: 10.1126/science.abb4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin Z., Du X., Xu Y., Deng Y., Liu M., Zhao Y., et al. Structure of M(pro) from COVID-19 virus and discovery of its inhibitors. Nature. 2020;582(7811):289–293. doi: 10.1038/s41586-020-2223-y. [DOI] [PubMed] [Google Scholar]
- 23.Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H., et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ledford H. How does COVID-19 kill? Uncertainty is hampering doctors' ability to choose treatments. Nature. 2020;580:311–312. doi: 10.1038/d41586-020-01056-7. [DOI] [PubMed] [Google Scholar]
- 25.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J., et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pedersen S.F., Ho Y.C. SARS-CoV-2: a storm is raging. J Clin Invest. 2020;130:2202–2205. doi: 10.1172/JCI137647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang F., Hou H., Luo Y., Tang G., Wu S., Huang M., et al. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight. 2020;5(10):e137799. doi: 10.1172/jci.insight.137799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ziegler C.G.K., Allon S.J., Nyquist S.K., Mbano I.M., Miao V.N., Tzouanas C.N., et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016–1035.e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weissleder R., Lee H., Ko J., Pittet M.J. COVID-19 diagnostics in context. Sci Transl Med. 2020;12(546):eabc1931. doi: 10.1126/scitranslmed.abc1931. [DOI] [PubMed] [Google Scholar]
- 30.Tang Y.W., Schmitz J.E., Persing D.H., Stratton C.W. The laboratory diagnosis of COVID-19 infection: current issues and challenges. J Clin Microbiol. 2020;58(6):e00512–e00520. doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K., et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Osório N.S., Correia-Neves M. Implication of SARS-CoV-2 evolution in the sensitivity of RT-qPCR diagnostic assays. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30435-7. S1473–3099(20)30435-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sethuraman N., Jeremiah S.S., Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020;323(22):2249–2251. doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- 34.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vogels C.B.F., Brito A.F., Wyllie A.L., Fauver J.R., Ott I.M., Kalinich C.C., et al. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT-qPCR primer-probe sets. Nat Microbiol. 2020;5:1299–1305. doi: 10.1038/s41564-020-0761-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han M.S., Byun J.H., Cho Y., Rim J.H. RT-PCR for SARS-CoV-2: quantitative versus qualitative. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30424-2. S1473-3099(20)30424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Y., Yan L.M., Wan L., Xiang T.X., Le A., Liu J.M., et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020;20(6):656–657. doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng M.P., Papenburg J., Desjardins M., Kanjilal S., Quach C., Libman M., et al. Diagnostic testing for severe acute respiratory syndrome-related coronavirus-2: a narrative review. Ann Intern Med. 2020;172(11):726–734. doi: 10.7326/M20-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woloshin S., Patel N., Kesselheim A.S. False negative tests for SARS-CoV-2 infection - challenges and implications. N Engl J Med. 2020;383(6):e38. doi: 10.1056/NEJMp2015897. [DOI] [PubMed] [Google Scholar]
- 40.Kucirka L.M., Lauer S.A., Laeyendecker O., Boon D., Lessler J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann Intern Med. 2020;173(4):262–267. doi: 10.7326/M20-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hogan C.A., Sahoo M.K., Pinsky B.A. Sample pooling as a strategy to detect community transmission of SARS-CoV-2. JAMA. 2020;323(19):1967–1969. doi: 10.1001/jama.2020.5445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lohse S., Pfuhl T., Berkó-Göttel B., Rissland J., Geißler T., Gärtner B., et al. Pooling of samples for testing for SARS-CoV-2 in asymptomatic people. Lancet Infect Dis. 2020:1231–1232. doi: 10.1016/S1473-3099(20)30362-5. www.thelancet.com/journals/laninf/issue/vol20no11/PIIS1473-3099(20)X0011-9www.thelancet.com/journals/laninf/issue/vol20no11/PIIS1473-3099(20)X0011-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mallapaty S. The mathematical strategy that could transform coronavirus testing. Nature. 2020;583(7817):504–505. doi: 10.1038/d41586-020-02053-6. [DOI] [PubMed] [Google Scholar]
- 44.Park G.S., Ku K., Baek S.H., Kim S.J., Kim S.I., Kim B.T., et al. Development of reverse transcription loop-mediated Isothermal amplification assays targeting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) J Mol Diagn. 2020;22(6):729–735. doi: 10.1016/j.jmoldx.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Broughton J.P., Deng X., Yu G., Fasching C.L., Servellita V., Singh J., et al. CRISPR-Cas12-based detection of SARS-CoV-2. Nat Biotechnol. 2020;38(7):870–874. doi: 10.1038/s41587-020-0513-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ackerman C.M., Myhrvold C., Thakku S.G., Freije C.A., Metsky H.C., Yang D.K., et al. Massively multiplexed nucleic acid detection with Cas13. Nature. 2020;582(7811):277–282. doi: 10.1038/s41586-020-2279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R., et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382(22):2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolfel R., Corman V.M., Guggemos W., Seilmaier M., Zange S., Muller M.A., et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 50.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Young B.E., Ong S.W.X., Kalimuddin S., Low J.G., Tan S.Y., Loh J., et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488–1494. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vermeiren C., Marchand-Senecal X., Sheldrake E., Bulir D., Smieja M., Chong S., et al. Comparison of Copan Eswab and FLOQswab for COVID-19 PCR diagnosis: working around a supply shortage. J Clin Microbiol. 2020;58(6):e00669-20. doi: 10.1128/JCM.00669-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marty F.M., Chen K., Verrill K.A. How to obtain a nasopharyngeal swab specimen. N Engl J Med. 2020;382(22):e76. doi: 10.1056/NEJMvcm2010260. [DOI] [PubMed] [Google Scholar]
- 55.To K.K., Tsang O.T., Leung W.S., Tam A.R., Wu T.C., Lung D.C., et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20(5):565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Williams E., Bond K., Zhang B., Putland M., Williamson D.A. Saliva as a non-invasive specimen for detection of SARS-CoV-2. J Clin Microbiol. 2020;58(8) doi: 10.1128/JCM.00776-20. e00776-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abbasi J. The promise and peril of antibody testing for COVID-19. JAMA. 2020;323(19):1881–1883. doi: 10.1001/jama.2020.6170. [DOI] [PubMed] [Google Scholar]
- 58.Petherick A. Developing antibody tests for SARS-CoV-2. Lancet. 2020;395:1101–1102. doi: 10.1016/S0140-6736(20)30788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Amanat F., Stadlbauer D., Strohmeier S., Nguyen T.H.O., Chromikova V., McMahon M., et al. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nat Med. 2020;26(7):1033–1036. doi: 10.1038/s41591-020-0913-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guo L., Ren L., Yang S., Xiao M., Chang D., Yang F., et al. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19) Clin Infect Dis. 2020;71(15):778–785. doi: 10.1093/cid/ciaa310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Long Q.X., Liu B.Z., Deng H.J., Wu G.C., Deng K., Chen Y.K., et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med. 2020;26(6):845–848. doi: 10.1038/s41591-020-0897-1. [DOI] [PubMed] [Google Scholar]
- 62.Peiris J.S., Lai S.T., Poon L.L., Guan Y., Yam L.Y., Lim W., et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zost S.J., Gilchuk P., Case J.B., Binshtein E., Chen R.E., Nkolola J.P. Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature. 2020;584(7821):443–449. doi: 10.1038/s41586-020-2548-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu Y., Eggo R.M., Kucharski A.J. Secondary attack rate and superspreading events for SARS-CoV-2. Lancet. 2020;395:e47. doi: 10.1016/S0140-6736(20)30462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu L., Wang P., Nair M.S., Yu J., Rapp M., Wang Q., et al. Potent neutralizing antibodies against multiple epitopes on SARS-CoV-2 spike. Nature. 2020;584(7821):450–456. doi: 10.1038/s41586-020-2571-7. [DOI] [PubMed] [Google Scholar]
- 66.Grifoni A., Weiskopf D., Ramirez S.I., Mateus J., Dan J.M., Moderbacher C.R., et al. Targets of T Cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181(7):1489–1501. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ju B., Zhang Q., Ge J., Wang R., Sun J., Ge X., et al. Human neutralizing antibodies elicited by SARS-CoV-2 infection. Nature. 2020;584(7819):115–119. doi: 10.1038/s41586-020-2380-z. [DOI] [PubMed] [Google Scholar]
- 68.Ou X., Liu Y., Lei X., Li P., Mi D., Ren L., et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sette A., Crotty S. Pre-existing immunity to SARS-CoV-2: the knowns and unknowns. Nat Rev Immunol. 2020;20(8):457–458. doi: 10.1038/s41577-020-0389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pinto D., Park Y.J., Beltramello M., Walls A.C., Tortorici M.A., Bianchi S., et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature. 2020;583(7815):290–295. doi: 10.1038/s41586-020-2349-y. [DOI] [PubMed] [Google Scholar]
- 71.Shen C., Wang Z., Zhao F., Yang Y., Li J., Yuan J., et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA. 2020;323(16):1582–1589. doi: 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rogers T.F., Zhao F., Huang D., Beutler N., Burns A., He W.T., et al. Isolation of potent SARS-CoV-2 neutralizing antibodies and protection from disease in a small animal model. Science. 2020;369(6506):956–963. doi: 10.1126/science.abc7520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lisboa Bastos M., Tavaziva G., Abidi S.K., Campbell J.R., Haraoui L.P., Johnston J.C., et al. Diagnostic accuracy of serological tests for covid-19: systematic review and meta-analysis. BMJ. 2020;370:m2516. doi: 10.1136/bmj.m2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Deeks J.J., Dinnes J., Takwoingi Y., Davenport C., Spijker R., Taylor-Phillips S., et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev. 2020;6:CD013652. doi: 10.1002/14651858.CD013652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.GeurtsvanKessel C.H., Okba N.M.A., Igloi Z., Bogers S., Embregts C.W.E., Laksono B.M., et al. An evaluation of COVID-19 serological assays informs future diagnostics and exposure assessment. Nat Commun. 2020;11(1):3436. doi: 10.1038/s41467-020-17317-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kofler N., Baylis F. Ten reasons why immunity passports are a bad idea. Nature. 2020;581(7809):379–381. doi: 10.1038/d41586-020-01451-0. [DOI] [PubMed] [Google Scholar]
- 77.Gupta N., Zhao Y.Y., Evans C.E. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 78.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.George P.M., Wells A.U., Jenkins R.G. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir Med. 2020;8(8):807–815. doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N., et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kanne J.P., Little B.P., Chung J.H., Elicker B.M., Ketai L.H. Essentials for radiologists on COVID-19: an update-radiology scientific expert panel. Radiology. 2020;296(2):E113–E114. doi: 10.1148/radiol.2020200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wong H.Y.F., Lam H.Y.S., Fong A.H., Leung S.T., Chin T.W., Lo C.S.Y., et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020;296(2):E72–E78. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382(23):2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Guidon A.C., Amato A.A. COVID-19 and neuromuscular disorders. Neurology. 2020;94(22):959–969. doi: 10.1212/WNL.0000000000009566. [DOI] [PubMed] [Google Scholar]
- 91.Wollina U., Karadağ A.S., Rowland-Payne C., Chiriac A., Lotti T. Cutaneous signs in COVID-19 patients: a review. Dermatol Ther. 2020:e13549. doi: 10.1111/dth.13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gabarre P., Dumas G., Dupont T., Darmon M., Azoulay E., Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020;46(7):1339–1348. doi: 10.1007/s00134-020-06153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cai Q., Huang D., Yu H., Zhu Z., Xia Z., Su Y., et al. COVID-19: abnormal liver function tests. J Hepatol. 2020;73(3):566–574. doi: 10.1016/j.jhep.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xu L., Liu J., Lu M., Yang D., Zheng X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020;40:998–1004. doi: 10.1111/liv.14435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ji D., Zhang D., Yang T.N., Mu J.S., Zhao P., Xu J., et al. Effect of COVID-19 on patients with compensated chronic liver diseases. Hepatol Int. 2020;14(5):701–710. doi: 10.1007/s12072-020-10058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ji D., Qin E., Xu J., Zhang D., Cheng G., Wang Y., et al. Non-alcoholic fatty liver diseases in patients with COVID-19: a retrospective study. J Hepatol. 2020;73(2):451–453. doi: 10.1016/j.jhep.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhou Y.J., Zheng K.I., Wang X.B., Yan H.D., Sun Q.F., Pan K.H., et al. Younger patients with MAFLD are at increased risk of severe COVID-19 illness: a multicenter preliminary analysis. J Hepatol. 2020;73(3):719–721. doi: 10.1016/j.jhep.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cheung K.S., Hung I.F., Chan P.P., Lung K.C., Tso E., Liu R., et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong cohort and systematic review and meta-analysis. Gastroenterology. 2020;159(1):81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ag. Insights for hepatology and liver transplant providers during the COVID-19 pandemic. 2020. http://www.aasld.org/sites/default/files/2020-04/AASLD-COVID19-ClinicalInsights-4.07.2020-Final.pdf Available at:
- 101.E-EPP Care of patients with liver disease during the COVID-19 pandemic. J Hepatol. 2020 https://easl.eu/wp-content/uploads/2020/04/EASL-ESCMID-Position-Paper-on-COVID-19-and-the-liver-2-April-2020.pdf in press. Available at: [Google Scholar]
- 102.Force AEPCRbACT Clinical practice guidance for hepatology and liver transplant providers during the COVID-19 pandemic. Hepatol Int. 2020;14(4):415–428. doi: 10.1007/s12072-020-10054-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhao B., Ni C., Gao R., Wang Y., Yang L., Wei J., et al. Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids. Protein Cell. 2020;11(10):771–775. doi: 10.1007/s13238-020-00718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Boeckmans J., Rodrigues R.M., Demuyser T., Pierard D., Vanhaecke T., Rogiers V. COVID-19 and drug-induced liver injury: a problem of plenty or a petty point? Arch Toxicol. 2020;94(4):1367–1369. doi: 10.1007/s00204-020-02734-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20:269–270. doi: 10.1038/s41577-020-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wang Y., Zhang D., Du G., Du R., Zhao J., Jin Y., et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395(10236):1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang X.J., Cheng X., Yan Z.Z., Fang J., Wang X., Wang W., et al. An ALOX12-12-HETE-GPR31 signaling axis is a key mediator of hepatic ischemia-reperfusion injury. Nat Med. 2018;24:73–83. doi: 10.1038/nm.4451. [DOI] [PubMed] [Google Scholar]
- 108.Lau G., Ward J. Synthesis of liver associations recommendations for hepatology and liver transplant care during the COVID-19 pandemic. Clin Liver Dis. 2020;15(5):204–209. doi: 10.1002/cld.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tian Y., Rong L., Nian W.D., He Y. Review article:gastrointestinal features in COVID-19 and the possibility of fecal transmission. Aliment Pharmacol Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mao R., Qiu Y., He J.S., Tan J.Y., Li X.H., Liang J., et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Young B.E., Ong S.W.X., Kalimuddin S., Low J.G., Tan S.Y., Loh J., et al. Epidemiologic features clinical course patients infected with SARS-CoV-2 Singapore. JAMA. 2020;323(15):1488–1494. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jin X., Lian J.S., Hu J.H., Gao J., Zheng L., Zhang Y.M., et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pan L., Mu M., Yang P., Sun Y., Wang R., Yan J., et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831–1833.e3. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cheung E., Ting V., Cheng L. Coronavirus: Hong Kong public housing estate evacuated after cluster of Covid-19 infections found. https://www.scmp.com/news/hong-kong/health-environment/article/3087526/coronavirus-new-cluster-infection-expands-elderly Available at:
- 116.Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wu X., Cai Y., Huang X., Yu X., Zhao L., Wang F., et al. Co-infection with SARS-CoV-2 and influenza A virus in patient with pneumonia. China Emerg Infect Dis. 2020;26(6):1324–1326. doi: 10.3201/eid2606.200299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tian H., Liu Y., Li Y., Wu C.H., Chen B., Kraemer M.U.G., et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kraemer M.U.G., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M., et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ferretti L., Wymant C., Kendall M., Zhao L., Nurtay A., Abeler-Dorner L., et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368:eabb6936. doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pushpakom S., Iorio F., Eyers P.A., Escott K.J., Hopper S., Wells A., et al. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov. 2019;18:41–58. doi: 10.1038/nrd.2018.168. [DOI] [PubMed] [Google Scholar]
- 122.Colson P., Rolain J.M., Raoult D. Chloroquine for the 2019 novel coronavirus SARS-CoV-2. Int J Antimicrob Agents. 2020;55:105923. doi: 10.1016/j.ijantimicag.2020.105923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Cortegiani A., Ingoglia G., Ippolito M., Giarratano A., Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;59:176–190. doi: 10.1016/j.jcrc.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tang W., Cao Z., Han M., Wang Z., Chen J., Sun W., et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020;369:m1849. doi: 10.1136/bmj.m1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Vastag B. Old drugs for a new bug: influenza, HIV drugs enlisted to fight SARS. JAMA. 2003;290:1695–1696. doi: 10.1001/jama.290.13.1695. [DOI] [PubMed] [Google Scholar]
- 126.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G., et al. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Choy K.T., Wong A.Y., Kaewpreedee P., Sia S.F., Chen D., Hui K.P.Y., et al. Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antiviral Res. 2020;178:104786. doi: 10.1016/j.antiviral.2020.104786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M., et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Grein J., Ohmagari N., Shin D., Diaz G., Asperges E., Castagna A., et al. Compassionate use of remdesivir for patients with severe covid-19. N Engl J Med. 2020;382:2327–2336. doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Goldman J.D., Lye D.C.B., Hui D.S., Marks K.M., Bruno R., Montejano R., et al. Remdesivir for 5 or 10 days in patients with severe Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2015301. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Blaising J., Polyak S.J., Pecheur E.I. Arbidol as a broad-spectrum antiviral: an update. Antiviral Res. 2014;107:84–94. doi: 10.1016/j.antiviral.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhu Z., Lu Z., Xu T., Chen C., Yang G., Zha T., et al. Arbidol monotherapy is superior to lopinavir/ritonavir in treating COVID-19. J Infect. 2020;81(1):e21–e23. doi: 10.1016/j.jinf.2020.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Cai Q., Yang M., Liu D., Chen J., Shu D., Xia J., et al. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering. 2020 doi: 10.1016/j.eng.2020.03.007. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Anand K., Ziebuhr J., Wadhwani P., Mesters J.R., Hilgenfeld R. Coronavirus main proteinase (3CLpro) structure: basis for design of anti-SARS drugs. Science. 2003;300(5626):1763–1767. doi: 10.1126/science.1085658. [DOI] [PubMed] [Google Scholar]
- 135.Freedberg D.E., Conigliaro J., Wang T.C., Tracey K.J., Callahan M.V., Abrams J.A., et al. Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 Patients: a propensity score matched retrospective cohort study. Gastroenterology. 2020;159(3):1129–1131.e3. doi: 10.1053/j.gastro.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L., Linsell L., et al. Dexamethasone in hospitalized patients with covid-19-preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Villar J., Ferrando C., Martínez D., Ambrós A., Muñoz T., Soler J.A., et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multi- centre, randomised controlled trial. Lancet Respir Med. 2020;8:267–276. doi: 10.1016/S2213-2600(19)30417-5. [DOI] [PubMed] [Google Scholar]
- 138.He X., Lau E.H.Y., Wu P., Deng X., Wang J., Hao X., et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 139.Hung I.F., Lung K.C., Tso E.Y., Liu R., Chung T.W., Chu M.Y., et al. Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet. 2020;395(10238):1695–1704. doi: 10.1016/S0140-6736(20)31042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Musumeci F., Greco C., Giacchello I., Fallacara A.L., Ibrahim M.M., Grossi G., et al. An update on JAK inhibitors. Curr Med Chem. 2019;26:1806–1832. doi: 10.2174/0929867325666180327093502. [DOI] [PubMed] [Google Scholar]
- 141.Winthrop K.L. The emerging safety profile of JAK inhibitors in rheumatic disease. Nat Rev Rheumatol. 2017;13:234–243. doi: 10.1038/nrrheum.2017.23. [DOI] [PubMed] [Google Scholar]
- 142.Gavegnano C., Brehm J.H., Dupuy F.P., Talla A., Ribeiro S.P., Kulpa D.A., et al. Novel mechanisms to inhibit HIV reservoir seeding using Jak inhibitors. PLoS Pathog. 2017;13:e1006740. doi: 10.1371/journal.ppat.1006740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Gavegnano C., Detorio M., Montero C., Bosque A., Planelles V., Schinazi R.F. Ruxolitinib and tofacitinib are potent and selective inhibitors of HIV-1 replication and virus reactivation in vitro. Antimicrob Agents Chemother. 2014;58:1977–1986. doi: 10.1128/AAC.02496-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Gavegnano C., Haile W.B., Hurwitz S., Tao S., Jiang Y., Schinazi R.F., et al. Baricitinib reverses HIV-associated neurocognitive disorders in a SCID mouse model and reservoir seeding in vitro. J Neuroinflammation. 2019;16:182. doi: 10.1186/s12974-019-1565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Richardson P., Griffin I., Tucker C., Smith D., Oechsle O., Phelan A., et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395:e30–e31. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stebbing J., Krishnan V., de Bono S., Ottaviani S., Casalini G., Richardson P.J., et al. Mechanism of baricitinib supports artificial intelligence-predicted testing in COVID-19 patients. EMBO Mol Med. 2020;12(8):e12697. doi: 10.15252/emmm.202012697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cantini F., Niccoli L., Matarrese D., Nicastri E., Stobbione P., Goletti D. Baricitinib therapy in COVID-19: a pilot study on safety and clinical impact. J Infect. 2020;81(2):318–356. doi: 10.1016/j.jinf.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Titanji B.K., Farley M.M., Mehta A., Connor-Schuler R., Moanna A., Cribbs S.K., et al. Use of Baricitinib in patients with moderate and severe COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dyall J., Coleman C.M., Hart B.J., Venkataraman T., Holbrook M.R., Kindrachuk J., et al. Repurposing of clinically developed drugs for treatment of Middle East respiratory syndrome coronavirus infection. Antimicrob Agents Chemother. 2014;58:4885–4893. doi: 10.1128/AAC.03036-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.La Rosée F., Bremer H.C., Gehrke I., Kehr A., Hochhaus A., Birndt S., et al. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation. Leukemia. 2020;34(7):1805–1815. doi: 10.1038/s41375-020-0891-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Deng W., Bao L., Liu J., Xiao C., Liu J., Xue J., et al. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020;369(6505):818–823. doi: 10.1126/science.abc5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Gudbjartsson D.F., Norddahl G.L., Melsted P., Gunnarsdottir K., Holm H., Eythorsson E., et al. Humoral immune response to SARS-CoV-2 in Iceland. N Engl J Med. 2020;383(18):1724–1734. doi: 10.1056/NEJMoa2026116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.To K.K., Hung I.F., Ip J.D., Chu A.W., Chan W.M., Tam A.R., et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1275. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Guarner J. Three emerging coronaviruses in two decades. Am J Clin Pathol. 2020;153:420–421. doi: 10.1093/ajcp/aqaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Du L., He Y., Zhou Y., Liu S., Zheng B.J., Jiang S. The spike protein of SARS-CoV–a target for vaccine and therapeutic development. Nat Rev Microbiol. 2009;7:226–236. doi: 10.1038/nrmicro2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Pardi N., Hogan M.J., Porter F.W., Weissman D. mRNA vaccines - a new era in vaccinology. Nat Rev Drug Discov. 2018;17:261–279. doi: 10.1038/nrd.2017.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Stadler K., Masignani V., Eickmann M., Becker S., Abrignani S., Klenk H.D., et al. SARS–beginning to understand a new virus. Nat Rev Microbiol. 2003;1:209–218. doi: 10.1038/nrmicro775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jackson L.A., Anderson E.J., Rouphael N.G., Roberts P.C., Makhene M., Coler R.N., et al. An mRNA vaccine against SARS-CoV-2-preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2022483. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Chandrashekar A., Liu J., Martinot A.J., McMahan K., Mercado N.B., Peter L., et al. SARS-CoV-2 infection protects against rechallenge in rhesus macaques. Science. 2020;369(6505):812–817. doi: 10.1126/science.abc4776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Cao W.-C., Liu W., Zhang P.-H., Zhang F., Richardus J.H. Disappearance of antibodies to SARS-associated coronavirus after recovery. N Engl J Med. 2007;357:1162–1163. doi: 10.1056/NEJMc070348. [DOI] [PubMed] [Google Scholar]
- 161.Folegatti P.M., Ewer K.J., Aley P.K., Angus B., Becker S., Belij-Rammerstorfer S., et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396(10249):467–478. doi: 10.1016/S0140-6736(20)31604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhu F.-C., Guan X.-H., Li Y.-H., Huang J.Y., Jiang T., Hou L.H., et al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;396(10249):479–488. doi: 10.1016/S0140-6736(20)31605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.